Abstract
Symptomatic gallstones in patients with situs inversus pose diagnostic and therapeutic challenges. The presentation and management of one such patient is discussed with an emphasis on operative technique.
Keywords: Situs inversus, Laparoscopic cholecystectomy
Situs inversus is a morphological anomaly of positioning of internal viscera wherein there is a reversal of the usual ‘handedness’ of visceral topography. The reversal may be thoracic, abdominal or both. It is estimated to occur in 1 in 5000–20,000 births.1,2 Though situs inversus on its own is not pathological, it may be associated with cardiorespiratory, hepatopancreaticobiliary, gastrointestinal, neurological, orthopaedic and urological anomalies, some of which may be life-threatening.1,3 In the published literature, there have been only about 40 reports of open cholecystectomy in the pre-laparoscopic era and 20 reports of laparoscopic cholecystectomy in patients with situs inversus.2,4,5 The variation from the norm of the sidedness of the gall bladder is attended by differences in presentation, difficulties in diagnosis and the need for modifications in operative technique as reported below.
Case report
A 57-year-old woman presented to the surgical clinic with a few months' history of intermittent left upper quadrant pain, radiating to the left scapular region and aggravated by fatty food. Imaging by an ultrasound scan and subsequently by a magnetic resonance cholangiopancreatogram showed abdominal situs inversus with gall stones in a left-sided gall bladder (Fig. 1). The liver was oriented in a mirror image of its usual anatomical lie, with the larger anatomical lobe lying on the left side while the smaller lobe crossed the midline to the right.
Figure 1.
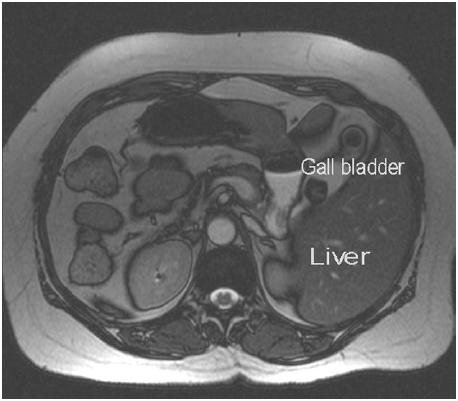
Magnetic resonance imaging showing a left-sided gallbladder with two stones.
Apart from well-controlled, type II diabetes mellitus and obesity, she had no co-morbidities or anomalies. A pre-operative chest X-ray showed dextrocardia consistent with situs inversus but there was no evidence of bronchiectasis.
The approach in the operating room required modification. The surgeon and the assistant were positioned on the right side of the patient and the scrub nurse on the left. A head-end-up and left-side-up positioning of the patient was adopted to optimise views of the gall bladder and the Calot's triangle. A 4-port technique was used – an umbilical (10 mm), a medial epigastric (10 mm) and two lateral subcostal (5 mm) ports (Fig. 2).
Figure 2.

Postoperative photograph of the patient's abdomen with dressings marking the port sites.
Initial inspection confirmed a left-sided liver and gall bladder. There was a total situs inversus with the spleen on the right side, the greater curve of the stomach to the right and the caecum to the left.
The epigastric port (10 mm) was placed just to the left of midline in the subxiphoid position with the tip on the peritoneal aspect to the left of the falciform ligament. This port was one of the two main operating ports and the instruments used were controlled by the left hand of the surgeon. It was used for retraction of the Hartmann's pouch of the gall bladder initially and later for passing the clip applicator.
The medial of the two lateral subcostal ports (5 mm) was placed about 5 cm subcostally just lateral to the left nipple line. This was the second of the two main operating ports and was used for passing the dissector, scissors, hook diathermy and the suction-irrigation apparatus as necessary. This port and its instruments were controlled by the right hand of the surgeon. The lateral subcostal port (5 mm) was placed about 5 cm subcostally close to the anterior axillary line and was used by the assistant to retract the fundus of the gall bladder cranially.
Dissection of the Calot's triangle, identification of the cystic duct–common hepatic duct junction, skeletonisation of the cystic duct and cystic artery before clipping and dissection of gallbladder proceeded as usual. There were no anomalies noted. The gall bladder was delivered using a retrieval bag through the umbilical port after switching the camera to the epigastric port.
The patient made an uneventful recovery and was discharged home in 24 h.
Discussion
There are several important aspects of the management of gallstones in patients with situs inversus that are worth highlighting. While there is no evidence to suggest that gall stones are more or less common in people with situs inversus, the presentation with left upper quadrant pain may delay the diagnosis of symptomatic gall stones. It has been reported that about a third of patients with situs inversus and symptomatic gall stones may, however, present with epigastric pain and about 10% of patients may present with right-sided pain.6 Patients with situs inversus who are scheduled for laparoscopic cholecystectomy should be assessed pre-operatively for any potentially serious cardiac or respiratory abnormalities.
As the unusual orientation while operating on a left-sided gall bladder requires mental adaptability and manual dexterity to cope with any evolving difficult or potentially dangerous intra-operative situation, laparoscopic cholecystectomy in patients with situs inversus should be performed by an experienced laparoscopic surgeon. While there is no evidence to suggest that there is an increased risk of bile duct injuries in patients with situs inversus, the orientation and ergonomic challenges may result in an increased operative time.7 Our total operating time was 75 min.
Positioning of the surgical team and port placements described in the literature are often a mirror image of the protocols used for conventional laparoscopic cholecystectomy. However, the ergonomics of a right-handed surgeon standing on the right side of the patient demand that either he crosses hands so as to allow the right hand to operate through the epigastric port4 or use the assistant to retract the Hartmann's pouch from the left side5 or as we have described here, use the epigastric port to retract with the left hand and operate with the right hand through the lateral subcostal port. The surgeon standing at the foot end, in between the legs of the patient while the patient is in a Lloyd-Davis position, is an alternative, as is delegating to a left-handed surgeon!
References
- 1.Varano NR, Merkin RJ. Situs inversus: review of the literature. Report of four cases and analysis of the clinical implications. J Int Coll Surg. 1991;33:131–5. [PubMed] [Google Scholar]
- 2.Takei HT, Maxvell JG, Clancy TV, Tinsley EA. Laparoscopic cholecystectomy in situs inversus totalis. J Laparoendosc Surg. 1992;2:171–6. doi: 10.1089/lps.1992.2.171. [DOI] [PubMed] [Google Scholar]
- 3.Johnson JR. Situs inversus with associated abnormalities. Review of the literature and report of three cases. Arch Surg. 1949;58:149–54. [PubMed] [Google Scholar]
- 4.Oms LM, Badia JM. Laparoscopic cholecystectomy in situs inversus totalis – the importance of being left-handed. Surg Endosc. 2003;17:1859–61. doi: 10.1007/s00464-003-9051-7. [DOI] [PubMed] [Google Scholar]
- 5.McKay D, Blake G. Laparoscopic cholecystectomy in situs inversus totalis: a case report. BMC Surg. 2005;5:5. doi: 10.1186/1471-2482-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rao PG, Katariya RN, Sood S, Rao PLNG. Situs inversus totalis with calculus cholecystitis and mucinous cystadenomas of ovaries. J Postgrad Med. 1977;23:89–90. [PubMed] [Google Scholar]
- 7.Yaghan RJ, Gharaibeh KI, Hammori S. Feasibility of laparoscopic cholecystectomy in situs inversus. J Laparoendosc Adv Surg Tech. 2001;11:233–7. doi: 10.1089/109264201750539763. [DOI] [PubMed] [Google Scholar]


