Abstract
INTRODUCTION
Time spent waiting to see a doctor in the out-patient department is a significant source of dissatisfaction for patients. Out-patient staff are often repeatedly questioned about the running of the clinic and why a delay has developed. These complaints and requests often result in further delays to the clinic.
PATIENTS AND METHODS
An information sheet was written to answer these questions. We set out to determine if the distribution of these sheets increased patient satisfaction with waiting times in the outpatient setting. Twelve sequential ENT clinics at the Lister Hospital, Stevenage were randomised into two groups. Patients attending clinics in Group A (n = 103) received an information sheet while those attending clinics in Group B (n = 124) received no information sheet. At the end of their clinic visit, all patients completed a questionnaire in which they were asked to provide a rating of their levels of satisfaction with various experiences in the out-patient department on a rating score from 1 to 5.
RESULTS
We found levels of satisfaction regarding waiting times to be significantly higher in the group who received information sheets (P < 0.001). No verbal complaints were received by the nursing staff at clinics where the information sheet was distributed. Four verbal complaints were received at the clinics where no sheets were distributed.
CONCLUSIONS
We believe that the use of information sheets is a cost-effective method of improving patient satisfaction and that this is a useful tool both in the primary care setting and in hospital out-patient departments.
Keywords: Out-patient, Waiting times, Satisfaction, Information sheets
The waiting time to see a doctor is the main source of dissatisfaction expressed by patients attending out-patient departments.1 The authors have observed that the most common verbal complaints relate to the out-patient waiting time. We feel that improving patient satisfaction would be key to reducing the levels of anger directed toward clinic staff which are already reported to be unacceptably high.2,3
Moderate waiting times are tolerated fairly well.1 However, when waiting times are lengthier, many patients will ask members of staff for an explanation. Patient information sheets or pamphlets have been used to good effect in other situations. Accompanying information sheets have been shown to improve patient compliance with a new form of treatment4 and, when used in the context of provision of pre-operative information, are welcomed by patients.5 There is strong evidence that written information sheets provided to patients prior to an out-patient appointment will reduce the level of non-attendance.6
In the interactions between patients and staff in the ENT out-patient department at the Lister Hospital, Stevenage, a few recurring questions arose about the running of the clinic and why the delay has been allowed to develop. We created a patient information sheet to answer these recurring questions and set out to see if the distribution of these sheets increased patient satisfaction in the outpatient setting.
Patients and Methods
An information sheet (Appendix 1) was devised after discussion with the out-patient nursing and clerical staff, where common questions and complaints were identified. Almost all of the common complaints were regarding the length of wait and the general running of the clinic.
The information sheet contained information and explanations under the headings of:
Why have I not been seen on time?
Why has someone who arrived after me seen first?
Why do some members of staff appear not to be seeing patients?
Why was my previous appointment cancelled?
Why have I not seen the consultant?
Twelve consecutive clinics at the Lister Hospital ENT department clinics were randomised to Group A or Group B, using a computer-generated random numbers with blinded randomisation allocation. Patients attending clinics in Group A (six clinics) received no information sheet, while all patients attending clinics in Group B (six clinics) received an information sheet.
For all clinics, the clerical and nursing staff recorded each verbal complaint expressed by the patients.
At the end of their visit to the clinic, all patients were asked to complete a questionnaire (appendix 2). Patients were asked to indicate age, sex, length of wait, whether a hearing test was performed before the consultation and whether this was a first appointment or a follow-up. They were then asked to indicate their levels of satisfaction with various aspects of their experiences in the clinic by a ranked scale from 1 to 5. A small pilot study was undertaken to calculate power and to assess the suitability of the information sheet and questionnaire. It was found that a visual analogue scale was difficult for may patients to interpret when unassisted. A 5-point scoring system was favoured for simplicity. The aspects about which patients were questioned included their satisfaction with: facilities and comfort at the clinic, treatment by clerical, nursing and medical staff, follow-up arrangements and waiting time.
The levels of expressed satisfaction between patients in Groups A and B were then compared using the Mann-Whitney U-test.
Results
Of the 249 patients who attended clinic, 232 (93%) questionnaires were received from the 12 clinics; 227 were correctly filled in (98%) and the remainder were discarded. Of the questionnaires that were not received or were discarded, 10 were from the group that received the information sheet and 12 from the group that did not. The number of patients in Group A and Group B comprised 103 and 124 patients, respectively. Average waiting time was 32.7 min with SD of 23.95 min.
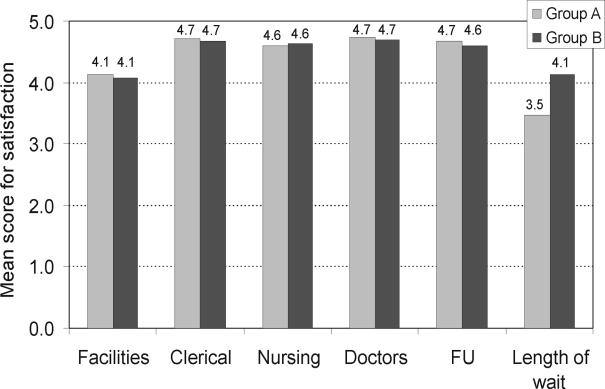
Differences in mean scores for expressed satisfaction between Group A and Group B are shown in Figure 1. We found a significantly higher level of satisfaction in Group B with respect to the length of wait (P < 0.001). As expected, there were no significant differences were found between groups for any of the other expressed satisfaction levels as no information was given about these variables.
Figure 1.
Mean scores for satisfaction for each category in questionnaire.
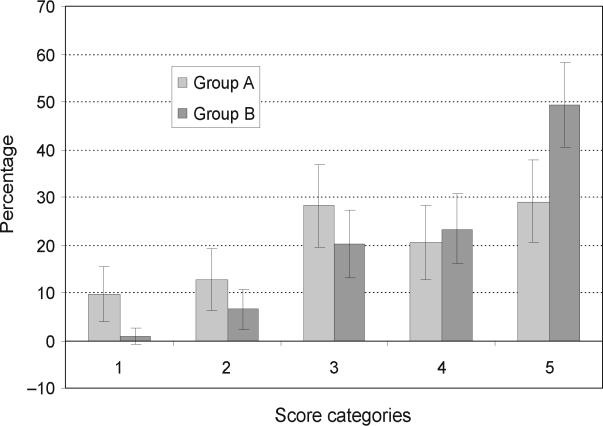
In addition, the number of maximum scores for satisfaction was significantly higher in group B (49.2%) than Group A (29.1%) (P < 0.05) as well as the number of minimum scores being significantly lower in Group B (0.8%) than in Group A (9.7%; P < 0.05; Fig. 2). The nursing staff received no complaints from patients at the clinics where the information sheets were distributed, but four from clinics where there were no sheets given. Of the four complaints, three were described as angry, one as abusive. All of the complaints were regarding waiting times.
Figure 2.
Percentage of responses in each numerical category (with 95% confidence intervals).
Discussion
The out-patient waiting time has been identified in this study to represent the most important concern expressed by patients attending ENT out-patient clinics at the Lister Hospital.
The use of information sheets is not only a cost-effective method to improve patient satisfaction but also reduces the number of complaints generated by patients waiting to be seen by a doctor.
This pilot study should be followed by larger and wider studies on out-patient attenders for other specialties. We feel that these results have useful implications both in the primary care setting, where patients wait to see their general practitioner, and in the hospital setting where patients wait to see medical staff in out-patient departments.
Conclusion
The use of patient information sheets is a cost-effective method of improving patient satisfaction in the out-patient department.
Appendix 1
Department of Ear, Nose and Throat Surgery–East and North Hertfordshire NHS Trust
OUTPATIENT DEPARTMENT PATIENT INFORMATION SHEET
Welcome to the ENT Outpatient Department. This handout has been produced to help explain the running of the clinic and to answer some questions frequently asked of the nursing and clerical staff.
Although the ENT Department is based at the Lister Hospital, the doctors and nurses are involved in running clinics at the Queen Elizabeth II and Hertford County Hospitals. The same staff are also responsible for ENT emergencies through an on-call system as well as being responsible for the patients on the ENT ward.
FREQUENTLY ASKED QUESTIONS
Why have I not been seen on time?
Although it is our goal to see everybody at the time of their appointment, there are many reasons why the clinic may run late:
The clinic can be overbooked because there may be urgent cases who need to be seen urgently. More patients may be followed up than anticipated when seen at previous clinics.
All patients are booked for a set amount of time as it is difficult to predict the amount of time required to assess and treat a patient. If there are a lot of complex cases, the clinic will take longer than anticipated.
Sometimes an emergency requiring immediate attention will sometimes occur on the ward or in the accident and emergency department. In these circumstances, a doctor will have to leave the clinic to attend the patient and this will significantly prolong waiting times.
Certain patients, particularly new patients, can only be seen by a senior member of the Department. If there are many such patients in a particular clinic, waiting times for that doctor will be prolonged.
There is a limited amount of specialist equipment available for use in the clinic and it is sometimes necessary to wait for treatment rooms to become available, or for a specific item of equipment to be prepared.
Doctors may arrive late owing to other urgent commitments such as theatre.
Why has a person who arrived after me been seen first?
The time of appointment is used, rather than the time of arrival, to allocate the order in which patients are seen. A patient arriving on time for a 14h00 appointment will be seen before a patient arriving at 13h45 for a 14h15 appointment. No special treatment is given, unless the clinical situation of the patient warrants it.
Some patients need to be seen by a senior member of the team and thus cannot be seen by a junior doctor even if he is ahead of schedule and seeing other patients who have only just arrived.
If a patient has had tests or investigations, these will need to be collected and processed before the doctor sees the patient. This may delay the patient being seen.
Patients who do not require tests or treatment at the time of the appointment may be seen before those who do, if there is a delay with equipment or treatment rooms.
Why do some staff members appear not to be seeing patients?
Some staff may have seen all the patients that they are allowed to see without direct supervision and are waiting for the consultant to review more patients that can be seen by junior staff.
The doctors or nurses may be waiting for results to be retrieved or for treatment facilities to become available.
Why was my previous appointment cancelled?
Sometimes it is difficult to predict the number of patients who will need to be seen urgently, if the addition of these extra patients exceeds the quota of the clinic, less serious cases need to be cancelled.
If doctors go sick, there is seldom time to organise cover for them and this will result in a smaller number of patients being seen.
Why am I not seeing the consultant?
The consultant assesses the notes of ALL patients attending the clinic before and during the clinic session and assigns patients to various members of the ENT team according to their skills and levels of experience.
Not all patients can be seen by the consultant, as there is normally only one consultant per clinic session.
The consultant is always available to give advice and assistance with any patient at the clinic seen by one of his team.
Appendix 2
Department of Ear, Nose and Throat Surgery–East and North Hertfordshire NHS Trust
OUTPATIENT DEPARTMENT PATIENT SATISFACTION QUESTIONNAIRE
General information
| Age | --------------- | |
| Gender | M/F | |
| First appointment----------- | Follow-up appointment--------------- | |
| Time of appointment | --------------- | |
| Time seen by doctor | --------------- | |
| Length of wait | --------------- | |
| Was a hearing test performed? | Y/N |
Satisfaction
Please rate your level of satisfaction with the following (please circle one):
| Comfort and facilities at the clinic | ||||||
| Not at all satisfied | 1 | 2 | 3 | 4 | 5 | Very satisfied |
| How you were treated by the clerical staff | ||||||
| Not at all satisfied | 1 | 2 | 3 | 4 | 5 | Very satisfied |
| How you were treated by the nursing staff | ||||||
| Not at all satisfied | 1 | 2 | 3 | 4 | 5 | Very satisfied |
| How you were treated by the doctors | ||||||
| Not at all satisfied | 1 | 2 | 3 | 4 | 5 | Very satisfied |
| Length of wait to be seen | ||||||
| Not at all satisfied | 1 | 2 | 3 | 4 | 5 | Very satisfied |
| Follow-up arrangements | ||||||
| Not at all satisfied | 1 | 2 | 3 | 4 | 5 | Very satisfied |
References
- 1.McKinnon K, Crofts PD, Edwards R, Campion PD, Edwards RH. The outpatient experience: results of a patient feedback survey. Int J Health Care. 1998;11:156–60. doi: 10.1108/09526869810230858. [DOI] [PubMed] [Google Scholar]
- 2.Wells J, Bowers L. How prevalent is violence towards nurses working in general hospitals in the UK? J Adv Nurs. 2002;39:230–40. doi: 10.1046/j.1365-2648.2002.02269.x. [DOI] [PubMed] [Google Scholar]
- 3.Brennan W. We don't have to take this: dealing with violence at work. Nurs Stand. 2000;14(28 Suppl):3–17. [PubMed] [Google Scholar]
- 4.Katz LG. The use of printed instruction sheets to enhance patient compliance. Semin Dermatol. 1991;10:91–5. [PubMed] [Google Scholar]
- 5.Wijtenburg E, Navez B, Cambier E, Guiot P. Patient's opinion about written information before laparoscopy: a consecutive series of 100 cases. Acta Chir Belg. 2002;102:17–9. doi: 10.1080/00015458.2002.11679256. [DOI] [PubMed] [Google Scholar]
- 6.Hardy KJ, O'Brien SV, Furlong NJ. Information given to patients before appointments and its effect on non-attendance rate. BMJ. 2001;323:1298–300. doi: 10.1136/bmj.323.7324.1298. [DOI] [PMC free article] [PubMed] [Google Scholar]