Abstract
The study purpose was to examine dissociation in body therapy for women receiving psychotherapy for childhood sexual abuse. An initial intervention study provided an opportunity to examine dissociation; the sample of 24 women received eight, one-hour body therapy sessions. The Dissociative Experiences Scale served as the predictor variable, and the outcome measures reflected psychological and physical health, and body connection. Repeated measures analysis of variance was used to examine dissociation reduction across time. Pearson correlations were used to describe associations between the relative change in dissociation and outcomes. The results demonstrated that the greatest change was the reduction of dissociation; there was an incremental effect across time and a strong association between change in dissociation and health outcomes. High dissociation at baseline (moderate levels) predicted positive outcomes. The results demonstrated the importance of moderate dissociation as an indicator of distress, and the central role of dissociation reduction in health and healing.
Keywords: Massage, Dissociation, Intervention Studies, Therapy, Child Abuse
INTRODUCTION
Study overview and aim
Dissociation can be a useful protection from the pain of inescapable childhood abuse, however it may become a liability later in life—it is associated with the psychological and physical distress in post traumatic stress disorder (PTSD)1, affect dysregulation and somatization2, problems with gastrointestinal health3, and appears to predict future dissociative experiences4 (for definitions see Table 1). A primary characteristic of dissociation is the fragmentation of consciousness; thus the experience of dissociation involves a sense of separation from self. Sexual symptoms and dysfunction, also common sequels of sexual abuse5, are thought to be related to dissociation from the body6. Clinical experts in the field emphasize the importance of reconnection with the self in healing from child sexual abuse — this involves recognizing, understanding and reducing dissociation7,8,9.
Table 1. Definition of Terms.
| Terms | Definition |
|---|---|
| Dissociative experiences | Life experiences that involve an aspect of dissociation. |
| Depersonalization/Derealization | Involves the feeling of separation or detachment; jointly defined as a “sensation of unreality concerning oneself, parts of oneself, or one’s environment27 ” |
| Amnesia | The failure to recall specific events or generalized time periods - in the past, and may include present time. |
| Pathological dissociation | Refers to a dissociative state that fits the diagnostic criteria for a dissociation disorder in the American Psychiatric Association’s Diagnostic Manual. Dissociative states are defined as a “disruption in the usually integrated functions of consciousness, memory, identity, or perception.” |
| Depersonalization Disorder | A dissociation disorder that fits the diagnositic criteria of depersonalization. |
| Dissociation Identity Disorder | A dissociation disorder involving fragmentation of identity (aka ‘multiple personality disorder’). |
| Moderate dissociation | Dissociative experiences that would lie on the continuum between ‘normal’ and ‘severe;’ typically involving symptoms of depersonalization/derealization; moderate dissociation is not be so severe as to fit diagnostic criteria for a dissociation disorder. |
| Severe dissociation | Dissociative experiences that involve fragmentation of identity, memory, and/or perception - and are associated with pathology. |
| Taxon membership | In an ordered group or category - a taxonomy. |
| Post Traumatic Stress Disorder (PTSD) | An anxiety disorder caused by a terrifying event in which physical harm occurred or was threatened. |
| Dissociative Experiences Scale (DES) | Used as a screening instrument for dissociation disorders. For more information and reference, see ‘Predictor variable’ in Methods section. |
| Child Sexual Abuse | Sexual contact or interaction between a child and an adult (or an older child in position of responsibility or power) that involves the child being used for stimulation of the perpetrator. |
To date there have been few intervention studies that either measure or examine the changes in dissociation associated with psychological care for childhood sexual abuse. The role of dissociation reduction on health outcomes in sexual abuse recovery in adults has rarely been explored. The lack of study in this area is surprising given that research demonstrates that dissociation serves as a mediator of psychological health in children with sexual abuse histories10, that dissociation is prevalent among adult sexual abuse survivors11,12, and that dissociation is recognized as a mental health problem in psychotherapeutic recovery from childhood sexual abuse7,8,13.
This is a study of dissociation in body therapy during sexual abuse recovery. The analysis originated from an intervention study examining two body therapy approaches, massage and a body-oriented therapy, as an adjunctive treatment for women in psychotherapy. Massage is a form of bodywork that involves manipulation of muscle and soft tissue to facilitate tension release. Body-oriented therapy is a form of body-psychotherapy that involves the combination of hands-on bodywork with a focus on body awareness and the emotional processing of psychotherapy. The primary aim of the original study was to examine the efficacy of body-oriented therapy with massage therapy as the comparison control. The hypothesis that body-oriented therapy would result in greater reduction in health outcomes compared to the control was not substantiated. Rather, the results indicated that both groups experienced significant change on all outcomes across time; the findings are reported in a previous publication14. The purpose of the present study was to describe dissociation with respect to body therapy in sexual abuse recovery, specifically a study of nonpathological dissociation (i.e., among participants without dissociation disorders). There were two hypotheses. The first hypothesis predicted that there would be an incremental decrease in dissociation over the course of the body therapy interventions. The second hypothesis posited that dissociation reduction would be positively associated with change in psychological well-being, physical well-being, and body connection across time.
Background: Dissociation conceptualization and measurement
The measurement of dissociation in research typically involves quantifying the frequency of dissociative experiences using the Dissociative Experiences Scale (DES)15. Designed to measure dissociation on a continuum, the DES includes items associated with the full range of dissociative experiences from normal to pathological. Factor analysis indicates that the items represent three sets of dissociative experiences: absorption (normal range), depersonalization/derealization (moderate range), and amnesia (severe range) (for definitions see Table 1). The DES score, however, is a sum of all possible dissociation experiences representing the frequency of overall dissociative experiences.
The need for increased specificity to identify the prevalence of particular aspects of dissociative experiences and their mental health correlates has led to the use of item subsets from the DES to examine, for example, depersonalization among clinical populations16 (16) and severe dissociation in the general population17. A newer instrument, the DES-T, was developed to include only items from the DES that are characteristic of dissociative disorders, thereby distinguishing pathological types of dissociation (i.e. taxon membership – for definition see Table 1) from non-pathological dissociation18; contributing to a typological model for conceptualizing dissociation as an alternative to the continuum model19. Increased specificity in dissociation research, from the perspectives of both conceptual models, has clarified the importance of distinguishing among dissociative symptoms as well as the need for better understanding of the health implications of dissociative experience. For example, in a study of taxon membership representing pathological dissociation, taxon membership was found in only 3.3 percent of the general population17. In contrast, a study of depersonalization in the general population (N = 1008) found 23 percent of the respondents reporting symptoms of depersonalization in the preceding year20. Importantly, research findings suggest that symptoms of moderate dissociation, specifically depersonalization, may be linked to emotional stress and associated with physical symptoms of chronic pain in the general population20, and emotional maltreatment in childhood – including sexual abuse - among a clinical population16.
Dissociation as a sequela of childhood sexual abuse has been primarily studied among a psychiatric population. There is substantial evidence that sexual abuse is associated with “dissociation identity disorder,” the least common and most extreme dissociative experience19,21. Dissociative experiences that include “moderate” symptomatology such as symptoms of depersonalization are common in many clinical populations, however we know little about the association between moderate dissociation and psychological and physical health among sexual abuse survivors. A recent study, however, found that both pathological (taxon membership) dissociation and moderate (non-taxon membership) dissociation were associated with comparable levels of psychological distress among women with a childhood sexual abuse history. Although there were distinctly different patterns of psychological distress between the severe and moderate dissociators, both groups had significantly greater psychological distress compared to normal (low) dissociators22. That is, elevated dissociation—whether in the moderate or severe range of dissociative experiences—was associated with significant psychological distress in this population.
Dissociation reduction, body therapy, and sexual abuse recovery
The reduction of dissociation is considered integral to sexual abuse recovery among clinicians working with adult sexual abuse survivors within the combined areas of bodywork and body-psychotherapy9,23,24,25. The emphasis on dissociation reduction among therapists who work with the body in trauma recovery is most likely due to the focus on body awareness in these approaches. The focus on body awareness in conjunction with touch (i.e., bodywork) provides a unique perspective on dissociation that highlights the experience of dissociation in the body as a barrier to emotional awareness and integration of aspects of the self – and is, therefore, particularly useful as a complement to psychotherapy for adults in trauma recovery.
The lack of sensory and emotional awareness – and the underlying processes of inner connection to the self - are common among women with a history of severe trauma8; and is referred to in this paper as a lack of “body connection.” Women typically seek body therapy in sexual abuse recovery to increase their sense of body connection –in other words, to increase the sense of continuity and integration between self and bodily experience14,26. For example, women who seek body therapy in trauma recovery often report minimal purposeful attention to bodily experience, which appears to be associated with a lack of sensory (physical) and emotional awareness. A common self-description includes being “cut off from the neck down” or “a walking head,” indicating that sense-of-self does not incorporate bodily experience. The feeling of being ‘cut-off’ from the body can be a distressing experience in daily life that is typically associated with the trigger of unresolved and negative emotional experiences stemming from abuse; the experience of being ‘cut-off,’ or separated, is a symptom of depersonalization27. Examples of bodywork and body-psychotherapy therapy techniques used to increase body connection and reduce dissociation include: increasing the capacity to be present (i.e., maintaining awareness of inner experience without dissociating) during bodywork; developing body literacy – the ability to identify and articulate bodily experience; teaching inner body awareness approaches to facilitate access to somatic and emotional awareness; and verbal processing of session experiences to facilitate cognitive understanding, acceptance and insight. Thus, these techniques are thought to facilitate increased body awareness as a primary strategy for dissociation reduction, involving the connection between sensory, emotional, and cognitive awareness9,14,23,24,25,28,29,30.
Anecdotal9,23,31 and experimental evidence14 suggests that body therapy (therapy that specifically involves hands-on bodywork) is associated with reductions in dissociation among adult survivors of childhood sexual abuse. However, with the exception of the author’s two prior studies14,32, measures of dissociation have not been included in body therapy research. Thus we know little about the effect of body therapy on dissociation, and nothing about the relationship between dissociation reduction and health outcomes in body therapy. This study is designed to examine dissociation in body therapy during sexual abuse recovery, a first step in this area of inquiry.
METHODS
Design
This research was part of a larger study to test the efficacy of body-oriented therapy as an adjunct to psychotherapy in comparison to a standardized massage, and to explore the perceived influence of these interventions on abuse recovery14. All research procedures were reviewed and approved by the University IRB. A two-group repeated measures design was employed. Participants were randomly assigned to receive eight one-hour sessions of either body-oriented or massage therapy from one of four research clinicians. Measures were administered at six time points: at baseline, after 2 weeks of sessions, after 4 weeks of sessions, one week post intervention, and at 1 and 3 months follow-up. For this study, the two groups (massage and body-oriented therapy) were combined to examine and describe dissociation in body therapy during psychotherapeutic treatment for abuse recovery.
Recruitment and selection
Women currently in psychotherapy for recovery from childhood sexual abuse were recruited for study participation through flyers posted at a university in the northwest, in mental health clinics, as well as from friendship networks and psychotherapy referrals. Prospective participants were screened during the initial phone contact. Study inclusion required that participants be female, over the age of 25, engaged in an established psychotherapeutic relationship of two months minimum, have a minimum of two years of psychotherapy, and agree to not seek (non-study) bodywork treatment during study involvement. Study exclusion included transition in psychotropic medication during the past eight weeks, addiction to alcohol or drugs, current abusive relationship, hospitalization for psychological care within 12 months, diagnosis or medication for psychosis, pregnant by more than three months, and prior body-oriented therapy (more than 20 sessions). Participants were told that at the initial appointment there would be additional screening for severe dissociation and that diagnosis of a dissociation disorder would not be an appropriate fit for the study. Participants were screened for severe dissociation with the DES-T.
Enrollment and sample characteristics
During the enrollment period, fifty women expressed interest in study participation; recruitment was completed in three months. Twenty-four individuals were not eligible based on screening criteria. Of the twenty-six women eligible for study participation, one never enrolled in the study and one withdrew from the study after two sessions (massage group) because she felt the experience too stimulating at this point in her recovery. The final N was 24.
The study participants ranged in age from 26–56, with a median age of 41. Participants attended one-hour of psychotherapy per week; the psychotherapeutic approaches varied but can be generally categorized as psychodynamic in orientation. The racial/ethnic identity of the participants included 1 Native American, 1 Hispanic, 2 African Americans, and 20 Caucasians. Overall, they endured extensive childhood abuse – involving rape and ongoing abuse over many childhood years, were highly educated, and had widely disparate household incomes. Detailed background characteristics are provided in Table 2.
Table 2. Background Characteristics of Study Participants.
| Characteristics | |
|---|---|
| Age, mean years (range) | 41 (26–56) |
| Psychotherapy in years, mean (range) | 6 (2–15) |
| Racial/ethnic identity | N |
| Caucasian | 20 |
| African American | 2 |
| Native American | 1 |
| Hispanic | 1 |
| Income (range) | $4,000–$200,000 |
| Less than $30,000 | 8 |
| Between $30–$50,000 | 11 |
| Over $50,000 | 5 |
| Education | |
| Completed BA | 18 |
| Completed graduate program | 6 |
| Current graduate student | 5 |
| Abuse History | |
| Childhood sexual abuse over multiple years | 18 |
| C.S.A. multiple years, from multiple perpetrators | 9 |
| Physically abused by parent(s) | 11 |
| Subsequent date rape in early adulthood | 8 |
Training and Fidelity
Four female bodywork therapists were employed as research clinicians for this study. All were licensed to practice massage therapy in the state of Washington, had at least 5 years experience as licensed practitioners, and had experience working with sexual trauma. Two clinicians had, in addition, graduate education in psychology; these clinicians provided the body-oriented therapy intervention. Training and supervision was provided by the investigator. Training involved hands-on instruction in research procedures and protocols and a training manual for each of the bodywork approaches. Evaluation of intervention compliance and quality involved review of audiotaped sessions and process evaluation forms filled out by clinicians at the end of each session. The investigator provided the clinicians with weekly individual feedback, and met regularly with the body-oriented therapists and massage therapists to discuss their clinical and research concerns and experiences.
Intervention procedures
The massage and body-oriented therapy interventions were quite distinct. The similarities between the interventions were that a) sessions were 1 hour in duration, b) massage in both interventions used the same hands-on protocol, c) the sessions were done over clothes, and d) a key protocol element involved ‘sense of safety.’
Sense of safety refers to the participant’s physical and emotional comfort. It was attended to throughout the sessions with use of frequent check-ins (i.e., asking client about the acceptability of touch) to assess comfort level and, if necessary, modification of the protocol to ensure participant comfort. The check-in provided the massage therapist with feedback regarding her level of tactile pressure, the acceptability of touch in a particular area of the body, general physical comfort, and room temperature. The check-in was also used to access information that might indicate participant emotional discomfort (i.e., dissociation, fear, aversion to touch).
Brief descriptions of the key elements of both intervention protocols are described below. Further intervention details can be found in the Price14 article.
Massage group
The massage group received a standardized protocol similar to that used in research at the Touch Therapy Institute33,34. The protocol had two primary elements: sense of safety and massage. Massage techniques were used to deliver a full-body massage at each session – covering the head and neck, arms, legs, feet and back - to facilitate relaxation.
Body-oriented therapy group
The body-oriented therapy protocol was separated into three distinct stages, each aimed at incrementally increasing awareness of inner body experience. The first stage (Sessions 1 and 2) involved massage with body literacy - the practice of identifying and articulating what is noticed in the body and the best words to describe the inner experience and sensations during massage. The second stage ( Sessions 3 and 4) involved 10 minutes of massage followed by and body awareness exercises aimed at increasing inner body awareness through attention to breath, the use of intention to facilitate relaxation, and the use of mindful presence towards inner body experience. The third stage, (Sessions 4–8) involved 10 minutes of massage followed by ‘Delving’ - a guided practice of mindful attention to inner body awareness derived from Focusing35. All sessions involved a seated intake to gather participant responses to questions regarding her emotional and physical well-being that served to guide the therapeutic focus of the session. All sessions also involved a seated ‘session review,’ during which the therapist facilitated a verbal overview of session highlights and the development of a take-home body awareness practice, to promote integration of the therapeutic elements in the session.
Measurement
Dissociation was examined for change across time, association with outcome variables, and as a predictor of health outcomes using the Dissociative Experiences Scale. Measures were scored such that high values reflected higher levels of the construct. Validity and reliability coefficients reported below are derived from other, larger samples.
The outcome measures reflected three key constructs—psychological well-being, physical well-being, and body connection—to serve the aims of this study. Psychological well-being was an assessment of intrapersonal and interpersonal health, both in relation to general measures of psychological health (Brief Symptom Inventory), and in relation to trauma history (Crime-Related Post Traumatic Stress Disorder Scale). Physical well-being was an assessment of physical symptoms of discomfort (Medical Symptom Checklist). Body Connection was an assessment of body awareness, body association, and body investment (Scale of Body Awareness; Body Investment Scale). Measures were scored such that high values reflected higher levels of the construct.Validity and reliability coefficients reported below are derived from other, larger samples.
Predictor variable
Dissociation
Dissociative Experiences Scale (DES) contains 28 items and measures the frequency of dissociative experiences, from 0% = never to 100% = always, on an 11-point scale. It is used to determine the contribution of dissociation to psychiatric disorders and as a screening instrument for dissociative disorders. The coefficient alphas for internal consistency ranged from .83–.93, and the test-retest reliability was .79 with a 6–8 week test-retest interval; reliability and validity of the scale are well documented15. Items determined by factor analysis to represent depersonalization were used in the depersonalization score16.
The DES-T consists of 8 items from the DES that represent severe or “pathological” dissociation and may indicate a dissociation disorder. The scale includes a cut-off score indication of severe dissociation18.
Outcome variables
Psychological Well-Being
Brief Symptoms Inventory (BSI) contains 53 items for 9 subscales (α = .71–.85) measuring symptoms of distress, the intensity of those symptoms, and the overall level of distress. The level of distress is rated on a 5-point scale from 0 meaning “not at all” to 4 meaning “extremely.” This study reported the “global severity index,” used to indicate overall level of psychological distress. Test-retest reliability is .68–.91 with a 2-week interval; the reliability and validity of the scale are well documented36.
Crime-Related Post Traumatic Stress Disorder Scale (PTSD) is based on 28 selected items from the BIS36 and the SCL-9037 that indicate post-traumatic stress disorder. Crime-related victimization includes sexual assault from anytime in life, including childhood. With excellent internal consistency (α = .93), the scale effectively discriminates between individuals with and without crime-related PTSD (F = 98.2, p < .001)38.
Physical Symptoms
Medical Symptoms Checklist measures the number and frequency of 26 common physical symptoms, and the discomfort associated with the symptoms. Number and frequency of symptoms is rated from 0 (never) to 8 (constant) on a 2-point scale. The degree of discomfort of each symptom is rated on an 11-point scale (0 = none to 10 = extreme). The scale has been used in other mind-body studies39,40. Thus, the scale was used to compute two related but different measures of physical symptoms: total number of endorsed medical symptoms (#MS) and total symptom discomfort (MSD).
Body Connection
The Scale of Body Connection has two distinct, uncorrelated dimensions measuring Body Awareness and Bodily Association. A 5-point scale, items range from 1 meaning “not at all” to 5 meaning “all of the time,” includes 12 items to measure body awareness (α = .85) and 8 items to measure body association (α = .79). Body awareness measures conscious attention to sensory cues indicating bodily state (for example tension, nervousness, peacefulness). Body association measures connection to (vs separation from) body, including emotional connection (for example difficulty paying attention to emotions). Developed for this study, the scale has demonstrated construct validity through exploratory and confirmatory factor analysis41.
The Body Investment Scale (BIS) is a 24-item, 5-point scale assesses attitudinal relationship to the body. It consists of four factors: (a) attitude and feeling (α = .75), (b) body care (α = .86), (c) body protection (α = .92), and (d) comfort in touch (α = .85)42.
ANALYSIS
Preliminary analysis
Preliminary analysis included sample baseline descriptive statistics for dissociation, and examination of the zero-order correlations between dissociation and key outcome variables.
Main analysis
Due to the similarity between groups on change across time in the original study, analyses were conducted combining individuals in both interventions (massage and body-oriented therapy). The first hypothesis stated that dissociation would reduce over the course of the interventions, with an incremental effect over time. For the analysis, dissociation reductions were examined across time using repeated measures analysis of variance (ANOVA). Trend analysis was used to describe the pattern of change for both interventions across time.
The second hypothesis stated that dissociation reduction would be positively associated with change in psychological well-being, physical well-being and body connection across time. The analysis involved two steps. First, analyses were conducted to describe the change in dissociation experiences relative to change in psychological wellbeing, physical well-being, and body connection across time using repeated measures ANOVA. Second, Pearson correlations were used to describe associations between the relative change in dissociation and in psychological well-being, physical well-being and body connection across time using change scores. Change scores were calculated as the difference between means at any two time-points (for example, DES mean at Time 2–DES mean at Time 1 = DES 1–2). Correlations between change scores, measuring relative amount of change at each time point (1–2, 1–3, 1–4, 1–5, 1–6) were then calculated. Given the small sample size, nonparametric (Spearman) correlations were also examined. These tests were comparable to the Pearson correlations, and thus Pearson correlations are reported here.
RESULTS
Baseline dissociation
Dissociation was elevated with a mean score of 12.2, compared to an average range of 4.4–7.8 for the general public15. Twelve of the participants had scores reflecting moderate dissociation (ranging from 13-27); on the depersonalization sub-score, 14 participants had scores that reflected frequent experiences of depersonalization (range from 10–30). The overall psychological and physical symptom profile at baseline indicated generally high levels of psychological and physical symptoms among participants14.
Preliminary findings
Prior to investigating the change in dissociation, the zero-order correlations between dissociation and key outcome variables were examined. Dissociation was highly and positively associated with psychological well-being measures (range between .64–.71), moderately and positively associated with physical well-being (range from .40–.50), and highly and negatively associated with body connection (range -.52 – -.63). That is, individuals who had elevated dissociation experiences at baseline also experienced elevated psychological and physical distress, and less body connection at baseline.
Change in dissociation across time
As predicted, dissociation decreased steadily across time during the massage and body-oriented therapy interventions (Table 3). The incremental decreases across time for both interventions were significant (F = 33, p < .001).
Table 3. Dissociation Mean Scores Across Time.
| Baseline | Time 2
(2 weeks) |
Time 3
(4 weeks) |
Time 4
Post-Intervention |
Time 5
1 month follow-up |
Time 6
3 month follow-up |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | (SD) | Mean | (SD) | Mean | (SD) | Mean | (SD) | Mean | (SD) | Mean | (SD) | |
| Dissociation (DES) | ||||||||||||
| (N=23) | 12.2 | (7.1) | 10.5 | (7.4) | 8.4 | (6.8) | 6.7 | (5.1) | 5.6 | (5.1) | 4.5 | (4.4) |
Association between change in dissociation and key outcome variables
The results demonstrated that, overall, dissociation reduction was positively associated with psychological well-being, physical well-being, and body connection across time for both intervention groups (Figures 1 and 2). Notably, the steepest slope among all outcome variables is in dissociation.
Figure 1.
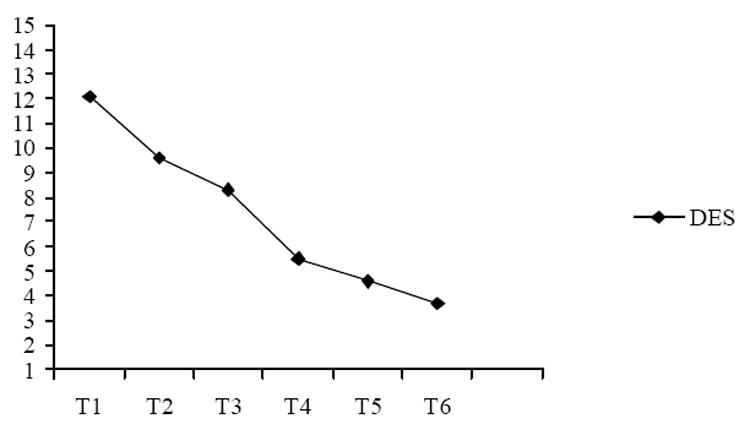
Change in dissociation (N = 24).
Figure 2.
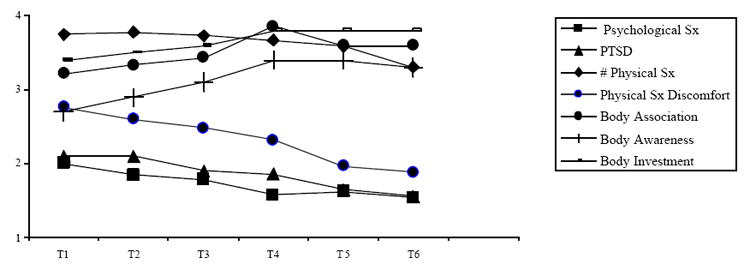
Change in health outcomes (N = 24).
Note: Scores in Figure 1 and Figure 2 were recalculated so all are on 5 -point scale.
T1=baseline, T4=post-intervention, T5=1 month post intervention, T6=3 month post-intervention
Correlations among change scores
To describe the role of dissociation in body therapy, Pearson correlations were used to explore the covariation in change in dissociation and outcome variables. All correlations were based on combined groups as a result of the similarity between groups on change across time in the original study. Due to the small sample size, the cut-off for significance tests was set at p < .10. The pattern of correlations for change scores is shown in Tables 4–6. The change score is the difference between means at any two time-points (for example, DES1–2 is the change in DES between time 1 and time 2). The table correlations are displayed on the diagonal because all change scores were calculated from baseline to each subsequent time point (for example, 1–2, 1–3, etc); change on intermediate time-points were not calculated.
Table 4. Change Score Correlations Between Dissociation and Psychological Well-Being (N=24).
| Change in Measure | BSI 1–2 | BSI 1–3 | BSI 1–4 | BSI 1–5 | BSI 1–6 | PTSD 1–2 | PTSD 1–3 | PTSD 1–4 | PTSD 1–5 | PTSD 1–6 |
|---|---|---|---|---|---|---|---|---|---|---|
| DES 1 – 2 | .11 | .33◆ | ||||||||
| DES 1 – 3 | .34◆ | .36* | ||||||||
| DES 1 – 4 | .30◆ | .33◆ | ||||||||
| DES 1 – 5 | .37* | .35◆ | ||||||||
| DES 1 – 6 | .32◆ | .40* |
p < .10
p < .05
p < .01
Note. DES = Dissociative Experiences Scale, measuring frequency of dissociative experiences, BSI = Brief Symptoms Inventory measuring frequency of psychological symptoms, CR-PTSD = Crime-Related Post Traumatic Stress Disorder, measuring frequency of PTSD indicators. The “change in measure” is the change score, the difference between means from baseline (time 1) to each subsequent measurement point (time 2–6).
Table 6. Change Score Correlations Between Dissociation and Body Connection (N=24).
| Change in Measure | BA 1–2 | BA 1–3 | BA 1–4 | BA 1–5 | BA 1–6 |
|---|---|---|---|---|---|
| DES 1–2 | -.26◆ | ||||
| DES 1–3 | -.61*** | ||||
| DES 1–4 | -.80*** | ||||
| DES 1–5 | -.72*** | ||||
| DES 1–6 | -.63*** | ||||
| Change in Measure | AB 1–2 | AB 1–3 | AB 1–4 | AB 1–5 | AB 1–6 |
|
| |||||
| DES 1–2 | -.38* | ||||
| DES 1–3 | -.56*** | ||||
| DES 1–4 | -.62*** | ||||
| DES 1–5 | -.62*** | ||||
| DES 1–6 | -.57*** | ||||
| Change in Measure | BIS 1–2 | BIS 1–3 | BIS 1–4 | BIS 1–5 | BIS 1–6 |
|
| |||||
| DES 1–2 | .14 | ||||
| DES 1–3 | -.44* | ||||
| DES 1–4 | -.46** | ||||
| DES 1–5 | -.52** | ||||
| DES 1–6 | -.40* | ||||
p < .10
p < .05
p < .01
p < .001
Note. DES = Dissociative Experiences Scale, measuring frequency of dissociation experiences; BA = Body Awareness, measuring level of body awareness; AB = Body Association, measuring level of connection to body; BIS = body investment, measuring degree of, and comfort with care, touch, feeling and protection towards body.
The results demonstrated that reduction in dissociation was moderately associated with increased psychological well-being (Table 4), moderate to highly associated with increased physical well-being (Table 5), and highly associated with increased body connection (Table 6). That is, individuals who experienced a reduction in dissociation between any two-time points, also experienced positive change on outcome variables between the same time points. These results confirmed the hypothesis that dissociation reduction was positively associated with change in psychological well-being, physical well-being and body connection across time.
Table 5. Change Score Correlations Between Dissociation and Physical Well-Being (N=24).
| Change in Measure | #MS 1–2 | #MS 1–3 | #MS 1–4 | #MS 1–5 | #MS 1–6 |
|---|---|---|---|---|---|
| DES 1–2 | .46** | ||||
| DES 1–3 | .46** | ||||
| DES 1–4 | .72** | ||||
| DES 1–5 | .49** | ||||
| DES 1–6 | .33◆ | ||||
| Change in Measure | MSD | MSD | MSD | MSD | MSD |
|
| |||||
| DES 1–2 | .31◆ | ||||
| DES 1–3 | .42* | ||||
| DES 1–4 | .72*** | ||||
| DES 1–5 | .67*** | ||||
| DES 1–6 | .58** | ||||
p < .10
p < .05
p < .01
p < .001
Note. DES = Dissociative Experiences Scale, measuring frequency of dissociative experiences, #MS = number of endorsed medical symptoms; MSD = medical symptom discomfort.
The results indicated that dissociation reduction and health outcomes were positively associated at each time point. This finding stimulated a couple of questions related to the influence of dissociation experience on change in health outcomes. Does frequency of dissociation experiences at baseline influence change in health outcomes across time? If so, is there a difference between change in outcomes between those with moderate dissociation and those with lower baseline dissociation? To explore these questions, an additional analysis was conducted examining baseline dissociative experiences in relationship to change on health outcomes across time.
Influence of baseline DES on change in variable outcome
To explore the role of baseline dissociation on change in outcomes, the scores were separated into a dichotomous variable representing moderate dissociation vs low dissociation at baseline. The cut-off for moderate dissociation was a score of 13 on the DES; DES scores above 13 are associated with depersonalization43. The change from pre-intervention (baseline) to post-intervention (T4) was compared between participants with moderate or low dissociation at baseline using ANOVA. The findings indicate a significant difference, for both groups, between moderate and low baseline dissociation on change from baseline to post-intervention on psychological symptoms, PTSD, number of physical symptoms, and body awareness (Table 7). That is, individuals with moderate dissociation experiences at baseline showed greater change on these outcome variables than individuals with low baseline dissociation. There were no significant dissociation group effects on physical symptom discomfort, body association or body investment. That is, there was no difference pre- to post-intervention on these outcomes for individuals with moderate compared to low dissociation. These findings indicate that participants with higher dissociation experiences prior to study participation had the greatest decrease in psychological symptoms, PTSD, number of physical symptoms, and the greatest increase in body awareness across time.
Table 7. Repeated Measures Analysis: Moderate versus Low Dissociation Baseline Effect on Pre to Post Outcomes.
| Outcome Measure | df | ms | f | p |
|---|---|---|---|---|
| Psych symptoms (BSI) | 1 | 1.0 | 6.4 | .02 |
| PTSD | 1 | 1.4 | 8.6 | .02 |
| # Medical symptoms | 1 | 97 | 14.0 | .00 |
| Medical symptom discomfort | 1 | 967 | 1.8 | .19 |
| Body awareness | 1 | 5.3 | 18.0 | .00 |
| Body association | 1 | 1.1 | 2.0 | .18 |
| Body investment | 1 | .24 | 2.1 | .17 |
DISCUSSION
The study results indicated, as hypothesized, an incremental decrease in dissociation across time for both the body therapy interventions, suggesting that dissociation reduction in body therapy as an adjunct to psychotherapy is an unfolding process that builds on itself step by step. Participants each had a minimum of 2 years in psychotherapy at the outset of study, and yet significant change in dissociation experiences occurred during the course of the intervention and the follow-up period. The overall similar rate of change for both groups suggests that dissociation responds to a variety of bodywork approaches; in this study these approaches included a standardized massage, massage with body literacy, body awareness work, and delving – a practice of inner body mindfulness.
The hypothesis that dissociation reduction would be positively associated with change on all outcome variables was upheld, suggesting a link between dissociation reduction and positive health outcomes with this population. This link was supported by correlation results demonstrating that change between any two points on dissociation was associated with change between the same two points on all outcome variables across time for participants in both intervention groups.
The results also indicated that dissociation at baseline does not interfere with the ability to change. Participants in both groups with higher dissociation experiences prior to study participation had the greatest decrease in psychological symptoms, PTSD, physical symptoms, and the greatest increase in body awareness across time. Twelve (50%) of the participants in this study had baseline dissociation in the moderate range with frequent symptoms of depersonalization; this dropped to 4 at post-intervention and only 1 at three-month follow-up. Thus, the significantly greater decrease on outcomes for participants with moderate compared to low dissociation at baseline suggests that bodywork improves health outcomes among individuals with moderate dissociation; and points to the importance of recognizing moderate dissociation as a psychological indicator of psychological and physical distress22.
Change in physical symptom discomfort, body association and body investment, unlike the other outcome variables, was not linked to baseline dissociation. Likewise, participants with moderate baseline dissociation did not experience significantly greater decreases on these variables across time compared to those with lower dissociation at baseline. The reason for this distinctly different pattern in relationship to baseline dissociation is unclear. However, one possible explanation involves the impact of receiving touch through bodywork, and a focus on the body among participants who were engaged in the study primarily to seek increased body connection14. Both body association and body investment represent the emotional connection and cognitive appraisal of the relationship to bodily self. It is possible that, in response to a body therapy intervention, change in these areas is equally likely to happen for individuals in this population regardless of baseline dissociation. Decrease in physical symptom discomfort may be associated with these aspects of increased body connection, and therefore also unlinked from baseline dissociation.
The importance of dissociation reduction in this population is not surprising given its prevalence and the role it plays to protect a survivor from the pain of her abuse. The therapeutic work of sexual abuse recovery is intimately related to the work of integration of psyche and soma that are frequently fragmented through the dissociative process of living with trauma. Reassociation with the body through body therapy may be a key to unlocking patterns of dissociation so common in this population, most likely explained by the process of (re)connection with a core sense of self through increased awareness of, and identification with bodily experience, as demonstrated by the strong association between increased body connection and dissociation reduction.
There are study limitations to be considered. The small sample size limits generalization of the study findings. Also, this study examined body therapy as an adjunct to psychotherapy – and lacked a control group - both limitations of the study design that restrict result interpretation. Despite these limitations, this study is an important first step in the study of dissociation and the role of body therapy for women in sexual abuse recovery. Future research in this area will ideally include larger samples to capture a broader range of dissociation at baseline, allowing for study of dissociation reduction in body therapy with individuals who have more frequent and severe dissociation experiences. Needed also are study designs that test dissociation reduction as a mediator of health outcomes in body therapy, and further explore the association between body connection and dissociation reduction to elucidate possible mechanisms underlying this association. To do so, it is important that there be further exploration of the measurement and conceptualization of dissociation experiences, specifically the relationship of body connection as a dimension of dissociation experience. Meanwhile, the general Dissociative Experiences Scale needs to be used judiciously in intervention research.
In summary, the study results indicate that dissociation follows a declining pattern for women in body therapy during sexual abuse recovery, and supports future research examining dissociation reduction as a mediator of health outcomes in body therapy. The positive association between dissociation reduction and health outcomes in this sample—in which there were symptoms of moderate dissociation and depersonalization with no indication of dissociative disorder—suggests that depersonalization experiences may be associated with important health concerns and barriers to sexual abuse recovery for this population. Re-association with the bodily self may be a key to healing problematic dissociation and improving mental and physical health in this population. This is a unique perspective offered by body therapy in trauma recovery, an untapped resource for the study of dissociation—its presentation and its treatment.
Acknowledgments
In grateful acknowledgement of my mentor Elaine Thompson, PhD who is faculty at the University of Washington School of Nursing. In appreciation of funding support from the National Center for Complementary and Alternative Medicine at National Institutes of Health (F31 AT01053), the McLaws Nursing Research Fund from the University of Washington School of Nursing, UW School of Nursing Curriculum Training Grant in Complementary Therapies (I R25 AT01240), and the UW School of Nursing Department of Psychosocial and Community Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Feeny N, Zoellner L, Gitzgibbons L, et al. Exploring the roles of emotional numbing, depression, and dissociation in PTSD. Journal of Traumatic Stress. 2000;13(3):489–98. doi: 10.1023/A:1007789409330. [DOI] [PubMed] [Google Scholar]
- 2.van der Kolk B, Pelcovitz D, Roth S, et al. Dissociation, somatization, and affect dysregulation: The complexity of adaptation to trauma. American Journal of Psychiatry. 1996;153(7):163–170. doi: 10.1176/ajp.153.7.83. [DOI] [PubMed] [Google Scholar]
- 3.Salmon P, Skaife K, Rhodes J. Abuse, dissociation, and somatization in irritable bowel syndrome: towards an explanatory model. Journal of Behavioral Medicine. 2003;26(1):1–18. doi: 10.1023/a:1021718304633. [DOI] [PubMed] [Google Scholar]
- 4.Bremner JD, Brett E. Trauma-related dissociative states and long-term psychopathology in posttraumatic stress disorder. Journal of Traumatic Stress. 1997;10(1):37–49. doi: 10.1023/a:1024804312978. [DOI] [PubMed] [Google Scholar]
- 5.Briere J, Elliott D. Prevalence and psychological sequelae of self-reported childhood physical and sexual abuse in a general population sample of men and women. Child Abuse and Neglect. 2003;27:1205–1222. doi: 10.1016/j.chiabu.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 6.Maltz W, Holman B. Incest and sexuality: A guide to understanding and healing. Lexington MA: Lexington Books; 1987. [Google Scholar]
- 7.Briere J. Therapy for adults molested as children: Beyond survival. New York NY: Springer Publishers; 1996. [Google Scholar]
- 8.Herman J. Trauma and recovery. NY, NY: HarperCollins Publishers; 1992. [Google Scholar]
- 9.Timms R, Connors P. Embodying healing: Integrating bodywork and psychotherapy in recovery from childhood sexual abuse. Orwell VT: The Safer Society Press; 1992. [Google Scholar]
- 10.Kiesel C, Lyons J. Dissociation as a mediator of psychopathology among sexually abused children and adolescents. The American Journal of Psychiatry. 2001;158(7):1034–9. doi: 10.1176/appi.ajp.158.7.1034. [DOI] [PubMed] [Google Scholar]
- 11.Briere J, Runtz M. Childhood sexual abuse: Long-term sequelae and implications for psychological assessment. Journal of Interpersonal Violence. 1993;8(3):312–330. [Google Scholar]
- 12.Neumann D, Houskamp B, Pollock V, et al. The long-term sequalae of childhood sexual abuse in women: A meta-analytic review. Child Maltreatment. 1997;1(1):6–16. [Google Scholar]
- 13.van der Kolk B, van der Hart O, Marmar C. Dissociation and information processing in Posttraumatic Stress Disorder. In: van der Kolk B, McFarlane C, Weisaeth L, editors. Traumatic Stress: The effects of overwhelming experience on mind, body and society. NY: Guilford Press; 1996. pp. 303–327. [Google Scholar]
- 14.Price C. Alternative therapies in health and medicine. 5. Vol. 11. 2005. Body-Oriented Therapy in recovery from childhood sexual abuse: An efficacy study; pp. 46–57. [PMC free article] [PubMed] [Google Scholar]
- 15.Carlson E, Putnam F. An update on the Dissociative Experiences Scale. Dissociation. 1993;6(1):16–27. [Google Scholar]
- 16.Simeon D, Guralnik O, Schmeidler J, et al. The role of childhood interpersonal trauma in depersonalization disorder. American Journal of Psychiatry. 2001;158(7):1027–1033. doi: 10.1176/appi.ajp.158.7.1027. [DOI] [PubMed] [Google Scholar]
- 17.Waller N, Ross C. The prevalence and biometric structure of pathological dissociation in the general population: Taxometric and behavior genetic findings. Journal of Abnormal Psychology. 1997;106(4):499–510. doi: 10.1037//0021-843x.106.4.499. [DOI] [PubMed] [Google Scholar]
- 18.Waller N, Putnam F, Carlson E. Types of dissociatiation and dissociative types: A taxometric analysis of dissociative experiences. Psychological Methods. 1996;1:300–321. [Google Scholar]
- 19.Putnam F, Guroff J, Silberman E, et al. The clinical phenomenology of multiple personality disorder: review of 100 recent cases. Journal of Clinical Psychiatry. 1986;147:285–293. [PubMed] [Google Scholar]
- 20.Aderibigbe Y, Bloch R, Walker W. Prevalence of depersonalization and derealizatio experiences in a rural population. Social Psychiatry Psychiatric Epidemiology. 2001;36(2):63–9. doi: 10.1007/s001270050291. [DOI] [PubMed] [Google Scholar]
- 21.Ross C, Miller S, Reagor P, et al. Structured interview data on 102 cases of multiple personality disorder from four centers. American Journal of Psychiatry. 1990;147:596–601. doi: 10.1176/ajp.147.5.596. [DOI] [PubMed] [Google Scholar]
- 22.Van Dien L. Dissertation Abstracts International: Section B: the Sciences and Engineering. 5B Vol. 62. US: University Microfilms International; 2001. Dissociation and long-term adaptation to childhood trauma: Dissociative ‘types’ and clinical syndromes. [Google Scholar]
- 23.Benjamin B. Massage and bodywork with survivors of abuse (Part V) Massage Therapy Journal. 1996;(Summer Issue) [Google Scholar]
- 24.Levine P. Waking the tiger: Healing trauma. CA: North Atlantic Books; 1997. [Google Scholar]
- 25.Ogden P, Minton K. Sensorimotor Psychotherapy: One method for processing traumatic memory. Traumatology. 2000;7(3) [Google Scholar]
- 26.Price C. Characteristics of women seeking bodywork as an adjunct to psychotherapy during recovery from childhood sexual abuse. Journal of Bodywork and Movement Therapies. 2004;8(1):35–42. [Google Scholar]
- 27.Sadock B, Sadock V, editors. Kaplan and Saddock’s comprehensive textbook of psychiatry. 7. Vol. 1. Philadelphia: Lippincott Williams and Wilkins; 2000. [Google Scholar]
- 28.Kurtz R. Body-Centered Psychotherapy: The Hakomi Method. Mendocino CA: LifeRythm; 1990. [Google Scholar]
- 29.Ford C. Compassionate touch. NY, NY: Simon and Schuster; 1993. [Google Scholar]
- 30.Aposhyan S. Body-Mind Psychotherapy: Principles, techniques, and practical applications. NY: Norton; 2004. [Google Scholar]
- 31.Ogden P. Hakomi Integrated Somatics: Hands-on psychotherapy. In: Caldwell C, editor. Getting in touch: The guide to new body-centered therapies. Wheaton IL: Quest; 1997. pp. 153–178. [Google Scholar]
- 32.Price C. Body-Oriented Therapy in sexual abuse recovery: A pilot-test comparison. Journal of Bodywork and Movement Therapies. 2006;10(1):58–64. [Google Scholar]
- 33.Field T, Grizzle N, Scafidi F, Schanberg S. Massage and relaxation therapies’ effects on depressed adolescent mothers. Adolescence. 1996;31(124):904–911. [PubMed] [Google Scholar]
- 34.Field T, Hernandez-Reif M, Hart S, et al. Effects of sexual abuse are lessened by massage therapy. Journal of Bodywork and Movement Therapies. 1997;1(2):65–69. [Google Scholar]
- 35.Gendlin E. Focusing. New York: Bantam; 1981. [Google Scholar]
- 36.Derogatis L. The Brief Symptom Inventory. National Computer Systems Inc; Minneapolis MN: 1993. [Google Scholar]
- 37.Derogatis L. The SCL-90-R. Baltimore MD: Clinical Psychometric Research; 1977. [Google Scholar]
- 38.Saunders B, Arata C, Killpatrick D. Development of a Crime-Related Post-Traumatic Stress Disorder Scale for Women Within the Symptom Checklist-90-Revised. Journal of Traumatic Stress. 1990;3:439–448. [PubMed] [Google Scholar]
- 39.Kroeneke K, Spitzer R. Gender differences in the reporting of physical and somatoform symptoms. Psychosomatic Medicine. 1998;60:150–155. doi: 10.1097/00006842-199803000-00006. [DOI] [PubMed] [Google Scholar]
- 40.Nakao M, Fricchione G, Myers P, et al. Anxiety is a good indicator for somatic symptom reduction through behavioral medicine intervention in a mind/body medicine clinic. Psychotherapy & Psychosomatics. 2001;70:50–57. doi: 10.1159/000056225. [DOI] [PubMed] [Google Scholar]
- 41.Price C, Thompson E. Measuring Dimensions of Body Connection: Body awareness and bodily dissociation. doi: 10.1089/acm.2007.0537. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Orbach I, Mikulincer M. The Body Investment Scale: Construction and validation of a body experience scale. Psychological Assessment. 1998;10(4):415–425. [Google Scholar]
- 43.Simeon D, Guralnik O, Gross S, et al. The detection and measurement of depersonalization disorder. The Journal of Nervous and Mental Disease. 1998;186(9):536–542. doi: 10.1097/00005053-199809000-00004. [DOI] [PubMed] [Google Scholar]


