Abstract
INTRODUCTION
Testicular cancer is a relatively uncommon, treatable condition. A general practitioner would expect to see, on average, one case of testicular cancer in the whole of their career. Benign scrotal conditions are extremely common and the source of many primary care consultations. The main patient expectations of these attendances are accurate diagnosis and adequate re-assurance as often they are the source of much anxiety and perceived embarrassment. The aim of this study was to examine the content and referral practice of primary care referral of testicular pathology and the resultant findings of the specialist practitioner.
PATIENTS AND METHODS
A total of 201 patients referred with scrotal pathology were prospectively analysed at the time of specialist practitioner assessment by means of data recording in a urological surgery unit and regional peripheral community clinics.
RESULTS
In the study group, 53 patients were referred under the 2-week rule. Of these, 9 (17%) were found to have testicular cancer. Five (36%) cancers were referred outside the 2-week rule referrals; 1 cancer was missed and 2 diagnoses delayed. In total, 44% of final clinical diagnoses differed between the referring primary care physician and the specialist practitioner. Of the 71 (35%) patients referred with a suspicion of cancer, 62 (87%) were subsequently found to be of clinically benign pathology. Overall, 80% of patients were referred more urgently than the opinion of the specialist practitioner.
CONCLUSIONS
Scrotal examination in the primary care setting appears to be of variable accuracy. Many patients referred with a high suspicion of cancer are found to have benign pathology. Two-week rule referrals have an acceptable positive predictive value for testicular cancer (17%). Disagreements exist in the referral priority of patients.
Keywords: Testicular cancer, scrotal swellings
Testicular cancer is a relatively rare condition contributing 0.05 cases per 2000 population per year;1 it affects young men and in many cases is imminently treatable.2 Benign scrotal conditions are common and usually can be managed conservatively.
Almost all scrotal pathology is initially assessed and referred, as appropriate, in the primary care setting. Benign conditions predominate; a general practitioner would only expect to see on average one case of testicular cancer every 20 years. Often, patients are embarrassed and seek only re-assurance and confirmation of benign pathology; the sooner this can be attained, the less the patient anxiety that exists.
The Department of Health Cancer Collaborative as a result of the NHS cancer plan3 introduced measures in December 2000 allowing all patients suspected of having testicular cancer to be seen by a specialist practitioner within 2 weeks of referral. The sole criterion to allow referral under the 2-week rule is the detection of a ‘lump within the body of the testis’: no other guidance is supplied.
Patients referred under the 2-week wait rule are expected to be highly sensitive for testicular cancer and the criteria for referral should allow patients at high risk for malignancy to be selected.
We sought to investigate the evaluation and referral of scrotal masses within the primary care setting.
Patients and Methods
Over a 6-month period, all patients referred to Gloucestershire NHS Trusts with scrotal pathology diagnosed on clinical examination in the primary care setting were included. Patients in whom scrotal ultrasonography had been performed prior to referral were excluded, as were patients in whom a practitioner outside the primary care setting had recently undertaken scrotal examination. Due to pressures on the radiological department at the time of this study, patients in our region were not allowed to be referred directly for scrotal ultrasonography by the primary care physician. Only the first examination performed by the specialist practitioner was analysed, the benefit of altering the assessment after ultrasonography was not allowed. Patients who subsequently underwent scrotal ultrasonography at the request of the specialist practitioner had their clinical and radiological findings correlated.
For the purposes of this study, assessment was not considered to be differing between primary care and specialist practitioner in patients for whom differing diagnosis did not alter clinical outcome (for example epididymal cyst and normal epididymis). In examinations where assessment suggested a malignant cause, findings were correlated to final histology.
Specialist practitioner was defined as a fully trained urologist; urology nurse specialists did not primarily assess patients in our study. Patients seen in both district general hospitals as well as all peripheral community clinics were included in the study.
By means of a data collection sheet, the specialist practitioners documented their own examination findings and in non-2-week rule referrals also documented the clinical findings of the primary care physician. Lag time between referral and specialist assessment was documented, as was the category of referral requested by the primary care physician. The specialist physician was also requested, in the light of clinical findings, to decide retrospectively, in their opinion, which was the most appropriate category of referral priority. Data were analysed using the Chi-squared test with the assumption that unrefered patients did not have cancer and that no false negatives existed in the specialist practitioner group (confirmed on cross referencing with histological records).
Results
A total of 201 patients were analysed with a mean age of 49 years (range, 5–87 years). Overall, the average wait between referral and specialist assessment was 53 days (median, 56 days). Of these patients, 53 (26%) were referred under the 2-week rule. For all testicular cancers picked up in this study (n = 14), the sensitivity of the 2-week rule referral category was 64% and the sensitivity of other category referrals to benign pathology was 98%, in both cases statistically different to that of the specialist practitioner (P < 0.05). The positive predictive value of referrals in the 2-week rule category was 17%.
Testicular cancers
Fourteen cases of testicular cancer were detected in this study, a slightly larger number than predicted by the national average, of which 9 (64%) were referred under the 2-week rule. Two cases (14%) were referred as urgent: (i) a 36-year-old waited 4 days to be assessed as his referral was expedited when his referral letter was read by the specialist practitioner; and (ii) a 31-year-old waited 54 days.
A 64-year-old was referred under the ‘soon’ category by a primary care physician suspecting a hydrocoele and this patient waited 56 days.
Two cases were referred under the ‘routine’ category of priority. The first, a 39-year-old, waited 75 days and the second, a 48-year-old, waited 32 days. In both of theses cases, the primary care physician suspected benign disease within the epididymis and sought re-assurance from the specialist physician to confirm this diagnosis.
Two-week rule patients
Of the 53 2-week rule patients, 51 (96%) were seen within the required 14 days. One patient waited 17 days and the other 21 days – both of these patients were subsequently found to have benign pathology outside the body of the testis.
Only 10 patients (19%) were assessed by the specialist practitioner as actually having a ‘lump within the body of the testis’ – 9 cases of testicular cancer and one benign cyst of the tunica albuginea. Of the 2-week rule patients, 43 (81%) were thought by the examining specialist practitioner to have been inappropriately referred under this category of priority purely on the restrictions of the Cancer Collaborative guidelines (Fig. 1). It was thought that in 16 patients (30%) the priority should have been three thresholds lower, i.e. referred on a routine basis.
Figure 1.
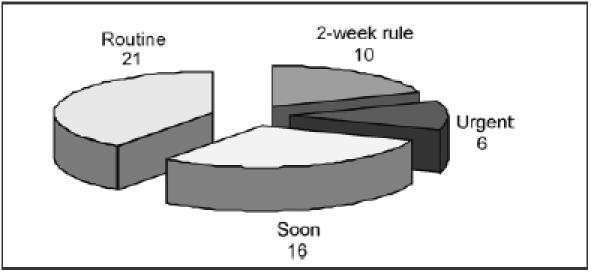
Recategorisation of priority (number of patients) by specialist practitioner in patients referred under the two-week rule (n = 53).
Primary care examination
Of the non-2-week wait rule referrals, the examination findings of the primary care physician and the specialist practitioner disagreed in 88 cases (59%). Seventy-one patients (35%) were referred with suspected testicular cancer by the primary care physician (categorised as either a 2-week rule referral or statements within the text of a referral letter of any priority category) of whom 62 (87%) were subsequently found by the specialist practitioner to have benign pathology (Fig. 2).
Figure 2.
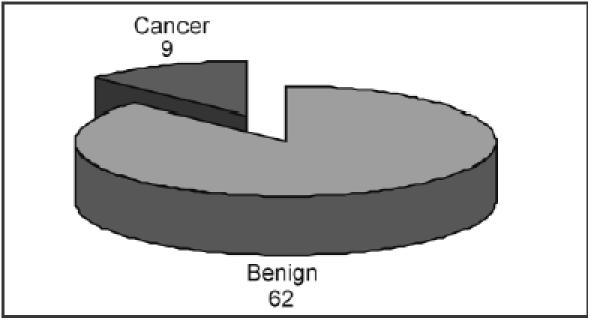
Clinical findings of patients referred as suspected cancer (n = 71).
Within the group of patients suspected by the primary care physician to have a high suspicion of testicular cancer, 32 patients (62%) were found by the specialist practitioner to have benign pathology involving normal variants of the epididymis.
As previously mentioned, one testicular cancer was misdiagnosed as benign and the inappropriate referral outside the 2-week rule referral category priority of two others delayed the diagnosis and treatment of one patient.
Prioritisation
Overall, primary care physicians and specialist practitioners agreed on the prioritisation category of patients in 106 cases (53%; P < 0.05).
Discussion
When providing for an effective healthcare system, a fast-track system that identifies high-risk patients in the primary care setting and facilitates swift specialist assessment and treatment is desirable and often attainable if resources permit.4 It is unavoidable that facilitating this service leads to the delay in assessing and treating patients who fall outside this fast-track system.5 It is, therefore, essential that three conditions are fulfilled: (i) the fast-track group of patients have a high sensitivity for the disease (and preferably also a high positive predictive value for the disease); (ii) few, if not no, patients with the disease fall outside the fast-track category; and (iii) diagnostic uncertainty or sought re-assurance is dealt with swiftly. With regards to the referral of suspected testicular cancer, our study suggests these conditions are failing. The inflexibility of the 2-week wait rule referral criterion is not allowing primary care physicians to refer patients as they see fit. Testicular cancers are still being diagnosed in other referral priority categories and inequity exists in patients needing second opinion diagnostic confirmation for borderline, but ultimately benign, conditions. As a result, the waiting times for the assessment of non-2-week rule referrals will be prolonged and by implication testicular cancer patients within these groups are subject to a delay in their management.
Soon, cancer patients will need to meet the target of having definitive treatment within 60 days and 18 weeks for other patients.6 It will, therefore, be even more essential to improve efficiency; cancer patients will need to be identified quickly from benign patients who often only need one-stop assessment. If this can only be performed outside primary care, then greater capacity will be needed within hospital medicine. It has been suggested that simply reducing overall waiting times for assessment may equally benefit health care provision7 and, in addition, the Department of Health Modernisation Agency document8 Ten High Impact Changes suggests pooling queues can have a profound impact on decreasing waiting times ‘where clinically appropriate’. In the case of scrotal pathology, this document would suggest that assessment in all patients should be performed within 2 weeks as, in our study, cancers were found in referrals outside the 2-week wait referrals.
It appears from this study that the assessment of scrotal pathology within the primary care setting is difficult. The main aim is to confirm the non-existence of cancer and a primary care physician acting in isolation cannot often achieve this. Without adequate back-up, inaccuracies lead to both misdiagnosis and the misprioritisation of referrals. This concurs favourably with studies in other specialities.9,10
This study is, however, limited by several factors. It is not possible to assess accurately any diagnostic uncertainties, additional information, patient pressure or clinical suspicions held by the primary care physician. It is also not possible to analyse those patients that were assessed by the primary care physician and not referred. The rigid referral criteria may skew the results; for example, the fact that 93% of testicular cancers occur below 60 years of age11 does not lead to any referral guidance may be adversely affecting the results.
In order to improve the situation, it could be suggested to allow all patients with any suspicion of scrotal pathology found by the primary care physician or on self-examination12 the opportunity of fast-track assessment by a specialist practitioner by means of a one-stop assessment. Many patients, especially those with benign disease, can be fully consulted, examined and counselled within a short period of time. The introduction of testicular ultrasonography into the primary care setting13 or into the specialist practitioners’ out-patient setting may be beneficial and in itself would not prolong the length of the consultation a great deal. Both options have implications on the workload, training and financial burden of the healthcare provider. Many regions offer primary care liaison activities and training sessions to assist in continuing primary care education and often this is invaluable in the reciprocation of information and education of both parties.
Unsurprisingly, this study confirms that primary care physicians and specialist practitioners do not agree on the prioritisation of patient referrals. There does not appear to be a move towards allowing the specialist practitioner to prioritise14 as he or she sees fit and perhaps removing the boundaries of prioritisation may be the easiest solution.
Conclusions
With regards to the referral of suspected testicular cancer and in agreement with other specialities,15–17 the 2-week rule does not appear to be the optimum solution for patient care. Overall, the sensitivity of the 2-week wait referrals for total cancers does seem acceptable when compared to other cancers (64%) but within the constraints of the referral criterion the positive predictive value appears only just acceptable (17%). A high proportion of patients will have their diagnosis changed by the specialist practitioner. The disagreement with regards to referral priority questions which practitioner should control the prioritising process.
Acknowledgments
The authors would like to acknowledge the help of Mr Hugh Gilbert and Mr Richard Kinder in the collection of patient data.
References
- 1.Department of Health. Referral Guidelines for Suspected Cancer. London, DH: 1999. [Google Scholar]
- 2.Clinical Oncology. Clinical Oncology Information Network Guidelines on the Management of Testicular Cancer. 2000. (©Royal College of Radiologists) [Google Scholar]
- 3.Department of Health. NHS Cancer Plan. London, DH: 2000. [Google Scholar]
- 4.Department of Health. The Cancer Services Collaborative 12 months on. London, DH: 2000. [Google Scholar]
- 5.Khawaja AR, Allan SM. Has the breast cancer ‘two week wait’ guarantee for assessment made any difference? Eur J Surg Oncol. 2000;26:536–9. doi: 10.1053/ejso.2000.0942. [DOI] [PubMed] [Google Scholar]
- 6.Department of Health. NHS Cancer Plan. London, DH: 2000. p. 48. [Google Scholar]
- 7.Thomas S, Burnet N. Two week rule for cancer referrals. Reducing waiting times from diagnosis to treatment might be more effective. BMJ. 2001;323:864. [PMC free article] [PubMed] [Google Scholar]
- 8.Department of Health Modernisation Agency Document. Ten High Impact Changes. London, DH: [Google Scholar]
- 9.Martin JP, Gabe SM, Pitcher MC, Jacyna MR. Referral patterns to a district general hospital gastroenterology outpatient clinic: implications for the ‘two-week target’. Int J Clin Pract. 2002;56:26–8. [PubMed] [Google Scholar]
- 10.Debnath D, Dielehner N, Gunning KA. Guidelines, compliance, and effectiveness: a 12 months’ audit in an acute district general healthcare trust on the two week rule for suspected colorectal cancer. Postgrad Med J. 2002;78:748–51. doi: 10.1136/pmj.78.926.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Department of Health. Referral Guidelines for Suspected Cancer. London, DH: 2000. [Google Scholar]
- 12.Moore RA, Topping A. Young men's knowledge of testicular cancer and testicular self-examination: a lost opportunity? Eur J Cancer Care. 1999;8:137–42. doi: 10.1046/j.1365-2354.1999.00151.x. [DOI] [PubMed] [Google Scholar]
- 13.Kromann-Andersen B, Hansen LB, Larsen PN, Lawetz K, Lynge P, Lysen D, et al. Clinical versus ultrasonographic evaluation of scrotal disorders. Br J Urol. 1988;61:350–3. doi: 10.1111/j.1464-410x.1988.tb13973.x. [DOI] [PubMed] [Google Scholar]
- 14.Sauven P. Two week rule for cancer referrals. Specialists, not GPs may be best qualified to assess urgency. BMJ. 2001;323:864–5. [PubMed] [Google Scholar]
- 15.Jones R, Rubin G, Hungin P. Is the two week rule for cancer referrals working? BMJ. 2001;322:1555–6. doi: 10.1136/bmj.322.7302.1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oliver MD. Two week rule for cancer referrals. All stages of care pathway need speeding up. BMJ. 2001;323:864. [PubMed] [Google Scholar]
- 17.Riesewyk C, Hayward C, Enser V, Northover J. Referral and diagnostic process in suspected colorectal cancer needs to be improved to achieve two week target. BMJ. 2000;321:1527. [PMC free article] [PubMed] [Google Scholar]


