Abstract
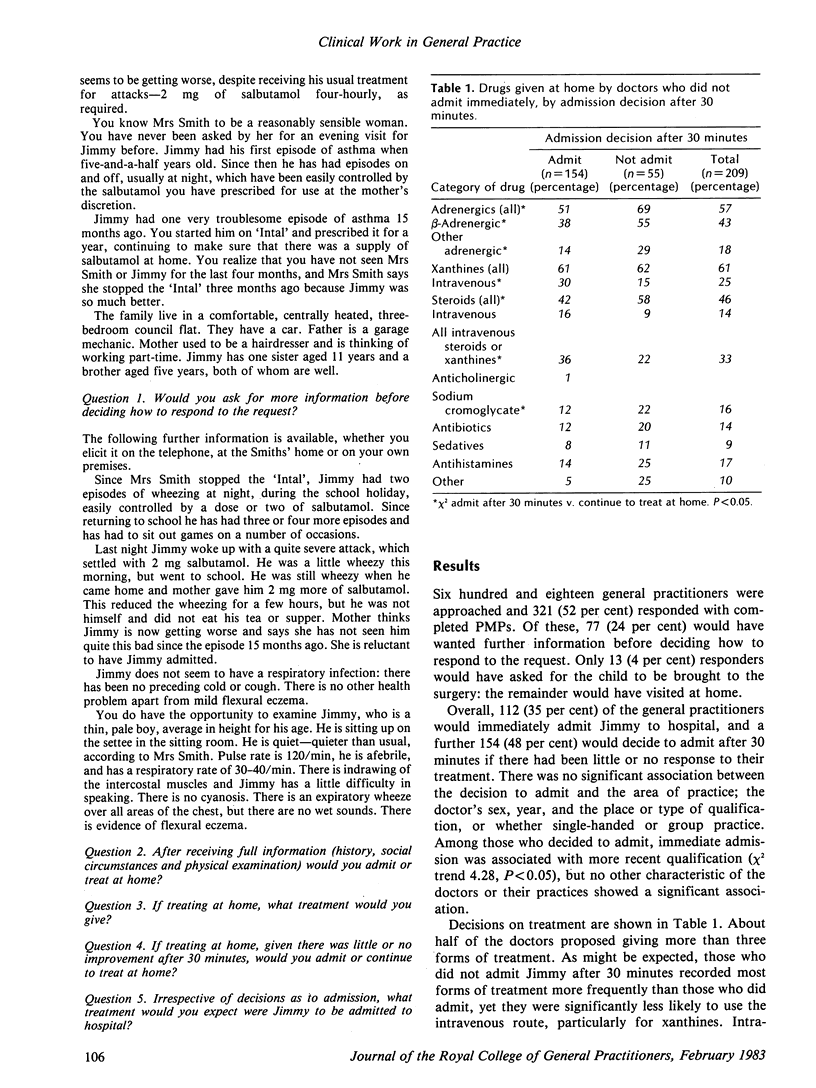
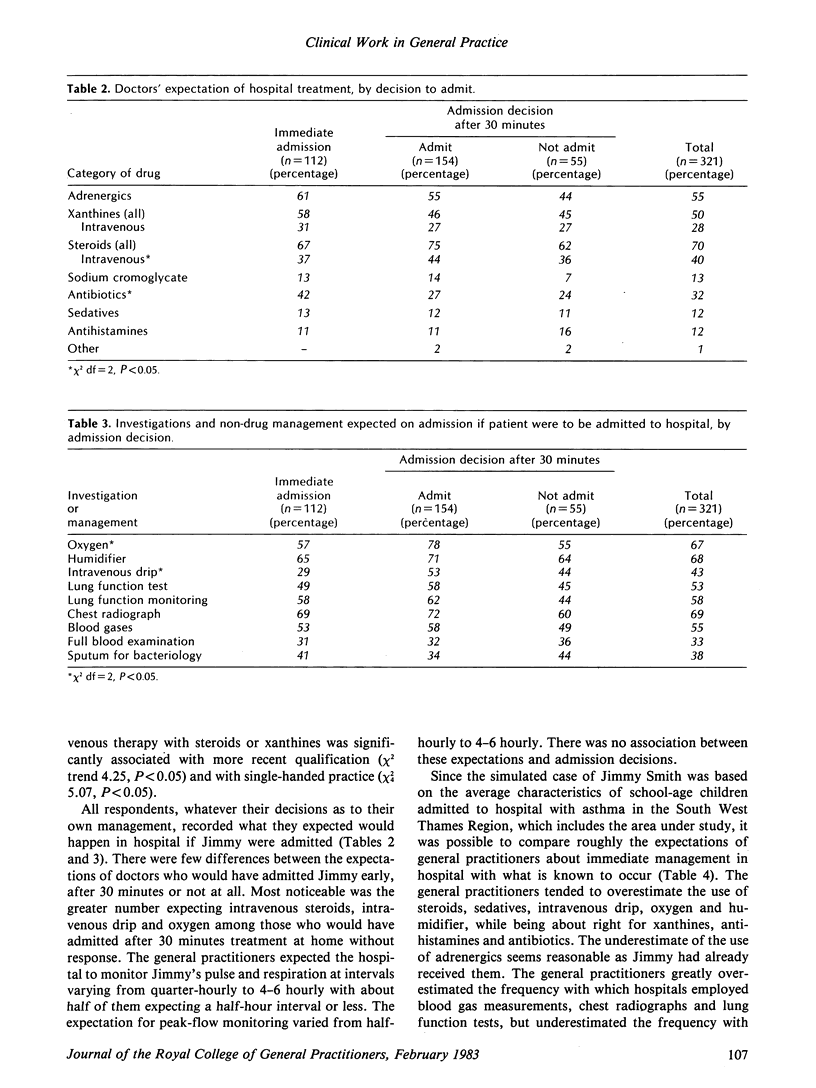
The management of an eight-year-old child with acute asthma was investigated by putting a semi-structured patient management problem (PMP) to 618 general practitioners. Of the 321 (52 per cent) who replied, 112 (35 per cent) would arrange for immediate admission to hospital and a further 154 (48 per cent) would have the child admitted after 30 minutes when initial home treatment appeared not to be working. Among those who would treat at home there was considerable variation in the type and intensity of treatment given. The more recently qualified were more likely to admit immediately or to treat vigorously at home (with intravenous steroids and/or aminophylline); no other characteristic of the doctor or the practice was related to admission decision or to treatment. Expectations concerning the immediate hospital management of the patient also varied widely. Comparison of the expected hospital management with actual management recorded in hospital case-notes suggested that general practitioners overestimate the use of intensive treatments (steroids, intravenous drip, oxygen) and investigations (blood gases, lung function tests, chest radiograph).
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson H. R., Bailey P. A., Cooper J. S., Palmer J. C. Influence of morbidity, illness label, and social, family, and health service factors on drug treatment of childhood asthma. Lancet. 1981 Nov 7;2(8254):1030–1032. doi: 10.1016/s0140-6736(81)91225-3. [DOI] [PubMed] [Google Scholar]
- Anderson H. R., Bailey P., West S. Trends in the hospital care of acute childhood asthma 1970-8: a regional study. Br Med J. 1980 Nov 1;281(6249):1191–1194. doi: 10.1136/bmj.281.6249.1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell A. J., Reinken J., Allan B. C., Martinez G. S. Falls in old age: a study of frequency and related clinical factors. Age Ageing. 1981 Nov;10(4):264–270. doi: 10.1093/ageing/10.4.264. [DOI] [PubMed] [Google Scholar]
- Chaput de Saintonge D. M., Hathaway N. R. Antibiotic use in otitis media: patient simulations as an aid to audit. Br Med J (Clin Res Ed) 1981 Oct 3;283(6296):883–884. doi: 10.1136/bmj.283.6296.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harden R. M., Dunn W. R., Murray T. S., Rogers J., Stoane C. Doctors accept a challenge: self-assessment exercises in continuing medical education. Br Med J. 1979 Sep 15;2(6191):652–653. doi: 10.1136/bmj.2.6191.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howie J. G. Further observations on diagnosis and management of general practice respiratory illness using simulated patient consultations. Br Med J. 1974 Jun 8;2(5918):540–543. doi: 10.1136/bmj.2.5918.540. [DOI] [PMC free article] [PubMed] [Google Scholar]


