Abstract
Aim:
To report data from a multinational survey investigating the relationship between gastro-oesophageal reflux disease (GERD) symptoms, treatment and subjective well-being.
Methods:
Patients formally diagnosed with GERD (n = 929) and undiagnosed subjects with symptoms suggestive of GERD (n = 924) were included.
Results:
Sixty per cent of diagnosed (mean age: 51.7 years) and 54% of undiagnosed (mean age: 44.3 years) participants were female. Over 50% of participants were overweight or obese. Most respondents consumed alcohol, and one-third were smokers. In total, 78% of diagnosed subjects were currently receiving medication prescribed by their doctor, and 65% were taking over-the-counter (OTC) treatments. The majority (97%) of undiagnosed subjects were taking OTC medication, the most common of which were antacids (78%). Despite medication, 58% of diagnosed and 73% of undiagnosed subjects still experienced GERD symptoms some of the time. Approximately one-third of subjects in each group reported that they ate less than usual, felt generally unwell, were tired/worn out or worried/fearful for the majority of the time because of their GERD symptoms, and around half reported decreased well-being, including reduced work or leisure time productivity.
Conclusions:
These findings attest to the severity and impact of GERD symptoms, highlighting the need to improve the management of GERD in routine practice. Many symptomatic and long-term sufferers, for example, may benefit from taking steps towards a healthier lifestyle (e.g. weight reduction) in addition to optimisation of acid-suppressive therapy.
What's known
Gastro-oesophageal reflux disease (GERD) is a prevalent and chronic condition in which reflux of the stomach contents into the oesophagus causes a range of troublesome symptoms that can cause marked disruption of physical, social and emotional well-being.
Despite the prevalence and impact of GERD, along with the availability of effective treatments on prescription, many subjects with symptoms suggestive of GERD do not seek medical attention.
What's new
The findings of this large multinational survey attest to the severity and impact of GERD symptoms, highlighting the need to improve the management of GERD in routine practice.
The study also emphasises the need to raise public awareness of GERD, in terms of both the impact of long-term, under-treated GERD and the options available for symptom relief.
Introduction
Gastro-oesophageal reflux disease (GERD) is a prevalent and chronic condition in which reflux of the stomach contents into the oesophagus causes a range of troublesome symptoms (including heartburn, acid regurgitation and epigastric pain) and complications (1). Such symptoms can cause marked disruption of physical, social and emotional well-being (2,3), with possible long-term complications of GERD including reflux oesophagitis, haemorrhage, stricture, Barrett's oesophagus and adenocarcinoma of the distal oesophagus (1).
The primary goals of GERD therapy are enduring symptom relief, protection from long-term complications and improved subjective well-being. Proton pump inhibitors (PPIs), which provide powerful gastric acid control (4,5), are the treatment of choice in this regard (1,6). Despite the prevalence and impact of GERD, however, along with the availability of effective treatments on prescription, many subjects with symptoms suggestive of GERD do not seek medical attention (7). Widespread self-medication with over-the-counter (OTC) treatments undoubtedly contributes to this problem of inadequate disease management.
In order to further investigate the relationship between GERD symptoms, treatment and subjective well-being, a large multinational survey was conducted in formally diagnosed GERD patients and undiagnosed subjects suffering from symptoms suggestive of GERD.
Methods
Potential survey participants were identified via random digit dialling of households in the USA, UK, France and Germany. Respondents were screened for eligibility and classified into one of two groups. The first group comprised patients who had been diagnosed by a doctor as suffering from GERD, acid regurgitation or heartburn and had been prescribed medication for their symptoms (either on the basis of a clinical diagnosis or as a result of investigations). The second group comprised undiagnosed symptomatic subjects, who had not approached a doctor about their condition and had suffered heartburn or acid regurgitation at least twice in the previous week (identified using a screening questionnaire). The sampling strategy dictated that the study population was to include 50% formally diagnosed subjects, and 50% undiagnosed symptomatic subjects. The survey was conducted in accordance with the MRS Code of Conduct and the ICC/ESOMAR guidelines (available at: http://www.esomar.org), and subjects provided consent before proceeding with the interview.
Assenting participants underwent face-to-face, computer-assisted interviews of maximum 45-min duration. A 100-item questionnaire was used to gather information about participants’ symptoms, lifestyle and medication usage. Symptom severity was rated by participants on a six-point scale (1 = did not have; 2 = very mild; 3 = mild; 4 = moderate; 5 = moderately severe; 6 = severe). Subgroup analyses were conducted on data received from diagnosed participants currently receiving treatment with PPIs. These participants were classified as being complete responders, well-controlled, incomplete responders, non-responders, or other, based on whether they were currently experiencing key GERD symptoms (acid regurgitation, heartburn or epigastric pain) (Table 1). All statistical analyses were descriptive.
Table 1.
Definition of response to treatment among subjects formally diagnosed with gastro-oesophageal reflux disease (GERD) and receiving prescribed proton pump inhibitor (PPI) therapy
| Category | Criteria |
|---|---|
| Complete responders | Suffered ‘no symptoms’* within the previous 7 days |
| Well controlled | Suffered any key GERD symptom* on one of the previous 7 days |
| Reported that ‘symptoms have improved a lot’ or ‘symptoms improveda little’ or that they experience symptoms ‘less frequently’ or ‘muchless frequently’ since first taking PPI | |
| Take prescribed PPI one to four times per day or ‘always’ or ‘usually’take PPI as the label advises | |
| Incomplete responders | Suffered any key GERD symptom* on ≥ 2 of the previous 7 days |
| Reported that ‘symptoms have improved a lot’ or ‘symptoms improveda little’ or that they experience symptoms ‘less frequently’ or ‘muchless frequently’ since first taking PPI | |
| Take prescribed PPI one to four times per day or ‘always’ or ‘usually’take PPI as the label advises | |
| Non-responders | Reported that ‘symptoms stayed the same’ or ‘symptoms worsened’since first taking PPI |
| Take prescribed PPI one to four times per day or ‘always’ or ‘usually’take PPI as the label advises | |
| Other | All PPI users who do not fit into the above categories |
Acid regurgitation, heartburn or epigastric pain. GERD, gastro-oesophageal reflux disease. Patients had to meet all of the listed criteria to be assigned to the respective category.
Results
In total, 212,099 households were identified via the random digit dialling method. Some 56% of calls (n = 117,880) proved unsuccessful and there were 58,580 refusals (28%). For calls that were successfully screened data were available for 1853 participants; 929 and 924 subjects, respectively, were assigned to the diagnosed and undiagnosed cohorts. The demographic characteristics of the two groups are reported in Table 2. Participants were mainly female and had a mean (SD) age of 51.7 (15.9) years and 44.3 (15.4) years in the diagnosed and undiagnosed groups respectively. There were slightly more patients aged ≥ 55 years in the diagnosed than in the undiagnosed group. Approximately 60% of the study population were overweight [body mass index (BMI) 25–29.9 kg/m2] or obese (BMI ≥ 30 kg/m2), and about the same proportions were in full- or part-time employment. Most respondents consumed alcohol, and one-third were smokers. The two groups were generally comparable in terms of the distribution of these lifestyle characteristics. Concomitant conditions were common among study participants, including hypertension, arthritis and hypercholesterolaemia. Arthritis and concomitant regular use (at least weekly) of non-steroidal anti-inflammatory drugs (NSAIDs) was more common among the diagnosed than the undiagnosed subjects. The most common NSAIDs in both groups were ibuprofen (11% and 15% in the diagnosed and undiagnosed groups respectively) and ‘others’ (25% and 17% respectively).
Table 2.
Characteristics of study participants (n = 1853)
| Characteristic | Diagnosed subjects, n = 929 (%) | Undiagnosed subjects, n = 924 (%) |
|---|---|---|
| Female gender | 60 | 54 |
| Age, years | ||
| 18–30 | 11 | 21 |
| 31–54 | 44 | 51 |
| ≥ 55 | 45 | 28 |
| Body mass index* | ||
| Normal | 40 | 47 |
| Overweight | 38 | 35 |
| Obese | 21 | 17 |
| Working status | ||
| Working full- or part-time | 53 | 64 |
| Not working | 47 | 36 |
| Smoker | 28 | 38 |
| Alcohol consumption | ||
| Frequently (daily or more than 2–3 times per week) | 29 | 34 |
| Occasionally (up to once per week) | 41 | 43 |
| Never | 25 | 19 |
| Not reported | 1 | 0 |
| Other conditions | ||
| Hypertension | 16 | 13 |
| Arthritis | 13 | 8 |
| Hypercholesterolaemia | 11 | 10 |
| Migraine | 8 | 9 |
| Diabetes | 8 | 6 |
| Anxiety | 9 | 7 |
| Asthma | 7 | 7 |
| Concomitant use of NSAIDs | 22 | 14 |
Overweight and obese defined as body mass index of 25–29.9 and ≥ 30 kg/m2 respectively. NSAID, non-steroidal anti-inflammatory drug.
Symptoms
Subjects in the diagnosed population had experienced symptoms suggestive of GERD for an average of 10.8 years. In the undiagnosed group, the mean length of time since symptoms were first experienced was 7.7 years. Symptoms were mainly mild or moderate in severity (Table 3). More subjects reported severe heartburn or acid regurgitation in the diagnosed than in the undiagnosed group (32% vs. 23% and 30% vs. 18%). In the diagnosed group, over two-thirds of respondents (67%) waited for up to 6 months before consultation and 11% waited over 4 years. For undiagnosed patients, the most frequent reasons for not consulting a doctor were that ‘non-prescription medicines work effectively’ and that ‘I have control of my symptoms’.
Table 3.
Severity of symptoms in diagnosed and undiagnosed subjects
| Symptom (% subjects) | ||||||
|---|---|---|---|---|---|---|
| Severity of symptom* | Heartburn | Acid regurgitation | Acid taste | Belching | Indigestion | Bloating |
| Diagnosed subjects | n = 602 | n = 482 | n = 279 | n = 248 | n = 232 | n = 227 |
| Mild | 26 | 24 | 30 | 38 | 33 | 30 |
| Moderate | 41 | 44 | 38 | 34 | 34 | 37 |
| Severe | 32 | 30 | 30 | 26 | 31 | 33 |
| Undiagnosed subjects | n = 710 | n = 475 | n = 295 | n = 249 | n = 225 | n = 200 |
| Mild | 36 | 38 | 43 | 44 | 39 | 37 |
| Moderate | 41 | 43 | 36 | 37 | 40 | 35 |
| Severe | 23 | 18 | 20 | 18 | 20 | 27 |
Among patients reporting the symptom. Values do not necessarily total 100% because of rounding and missing data.
Common trigger factors for GERD symptoms included eating (80% and 84% in the diagnosed and undiagnosed subjects respectively), stress (30% and 28% respectively) and physical activity (18% and 14% respectively). Most subjects reported that they had attempted to change their lifestyle accordingly to try and avoid or limit the impact of these trigger factors, but symptoms often continued to be experienced at least some of the time.
Current medications for GERD
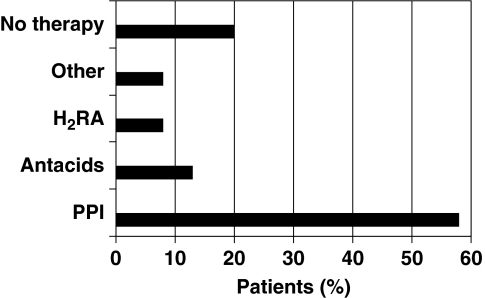
Among diagnosed participants, PPIs were the most commonly prescribed treatment, followed by antacids and H2-receptor antagonists (H2RAs) (Figure 1). Use of OTC medication was also common among diagnosed subjects; 52% of subjects were taking antacids, 10% were taking H2RAs and 3% were taking PPIs.
Figure 1.
Current medicines prescribed by a doctor in participants with a formal diagnosis of gastro-oesophageal reflux disease (n = 929); multiple responses possible. PPI, proton pump inhibitor; H2RA, H2-receptor antagonist
The majority (97%) of undiagnosed symptomatic subjects were currently taking OTC medication, the most common of which was antacids (78%). In general, these participants had been using OTC medication for 1–4 years.
Self-reported adherence to treatment prescribed by a doctor was generally good. Some 71% of diagnosed participants reported that they ‘usually’ or ‘always’ took their prescribed medicine as the label advised. Some 35% of diagnosed patients reported that they often took their prescribed medication in anticipation of symptoms occurring. High levels of self-reported adherence were also observed among PPI-treated patients. Adherence was poor in patients taking OTC medication; only 53% of diagnosed and 53% of undiagnosed participants took their medication as the label advised. Approximately one-third of all subjects in each group took their OTC medication prophylactically.
Effects of current medication on symptoms
Symptoms were not completely alleviated with current treatments. Among diagnosed patients, 58% reported that they continued to experience symptoms ‘some of the time’, although the majority reported that symptoms had improved [in terms of severity (84%) and frequency (73%)] since they first started treatment. Only one-third (33%) of diagnosed patients responded that they were ‘very satisfied’ with treatment [the corresponding value among those receiving PPIs (n = 537) was 36%].
Of the subgroup of diagnosed patients receiving PPI treatment who were evaluable for response (n = 482), only 186 (39%) were classified as either complete responders (n = 125) or well controlled (n = 61); 247 (51%) were incomplete responders and 49 (10%) were non-responders. Patients in the latter group were more likely to use OTC medications in addition to their PPI (71% vs. 42% of complete responders and 56% of well-controlled subjects).
Forty-seven per cent of undiagnosed subjects reported no change in the frequency of their symptoms since first taking OTC medication. Similarly, 28% reported no change in the severity of their symptoms.
Effects of symptoms on subjective well-being and productivity
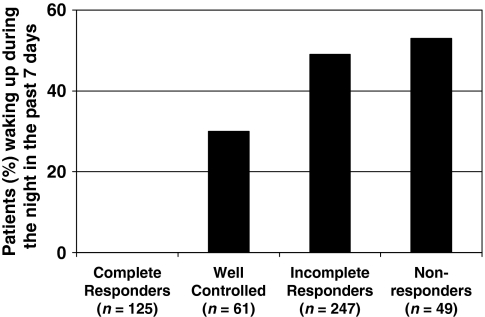
Sleep disturbances attributed to symptoms were reported in approximately half of both diagnosed (55%) and undiagnosed (45%) participants who had experienced any symptom of GERD in the past 7 days. Diagnosed subjects reported that they had been woken by their symptoms an average of 3.0 times in the past 7 days, compared with 2.7 times in undiagnosed subjects. The mean duration of night-time wakefulness was estimated at 74.9 and 62.5 min, respectively, per episode. Of the subgroup of diagnosed patients receiving PPI treatment, the extent of sleep disturbance decreased with increasing level of symptom control and response to treatment (Figure 2).
Figure 2.
Extent of sleep disturbance in relation to the level of symptom control among diagnosed patients receiving treatment with a proton pump inhibitor (n = 537)
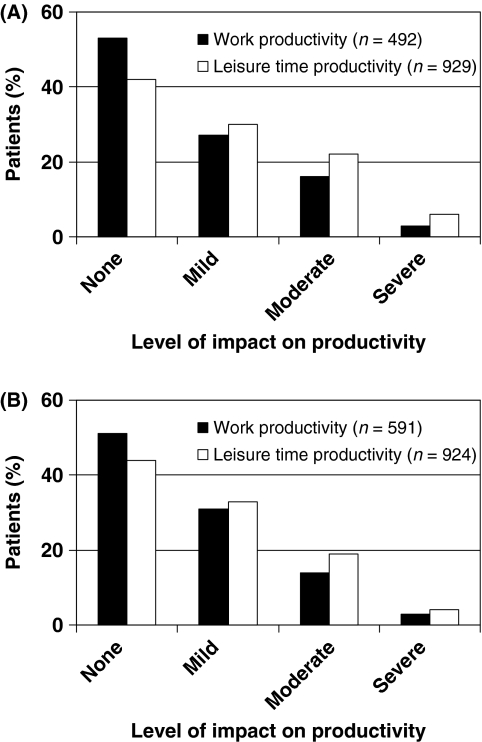
Gastro-oesophageal reflux disease symptoms were perceived to impact negatively on both professional and leisure activity; approximately half of participants in each group estimated that work and leisure time productivity were mildly or moderately affected by their GERD symptoms (Figure 3A,B). Both employed diagnosed and undiagnosed subjects reported that they were absent from work for a mean of 20 min per week because of problems associated with their GERD symptoms.
Figure 3.
Proportion of (A) diagnosed and (B) undiagnosed respondents with lost work (among participants working full- or part-time) and leisure time productivity because of gastro-oesophageal reflux disease symptoms. The extent of impact on productivity was assessed between 0% and 100%, where 0% equals work or regular leisure activities completely unaffected and 100% equals completely affected. Categories were designated are as follows: None, 0%; Mild, > 0–20%; Moderate, 20–60%; and Severe, > 60%
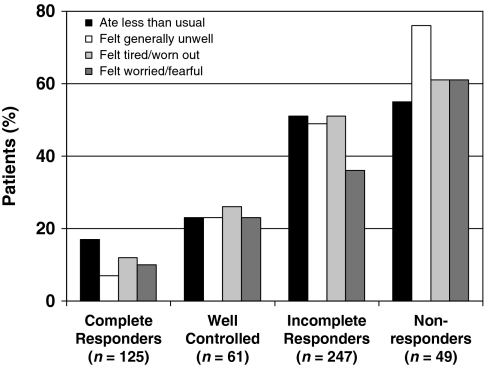
Gastro-oesophageal reflux disease symptoms were also perceived to have detrimental effects on other aspects of subjective well-being. Considering the last 7 days, approximately one-third of diagnosed and undiagnosed subjects reported that they ate less than usual (46% and 38% respectively) or that they felt generally unwell (37% and 34% respectively), were tired/worn out (37% and 29% respectively) or worried/fearful (27% and 22% respectively) the majority of the time because of their symptoms. Of the subgroup of diagnosed patients receiving PPI treatment, the impact of GERD on these aspects of well-being was decreased for those who were complete responders or well controlled (Figure 4).
Figure 4.
Proportion of diagnosed patients receiving proton pump inhibitor treatment (n = 537) who reported that they ate less than usual, felt generally unwell, tired/worn out or worried/fearful at least some of the time in the last 7 days, according to level of response to treatment
Discussion
This large, multinational survey is the first to report data from both formally diagnosed GERD patients and undiagnosed subjects experiencing symptoms suggestive of GERD. An important finding is that GERD symptoms were persistent in many diagnosed respondents despite the use of medicines prescribed by a doctor, including PPIs. Poor symptom control in our study probably explains why a high proportion of patients taking medication prescribed by their doctor were also taking OTC medicines. These results are similar to those observed in a recent study (7), in which 20.5% of patients receiving any therapy prescribed by a doctor for GERD were also taking OTC medicines, the main reason for which was that ‘prescription therapy alone was not effective’. Similarly, Fass et al. (8) reported that 30% of patients classified as having GERD and receiving PPI treatment continued to experience symptoms.
A variety of factors may contribute to failure of therapy prescribed by a doctor to provide enduring relief of symptoms, including poor treatment adherence. Patients may take their medication on an ‘on-demand’ basis (whether they are told to or not) and it is inevitable that they will subsequently continue to experience symptoms because taking medication is triggered by symptom recurrence. However, self-reported treatment adherence was generally fairly high in patients taking medication prescribed by their doctor. We are unable to comment on the possibility that symptom control is better in the 35% of patients who took their prescribed medication prophylactically, but recognise that this may be an appropriate approach to symptom-led treatment. It is unlikely, therefore, to have been an issue in the present study. Instead, poor symptom control may have been attributable to non-acid or weakly acidic reflux, such as duodenogastro-oesophageal reflux or functional heartburn (9,10), or delayed gastric emptying and/or visceral hypersensitivity. The diagnosis, therefore, should be carefully reviewed, especially among non-responders.
Use of OTC medication was a common finding in the present study, with many undiagnosed subjects preferring to self-medicate with OTC medicines as an alternative to seeing their doctor. This is a recognised phenomenon, and outlines the need for greater awareness among the general population as to the potential seriousness of GERD and the need to consult a doctor for appropriate treatment.
Symptom-induced sleep disturbances, with resultant daytime sleepiness, are likely to have contributed to the decreased work and leisure time productivity observed in our study. Indeed, this effect was particularly pronounced in subjects with a lack of response to PPI treatment. Our findings are therefore consistent with those of a previous study (11), in which nocturnal symptoms were negatively associated with work productivity.
Important limitations of this study, which may limit applicability of the results to the general population, are the reliance on self-reported data, the potential bias towards subjects willing to participate in survey research and the lack of a control group without GERD-like symptoms. Furthermore, the high levels of self-reported treatment adherence may well have been overestimated, as most patients are likely to reply positively to the question ‘Do you always take your medicine as the label advises?’ Similarly, the reported effects of symptoms on sleep, productivity and general well-being in this survey should be interpreted cautiously, as subjective estimations rather than a validated questionnaire were used to gather information on well-being. The influence of other confounding factors on well-being, such as age, obesity and concomitant conditions, must also be considered. In the present study, the diagnosed population comprised more patients aged ≥ 55 years than the undiagnosed population. In addition, the prevalence of arthritis was higher in the diagnosed population, which may be a reflection of the older age of these subjects. Concomitant NSAID use was also higher in diagnosed than in undiagnosed subjects, which is likely to be as a result of the presence of age-related conditions such as arthritis, and this may have contributed to their symptoms. A higher prevalence of NSAID use could also be a result of the fact that subjects in the diagnosed group may be more likely to visit their doctor, and therefore receive medication prescribed by a doctor, than those in the undiagnosed group. The use of an age-matched control group without GERD-like symptoms would allow better understanding of the effects of symptoms on subjective well-being. A further limitation is that there may be an over-representation of ‘incomplete responders’ in our study compared with the general population, given that diagnosed patients with well-controlled symptoms were probably less likely to have entered the study.
The perceived burden of symptoms on well-being among subjects in our study demonstrates a considerable unmet need for enduring relief of symptoms among subjects with confirmed, or suspected, GERD. Indeed, long-term sufferers and persistently symptomatic subjects may benefit from a careful review of their symptoms and optimisation of acid-suppressive therapy by switching to another more potent PPI. Doctors should also encourage their patients to adopt a healthier lifestyle, given that the survey revealed many subjects to be smokers, regular consumers of alcohol and/or overweight or obese. It is notable, however, that many respondents had attempted to modify their lifestyle in order to control their symptoms but with limited success, which is in agreement with the recent evidence-based analysis of Kaltenbach et al. (12). Perhaps the strongest educational message is that overweight or obese subjects should be encouraged to lose weight, given that this can help improve symptoms (12). Many symptomatic subjects may benefit from weight loss (as part of a healthier lifestyle) in addition to optimisation of acid-suppressive therapy, recognising of course that certain activities may themselves exacerbate symptoms and should be avoided.
Conclusions
In summary, the findings of this study show that GERD symptoms may persist despite treatment with OTC agents or medicines prescribed by a doctor and, in turn, such symptoms have a significant impact on subjective well-being. A need therefore exists to improve the management of GERD in routine practice to ensure that patients achieve enduring relief from the disruption and frustration caused by their symptoms. In particular, it would be useful to identify long-term sufferers and those with inadequate symptom control who may benefit from more effective acid-suppressive therapy, while the diagnosis should be carefully reviewed among the small proportion of non-responders who may have a different cause for their symptoms.
Acknowledgments
This study was supported by AstraZeneca. We thank Vicki Oldfield, Claire Byrne and Steve Winter, from Wolters Kluwer Health, who provided medical writing support funded by AstraZeneca.
References
- 1.Vakil N, et al. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–20. doi: 10.1111/j.1572-0241.2006.00630.x. [DOI] [PubMed] [Google Scholar]
- 2.Wiklund I. Review of the quality of life and burden of illness in gastroesophageal reflux disease. Dig Dis. 2004;22:108–14. doi: 10.1159/000080308. [DOI] [PubMed] [Google Scholar]
- 3.Wiklund I. Gastroesophageal reflux symptoms and well-being in a random sample of the general population of a Swedish community. Am J Gastroenterol. 2006;101:18–28. doi: 10.1111/j.1572-0241.2005.00343.x. [DOI] [PubMed] [Google Scholar]
- 4.Miner P., Jr Gastric acid control with esomeprazole, lansoprazole, omeprazole, pantoprazole, and rabeprazole: a five-way crossover study. Am J Gastroenterol. 2003;98:2616–20. doi: 10.1111/j.1572-0241.2003.08783.x. [DOI] [PubMed] [Google Scholar]
- 5.Röhss K. Esomeprazole 40 mg provides more effective intragastric acid control than lansoprazole 30 mg, omeprazole 20 mg, pantoprazole 40 mg and rabeprazole 20 mg in patients with gastro-oesophageal reflux symptoms. Eur J Clin Pharmacol. 2004;60:531–9. doi: 10.1007/s00228-004-0804-6. [DOI] [PubMed] [Google Scholar]
- 6.DeVault KR. Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. Am J Gastroenterol. 2005;100:190–200. doi: 10.1111/j.1572-0241.2005.41217.x. [DOI] [PubMed] [Google Scholar]
- 7.Jones R, et al. Does the treatment of gastroesophageal reflux disease (GERD) meet patients’ needs? A survey-based study. Curr Med Res Opin. 2006;22:657–62. doi: 10.1185/030079906X100032. [DOI] [PubMed] [Google Scholar]
- 8.Fass R, et al. Systematic review: proton-pump inhibitor failure in gastro-oesophageal reflux disease – where next? Aliment Pharmacol Ther. 2005;22:79–94. doi: 10.1111/j.1365-2036.2005.02531.x. [DOI] [PubMed] [Google Scholar]
- 9.Dent J, et al. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2005;54:710–7. doi: 10.1136/gut.2004.051821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sifrim D. Gastro-oesophageal reflux monitoring: review and consensus report on detection and definitions of acid, non-acid, and gas reflux. Gut. 2004;53:1024–31. doi: 10.1136/gut.2003.033290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dean BB, et al. The burden of illness of gastro-oesophageal reflux disease: impact on work productivity. Aliment Pharmacol Ther. 2003;17:1309–17. doi: 10.1046/j.1365-2036.2003.01588.x. [DOI] [PubMed] [Google Scholar]
- 12.Kaltenbach T. Are lifestyle measures effective in patients with gastroesophageal reflux disease? An evidence-based approach. Arch Intern Med. 2006;166:965–71. doi: 10.1001/archinte.166.9.965. [DOI] [PubMed] [Google Scholar]