Abstract
A working group coordinated by the World Health Organization developed a set of indicators to protect children’s health from environmental risks and to support current and future European policy needs. On the basis of identified policy needs, the group developed a core set of 29 indicators for implementation plus an extended set of eight additional indicators for future development, focusing on exposure, health effects, and action. As far as possible, the indicators were designed to use existing information and are flexible enough to be developed further to meet the needs of policy makers and changing health priorities. These indicators cover most of the priority topic areas specified in the Children’s Environment and Health Action Plan for Europe (CEHAPE) as adopted in the Fourth Ministerial Conference on Health and Environment in 2004, and will be used to monitor the implementation of CEHAPE. This effort can be viewed as an integral part of the Global Initiative on Children’s Environmental Health Indicators, launched at the World Summit on Sustainable Development in 2002.
Keywords: children, environmental health, Europe, indicators, policy
Approximately a quarter of the global burden of disease can be attributed to environmental factors (Prüss-Ustün and Corvalán 2006). Children < 5 years of age bear > 40% of this burden [Smith et al. 1999; World Health Organization (WHO) 2002a]. Contaminated air, food, and drinking water are particular environmental factors affecting children in developing regions of the world (Abalak et al. 2001; Smith et al. 2000). An estimated 1.7 million deaths per year globally are attributed to unsafe water, sanitation, and hygiene; nine of 10 of these deaths occur in children, and nearly all of these occur in developing countries (Prüss-Ustün and Corvalán 2006). Although the traditional infectious disease threats to children’s health have largely been controlled in most industrialized countries by advances in water treatment, immunizations, waste disposal, and the provision of adequate food (Suk et al. 2003), diseases such as asthma and cancers including leukemia, learning disabilities, and congenital malformations are increasing in children in western Europe (Landrigan et al. 1998; Richardson et al. 2005; Simoni et al. 2005). Even if most of the deterministic processes leading to these diseases are multifactoral, there is increasing evidence that these diseases are influenced by environmental factors. Exposure to air pollution, lead, chemicals, and noise has been shown to impair children’s health and their cognitive development (Bellinger 2004; Niemann et al. 2005; Schwartz 2004). Despite the fact that the European Region contains some of the world’s wealthiest countries, widening health inequalities remain the principal determinant of mortality (Anonymous 2005), illustrated by the fact that almost 140 million (16%) people in the WHO European Region do not have a household connection to a drinking-water supply, 85 million (10%) do not have improved sanitation, and > 41 million (5%) do not have access to a safe drinking-water supply (Anonymous 2005). From a burden perspective, injury is responsible for 23% of all deaths and 19% of disability-adjusted life-years (DALYs) in 0- to 19-year-olds in the WHO European Region and has the largest environmental burden for children compared with outdoor/indoor contaminants, water sanitation and hygienic issues, or lead contaminants (Valent et al. 2004)
The Fourth Ministerial Conference on Environment and Health, held in Budapest, Hungary, in June 2004 (“The Budapest Conference”), focused on “the future for our children,” recognizing the need to address the rights of children, their health, and their particular vulnerability toward environmental risks, as well as to respond to emerging environmental concerns. The Declaration from the conference reaffirmed that the Environment and Health Information System (EHIS) is an essential tool for policy making relevant to children’s environmental health (bWHO Regional Office for Europe 2004b).
The Budapest Conference through its Declaration adopted the Children’s Environment and Health Action Plan for Europe (CEHAPE), an international instrument negotiated with member states to develop and manage environmental health indicators. CEHAPE sets four regional priority goals (RPGs) that encapsulate key themes for action on children’s health in relation to environmental factors: a) gastrointestinal health related to safe water and adequate sanitation; b) healthy and safe transport, mobility, and home environment to reduce injuries and enhance physical activity; c) respiratory health and clean air; and d) health through environment free of hazardous chemicals, physical, and biological factors.
Although the RPGs do not explicitly cover social indicators, the CEHAPE recognizes that these factors are critical in determining a child’s possible increased exposure or vulnerability to a number of environmental factors.
Reliable information is essential for prioritizing actions related to environmental exposures and their health effects as well as for monitoring the effectiveness of the actions taken. Currently, this information is widely scattered and difficult to obtain on international and national levels. Where it does exist, its contents and format are often inappropriate for international comparisons, for policy support, or for public communication. Providing decision makers with appropriate information regarding health effects attributable to environmental risks is of crucial importance. They require information about the issues of concern and an indication of the hazards and the risks that need to be addressed (Briggs 2003). Such information should enable them to assess the implications of their decisions, compare the potential effects of different decisions and choices, and ultimately develop effective prevention strategies (Corvalán et al. 2000). Such information includes environmental quality guidelines based on epidemiologic and toxicologic studies (e.g., WHO air quality guidelines; WHO 2006a). Overall, the information needs to be clear, concise, relevant, and powerful (Briggs 2003).
WHO has been coordinating the development of methods and tools for a pan-European EHIS to support policy making since 1999. In particular, the development of environmental health indicators—the EHIS central element—has been significantly advanced through a series of projects in collaboration with relevant international organizations. The project Development of Environment and Health Indicators for European Union (EU) countries (ECOEHIS), co-funded by the Directorate-General for Health and Consumer Protection of the European Commission (EC) and coordinated by WHO, was a part of this process and resulted in the proposal of 17 core indicators under six themes for monitoring the EU population’s exposure to environmental hazards, their health effects, and related policy actions (aWHO Regional Office for Europe 2004a; Kim et al. 2005).
The Declaration from the Budapest Conference reaffirmed that the EHIS is an essential tool for policy making relevant to children’s environmental health. The development and application of indicators focusing on children’s environmental health and facilitating monitoring and evaluation of the environmental health risks and the effect of interventions has become a significant objective (bWHO Regional Office for Europe 2004b).
An international project, Implementing Environment and Health Information System in Europe (ENHIS), co-funded by the EC and coordinated by the WHO Regional Office for Europe, developed a prototype of an evidence-based system to support children’s health and environmental policies in the European Region. Among the key products is a core set of children’s environmental health indicators to monitor the implementation of the CEHAPE with a prototype pan-European EHIS. Here we report the process and products of the ENHIS project related to developing children’s environmental health indicators.
Methods
A working group comprised a core group of international experts representing each of the technical areas identified by the RPGs, plus a network of invited experts in each of the fields. This group carried out the following tasks: determine the needs of current and future environmental health policies; define the scope and target of the indicators; produce the methodologic guidelines for each of the indicators; pilot test the indicators and then further refine the indicators; and select a core set of indicators for pilot implementation. During the process, the group was concerned primarily with the need to select reliable indicators for which there was evidence in published literature that a clear health link exists between the environmental exposure and health outcome, while allowing comparison in the framework of the implementation of the CEHAPE. However, the group was mindful of the need not to place too much of a reporting burden on countries and therefore, where possible, to prioritize indicators for which routine monitoring and published data were readily available in most countries.
The indicators were designed to a) enable monitoring of children’s environmental health risks, their determinants, and effects of the intervention; b) provide appropriate information to countries to monitor the state of children’s environmental health, allow trends to be established, and support national policies and action programs; c) provide a sustainable basis for reporting and dissemination of evidence-based information (i.e., there is a policy need plus there is an established link between the exposure and health outcome) on children’s environmental health, avoiding duplication and ensuring continuity; and d) provide a basis for improvement of existing monitoring and surveillance systems by pointing out priority data gaps in order to inform policy-making decisions.
Overall process of development of the indicators
Based on these criteria the process of development of the indicators was initiated. To present the links between environment, health outcomes, and actions the DPSEEA framework developed by Corvalán et al. (1996) was used. This framework defines driving forces (D), that lead to pressures on the environment (P), which in turn change the state of the environment (S), resulting in human exposures (Ex) and then to health effects (E). Actions (A) can be taken at any point during the chain to mitigate health effects.
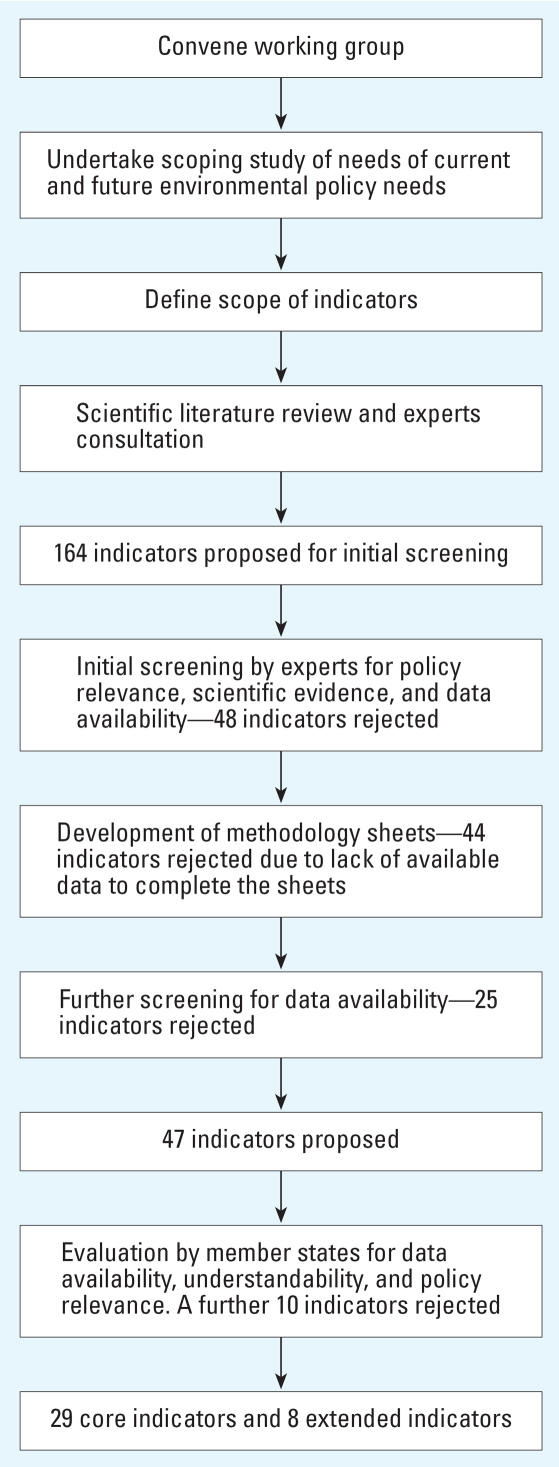
The scope of indicators developed for the current project focused on exposure, health effects, and policy actions within the conceptual framework of cause-effect proposed by WHO (1999). The process of development is detailed in the following sections and summarized in Figure 1.
Figure 1.
Overall process of development of the indicators.
Initial selection of candidate indicators
The working group undertook to assess the information needs of European environmental health policies by identifying the requirements of relevant legislation and guidelines such as the Protocol on Water and Health (cWHO Regional Office for Europe 2004c). This was done through the development of a questionnaire on current and planned children’s environmental and health policies at EU and domestic levels for the creation of an inventory. The questionnaire was sent to national collaborating centers of the ENHIS project and was completed by public health and environmental officials or national experts in the existing policies. The topics that were identified as policy priorities from this process were water and sanitation, noise, air pollution [including environmental tobacco smoke (ETS)], housing (including injuries), transport, and radiation. Social determinants were also considered important but these are not included in the key themes of CEHAPE, and it was eventually decided not to include social indicators in the project.
To address the assessment of the information needs of European environmental health policies, the working group reviewed the scientific literature of the links between environmental factors and health effects, and proposed a series of indicators of relevance to the RPGs regardless of data availability and existence of methodology sheets.
The review of the policy needs identified topic areas for which no clear regulatory framework exists. Examples include drinking-water safety, ensuring safe transport and mobility, counteracting obesity, and indoor air quality. The policy measures with clear legal and regulatory context are dedicated mainly to environmental protection and improvement of environmental quality. Furthermore, these policies do not cover the range of harmful health effects, particularly on children’s health, resulting from exposure to a regulated environmental substance.
These considerations guided the working group to select environmental public health thematic issues for which policy indicators needed to be developed. The working group sought to develop policy indicators to provide a snapshot of the measures put in place in countries to reduce and prevent hazardous exposures and related health effects in children. At the same time, the analysis of the policy indicators would identify policy gaps—areas not addressed by current policy measures.
Policy indicators were conceived as a composite index across a set of policy actions using a simple equal-weight linear model. To obtain the index, each individual policy measure was scored with the following options: 0 = not existing, 1 = partly existing, 2 = clearly stated and implemented across the country.
Because there is no consensus nor many systematic reviews on policy actions’ interventions, the working group checked international health regulation documents to select the policy components for the composite measure. These included the WHO Framework Convention on Tobacco Control (WHO 2003a), European Strategy for Tobacco Control (WHO Regional Office for Europe 2002), First Action Plan for Food and Nutrition Policy (WHO Regional Office for Europe 2001), European Child Safety Alliance (2004b), Child Safety Action Plan Project (European Child Safety Alliance 2004a), and the CEHAPE program and related table of actions (WHO Regional Office for Europe 2005).
This process resulted in 164 indicators (including those that had already been tested in the ECOEHIS project). The phase of reducing the number of indicators then began through a series of expert working group consultations. Initially, indicators that had already been tested and recommended by the ECOEHIS project and could be adjusted to meet the requirements of CEHAPE were selected. In addition, new indicators that corresponded to emerging policy and health priorities covered by the RPG action items of the CEHAPE were selected and developed. The proposed indicators were screened according to their policy relevance, health relevance, and potential data availability, including a review of published literature linking environmental factors and health outcomes as well as using the results from the policy questionnaire described above.
We assessed each indicator in terms of its credibility (i.e., based on a knowledge link between environment and health taking into account uncertainties), basic information on the definition, calculation method, interpretation, and potential data sources. The process and contents of assessments were recorded. There is scientific uncertainty in environmental health that needs to be reduced. During the process of selecting the indicators, we screened published literature to assess the scientific credibility of the available data. Within these criteria, the indicators were either set aside or accepted for development. This assessment reduced the number of proposed indicators to 116.
Methodology sheets
To ensure the information collected on the proposed indicators was consistent and user friendly, we adopted a template for a methodology sheet used in the ECOEHIS project (Table 1).
Table 1.
Template of the methodology sheet used to define the indicators.
| Indicator | Position in DPSEEA chain |
|---|---|
| Issue | Specification of the environmental health issue as stated in the CEHAPE regional priority goals to which the indicator relates |
| Justification for this indicator | Describe the importance of this indicator in terms of the priorities of children’s environmental health considering the magnitude, severity, amenability, and public concerns of the problem, with special attention to CEHAPE action item. State the evidence linking exposure, effect, and policy actions. Specify how this indicator can effectively monitor the achievement or actions of CEHAPE regional priority goals
Quote the relevant part from CEHAPE as a key justification, followed by a summary of scientific evidence and policy effectiveness |
| Definition of indicator | Detailed technical definition of the indicator. If there are subindicators, provide their definitions. |
| Underlying definitions and concepts | Definition of all terms and concepts involved in describing and constructing the indicator |
| Specification of data needed | List data elements needed to construct the indicator |
| Data sources, availability, and quality | Outline potential sources of data, and comment on their quality and characteristics in terms of the indicator. Where appropriate, indicate ways of obtaining data that are not readily available |
| Computation | Specify how the indicator is computed: i.e., how the data are analyzed/processed to construct the indicator. Where relevant, express the computation process mathematically, and define the terms used |
| Units of measurement | Specify the units of measurement used in presenting the indicator |
| Scale of application | Specify the potential scales of application or level of aggregation. The scale specified refers to the area across which the indicator can be used; for geographic comparisons, the indicator might be developed at lower levels of aggregation. Definitions: local (within a city or community); regional (within a subnational region); national (for a country); international (across several countries or globally) |
| Interpretation | Describe how the indicator may be interpreted in relation to the issue(s) specified |
| Linkage with other indicators | Describe the relationship between this and other indicators relating to the issue(s) specified, listing all indicators and their position in the DPSEEA chain |
| Related data, indicator sets, websites | List similar or related indicators, proposed or developed as part of other indicator sets |
| Policy/regulatory context | List and briefly explain any international policy or regulations in the forms of declaration, action plan, framework, treaty, directives related the issue that this indicator is dealing with |
| Reporting obligations | Describe whether the reporting of the data elements for this indicator is obliged for the member states by the international legislations or constitutions |
Through the development of methodology sheets for each indicator, it became apparent that in the case of 44 indicators there were insufficient data available to continue development. These indicators were put aside, despite being considered potentially useful for the future.
To avoid duplication and assure continuity of developmental work, we reviewed the indicators tested and proposed in the ECOEHIS project for their relevance to children’s environmental health. Eleven indicators from the core indicators selected in the ECOEHIS project were adopted on the basis of their relevance to children’s health and the availability of data.
Adjustment and screening of the indicators
Further review of the indicators was undertaken by member states and technical experts, until a final list of 29 core indicators was produced. The primary reason for rejecting proposed core indicators at this stage was unavailability of data from international sources. Nine indicators that were rejected from the core set were retained for future use and were termed “extended set.” These indicators were deemed highly relevant to children’s health, but at present the required data to compute the indicator do not exist.
Before finalization of the 29 core indicators, the experts were still uncertain about the feasibility and applicability of eight indicators that had not been evaluated in the ECOEHIS project. It was decided that these indicators should undergo an evaluation process in the countries represented in ENHIS (Austria, the Czech Republic, Finland, France, Germany, Hungary, the Netherlands, Poland, Romania, Spain). Four of these were action indicators and four were exposure indicators. The indicators screened were policies to promote safe mobility and transport for children; policies to reduce child unintentional injury unrelated to traffic accidents; policies to reduce child obesity; children living in homes using a hazardous source of fuel for cooking and heating; children living in proximity to heavily trafficked roads; children going to school with indoor air problems; actions to reduce children’s exposure to ultraviolet (UV) radiation; blood lead levels in young children. It was not deemed necessary to evaluate the indicators that had been developed for or adapted from the ECOEHIS project because these had already been tested. Details of the process taken to test the indicators selected for the ECOEHIS project are discussed by the WHO Regional Office for Europe (2004a).
The request to evaluate the indicators was sent to officials from the ministry of health and/or environment in the participating countries together with the methodology sheet and the contact data of the national partner institution. The questionnaire that accompanied the methodology sheets focused on four criteria of evaluating indicators and data elements: data quality, usefulness (combined as one category in Table 2 and described as understandability) data availability, and policy relevance (Table 2). The responses were collected using the questionnaire from April to June 2005.
Table 2.
Summary of screening results.
| Austria | Czech Republic | France | Hungary | Netherlands | Poland | Romania | Spain | |
|---|---|---|---|---|---|---|---|---|
| Policies to promote safe mobility and transport for children | ||||||||
| Data availability | X | X | X | X | X | X | X | X |
| Understandability | X | X | X | X | X | X | X | |
| Policy relevance | X | X | X | X | X | X | X | |
| Policies to reduce children’s unintentional injury unrelated to traffic accidents | ||||||||
| Data availability | X | X | X | X | X | X | X | X |
| Understandability | X | X | X | X | X | X | X | |
| Policy relevance | X | X | X | X | X | X | X | X |
| Policies to reduce child obesity | ||||||||
| Data availability | X | X | X | X | X | X | X | X |
| Understandability | X | X | X | X | X | X | X | |
| Policy relevance | X | X | X | X | X | X | X | X |
| Children living at home using a hazardous source of fuel for cooking or heating | ||||||||
| Data availability | X | |||||||
| Understandability | X | X | X | X | X | |||
| Policy relevance | X | X | X | X | X | |||
| Children living in proximity to heavily trafficked roads | ||||||||
| Data availability | X | X | ||||||
| Understandability | X | X | X | X | X | X | X | |
| Policy relevance | X | X | X | X | X | X | X | |
| Children going to schools with indoor air problems | ||||||||
| Data availability | ||||||||
| Understandability | X | X | X | |||||
| Policy relevance | X | X | X | X | ||||
| Actions to reduce children’s exposure to UV | ||||||||
| Data availability | X | X | X | X | X | X | ||
| Understandability | X | X | X | X | X | X | X | |
| Policy relevance | X | X | X | X | X | X | ||
| Blood lead levels in young children | ||||||||
| Data availability | X | X | ||||||
| Understandability | X | X | X | X | X | X | X | |
| Policy relevance | X | X | X | X | X | |||
Results
Screening in participating member states
Table 2 shows a summary of the results of the screening process in eight participating member states. The results revealed lack of data in four areas related to air pollution: the protection of children from air pollutants derived from cooking and heating facilities; the protection of children living in proximity to heavily trafficked areas; the protection of children going to schools with indoor air problems; and the protection of children from exposure to heavy metals such as lead (expressed as blood lead levels in young children). In addition, limited data were available in relation to the indicators on actions to reduce children’s exposure to UV. However, their relevance to policy in Europe was considered to be high.
Core set of indicators
Tables 3–6 show the final set of children’s environmental health indicators according to the RPGs. The core indicators were deemed policy relevant and readily available from international data sources with sufficient quality and comparability. The eight indicators listed under “extended set” were retained for future development and use.
Table 3.
Core and extended indicators related to CEHAPE regional priority goal I.
| Indicator title (and type) | Origin and international data source, if available | Definition of the indicator |
|---|---|---|
| Core indicators | ||
| Wastewater treatment (exposure) | Adapted from ECOEHIS | Percentage of the child population served by sewage connected to a wastewater treatment facility that produces a regulated effluent discharge monitored by the competent authorities, or to an alternative safe local wastewater disposal system, e.g., septic tank |
| Recreational water quality (exposure) | Adapted from ECOEHIS | Proportion of identified bathing waters, falling under the EU bathing water directive definition (CEC 1976) |
| Drinking-water compliance (exposure) | Adapted from ECOEHIS | Proportion of the drinking-water samples analyzed from regulated public supplies that fail to comply with the Escherichia coli parameter of the EU drinking-water directive (CEC 1998) |
| Safe drinking water (exposure/policy) | Adapted from ECOEHIS | Proportion of the child population with continuous access to an adequate amount of safe drinking water in the home |
| Management of bathing waters (policy) | Adapted from ECOEHIS | Percentage of identified bathing waters which are covered by management systems as described by WHO (2003b) |
| Water safety plans (policy) | Adapted from ECOEHIS | Proportion of the child population served by a potable water supply covered by a ‘water safety plan’ as described by WHO (2006b) |
| Extended set of indicators | ||
| Reliability of the water supply (exposure) | New | Percentage of the child population who have access to a reliable water supply |
| Outbreaks of waterborne diseases in children (health) | New | Number of outbreaks of fecal–oral water-related illness in the child population reported separately for drinking-water and recreational waters |
| Incidence of priority diseases in children (health) | New | The incidence of key water-related infections in the child population |
Table 6.
Core and extended indicators related to CEHAPE regional priority goal IV.
| Indicator title | Origin and data source, if available | Definition of the indicator |
|---|---|---|
| Core indicators | ||
| Children exposed to harmful noise at school (exposure) | New. Noise map available in 2008 according to EU directive on environmental noise (CEC 2002) | Percentage of children going to primary or secondary schools located in places that are considered to be exposed to transport (road, rail, and aircraft) noises > 55 dB (A) average during school hours |
| Actions to reduce children’s exposure to UV (policy) | New | This is a composite index of national efforts to improve protection of children against UV exposure |
| Incidence of melanoma (health) | Adapted from ECOEHIS. Data available from International Agency for Research on Cancer | Incidence of melanoma by age periods of 5 years, among children and adults up to 45–50 years of age |
| Incidence of childhood leukemia (health) | New | Annual incidence rate of leukemia |
| Work injuries among employees < 18 years of age (health) | New. Data available from EUROSTAT (Eurostat 2007) | Incidence rate of work accidents with victims < 18 years of age per 100,000 workers
According to the severity, there are two subindicators: Nonfatal work injuries with > 3 days’ absence from work Fatal work injuries |
| Children’s exposure to chemical hazards in food (exposure/policy) | New. Data available from WHO (2007) | Dietary exposure assessment to potentially hazardous chemicals monitored in children’s food Global Environmental Monitoring System/Food Contamination Monitoring and Assessment Programme (GEMS/Food) |
| Persistent organic pollutants in human milk (exposure) | New. Data available from WHO (2007) | Concentrations of dioxins and polychlorinated biphenyls in human milk fat (expressed as WHO toxicity equivalents in pg/g) in pooled samples using standardized collection and analytical protocols established by WHO |
| Blood lead levels in children (exposure) | New | Average of blood lead levels (μg/dL) in children < 6 years of age
Percentage of children < 6 years of age with elevated blood lead levels (> 10 μg/dL) |
| Extended set of indicators | ||
| Radon levels in schools (exposure) | Distribution of annual radon levels in classrooms and inhabited rooms of kindergarten, schools, and colleges
Estimated arithmetic mean, median of radon concentration Estimated percentage (and number) of classrooms and other rooms with annual mean levels of radon > 200, 400 Bq/m3 Specified at the national or regional level |
|
| Children with hearing loss and reporting tinnitus (health) | Proportion of children with hearing loss due to noise | |
Discussion
The indicators developed in this project met a specific task identified by the Budapest Declaration: to address the environmental factors that most affect the health of European children (bWHO Regional Office for Europe 2004b). Through the development of these indicators, the project has helped identify and prioritize the environmental health issues that are widespread in the European Region.
The screening process undertaken by eight countries highlighted the national variations in data availability, policy relevance, and priorities. It became clear through this process that even in this small number of member states there are gaps in policies relating to some areas of children’s environmental health as well as available data. One such area is indoor air quality. However, indoor air is an important issue with respect to children’s environmental health specifically targeted in CEHPAE, and keeping such indicators was considered valuable to encourage efforts to collect relevant data. Although not all of the issues are a priority in all countries, and countries should therefore choose the indicators that best suit their priorities and conditions, including resources, when establishing their own environmental health information system, there is clearly a need to fill these gaps through the development of national or international data collection systems.
The next phase of the project (begun in November 2005) was to implement the indicators in the European Region. This is making it possible to monitor the effect of actions taken to address the environmental health issues affecting children using standardized methodologies for data collection, processing, and dissemination, allowing inter- and intra-country comparisons and time trend analysis.
In the long term, the overall goal is to maintain an active and up-to-date European database of environmental health policies and data, which would facilitate the development of harmonized and science-based environmental health policies across Europe and increase their accountability in population health terms. Differences between national policies will and should remain, but they should be based on different conditions and needs, rather than on the lack of information to assess their effectiveness and accountability.
The environmental health indicators developed in this project can be readily applied in most EU countries in monitoring the implementation of CEHAPE. The indicators will need to be reviewed and updated regularly to maintain flexibility and responsiveness. By outlining the priority data flows in a pan-European EHIS, the core indicators will provide guidelines for the reporting on the progress of realization of four RPGs of the CEHAPE.
The development of environmental health indicators to monitor the trends in the state of European children contributes toward the objectives of the Global Initiative on Children’s Environmental Health Indicators launched at the World Summit on Sustainable Development in 2002, initiated by and building on efforts of the U.S. Environmental Protection Agency (WHO 2002b). The indicators developed and made available through the regional pilot surveys as well as information from ongoing international surveys and reporting mechanisms will be part of the comprehensive evidence base toward healthy public policies to better protect the health of our children and the generations to come.
Table 4.
Core and extended indicators related to CEHAPE regional priority goal II.
| Indicator title (and type) | Origin and data source, if available | Definition of the indicator |
|---|---|---|
| Core indicators | ||
| Child mortality from traffic accidents (health) | Amended from ECOEHIS | Child mortality from traffic accidents by age group and by mode of accident |
| Policies for safe transportation for children (policy) | Child Safety Action Plan (European Child Safety Alliance 2004a) | Existence and actual enforcement of legislation and regulations establishing mandatory requirements for safe mobility and transport for children |
| Children’s mortality due to unintentional injuries not related to traffic accidents (health) | Amended from ECOEHIS | Data available from the WHO Mortality Database (WHO 2005). Cause-specific child mortality rates per 100,000 population for unintentional injuries not related to traffic accidents |
| Policies to reduce children’s mortality due to unintentional injuries not related to traffic accidents (policy) | Child Safety Action Plan (European Child Safety Alliance 2004a) | Existence and enforcement of legislation and regulations aimed at reducing child injury |
| Prevalence of overweight and obesity in adolescents (health) | New. Data found in HBSC (Currie et al. 2004) | Percentage of adolescents 15–19 years of age who are adequate weight, overweight, or obese, where adequate weight is defined as a BMI < 25 kg/m2, overweight is defined as a BMI 25–30 kg/m2, obesity is defined as a BMI of ≥30 kg/m2 |
| Percentage of physically active children (exposure) | New. Data available in HBSC (Currie et al. 2004) | The percentage of children reporting to be physically active for 1 hr/day at least 3 times per week |
| Policies to reduce childhood obesity (policy) | New | Composite index of the willingness and commitment to implement a national strategy to prevent obesity in accordance with the WHO Global Strategy on Diet, Physical Activity and Health (WHO 2004) and the WHO Food and Nutrition Action Plan for the WHO European Region, 2000–2005 (WHO Regional Office for Europe 2001) |
| Extended set of indicators | ||
| Mode of child transportation to school (exposure) | New | Percentage of children going to school by different modes |
Abbreviations: BMI, body mass index; HBSC, Health Behaviour in School-aged Children study.
Table 5.
Core and extended indicators related to CEHAPE regional priority goal III.
| Indicator (and type) | Origin and data source, if available | Definition of the indicator |
|---|---|---|
| Core indicators | ||
| Policies to reduce tobacco smoke exposure in children (policy) | Adapted from ECOEHIS indicator | This indicator is aimed at constructing a composite index of capability for implementing policies to reduce smoking and exposure to ETS in children and adolescents |
| Prevalence of allergies and asthma in children (health) | New | Prevalence (%) of children with asthma in age groups (years) 0–4, 5–9, 10–14, 15–19 of total population of children in the respective age group
Prevalence (%) of allergy toward house dust mites, pollens, furry animals, and molds |
| Infant mortality due to respiratory diseases (health) | New | Annual mortality rate due to respiratory diseases in children > 1 month and < 1 year of age |
| Children’s exposure to air pollutants (exposure) | Adapted from ECOEHIS indicator | PM10: Child population-weighted annual mean PM10 concentration
PM2.5: Child population-weighted annual mean PM2.5 concentration O3: Child population-weighted annual mean (of maximum daily 8 hr means) O3 concentration NO2: Child population distribution of exceedance hours of air quality limit values SO2: Child population distribution of exceedance days of air quality values |
| Children living in homes with dampness problems (exposure) | Adapted from ECOEHIS indicator | Percentage of children 0–4, 5–9, 10–14, 15–19 years old living in damp housing
This indicator uses the Eurostat SILC (variable HH040) on dampness-related problems such as a) leaking roof, b) damp walls/floors/foundations, and c) rot in window frames or floor; all of which could lead to or represent mold growth |
| Children exposed to tobacco smoke (exposure) | New | Percentage of children 0–4, 5–9, 10–14 years old daily exposed to ETS
Percentage of smokers among children 10–14, 15–19 years old |
| Children living in homes using solid fuels (exposure) | New. Data from international surveys, e.g., demographic and health surveys (Measure DHS 2007), world health statistics (WHO 2006c), and censuses. Data also available from the Millennium Indicator Database (UN 2006) and Eurostat (2007) | Percentage of children 0–4, 5–9, 10–14 years old living in households using: coal, wood, dung, gas, or kerosene as the main source of heating and cooking fuel |
| Children living in proximity to heavily trafficked roads (exposure) | New | Percentage of children 0–4, 5–9, or 10–14 years old living in proximity to heavily trafficked roads |
| Extended set of indicators | ||
| Hospital admissions and emergency room visits due to asthma in children (health) | New | No. of hospital admissions or emergency room visits for asthma per 1,000 children by age group |
| Children going to schools with indoor air problems (exposure) | New | Percentage of children going to schools or day care centers with moisture damage or mold growth during the year
Percentage of children going to schools and day care centres with a ventilation < 7 L/sec per person |
Abbreviations: ETS, environmental tobacco smoke; PM2.5, PM10, particulate matter < 2.5 or 10 μm in aerodynamic diameter.
Footnotes
The authors thank the following experts who helped to develop the indicators: D. Kay, R. Aertgeerts, D. Lupulescu, F. Racioppi, M. Martuzzi, J. Pronczuk, G. Moy, D. Sethi, R.C. Vallenas, I. Ivanov, E. Rehfuess, and J. Vincenten.
This work was funded by the European Commission, Directorate-General for Health and Consumer Protection under grant 2003112.
References
- Abalak R, Bruce N, McCraken JP, Smith KR, de Gallardo T. Indoor respirable particulate matter concentrations from an open fire, improved cook stoves and LPG/open fire, combination in rural Guatemalan community. Environ Sci Technol. 2001;35:2650–2655. doi: 10.1021/es001940m. [DOI] [PubMed] [Google Scholar]
- [Anonymous] Children’s health coming of age in Europe [Editorial] Lancet. 2005;366(9491):1052. doi: 10.1016/S0140-6736(05)67399-0. [DOI] [PubMed] [Google Scholar]
- Bellinger DC. Lead. Pediatrics. 2004;113:1016–1022. [PubMed] [Google Scholar]
- Briggs A. Geneva: World Health Organization; 2003. [accessed 8 March 2007]. Making A Difference: Indicators to Improve Children’s Environmental Health. Available: http://www.int/ceh/publications/ceh1590599/en/index.html. [Google Scholar]
- CEC (Council of the European Communities) Bathing Water Quality. Directive 76/160/EEC. 1976. [accessed 27 March 2007]. Available: http://ec.europa.eu/water/water-bathing/directiv.html.
- CEC (Council of the European Communities) Directive (98/83/EC) on the Quality of Water Intended for Human Consumption. 1998. [accessed 27 March 2007]. Available: http://eur-lex.europa.eu/LexUriServ/site/en/oj/1998/l_330/l_33019981205en00320054.pdf.
- CEC (Council of the European Communities) Noise: Activities Linked to the Environmental Noise Directive. 2002. [accessed 26 March 2007]. Available: http://ec.europa.eu/environment/noise/activities.htm.
- Corvalán C, Briggs D, Kjellstrom T. Development of environmental health indicators. In: Briggs D, Corvalán C, Nurminen M, editors. Linkage Methods For Environment And Health Analysis. General Guidelines. Geneva: World Health Organization; 1996. pp. 19–53. [Google Scholar]
- Corvalán C, Briggs D, Zielhuis G. Decision-Making in Environmental Health: From Evidence to Action. London: E&FN Spon; 2000. [Google Scholar]
- Currie C, Roberts C, Morgan A, Smith R, Settertobulte W, Samdal O, et al. Health Behaviour in School-aged Children (HBSC) Study: International Report from the 2001/2002 Survey. Copenhagen: WHO Regional Office for Europe; 2004. [accessed 30 July 2007]. Young People’s Health in Context. Available: http://www.euro.who.int/InformationSources/Publications/catalogue/20040518_1. [Google Scholar]
- European Child Safety Alliance. Child Safety Action Plan. 2004a. [accessed 27 March 2007]. Available: http://www.eurosafe.eu.com/csi/eurosafe2006.nsf/wwwVwContent/61CE5CD93275507BC1257194004DE694?opendocument&context=C695AC19E93E2400C125717700353994.
- European Child Safety Alliance. 2. Amsterdam: European Child Safety Alliance; 2004b. [accessed 27 March 2007]. Priorities for Child Safety in the European Union: Agenda for Action. Available: http://www.childsafetyeurope.org/csi/ecsa.nsf/index/injurythemes/$file/2004whitebook.pdf. [Google Scholar]
- Eurostat. Eurostat Data. 2007. [accessed 27 March 2007]. Available: http://epp.eurostat.ec.europa.eu/
- Kim R, Dalbokova D, Krzyzanowski M. Development of environmental health indicators for European Union countries. EpiMarker. 2005;9(3):1–4. [Google Scholar]
- Landrigan PJ, Carlson JE, Bearer JS, Cranmer CF, Bullard R, Etzel RA, et al. Children’s health and the environment: a new agenda for prevention research. Environ Health Perspect. 1998;106:787–794. doi: 10.1289/ehp.98106787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Measure DHS. Demographic and Health Surveys. 2007. [accessed 27 March 2007]. Available: http://www.measuredhs.com/
- Niemann H, Maschke C, Hecht K. Noise induced annoyance and morbidity. Results from the pan European LARES-survey. Bundesgesundheitsblatt Gesundheits-forschung Gesundheitsschutz. 2005;48(3):315–328. doi: 10.1007/s00103-004-0997-y. [DOI] [PubMed] [Google Scholar]
- Prüss-Ustün A, Corvalán C. Towards an Estimate of The Environmental Burden of Disease. Geneva: World Health Organization; 2006. [accessed 6 December 2006]. Preventing Disease Through Healthy Environments. Available: http://www.who.int/quantifying_ehimpacts/publications/preventingdisease/en/ [Google Scholar]
- Richardson G, Eick S, Jones R. How is the indoor environment related to asthma? Literature review. J Adv Nurs. 2005;52(3):328–339. doi: 10.1111/j.1365-2648.2005.03591.x. [DOI] [PubMed] [Google Scholar]
- Schwartz J. Air pollution and children’s health. Pediatrics. 2004;113:1037–1043. [PubMed] [Google Scholar]
- Simoni M, Lombardi E, Berti G, Rusconi F, La Grutta S, Piffer S, et al. Mould/dampness exposure at home is associated with respiratory disorders in Italian children and adolescents: the SIDRIA-2 Study. Occup Environ Med. 2005;62(9):616–622. doi: 10.1136/oem.2004.018291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith KR, Corvalán CF, Kjellstrom T. How much global ill health is attributable to environmental factors? Epidemiology. 1999;10:573–584. [PubMed] [Google Scholar]
- Smith KR, Samet JM, Romieu I, Bruce N. Indoor air pollution in developing countries and acute lower respiratory infections in children. Thorax. 2000;55:518–522. doi: 10.1136/thorax.55.6.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suk W, Murray K, Avakian MD. Environmental hazards to children’s health in the modern world. Mutat Res. 2003;544:235–242. doi: 10.1016/j.mrrev.2003.06.007. [DOI] [PubMed] [Google Scholar]
- UN. New York: United Nations Statistics Division; 2006. [accessed 27 March 2007]. MDGInfo 2006. Available: http://mdgs.un.org/unsd/mdg/News.aspx?ArticleId=18. [Google Scholar]
- Valent F, Little D, Bertollini R, Leda NE, Barbone F, Tamburlini G. Burden of disease attributable to selected environmental factors and injury among children and adolescents in Europe. Lancet. 2004;363(9426):2032–2039. doi: 10.1016/S0140-6736(04)16452-0. [DOI] [PubMed] [Google Scholar]
- WHO. Report of the International Conference on Environmental Threats to the Health of Children: Hazards and Vulnerability; Bangkok, Thailand. 3–7 March, 2002; Geneva: World Health Organization; 2002a. [accessed 6 December 2006]. Available: http://www.who.int/docstore/peh/ceh/Bangkok/Bangkokconfreport.pdf. [Google Scholar]
- WHO. Global Initiative on Children's Environmental Health Indicators. 2002b. [accessed 30 July 2007]. Available: http://www.who.int/ceh/indicators/globinit/en/
- WHO. Geneva: World Health Organization; 1999. [accessed 6 December 2006]. Environmental Health Indicators: Framework and Methodologies. Available: http://whqlibdoc.who.int/hq/1999/WHO_SDE_OEH_99.10.pdf. [Google Scholar]
- WHO. Geneva: World Health Organization; 2003a. [accessed 27 March 2007]. WHO Framework Convention on Tobacco Control. Available: http://www.who.int/tobacco/framework/WHO_FCTC_english.pdf. [Google Scholar]
- WHO. Geneva: World Health Organization; 2003b. [accessed 30 July 2007]. Guidelines for Safe Recreational Water Environments. Vol 1: Coastal and Freshwaters. Available: http://whqlibdoc.who.int/publications/2003/9241545801.pdf. [Google Scholar]
- WHO. Geneva: World Health Organization; 2004. [accessed 27 March 2007]. Global Strategy on Diet, Physical Activity and Health. Available: http://www.who.int/dietphysicalactivity/strategy/eb11344/strategy_english_web.pdf. [Google Scholar]
- WHO (World Health Organization) Mortality Database. 2005. [accessed 27 March 2007]. Available: http://www3.who.int/whosis/menu.cfm.
- WHO. Geneva: World Health Organization; 2006a. [accessed 30 July 2007]. WHO Air Quality Guidelines for Particulate Matter, Ozone, Nitrogen Dioxide and Sulfur Dioxide. Global Update 2005. Summary of Risk Assessment. Available: http://whqlibdoc.who.int/hq/2006/WHO_SDE_PHE_OEH_06.02_eng.pdf. [Google Scholar]
- WHO. Geneva: World Health Organization; 2006b. [accessed 27 March 2007]. Guidelines for Drinking-water Quality. Vol 1: Recommendations. Available: http://www.who.int/water_sanitation_health/dwq/gdwq0506begin.pdf. [Google Scholar]
- WHO. Geneva: World Health Organization; 2006c. [accessed 27 March 2007]. World Health Statistics 2006. Available: http://www.who.int/whosis/whostat2006_toc2intro.pdf. [Google Scholar]
- WHO. Copenhagen: World Health Organization; 2007. [accessed 27 March 2007]. WHO SIGHT. Summary Information and Global Health Trends. Available: http://sight.who.int/ [Google Scholar]
- WHO Regional Office for Europe. Copenhagen: World Health Organization; 2001. [accessed 27 March 2007]. The First Action Plan for Food and Nutrition Policy. Available: http://www.euro.who.int/Document/E72199.pdf. [Google Scholar]
- WHO Regional Office for Europe. Copenhagen: World Health Organization; 2002. [accessed 27 March 2007]. European Strategy for Tobacco Control. Available: http://www.euro.who.int/Document/E77976.pdf. [Google Scholar]
- WHO Regional Office for Europe. Development of Environment and Health Indicators for European Union Countries: Results of a Pilot Study. 2004a. [accessed 6 December 2006]. Available: http://www.euro.who.int/document/E85061.pdf.
- WHO Regional Office for Europe. Fourth Ministerial Conference on Environment and Health; Budapest, Hungary. 23–25 June 2004; 2004b. [accessed 6 December 2006]. Declaration. Available: http://www.euro.who.int/document/e83335.pdf. [Google Scholar]
- WHO Regional Office for Europe. Protocol on Water and Health to the 1992 Convention on Protection and Use of Transboundary Waters and International Lakes. 2004c. [accessed 6 December 2004]. Available: http://www.euro.who.int/watsan/waterprotocol/20030523_1.
- WHO Regional Office for Europe. Copenhagen: World Health Organization; 2005. [accessed 30 July 2007]. Children’s Health and Environment. Developing Action Plans. Available: http://www.euro.who.int/document/E86888.pdf. [Google Scholar]