Abstract
INTRODUCTION
A retrospective study was undertaken of a consecutive cohort of 86 patients (101 hips) under the age of 60 years operated on by a single orthopaedic team between 1993 and 2003 at a district general hospital.
PATIENTS AND METHODS
Demographic and diagnostic data were collected from patients’ hospital records, and a detailed questionnaire regarding occupational status was used at follow-up.
RESULTS
Nearly all of the patients working prior to surgery returned to employment following surgery. Nearly half of those not working pre-operatively regained employment postoperatively; among those that did not return to work, this was for reasons unrelated to their hip. Those patients who had been out of work prior to their surgery took significantly longer to return to work.
CONCLUSIONS
Our study demonstrates that total hip replacement is effective in keeping patients under the age of 60 years employed. It is also effective in allowing those already off work due to hip pain to return to work, although there is a much greater delay.
Keywords: Total hip replacement, Young patients, Work, Employment
Introduction
Total hip replacement (THR) is a common elective orthopaedic procedure, with over 30,000 performed by the NHS in England each year. It has been shown to be an effective procedure at reducing patients’ pain and increasing their mobility.1,2
Whilst the majority of hip replacements are carried out in patients over the age of 65 years and, therefore, retired, about 15% are undertaken in patients of working age.3 Few studies have been conducted to examine the impact of THR on the work status of this specific group, and none of these have been carried out in the UK. Those studies that have addressed this issue have reported that between 25% and 92% of patients undergoing THR return to work postoperatively.4–7
The objective of this study was to look specifically at the effect of THR on the work status of patients under 60 years in the UK, who were operated on consecutively by the same surgical team between 1993 and 2003. The economic implications of the data on the provision of THR to young patients are also discussed.
Patients and Methods
Between 1993 and 2003, 101 primary THRs were performed in 86 patients under the age of 60 years by one surgical team. All pre-operative data were collected from fully documented patient records, including patients’ age and sex, diagnosis and time spent awaiting surgery. The patients were followed up for between 6 months and 10 years postoperatively (mean, 3 years). A questionnaire was administered either via telephone or in person when the patient visited clinic. This contained items related to profession, employment status pre- and postoperatively, length of time taken to resume work, changes in working patterns and, where relevant, reasons for not returning to work.
Five patients were not followed up (2 had died, 1 had emigrated and a further 2 were lost to follow-up). Fifteen patients had both hips replaced (8 men and 7 women). In these cases, the time off work prior to the first hip replacement was considered to represent ‘time off work prior to surgery’. Similarly, time off work after the second hip replacement was considered to represent ‘time taken to return to work’.
Of the 86 patients, 59 had a primary diagnosis of osteoarthritis, 15 had development dysplasia of the hip, 8 had post-traumatic osteoarthritis, 2 had osteonecrosis, 1 had rheumatoid arthritis and 1 had suffered previously with septic arthritis.
There were 56 men and 30 women. The mean age was 51.4 years (range, 29–60 years). There was no difference in the mean age of men and women. The age distribution of the cohort is shown in Figure 1.
Figure 1.
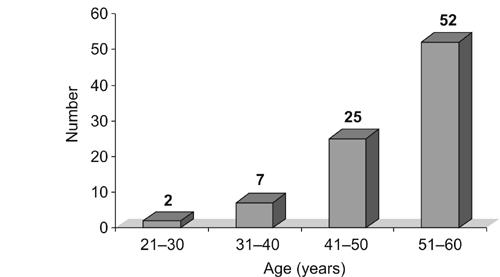
The age distribution of the patients.
Results
There were only two complications – a postoperative deep vein thrombosis which was diagnosed and treated, and one superficial wound infection which was treated successfully with antibiotics.
Fifty-one patients had been in employment prior to surgery and 30 were not. Of the 51 that were in employment pre-operatively, 49 remained in employment postoperatively. Of the 30 that were not in employment pre-operatively, 13 returned to some form of employment after surgery. Seventeen remained unemployed (Fig. 2).
Figure 2.
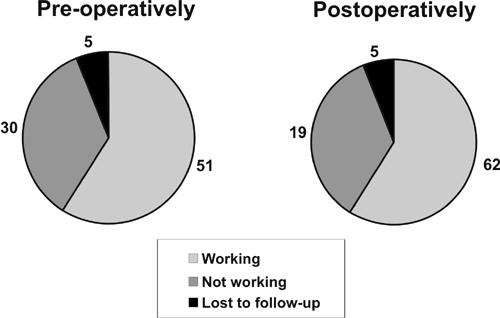
The work status of the patients pre-operatively and postoperatively.
Only 12 of the 30 patients not working pre-operatively claimed that hip pain prevented them from working; 11 of these 12 patients returned to work postoperatively.
From a total of 81 patients followed up, 19 were not in employment postoperatively. Of these, 5 had retired as planned, 4 were housewives, and 10 did not work for reasons unrelated to their hip disease.
Patients working pre-operatively took an average of 10.5 weeks to return to work. Patients not working pre-operatively took an average of 35 weeks to gain employment. Those out of work because of hip pain were unemployed for an average 26 weeks and took an average 28 weeks to regain employment. Being self-employed rather than a salaried employee did not affect the time to return to work postoperatively (Fig. 3). Women took longer to get back to work (25 weeks compared to 12 weeks for men).
Figure 3.
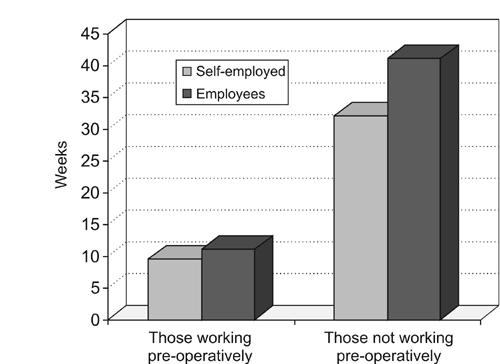
Time taken to return to work after THR.
Generally, the nature of work that patients returned to did not change; while 13 of the 62 patients who returned to work postoperatively changed occupation, only 6 of these adopted jobs of reduced physical intensity.
Finally, if patients were unemployed for over 1 year pre-operatively (11 patients), they were unlikely to regain employment postoperatively (8 patients).
Discussion
The positive effect of total hip replacement on health-related quality of life is well documented, and a number of outcome measures have been used to illustrate this point. These include the Harris hip score, the Merle d'Aubigne hip score and the Western Ontario and McMaster University (WOMAC) Osteoarthritis Index. Improvements in such outcome measures, reflecting levels of pain, mobility and psychological well-being, do not necessarily correlate with levels of return to work.8 Only a few studies have been undertaken looking specifically at the effect of THR on the ability of patients of working age to continue or resume active employment.4–7 This is important because the cost of sick leave in patients awaiting total hip replacement is substantial.9
In our study, all but one of those who were working pre-operatively remained in work. Furthermore, all 19 patients not working after THR listed reasons other than hip pain, usually quoting other health-related reasons. THR is, therefore, clearly a powerful tool in maintaining patients’ employment status.
Because of the wide variation in follow-up intervals, we cannot conclude from these data how long patients are likely to continue working. Cost–benefit calculations made in the past have used estimates which assume that the ‘typical person having a total hip replacement in his middle or late fifties would be able to work for five more years than otherwise’.10 However, Nevitt et al.,7 in a study which obtained comprehensive 1- and 4-year follow-up data in a North American context, concluded that ‘benefits accruing from reductions in work disability among younger recipients may not be as great as previously assumed’. Accurate cost–benefit estimations in the UK would, therefore, require data from longitudinal studies implemented over a longer period.
The most striking aspect of our results is the difference in time to return to work that existed between those that had taken sick-leave or been made redundant prior to their THR, and those that were able to continue working right up until their surgery. Johnsson and Persson5 went as far as to discover a positive association between the duration of pre-operative and postoperative sick leaves and demonstrated that a reduction of sick leave to 6 months or less meant a productive gain to society. Our results parallel this study and the study of Jensen et al.6 on occupational capacity after hip replacement. In their study, of 99 patients under 60 years, the majority of those working pre-operatively continued to work after hip replacement and two-thirds of sick-listed patients returned to work. However, we found that if patients were out of employment pre-operatively for over 1 year for whatever reason, they were much less likely to regain employment.
Eleven of the 13 patients in our study who regained employment after THR had been off work prior to surgery purely because of symptoms from their arthritic hip. No clear correlation could be demonstrated in these individual patients between amounts of time off work pre- and postoperatively, although it is possible that other factors such as ability to find work came into play. However, it would be reasonable to suppose that if this group of patients who are out of work or are struggling to stay at work because of hip pain have a minimum period of pre-operative sick leave, the chances of regaining postoperative employment would be maximised.
References
- 1.Visuri T, Honkanen R. The influence of total hip replacement on selected activities of daily living and on the use of domestic aid. Scand J Rehabil Med. 1978;10:221–5. [PubMed] [Google Scholar]
- 2.Keener JD, Callaghan JJ, Goetz DD, Pederson D, Sullivan P, Johnston RC. Long-term function after Charnley total hip arthroplasty. Clin Orthop. 2003;417:148–56. doi: 10.1097/01.blo.0000096807.78689.19. [DOI] [PubMed] [Google Scholar]
- 3.Tennent TD, Goddard NJ. Current attitudes to total hip replacement in the younger patient: results of a national survey. Ann R Coll Surg Engl. 2000;82:33–8. [PMC free article] [PubMed] [Google Scholar]
- 4.Suarez J, Arguelles J, Costales M, Arechega C, Cabeza F, Vijande M. Factors influencing the return to work of patients after hip replacement and rehabilitation. Arch Phys Med Rehabil. 1996;77:269–72. doi: 10.1016/s0003-9993(96)90110-0. [DOI] [PubMed] [Google Scholar]
- 5.Johnsson R, Persson BM. Occupation after hip replacement for arthrosis. Acta Orthop Scand. 1986;57:197–200. doi: 10.3109/17453678608994374. [DOI] [PubMed] [Google Scholar]
- 6.Jensen JS, Mathiesen B, Tvede N. Occupational capacity after hip replacement. Acta Orthop Scand. 1985;56:135–7. doi: 10.3109/17453678508994338. [DOI] [PubMed] [Google Scholar]
- 7.Nevitt MC, Epstein WV, Masem M, Murray WR. Work disability before and after total hip arthroplasty. Assessment of effectiveness in reducing disability. Arthritis Rheum. 1984;27:410–21. doi: 10.1002/art.1780270408. [DOI] [PubMed] [Google Scholar]
- 8.Laupacis A, Bourne R, Rorabeck C, Feeny D, Wong C, Tugwell P, et al. The effect of elective total hip replacement on health-related quality of life. J Bone Joint Surg (Am) 1993;75:1619–26. doi: 10.2106/00004623-199311000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Hertzman P, Johnsson R, Lindgren B. Cost of sick leave for total hip replacement. Acta Orthop Scand. 1988;59:266–9. doi: 10.3109/17453678809149359. [DOI] [PubMed] [Google Scholar]
- 10.Kelsey J. Total hip replacement: epidemiology and impact, NIH consensus development conference. Total hip joint replacement program abstracts, National Institutes of Health. 1982:23–30. [Google Scholar]


