Abstract
INTRODUCTION
Transrectal ultrasound guided prostate needle biopsy (TRUS) is the standard procedure to diagnose or exclude prostate cancer. This procedure can be associated with significant discomfort, both on insertion of the ultrasound probe as well as on taking the biopsy. We evaluated a new technique for pain relief during TRUS biopsy.
PATIENTS AND METHODS
In Group 1 (n = 60), the biopsies were taken without any analgesia. In Group 2 (n = 60), 11 ml of Instillagel (2% lignocaine) was administered rectally prior to probe insertion and 5 ml of 1% lignocaine periprostatic injection was administered before taking the biopsy. The discomfort encountered during the procedure was graded by the patient on a scale ranging from no discomfort to mild, moderate and severe pain.
RESULTS
In Group 2, there was a marked reduction in the pain experienced during the procedure. The Chi-squared test for trend showed a significant association between the rectal administration of local anaesthetic gel and reduction in pain on probe insertion (P = 0.0001). There was also a significant association between the use of periprostatic lignocaine injection and reduction in pain on taking the biopsy (P < 0.0001).
CONCLUSIONS
The use of lignocaine gel prior to probe insertion and periprostatic infiltration of lignocaine before taking the needle biopsy significantly reduces the pain experienced by the patient during TRUS-guided prostate biopsy.
Keywords: Prostate, Transrectal ultrasound, Biopsy, Periprostatic infiltration
Prostate cancer is the most frequent urological malignancy encountered by urologists. It is the most common cancer affecting men.1,2 TRUS-guided prostate needle biopsy using an 18-G Tru-cut needle loaded on a biopsy gun is the standard procedure to diagnose or rule out prostate cancer;3,13 6–16 cores may be obtained.4,5
In addition to the finite morbidity of the procedure such as haematuria, haemospermia, bleeding per rectum and infection, the procedure can be quite uncomfortable and discouraging to the patient, especially if repeated biopsies are needed.6
Studies have been done in the past to determine an effective method for pain relief for TRUS-guided needle biopsies. Walker et al.12 found that pericapsular injection with 1% lignocaine significantly reduces the pain of TRUS biopsy. A similar conclusion was drawn by Bulbul et al.6 Saad et al.13 stated that the rectal administration of lignocaine gel reduces the pain experienced during the biopsy. Desgrandchamps et al.11 disagree and state that the rectal administration of lignocaine gel has no benefit over placebo.
Nowadays, periprostatic lignocaine injection is used in many centres to provide analgesia during TRUS biopsies. Aqueous gel is used for probe insertion. In our centre, we realised that apart from experiencing pain on taking the prostate biopsy, patients also experience pain on insertion of the ultrasound probe. Keeping this in mind, we initiated the rectal use of lignocaine gel prior to probe insertion. We used this in combination with periprostatic lignocaine injection administered before the needle biopsy. We have conducted this study to determine the efficacy of the protocol and its effect on pain relief during the procedure. The results were compared with a group of patients who had a similar procedure without any form of anaesthesia.
Patients and Methods
This was a non-randomised study, consisting of a retrospective element (Group 1) and a prospective element (Group 2). Patients with an elevated prostate specific antigen (PSA) above 4 ng/ml or suspicious digital rectal examination (DRE) had TRUS-guided prostate needle biopsies. The mean age of Groups 1 and 2 was 66.5 years (range, 52–88 years) and 68 years (range, 52–86 years), respectively.
In Group 1 (n = 60), the TRUS-guided prostate needle biopsy was carried out without any form of anaesthesia. Aqueous gel was used for probe insertion and no anaesthesia was administered for the biopsy. Biopsies were performed with an 18-G Tru-cut needle loaded on a biopsy gun. Antibiotic prophylaxis was given to the patients (gentamicin, 120 mg i.v. pre-operatively followed by a rectal suppository of metronidazole 500 mg post biopsy and a 3-day course of oral ciprofloxacin 500 mg b.d.). Six random core biopsies were obtained, 3 from each lobe of the prostate gland.
The patients in Group 1, the retrospective component of the study, were sent postal questionnaires a few weeks after the procedure to evaluate the pain experienced during the procedure. The discomfort encountered was graded by the patient on a scale ranging from no discomfort to mild, moderate and severe pain. This grading was done separately for probe insertion and prostate biopsy.
Group 2 (n = 60), the prospective component of the study, had biopsies taken with the new protocol. Instillagel (11 ml, 2% lignocaine) was administered rectally prior to probe insertion. The time interval between the rectal administration of lignocaine gel and probe insertion was 1 min. This was followed by 5 ml of 1% lignocaine periprostatic infiltration around the neurovascular bundle of the prostate gland. This was carried out with a 22-G spinal needle guided by transrectal ultrasonography. Biopsies were performed with an 18-G Tru-cut needle loaded on a biopsy gun. Antibiotic prophylaxis was given to the patients (gentamicin 120 mg i.v. preoperatively followed by a rectal suppository of metronidazole 500 mg post biopsy and a 3-day course of oral ciprofloxacin 500 mg b.d.). A minimum of 6 random core biopsies were obtained. Immediately after the procedure, patients filled in a questionnaire and graded the discomfort encountered during the procedure on a scale ranging from no discomfort to mild, moderate and severe pain. This grading was done separately for probe insertion and prostate biopsy.
Figure 1.
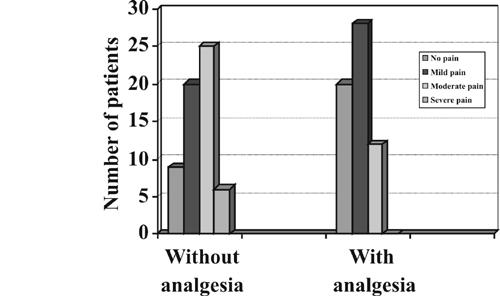
Comparison of pain score in the non-analgesic and analgesic group on probe insertion.
Figure 2.
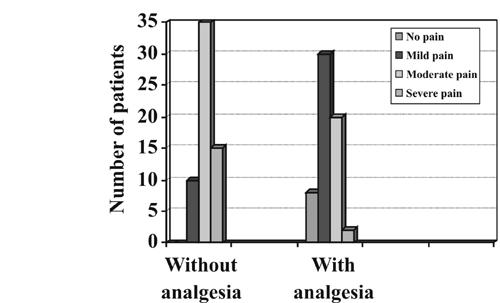
Comparison of pain score in non-analgesic and analgesic group on TRUS biopsy.
Figure 3.
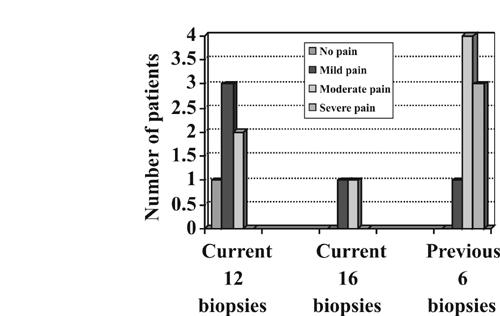
Comparison between current and previous biopsy pain score in the same patients.
Results
Patients in Group 1 had a mean age of 66.5 years (range, 52–88 years) whereas those in Group 2 had a mean age of 68 years (range, 52–86 years). All patients had PSA levels above 4 ng/ml. Each patient in Group 1 had six random core biopsies taken, three from the right and three from the left lobe of the prostate gland. In Group 2, the number of biopsies taken varied, from a minimum of six to a maximum of 16 biopsies. Seven patients in Group 2 had 16 biopsies taken and in 23 patients 12 biopsies were possible. Three and 27 patients had 9 and 6 biopsies taken, respectively.
No pain was experienced on probe insertion by 33% of the patients in the analgesic group (Group 2) as compared to 15% in the non-analgesic group (Group 1). Mild pain and moderate pain was experienced by 47% and 20% of the patients, respectively, in Group 2; in Group 1, 33% experienced mild pain and a much higher percentage of 42% experienced moderate pain. No patient recorded severe pain on probe insertion in Group 2 as compared to 10% in Group 1.
With regards to the pain experienced on taking the biopsy, in the analgesic group (Group 2), 13% of the patients experienced no pain at all. None of the patients in the non-analgesic group (Group 1) reported the procedure to be pain-free. In Group 2, 50% and 33% of the patients experienced mild and moderate pain, respectively, as compared to Group 1 in which 17% experienced mild pain and 58% experienced moderate pain. Only 3% of the patients recorded severe pain in Group 2 as compared to 25% patients in Group 1.
The results indicate a reduction in the pain experienced both on probe insertion as well as on taking the biopsy with a combination of rectal administration of lignocaine gel and lignocaine periprostatic injection. The Chi-squared test for trend showed a highly significant association between the use of local anaesthetic gel and a reduction in pain on probe insertion (P = 0.0001). A similar association was seen on taking of the biopsy (P < 0.0001).
Further interpretation of the results indicated that 8 patients had repeat biopsies taken. These 8 patients previously had 6 cores taken without analgesia; 1, 4 and 3 of the patients recorded mild, moderate, and severe pain, respectively, on biopsy at the time. On repeat biopsy with the combination analgesia, 16 cores were achieved in 2 of the patients, 1 patient recorded mild and the other experienced moderate pain. In the remaining 6 patients, 12 cores were achieved, 1 patient experienced no pain, 3 recorded mild pain and 2 stated moderate pain.
Discussion
The adoption of serum PSA as a tumour marker for prostate cancer has increased over the past few years.7 PSA being a tumour-associated antigen with a positive predictive value of 30–40% forces us to address elevated levels via prostate biopsy.8,9 This, in turn, translates to an increase in the number of prostate biopsies performed to confirm or exclude prostate cancer.10
TRUS-guided prostate biopsies are associated with finite complications including pain or discomfort, haematuria, haemospermia, blood per rectum and infection.6 Bleeding has been managed by stopping anticoagulants prior to the biopsy and avoiding the urethra while taking the cores. Infection is prevented by pre- and post-biopsy antibiotic prophylaxis. The most commonly reported side-effect (60–70%) of the procedure is discomfort and pain.6 The discomfort during transrectal biopsy appears to be proportional to the number of biopsies taken.11 This is of particular concern as it discourages patients with progressively rising PSA to undergo a repeat biopsy.
The pain fibres of the prostate gland run in the periprostatic area along the neurovascular bundle.12 Prostate biopsies, especially digital-guided biopsies, may be performed without any form of anaesthesia. However, nowadays, periprostatic infiltration of lignocaine in the pain fibres along the neurovascular bundle is an established technique used by many urologists.
In studies conducted in the past, Saad et al.13 and Desgrandchamps et al.11 evaluated the effect of the rectal administration of lignocaine gel on pain relief during prostate biopsy. Saad et al.,13 in their study on 360 patients, found the rectal administration of lidocaine gel to provide better pain relief as compared to placebo (P = 0.0001). Desgrandchamps et al.11 did not agree. In their study on 109 patients, they found no difference in pain control between the group having rectal lidocaine gel and that having placebo (P = 0.39). Walker et al.12 and Bulbul et al.6 in their studies on 121 and 72 patients, respectively, evaluated the effect of periprostatic local anaesthetic injection on pain relief during prostate biopsy. Walker et al.12 concluded that the periprostatic infiltration of 1% lignocaine significantly reduces the pain experienced during TRUS biopsy (P < 0.001). Bulbul et al.6 reached a similar conclusion. They found that the periprostatic infiltration with 2% lidocaine significantly reduces the pain of prostate biopsy.
In our study of 120 patients, we found a significant reduction in pain, both on probe insertion and on biopsy in the group which received the combination of rectal administration of 2% lignocaine gel and 1% lignocaine periprostatic injection, thus making the procedure more tolerable.
This study has certain limitations. It had retrospective as well as prospective components. Furthermore, this was a non-randomised study. Lastly, the questionnaires for Group 1 were filled in by the patients a few weeks after the procedure whereas the patients in Group 2 completed the questionnaire immediately after the procedure. Until there is a more effective way to check the prostate for cancer, TRUS-guided needle biopsy will continue to be the gold standard. Though refinements in the procedure have been introduced over the years, discomfort continues to be the most common side effect and any new technique that can alleviate this discomfort is welcome.
Conclusions
The combination of rectal administration of 2% lignocaine gel prior to probe insertion and 1% periprostatic lignocaine injection prior to the biopsy is quick, safe, cost-effective and provides good analgesia. However, this study is an initial assessment; therefore, a randomised, prospective and double-blinded study is advocated to confirm these findings.
Acknowledgments
We thank Dr DP Mikhailidis Reader and Consultant, Department of Chemical Pathology, Royal Free Hospital and Medical School, for his valuable advice. We would also like to thank Dr Richard Morris, Senior Lecturer in Medical Statistics, Royal Free and University College Medical School, for statistical advice.
References
- 1.Wingo PA, Tong T, Bolden S. Cancer statistics 1995. CA Cancer J Clin. 1995;45:8–30. doi: 10.3322/canjclin.45.1.8. [DOI] [PubMed] [Google Scholar]
- 2.Landis SH, Murray T, Bolden S, Wingo P. Cancer statistics 1998. CA Cancer J Clin. 1998;48:6–29. doi: 10.3322/canjclin.48.1.6. [DOI] [PubMed] [Google Scholar]
- 3.Stamey TA. Making the best out of six systemic sextant biopsies. Urology. 1995;45:2–12. doi: 10.1016/s0090-4295(95)96168-2. [DOI] [PubMed] [Google Scholar]
- 4.Eskew LA, Bare RL, McCullough DL. Systematic 5 region prostate biopsy is superior to sextant method for diagnosing carcinoma of the prostate. J Urol. 1997;157:199–202. [PubMed] [Google Scholar]
- 5.Ravery V, Goldblatt L, Royer B, Blanc E, Toublanc M, Bocco-Gibod L. Extensive biopsy protocol improves the detection rate of prostate cancer. J Urol. 2000;164:393–6. [PubMed] [Google Scholar]
- 6.Bulbul MA, Haddad MC, Khauli RB, Hemady K, Shaar A, Khouzami R, et al. Periprostatic infiltration with local anesthesia during transrectal ultrasound-guided prostate biopsy is safe, simple, and effective: a pilot study. Clin Imaging. 2002;26:129–32. doi: 10.1016/s0899-7071(01)00365-5. [DOI] [PubMed] [Google Scholar]
- 7.Robert RO, Bergstralh EJ, Lieber MM, Jacobsen SJ. Digital rectal examination and prostate-specific antigen abnormalities at the time of prostate biopsy and biopsy outcomes, 1980 to 1997. Urology. 2000;56:817–22. doi: 10.1016/s0090-4295(00)00790-1. [DOI] [PubMed] [Google Scholar]
- 8.Ornstein DK. The effect of prostate volume, age, total prostate specific antigen level and acute inflammation on the percentage of free serum prostate specific antigen levels in men without clinically detectable prostate cancer. J Urol. 1998;159:1234–7. [PubMed] [Google Scholar]
- 9.Schatterman PH. Inflammation in prostate biopsies of men without prostate malignancy or clinical prostatitis: correlation with total serum PSA and PSA density. Eur Urol. 2000;37:404–12. doi: 10.1159/000020161. [DOI] [PubMed] [Google Scholar]
- 10.Partin AW, Stutzman RE. Elevated prostate-specific antigen, abnormal prostate evaluation on digital rectal examination and transrectal ultrasound and prostate biopsy. Urol Clin North Am. 1998;25:581–9. doi: 10.1016/s0094-0143(05)70049-5. [DOI] [PubMed] [Google Scholar]
- 11.Desgrandchamps F, Meria P, Irani J, Desgrippes A, Teillac P, Le Duc A. The rectal administration of lidocaine gel and tolerance of transrectal ultrasonography-guided biopsy of the prostate: a prospective randomized placebo-controlled study. BJU Int. 1999;83:1007–9. doi: 10.1046/j.1464-410x.1999.00080.x. [DOI] [PubMed] [Google Scholar]
- 12.Walker AE, Schelvan C, Rockall AG, Rickards D, Kellett MJ. Does pericapsular lignocaine reduce pain during transrectal ultrasonography-guided biopsy of the prostate? BJU Int. 2002;90:883–6. doi: 10.1046/j.1464-410x.2002.03025.x. [DOI] [PubMed] [Google Scholar]
- 13.Saad F, Sabbagh R, McCormack M, Peloquin F. A prospective randomized trial comparing lidocaine and lubricating gel on pain level in patients undergoing transrectal ultrasound prostate biopsy. Can J Urol. 2002;9:1592–4. [PubMed] [Google Scholar]


