Abstract
INTRODUCTION
The Modified Early Warning Score (MEWS) is a simple, physiological score that may allow improvement in the quality and safety of management provided to surgical ward patients. The primary purpose is to prevent delay in intervention or transfer of critically ill patients.
PATIENTS AND METHODS
A total of 334 consecutive ward patients were prospectively studied. MEWS were recorded on all patients and the primary end-point was transfer to ITU or HDU.
RESULTS
Fifty-seven (17%) ward patients triggered the call-out algorithm by scoring four or more on MEWS. Emergency patients were more likely to trigger the system than elective patients. Sixteen (5% of the total) patients were admitted to the ITU or HDU. MEWS with a threshold of four or more was 75% sensitive and 83% specific for patients who required transfer to ITU or HDU.
CONCLUSIONS
The MEWS in association with a call-out algorithm is a useful and appropriate risk-management tool that should be implemented for all surgical in-patients.
Keywords: Modified Early Warning Score, MEWS, Surgical in-patients, Management
In 1999, the Audit Commission reported that the effectiveness of critical care services varied between hospitals and recommended the development of early warning systems (EWSs) to help ward staff identify when to call for specialist advice.1 In 1999, Stenhouse et al.2 proposed a modification of Morgan's Early Warning Score.3 This Modified Early Warning Score (MEWS) was evaluated in 206 surgical patients over 9 months. The score was used selectively but there was some evidence that its use may result in earlier admission to intensive care. The components, which are recorded every time a set of observations are made, are aggregated to yield the score (Table 1). The purpose of the MEWS is to facilitate prompt communication between nursing and medical staff when deterioration in a ward patient's condition first becomes apparent on the observations chart. The authors intended this system to result in earlier intervention on the ward so that transfer to a critical care facility is either prevented or occurs without unnecessary delay.
Table 1.
Modified Early Warning Score
| Score | 3 | 2 | 1 | 0 | 1 | 2 | 3 |
|---|---|---|---|---|---|---|---|
| Respiratory rate (min−1) | ≤ 8 | 9–14 | 15–20 | 21–29 | > 29 | ||
| Heart rate (min−1) | ≤ 40 | 41–50 | 51–100 | 101–110 | 111–129 | > 129 | |
| Systolic BP (mmHg) | ≤ 70 | 71–80 | 81–100 | 101–199 | ≥ 200 | ||
| Urine output (ml/kg/h) | Nil | < 0.5 | |||||
| Temperature (°C) | ≤ 35 | 35.1–36 | 36.1–38 | 38.1–38.5 | ≥ 38.6 | ||
| Neurological | Alert | Reacting to voice | Reacting to pain | Unresponsive |
The scores for each parameter are recorded at the time that observations are taken. If the total is 4 or more then the ward doctor is informed.
The feasibility of introducing the MEWS into an acute surgical service has been demonstrated in Lanarkshire. Carberry et al.4 implemented the MEWS in a selected group which amounted to 35% of their patients. All acute admissions, postoperative patients for the first 24 h and ‘any patient causing concern’ were included. They introduced a clear call-out algorithm so that the house officer or SHO was called out to review any patient scoring four or more. This study retrospectively demonstrated that of 332 audited patients, 14 (4%) were admitted to ITU and HDU. Eleven (79%) of these had been monitored using the MEWS prior to admission but three (21%) had not had their MEWS recorded.
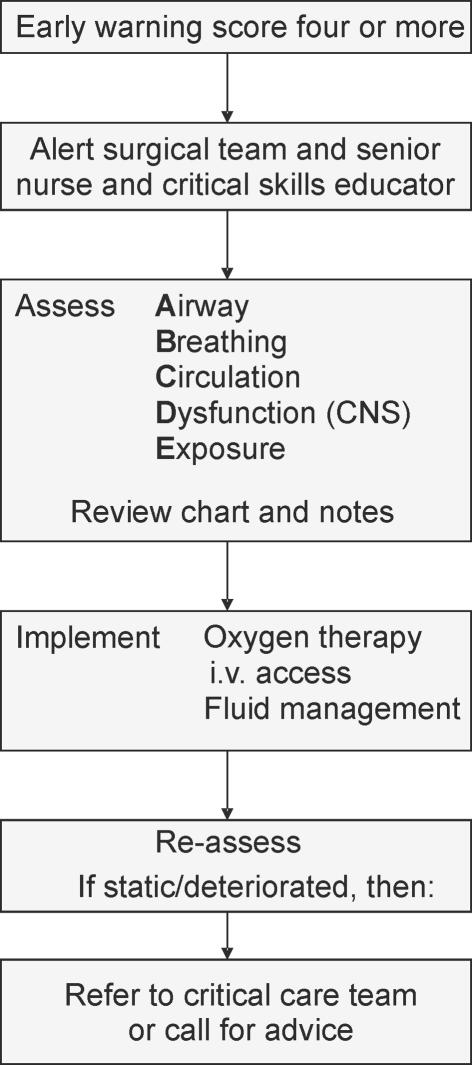
The MEWS has been implemented for surgical patients at the West Suffolk Hospital. The MEWS is recorded on the observation chart every time a set of observations is made for all patients. The call-out algorithm is shown in Figure 1. We believe that the MEWS should be used routinely on all in-patients. This approach should remove the element of subjectivity in selecting patients and for the first time has allowed us to calculate the sensitivity and specificity of the MEWS for its purpose.
Figure 1.
Call-out algorithm in use on surgical wards.
Patients and Methods
Patients
A total of 334 consecutive emergency and elective patients were admitted under the colorectal team between 16 May and 23 September 2003. Children admitted to the paediatric ward, day cases, and urological emergencies admitted initially under general surgeons but which were handed on to the care of the urologists within 24 h were excluded. Patients subject to DNAR orders were included because knowledge of their physiological state may be valuable with respect to the timing of discussion with their families.5
Prospective data collection
Patient age, gender, ASA, operation, presence of malignancy, and the length of stay were recorded. The primary end-point was admission to a critical care facility (ITU or HDU). Every weekday, the MEWS for each observation time-point was recorded from the observation charts. The component factors that made up the highest MEWS for the 24-h period were recorded. The MEWS was in use clinically on weekends. For the study, these weekend scores were collated on Mondays. In order to provide benchmarks to compare the sensitivity of the MEWS as a predictor of critical care admission, the white cell count and CRP were recorded if these had been measured as part of the patient's management. For the same reason, if any patient had the criteria of systemic inflammatory response syndrome (SIRS), this was documented prospectively. SIRS was defined using the definition of the Society of Critical Care Consensus Conference,6 which requires two or more of: (i) temperature > 38°C or < 36°C; (ii) heart rate > 90 bpm; (iii) respiratory rate > 20 min−1 or pCO2 < 4.2 kPa; and (iv) white cell count > 12.0 × 109 l−1 or < 4.0 × 109 l−1.
Data analysis and statistics
Age and daily patient count were considered as parametric data. These data are presented as mean ± SD and were analysed using ANOVA. Length of stay and ASA grade were considered as ordinal data. These were analysed for significance using the Mann-Whitney U-test. Gender, emergency or elective status, death, diagnosis of obstruction or malignancy, and existence of bowel anastomosis (categorical data) were analysed using the chi-squared statistic comparing the actual values to those that would be expected if each variable was evenly distributed between the high and low MEWS groups. Sensitivity for ITU or HDU admission was calculated by number of patients triggering system who were transferred divided by all patients transferred. Specificity was calculated by true negative divided by the total number of patients. Positive predictive value (PPV) was calculated by number transferred divided by the number triggering system. Negative predictive value (NPV) was calculated by true negative divided by the number that did not trigger the system.
Results
Patients
The mean age of the population was 58.6 years (SD ± 19.2 years). The male:female ratio was 1:1.02. Of the admissions, 123 (37%) were elective and 211 (63%) were emergency.
Trigger of early warning system
Fifty-seven (17%) of the 334 consecutive unselected ward patients triggered the call-out algorithm by scoring four or more on the MEWS. Elective patients were less likely to trigger the system than emergency patients. Compared to 22% of emergency patients, 8% of elective patients scored four or more. The group of patients that triggered the MEWS were older, more likely to have a diagnosis of malignancy or bowel obstruction, and to have a bowel anastomosis (see Table 2). This group had a higher mortality and longer hospital stay.
Table 2.
Comparison between the group of patients who triggered the call-out algorithm with the group that did not
| MEWS < 4 | MEWS ≥ 4 | Statistical test | Significance | |
|---|---|---|---|---|
| Age (years mean ± SD) | 57 ± 19.4 | 66 ± 16.7 | ANOVA | P < 0.01 |
| Gender ratio (M:F) | 140:136 | 25:33 | Chi-square | N/S |
| Percentage that were emergency admissions | 59% | 82% | Chi-square | P < 0.001 |
| ASA grade (median and range) | 2 (1−4) | 2 (1−4) | Not applicable | Not applicable |
| Anastomosis during this admission | 7.9% | 34.5% | Chi-square | P < 0.001 |
| Diagnosis of bowel obstruction | 5.8% | 23.6% | Chi-square | P < 0.001 |
| Diagnosis of malignancy | 12.6% | 38.2% | Chi-square | P < 0.001 |
| Death | 0% | 7.2% | Chi-square | P < 0.001 |
| Length of hospital stay (median and range) | 3 (1−41) | 10 (2−41) | Mann-Whitney U-test | P < 0.05 |
N/S, not significant.
Transfer to ITU or HDU
Sixteen (5% of the total) patients were admitted to the ITU or HDU. Twelve of these were transferred from theatre immediately after an emergency operation. Three emergency patients had conditions which required supportive care in ITU or HDU but did not require surgery. Only one elective case required critical care.
Mortality
There were four deaths. Two patients were admitted to ITU immediately after emergency surgery but died after support was withdrawn. The remaining two patients had advanced malignancy and were treated palliatively on the ward. None of these patients were considered to have died as a result of delayed referral to critical care.
Validation of the MEWS threshold
The value of the MEWS as a test to identify patients requiring transfer from the surgical ward to a critical care facility is shown in Table 3. For purposes of comparison, the sensitivity and specificity of a known abnormal white cell count or CRP > 100 mg/l when the patient's notes would have been reviewed are shown. The effect of using other threshold values is also shown.
Table 3.
Sensitivity and specificity of the MEWS as a predictor of admission to a critical care unit and comparison with the test results apparent on chart review
| Sensitivity | Specificity | PPV | NPV | |
|---|---|---|---|---|
| Abnormal WCC | 14/16 (88%) | 202/334 (60%) | 14/130 (11%) | 202/204 (99%) |
| CRP > 100 mg/l | 11/16 (69%) | 200/334 (60%) | 11/103 (11%) | 200/231 (87%) |
| Documented SIRS | 10/16 (63%) | 287/334 (86%) | 10/45 (22%) | 287/289 (99%) |
| MEWS 3 or more | 14/16 (88%) | 228/334 (68%) | 14/103 (14%) | 228/231 (99%) |
| MEWS 4 or more | 12/16 (75%) | 276/334 (83%) | 12/55 (22%) | 276/279 (99%) |
| MEWS 5 or more | 6/16 (38%) | 298/334 (89%) | 6/27 (22%) | 298/307 (96%) |
| MEWS 6 or more | 3/16 (19%) | 311/334 (93%) | 3/9 (33%) | 311/325 (96%) |
| MEWS 7 or more | 1/16 (6%) | 314/334 (94%) | 1/2 (50%) | 314/332 (95%) |
Using the threshold of four or more, 75% of patients who actually went to critical care had triggered the early warning system. Of those who were reviewed because of the early warning system, 22% were admitted to ITU or HDU for supportive care. This is equivalent to an NNT of 5. As expected, raising the threshold would increase the specificity but also decrease the sensitivity to unacceptable levels. Conversely, lowering the threshold would increase the sensitivity but the PPV would become unacceptably low. Findings of abnormal white cell count or CRP > 100 mg/l on review of the records were not valuable for identifying patients requiring ITU admission. However, the negative predictive value of a normal white cell count was high (99%). The MEWS showed better sensitivity than the presence of SIRS.
Four patients were transferred to ITU without triggering the early warning system. The first had necrotising fasciitis and required haemofiltration postoperatively (peak MEWS 0). The second was admitted postoperatively after anterior resection of rectum (peak score 3). The third required splenectomy for bleeding splenic artery aneurysm (peak score 2) and the fourth required a laparotomy for penetrating abdominal trauma (peak score 1). The last two cases were given aggressive fluid resuscitation before any MEWS was recorded and the decision for surgery and postoperative intensive care was easy.
Management of critically ill patients on the ward
The majority (79%) of patients who triggered the early warning system were managed successfully on the general ward. These patients are summarised in Table 4.
Table 4.
Patients scoring four or more on the MEWS who were managed successfully on the ward
| Cause for raised MEWS | Number (%) | Diagnosis | Benefits of EWS call-out |
|---|---|---|---|
| Surgical disease (prior to definitive treatment) | 4 (9.3 %) |
|
Opportunity for optimisation of fluid resuscitation |
| Recognition of urgency of surgical or endoscopic treatment of the underlying cause | |||
| Surgical disease (non-operative plan established) | 12 (28 %) |
|
Review of non-operative management plan |
| Optimise fluid and antimicrobial management | |||
| Peri-operative complications | 4 (9.3 %) |
|
Early recognition and correction of postoperative fluid overload or dehydration |
| 2 (4.6 %) |
|
Medical treatment of AF | |
| 12 (28 %) | Postoperative pyrexia/tachycardia | Consideration of septic screen, emergency chest physiotherapy | |
| ‘Non-surgical’ diagnosis made after admission | 7 (16.2 %) |
|
Changes in the vital signs can lead to early recognition of the true diagnosis (e.g. PUO as presentation of brain tumour) |
| Terminal disease | 2 (4.6 %) |
|
Palliative care for patient and informed discussion with families |
Effect of early warning system on junior doctors' daily workload
The junior doctor team were responsible for an average of 18 (SD ± 7.5) ward patients per day. The range was 4–35 patients. On 58 out of the 131 days (44%), there was one or more patient scoring 4 or more on the MEWS. The maximum number of patients on any one day with a MEWS of 4 or more was five. In accordance with the protocol, the nursing staff requested review by junior doctors in all these patients.
Discussion
It can be difficult to identify ward patients who are in danger of deterioration. According to McQuillan et al.,7 at least 39% of acute emergency patients admitted to the ITU are referred late in the clinical course of the illness. Major causes of ‘suboptimal care’ prior to transfer from the ward in their study included failure of organisation, lack of knowledge, failure to appreciate clinical urgency, lack of supervision and failure to seek advice. Initially, only the least experienced members of the surgical team may be available to assess these patients. These doctors may be responsible for a large number of in-patients with a corresponding routine workload.
The MEWS is intended to improve communication between nursing staff and junior doctors and to ‘flag-up’ patients who need to be given immediate priority. The call-out algorithm is intended to ensure that appropriate immediate management is started and that the need for critical care expertise should be considered at an early stage. The MEWS is an important part of a risk management strategy that is simple to implement. To our knowledge, there is no published sensitivity or specificity data because in previous studies the MEWS has been applied selectively. This information is important in order to convince junior surgical staff that the MEWS will genuinely help them to prioritise patients and to give them confidence to call for advice when they are dealing with these patients.
In this study, the sensitivity of the MEWS used with a threshold score of four was 75% for ITU or HDU admission. The specificity was 83%. As expected, increasing the threshold resulted in increased specificity at the expense of sensitivity. The positive predictive value was 22%. That is, one out of every five patients who triggered the mechanism were in fact transferred from the ward to ITU or HDU. The remaining four out of five patients with deranged physiological observations undoubtedly needed review in order to optimise their management on the ward.
When any patient scores a MEWS of four or more, the surgical team should be informed immediately. The responsible junior doctor should immediately review the patient to optimise fluid balance, examine for atrial fibrillation and to re-evaluate the definitive management plan. Patients managed on the ward scoring four or more should be discussed during the junior doctor's hand-over. The critical care team should be informed about many of these patients because appropriate care for about one in five is provided on ITU or HDU.
Conclusion
An early warning system is an important risk management tool that should be implemented for all surgical in-patients.
References
- 1.Audit Commission. Critical to Success: The Place of Efficient and Effective Critical Care Services Within the Acute Hospital. London: Audit Commission; 1999. [Google Scholar]
- 2.Stenhouse C, Coates S, Tivey M, Allsop P, Parker T. Prospective evaluation of a modified Early Warning Score to aid earlier detection of patients developing critical illness on a general surgical ward [Abstract] Br J Anaesth. 1999;84:663P. [Google Scholar]
- 3.Morgan RJM, Williams F, Wright MM. An early warning scoring system for detecting developing critical illness. Clin Intensive Care. 1997;8:100. [Google Scholar]
- 4.Carberry M. Implementing the modified early warning system: our experiences. Nurs Crit Care. 2002;7:220–6. [PubMed] [Google Scholar]
- 5.Subbe CP, Kruger M, Rutherford P, Gemmel L. Validation of a modified Early Warning Score in medical admissions. Q J Med. 2001;94:507–10. doi: 10.1093/qjmed/94.10.521. [DOI] [PubMed] [Google Scholar]
- 6.American College of Chest Physicians–Society of Critical Care Medicine Consensus Conference. Definitions of sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992;20:864–75. [PubMed] [Google Scholar]
- 7.McQuillan P, Pilkington S, Allan A, Taylor B, Short A, Morgan G, et al. Confidential inquiry into quality of care before admission to intensive care. BMJ. 1998;316:1853–8. doi: 10.1136/bmj.316.7148.1853. [DOI] [PMC free article] [PubMed] [Google Scholar]