The β‐haemolytic phenotype of Streptococcus pyogenes on blood media, which is due to the liberation of streptolysin S, is critical to the recognition of this pathogen in the diagnostic laboratory. We report the isolation of a non‐haemolytic variant of S pyogenes from a blood culture that was taken from a patient who died of sepsis. Non‐haemolytic isolates of S pyogenes are uncommon, very rarely associated with bacteraemia or sepsis, and may be difficult to recognise, especially if isolated from non‐sterile sites.
Case report
A morbidly obese woman in her 80s was admitted with a 1‐week history of a productive cough and breathlessness. Her past history included type II diabetes mellitus, hypertension and chronic leg ulcers. On examination, she was pyrexial (39°C), pulse was 120/min and respiratory rate 26/min. Blood pressure was 95/45 mm Hg. There was no evidence of cellulitis, and no murmurs were detected. A chest radiograph revealed left ventricular failure; no consolidation was evident, although the basal lung fields were poorly visualised. She had a haemoglobin of 10.8 g/dl and a total white blood cell count of 17×109/l (95% polymorphonuclear cells). C‐reactive protein was 198 mg/l. She was treated with intravenous co‐amoxiclav for presumed lower respiratory tract infection and sepsis, but died on the day of admission.
Blood cultures (one aerobic and one anaerobic bottle) signalled positive on a Bactec 9240 instrument after 1 day of incubation and Gram‐positive cocci in chains were seen in the Gram film. The following day, cream, non‐mucoid, non‐haemolytic, catalase‐negative colonies grew on horse blood agar (Oxoid) incubated aerobically and anaerobically. The colonies became large (3–4 mm in diameter) with a crenated edge and a depressed central ring after 48 h incubation, but remained non‐haemolytic (fig 1). Only minimal α‐haemolysis was observed around densely grouped colonies. The isolate was sensitive to bacitracin, L‐pyrrolidonyl‐β‐naphthylamide and DNase positive and possessed only the Lancefield group A antigen (Prolex Streptococcal Grouping Latex kit; Pro‐Lab Diagnostics, Neston, UK). Identification using both the Vitek 2 and the API Strep systems confirmed the isolate to be S pyogenes. The isolate was sensitive to penicillin, erythromycin and tetracycline using the British Society for Antimicrobial Chemotherapy (BSAC) disk testing methodology. The non‐haemolytic phenotype remained stable on repeated subculture. The isolate was typed as emm‐type 28, T‐type 28, opacity factor positive (Laboratory of HealthCare Associated Infection, Centre for Infections, Health Protection Agency, Colindale, London).
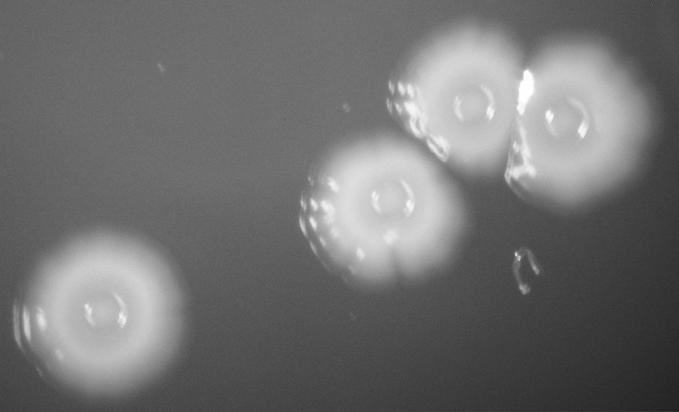
Figure 1 Colonies of non‐haemolytic Streptococcus pyogenes incubated on horse blood agar for 48 h. Aerobic and anaerobic cultures were identical in appearance.
Discussion
S pyogenes typically produces β‐haemolytic colonies on blood agar, and some strains are well‐recognised to produce mucoid colonies. Non‐mucoid, non‐haemolytic variants of S pyogenes have been recognised previously,1 but have rarely been reported from blood cultures.2,3,4 The β‐haemolytic phenotype is due to the liberation of streptolysin S. Strains that only produce streptolysin O do not exhibit typical β‐haemolysis on traditional blood media. Furthermore, streptolysin S isogenic mutants of S pyogenes have been shown to be markedly less virulent in a murine model of infection.5 This may, at least in part, explain the apparent rarity of invasive infections caused by non‐haemolytic isolates of S pyogenes. Of the four cases of bacteraemia previously reported, three were elderly patients, including one fatal case of pneumonia,2 and one was a 7‐year‐old child.3 In the latter case, a throat swab from the child had initially yielded a false‐negative result. The two cases of bacteraemia previously reported in the UK were due to an infrequently encountered emm‐type 58 S pyogenes.4
Non‐haemolytic variants of S pyogenes may be difficult to recognise when isolated on blood media.3,4,6 In the present case, the isolate was obtained in pure growth from a blood culture, and consequently was formally identified. Had the isolate been obtained in mixed culture or from a non‐sterile site such as the nasopharynx, the non‐haemolytic appearance may have led to the organism being dismissed as a contaminant or as commensal flora without further identification. Clinical microbiologists and biomedical scientists should be alert to the possibility of non‐haemolytic variants of S pyogenes from both sterile and non‐sterile sites.
Acknowledgements
The authors wish to thank the Laboratory of HealthCare Associated Infection for typing the isolate.
Footnotes
Competing interests: None declared.
References
- 1.Colebrooke L, Elliott S D, Maxted W R, Morley C W, Mortell M. Non‐haemolytic group‐A streptococci. Lancet 1942ii30–31. [Google Scholar]
- 2.Taylor M B, Barkham T. Fatal case of pneumonia caused by a nonhemolytic strain of Streptococcus pyogenes. J Clin Microbiol 2002402311–2312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cimolai N, Trombley C, Bhanju N M. Nonhemolytic Streptococcus pyogenes causing invasive infection. Clin Pediatr (Phila) 200241453. [DOI] [PubMed] [Google Scholar]
- 4.Weightman N C, Barnham M R. Report of unusual clinical appearance in bacteraemia with nonhaemolytic M‐type 58 Streptococcus pyogenes. Indian J Med Res 200411917–21. [PubMed] [Google Scholar]
- 5.Betschel S D, Borgia S M, Barg N L.et al Reduced virulence of group A streptococcal Tn916 mutants that do not produce streptolysin S. Infect Immun 1998661671–1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dierksen K P, Tagg J R. Haemolysin‐deficient variants of Streptococcus pyogenes and S. dysgalactiae subsp equisimilis may be overlooked as aetiological agents of pharyngitis. J Med Microbiol 200049811–816. [DOI] [PubMed] [Google Scholar]


