Abstract
Aneurysms of the sinuses of Valsalva, when detected before rupture, are repaired electively. When they are small, they are most frequently repaired by direct closure; when they are large, they are repaired with a prosthetic patch. When they are associated with prolapse of the corresponding aortic cusp and aortic insufficiency, valve replacement is usually performed concomitantly. We present the case of a patient in whom both abnormalities were corrected by implantation of a Freestyle® bioprosthesis, the wall of which completely excluded the aneurysm of the sinus of Valsalva. The patient remains asymptomatic 18 months after surgery. (Tex Heart Inst J 2003;30:202–4)
Key words: Aortic aneurysm/surgery, heart valve prosthesis implantation, sinus of Valsalva/surgery
Aneurysms of the sinuses of Valsalva are thin-walled outpouchings most commonly involving the right or noncoronary sinuses. Because they are asymptomatic, they are rarely discovered before they rupture (usually into a right cardiac chamber) and form an aorto-cardiac fistula. We describe a patient in whom the aneurysm was discovered, still intact, during preoperative investigations for mitral and aortic valvular insufficiency.
In April 2001, a 39-year-old man was first seen in the emergency department with congestive heart failure. He had experienced progressive dyspnea and decreased exercise tolerance for more than 1 year but had not sought medical attention. He had not been seen by a physician for many years. He was of normal height and build, with normal features, and had normal vision. Auscultation revealed a 3/6 diastolic murmur along the left sternal border and a 3/6 holosystolic murmur at the apex, with radiation to the axilla. Electrocardiography showed 1st-degree heart block, and chest radiography revealed cardiomegaly, left ventricular dilatation, and left atrial enlargement. Transesophageal echocardiography (TEE) demonstrated a bicuspid aortic valve with severe regurgitation and aneurysmal dilatation of the noncoronary sinus of Valsalva (ASV), severe mitral regurgitation with prolapse of both leaflets, left atrial enlargement, and pulmonary artery hypertension, with depressed left ventricular function and an ejection fraction of 0.40. Angiography confirmed these findings and revealed normal coronary anatomy. The patient accepted our proposal of valve repair or replacement but refused long-term anticoagulation. He underwent double-valve replacement and repair of the ASV. His postoperative course was uneventful. He was discharged from the hospital 5 days after the operation. Repeat echocardiography at the 1-year follow-up visit showed no evidence of valvular insufficiency or other abnormalities. Eighteen months after the operation, the patient is asymptomatic and in New York Heart Association functional class I.
Surgical Technique
Cardiopulmonary bypass was instituted with aortic and bicaval cannulation. Cardioplegic arrest was achieved with the induction of warm cardioplegic solution via the coronary sinus, followed by cold cardioplegic solution; this last was repeated every 15 minutes.
The mitral valve was inspected first. There was massive dilatation of the annulus, with prolapse and distortion of both leaflets and chordae. It was anticipated that repair would not provide optimal results. The annulus was plicated with transverse mattress sutures to reduce its size to accept a 31-mm Hancock® II mitral bioprosthesis (Medtronic, Inc.; Minneapolis, Minn). In order to optimize left ventricular function, the subvalvular apparatus was preserved and the chordae shortened.
An intraoperative TEE (Fig. 1) confirmed the presence of a nonruptured ASV. A transverse aortotomy was made 5 mm above the sinotubular junction (STJ), in healthy tissue above the lesion. The STJ was sized at 25 mm, and the aortic annulus was estimated at 27 mm. A 27-mm Freestyle® aortic root bioprosthesis (Medtronic, Inc.) was selected. The ASV was measured, and its perimeter was smaller than the height and width of the porcine aortic wall adjacent to the noncoronary cusp. The bioprosthesis was then rotated 120 degrees in order to position its right sinus over the patient's affected noncoronary sinus. This maneuver enabled us to completely cover the ASV with the bioprosthesis. Interrupted 4-0 braided polyester inflow sutures were placed on a plane parallel to and below the aortic annulus. The valve was seated and trimmed (Fig. 2). The ASV was then completely excluded with the continuous outflow suture line. Before we declamped the aorta, warm cardioplegic solution was infused, followed by warm blood. Blood infusion was continued via the coronary sinus until strong cardiac contractions were present and air bubbles were no longer visible in the TEE. The remainder of the operation was completed in the usual manner. Intraoperative TEE, with volume and pressure loading, demonstrated complete exclusion of the ASV (Fig. 3).
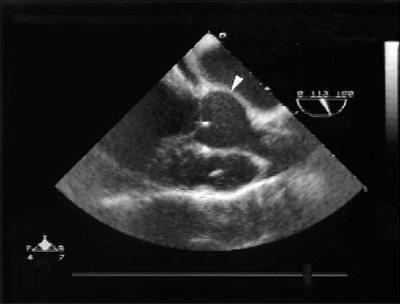
Fig. 1 Intraoperative transesophageal echocardiogram shows the nonruptured aneurysm of the sinus of Valsalva (arrowhead).
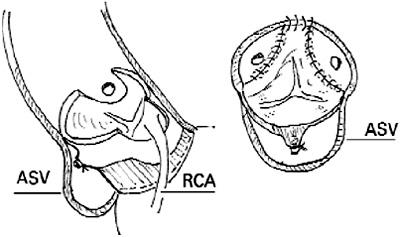
Fig. 2 Longitudinal and cross-sectional diagrams depict the implantation technique and the rotation of the Freestyle bioprosthesis.
ASV equals; aneurysm of the sinus of Valsalva; RCA = right coronary artery
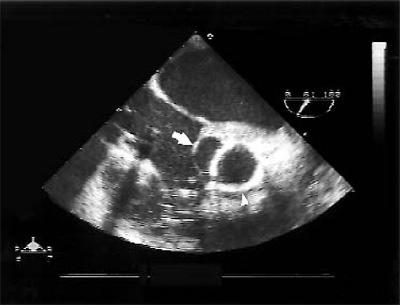
Fig. 3 Intraoperative transesophageal echocardiogram shows complete exclusion of the aneurysm of the sinus of Valsalva (arrow) by the Freestyle bioprosthesis (arrowhead).
Discussion
Early aggressive treatment is recommended for ASV in order to prevent endocarditis or enlargement of the lesion, which would necessitate more extensive repair. 1 Delay in operation may result in worsening of symptoms and death. 1,2 Cases of intact ASV are usually asymptomatic. In our patient, the aneurysm was found accidentally while he was being evaluated for valvular insufficiency. Marfan syndrome was considered in the differential diagnosis. However, our patient's lack of any other physical abnormalities characteristic of Marfan syndrome and the absence of secondary effacement of the sinotubular junction and dilatation of the ascending aorta precluded this diagnosis. 3 Currently, in any event, there are no available data on whether the mitral valve should be repaired or replaced in patients with Marfan syndrome and concomitant mitral regurgitation.
We elected not to repair the mitral valve, because its significant dilatation and deformity rendered unlikely a satisfactory and durable repair. An unsatisfactory repair followed by a 2nd period of cardiopulmonary bypass and aortic cross-clamping would have substantially increased this patient's operative risk, due to his poor ventricular function. Furthermore, if the same degenerative process affected both valves, the durability of the mitral valve repair would be questionable. Mild aortic regurgitation improves or disappears when sinus of Valsalva aneurysms are repaired with a circumferential patch, 4 but patients with residual aortic regurgitation after repair of a congenital ASV often need reoperation and aortic valve replacement. 4 Early reoperation would have put this patient at substantial risk because of his multivalvular disease and cardiac decompensation. The technique described here will probably decrease the risk of reoperation, because the need for reoperation will be determined by the durability of the prosthesis and not by failure of the ASV repair.
Because of the severity of the aortic insufficiency, we did not use antegrade cardioplegia, which would have dilated the left ventricle and failed to appropriately perfuse the coronary arteries. Retrograde cardioplegia in the presence of normal coronary arteries provided optimal myocardial protection. The native aortic valve was not repaired, because it was bicuspid, was calcified at the base of the cusps, and had significant distortion of the noncoronary cusp at the point of its attachment to the coronary sinus. Bicuspid aortic valves are present in 17% of patients with ASV. 1 Furthermore, involvement of the aortic valve in patients with ASV is thought to be the result of lack of supporting tissues, which causes sagging of the aortic cusps, turbulence, and eventually fibrosis. 5 When these changes have occurred, valve replacement is indicated. 6 Although some small sinus of Valsalva aneurysms can be treated by primary closure, the incidence of sequelae is higher than when the ASV is treated with a patch. 7
The noncoronary sinus is affected in 28% of patients with ASV. 4 In human beings, the noncoronary sinus is usually the largest of the 3 coronary sinuses. In the porcine aortic root, the right coronary sinus is the largest and has, at its base, a well-developed ventricular muscle bar. The Freestyle bioprosthesis is constructed with a skirt of Dacron that covers this muscle bar, thus strengthening this area and reducing its antigenicity. In our patient, this feature made this valve ideal, upon rotation, for completely covering and excluding the aneurysm that involved the noncoronary sinus. Although our patient's coronary ostia were slightly closer than in patients with tricuspid aortic valves, we were able to fit the trimmed post of the bioprosthesis between them without obstructing their lumen. This technique substantially reduced operative time, in comparison with such alternatives as aortic valve replacement and patching of the ASV. The technique is reproducible, provided that the aneurysm can be completely excluded and the sutures placed in non-aneurysmal tissue.
Acknowledgment
We are grateful to Christine Eusoof-Alviz, RN, BSN, CCRN, for her assistance in the preparation of this manuscript.
Footnotes
Address for reprints: C. Del Campo, MD, Suite 195, 301 W. Bastanchury Rd., Fullerton, CA 92835
E-mail: cdelcampo@pol.net
References
- 1.Takach TJ, Reul GJ, Duncan JM, Cooley DA, Livesay JJ, Ott DA, Frazier OH. Sinus of Valsalva aneurysm or fistula: management and outcome. Ann Thorac Surg 1999;68:1573–7. [DOI] [PubMed]
- 2.Munk MD, Gatzoulis MA, King DE, Webb GD. Cardiac tamponade and death from intrapericardial rupture [corrected] of sinus of Valsalva aneurysm [published erratum appears in Eur J Cardiothorac Surg 1999;15:379]. Eur J Cardiothorac Surg 1999;15:100–2. [DOI] [PubMed]
- 3.El Habbal MH. Cardiovascular manifestations of Marfan's syndrome in the young. Am Heart J 1992;123:752–7. [DOI] [PubMed]
- 4.Barragry TP, Ring WS, Moller JH, Lillehei CW. 15- to 30-year follow-up of patients undergoing repair of ruptured congenital aneurysms of the sinus of Valsalva. Ann Thorac Surg 1988;46:515–9. [DOI] [PubMed]
- 5.Verghese M, Jairaj PS, Babuthaman C, Sukumar IP, John S. Surgical treatment of ruptured aneurysms of the sinus of Valsalva. Ann Thorac Surg 1986;41:284–6. [DOI] [PubMed]
- 6.Taguchi K, Sasaki N, Matsuura Y, Uemura R. Surgical correction of aneurysm of the sinus of Valsalva. A report of forty-five consecutive patients including eight with total replacement of the aortic valve. Am J Cardiol 1969;23:180–91. [DOI] [PubMed]
- 7.Kirali K, Guler M, Daglar B, Yakut N, Mansuroglu D, Balkanay M, et al. Surgical repair in ruptured congenital sinus of Valsalva aneurysms: a 13-year experience. J Heart Valve Dis 1999;8:424–9. [PubMed]


