Abstract
Aims
This study examined the rates and predictors of 3-year remission, and subsequent 16-year relapse, among initially untreated individuals with alcohol use disorders who did not obtain help or who participated in treatment and/or Alcoholics Anonymous in the first year after recognizing their need for help.
Design and measures
A sample of individuals (n = 461) who initiated help-seeking was surveyed at baseline and 1 year, 3 years, 8 years and 16 years later. Participants provided information on their life history of drinking, alcohol-related functioning and life context and coping.
Findings
Compared to individuals who obtained help, those who did not were less likely to achieve 3-year remission and subsequently were more likely to relapse. Less alcohol consumption and fewer drinking problems, more self-efficacy and less reliance on avoidance coping at baseline predicted 3-year remission; this was especially true of individuals who remitted without help. Among individuals who were remitted at 3 years, those who consumed more alcohol but were less likely to see their drinking as a significant problem, had less self-efficacy, and relied more on avoidance coping, were more likely to relapse by 16 years. These findings held for individuals who initially obtained help and for those who did not.
Conclusions
Natural remission may be followed by a high likelihood of relapse; thus, preventive interventions may be indicated to forestall future alcohol problems among individuals who cut down temporarily on drinking on their own.
Keywords: Alcoholics Anonymous, alcohol use disorder, relapse, remission, treatment
INTRODUCTION
There is considerable information about short-term remission rates among individuals who have been treated for alcohol use disorders, but much less is known about prospectively ascertained natural remission rates. Moreover, we have virtually no information about relapse rates following remission among untreated individuals, or how they compare with relapse rates following remission among treated individuals. Two important related issues involve identification of predictors of short-term remission and subsequent relapse among remitted individuals, and specification of differential predictors of remission and relapse for treated versus untreated individuals.
We address these issues here in a 16-year prospective study of initially untreated individuals with alcohol use disorders and focus on four questions:
What are the short-term (3-year) remission rates among initially untreated individuals? Do individuals who obtain no help or who obtain help by entering treatment and/or Alcoholics Anonymous (AA) in the first year after they initiate help-seeking have higher short-term remission rates than individuals who obtain no help?
What are the long-term (16-year) relapse rates among helped and non-helped individuals who achieve short-term remission? Do individuals who remit without obtaining help have higher relapse rates than individuals who remit after participation in treatment and/or AA?
What are the demographic and life history, alcohol-related and life context and coping predictors of short-term remission; do they differ between individuals who do versus those who do not obtain help in the first year after they initiate help-seeking?
What are the demographic and life history, alcohol-related and life context and coping predictors of subsequent relapse among individuals who achieve short-term remission; do these predictors differ between individuals who do versus those who do not obtain help in the first year after they initiate help-seeking?
Rates of short-term remission and subsequent relapse
Among treated individuals, short-term remission rates vary between 20 and 50%, depending on the severity of the disorder and the criteria for remission [1,2]. Initial studies suggested that between 5 and 45% of untreated individuals with alcohol use disorders may achieve some improvement or remission [3,4]. Subsequent studies estimated untreated remission rates to range from 50 to 80% or more, depending on the severity of alcohol problems. However, these studies focused primarily on general population or media-recruited samples; that is, on individuals who had not initiated help-seeking and who may have had less severe and as yet unrecognized problems [5,6].
In a meta-analysis of alcoholism treatment outcome studies, average short-term abstinence rates were 21% for untreated individuals in waiting-list, no-treatment or placebo conditions, compared to 43% for treated individuals [2,7]. Similarly, Weisner, Matzger & Kaskutas [8] found that treated alcohol-dependent individuals had higher 1-year non-problem use outcomes (40% versus 23%) than did untreated individuals. Overall, these studies suggest that, especially among individuals who recognize their alcohol problems, treated individuals achieve higher remission rates than do untreated individuals.
Much less attention has been paid to relapse rates among individuals who achieve short-term remission. In treated samples, estimated long-term relapse rates have varied between 20 and 80% [9,10]. However, as far as we know there is no prospective information about relapse rates for individuals who achieve short-term remission without obtaining help. In earlier work on the sample we focus on here, obtaining help relatively quickly was associated with more improvement in drinking patterns and problems [11]. Here, we compare 3-year remission rates and subsequent 16-year relapse rates for individuals who did versus those who did not enter treatment or Alcoholics Anonymous (AA) in the first year after seeking help. We also estimate the proportion of individuals who do not obtain help in the first year but enter treatment or AA subsequently, and examine whether obtaining help affects their remission or relapse rates.
Predictors of short-term remission
Three sets of factors have been associated with short-term remission among treated and untreated individuals: (1) demographic and life history factors, (2) drinking patterns and related indices of functioning and (3) life context and coping indices.
Demographic and life history factors
In treated samples, women and older, married and bettereducated individuals tend to experience better short-term outcomes [12-14]. We have not identified previous studies of demographic predictors of remission among untreated individuals. However, compared to untreated individuals with active alcohol use disorders, untreated remitted individuals are older and more likely to be women, married and employed and have a later onset of alcohol problems [15-17]. Compared to individuals who remitted with help, those who remitted without help tend to be more socially stable and to have had fewer life-time drinking problems [18,19].
Drinking patterns and related indices of functioning
Among both treated and untreated individuals, more frequent and heavier alcohol consumption and more psychological and social drinking problems are associated with a lower likelihood of remission [3,13,16]. In contrast, self-efficacy to resist alcohol consumption in high-risk situations is associated with a higher likelihood of remission [20-22]. Compared to individuals who remit with help, those who remit without help tend to consume less alcohol and to have less severe drinking problems [23,24].
Life context and coping
More social resources, especially supportive relationships with family members and friends, are associated with both treated and untreated remission [15,25,26]. More reliance on approach coping and less on avoidance coping also is linked to a higher likelihood of remission [27-29]. In addition, compared to individuals who remit with help, those who remit without help tend to have more supportive family relationships and to rely less on avoidance coping [20,30].
In earlier analyses based on this sample, we identified baseline predictors of overall 1-year non-remission [31]. Here, we focus separately on groups of individuals who did versus those who did not obtain help and examine baseline predictors of 3-year remission and potential differential predictors of remission in these two groups.
Predictors of relapse among remitted individuals
Cross-sectional studies of individuals who attained remission without help suggest that long-term recovery is enhanced by maintenance factors, such as high self-efficacy, more reliance on approach and less on avoidance coping, support from family members and friends, and positive life events [18,32-35]. The relative absence of these maintenance factors should increase the risk of relapse; however, we do not know of prospective studies on this issue among individuals who remitted without help.
Among treated individuals, more severe alcohol-related problems and depressive symptoms, lack of self-efficacy and poor coping skills have been associated with short-term relapse [36-39]. In general, these predictors are consistent with Marlatt & Gordon’s [40] model of relapse, which focuses on the role of low self-efficacy and lack of effective coping skills as risk factors for relapse.
In earlier analyses based on this sample, we identified 1-year risk factors for overall 8-year non-remission [31]. Here, we focus separately on groups of individuals who achieved 3-year remission with or without help and, among these remitted individuals, examine overall predictors of 16-year relapse and potential differential predictors in the two groups.
METHODS
Sample and procedure
The participants were individuals with alcohol use disorders who, at baseline, had not received previous professional treatment for this disorder. These individuals recognized that they had alcohol-related problems and initiated help-seeking, as reflected by an initial contact with the alcoholism treatment system via an Information and Referral (I&R) center or detoxification program. After providing informed consent, 628 eligible individuals completed a baseline inventory described below (for more information about the initial data collection process, see Finney & Moos [41]). Individuals who entered the study had an alcohol use disorder, as determined by one or more substance use problems, dependence symptoms, drinking to intoxication in the past month and/or perception of alcohol abuse as a significant problem.
At 1, 3, 8 and 16 years after entering the study, participants were located and contacted by telephone and asked to complete an inventory that was essentially identical to the baseline inventory. A total of 121 of the 628 baseline participants (19.3%) had died by the 16-year follow-up. Of the remaining 507 individuals, we focus here on the 461 (90.9%) surviving individuals who completed two or more follow-ups or the 16-year follow-up. A total of 88.3%, 83.9%, 87.2% and 87.9% of these individuals completed the 1-year, 3-year, 8-year and 16-year follow-ups, respectively. Compared with the remaining 46 individuals, these 461 individuals were more likely to be women (50.3% versus 32.6%; t = 2.30, P < 0.05) and to be employed at baseline (44.3% versus 21.7%; t = 2.97, P < 0.01).
The 461 individuals were divided almost evenly between women (50.3%) and men (49.7%). Most were Caucasian (80.0%), unmarried (76.4%) and unemployed (55.7%). On average, at baseline, these individuals were in their mid-30s (mean = 33.5; SD = 8.8) and had 13 years of education (mean = 13.1; SD = 2.2) and an annual income of $12 800. They consumed an average of 12.5 ounces of ethanol (SD = 11.2) on a typical drinking day, were intoxicated on an average of 13.0 days (SD = 10.8) in the last month and had an average of 5.0 dependence symptoms (SD = 2.9) and 4.8 drinking problems (SD = 2.4). These characteristics are broadly comparable to those of individuals in treatment for alcohol use disorders in publicly funded programs in the local geographical area, except that the present sample is younger, somewhat better educated and has a higher proportion of Caucasians and women.
At each follow-up, participants were asked whether or not they had obtained professional treatment for their alcohol problems or had participated in AA at any time since they completed the last follow-up. We divided the 461 participants into two groups on the basis of their help-seeking in the first year: (1) the no help group (n = 99) was composed of individuals who did not enter treatment or AA; and (2) the helped group (n = 362) was composed of individuals who participated in treatment and/or AA. Of these individuals, 89 participated only in AA and 273 obtained treatment (with or without AA). Individuals who participated only in AA and those who entered treatment were comparable at baseline and achieved comparable 3-year and 16-year remission rates; accordingly, these two groups were combined [42].
Measures
In addition to obtaining demographic and life history information, we assessed respondents’ drinking patterns and problems, psychosocial functioning and life context and coping factors at baseline and each follow-up. We asked participants about the age they first recognized their drinking problem, life-time drinking problems, based on 27 items that reflected Diagnostic and Statistical Manual version III (revised) (DSM-III-R) symptoms of alcohol abuse and dependence (alpha = 0.94 [43]), and whether they had previously tried to cut down on drinking.
Drinking patterns and problems
Frequency of alcohol consumption was assessed by responses to three questions asking how often per week (never, less than once, once or twice, three to four times, nearly every day) participants consumed typical amounts of wine, beer and hard liquor in the last month. Quantity of alcohol consumption was assessed by three items that asked about the largest amount of wine, beer and hard liquor consumed on any one day in the last month. We converted the responses to reflect the ethanol content of these beverages and then summed them.
An index of current drinking problems was drawn from the Health and Daily Living form (HDL [44]). Respondents rated how often (on a five-point scale varying from 0 = never to 4 = often) in the last 6 months they had experienced each of nine problems (e.g. with health, job, money, family arguments) as a result of drinking (alpha at baseline = 0.80). Collaterals and participants showed significant agreement at baseline on this index [41]. In addition, we asked participants about whether they thought they had a significant drinking problem, as rated on a five-point scale from ‘no problem’ to ‘serious problem’.
To be considered remitted, individuals had to meet several criteria by the 3-year follow-up: abstinence from alcohol or moderate drinking in each of the past 6 months, no drinking problems in the past 6 months and no intoxication or consumption of more than 3 ounces of ethanol on drinking days in the past month. Initially, remitted individuals who did not meet these criteria at the 8-year and/or 16-year follow-ups were considered to be relapsed.
Psychosocial functioning
Self-efficacy or confidence to resist alcohol consumption was assessed with 10 items (alpha at baseline = 0.93) adapted from the Situational Confidence Questionnaire [45]. The items covered situations involving negative and positive emotions, interpersonal conflict and testing one’s self-control. Each item was rated on a six-point scale varying from not at all confident to very confident; individuals received a score of 1 for each item they rated as very confident.
Depression was based on a measure derived from the research diagnostic criteria and included in the Health and Daily Living form [44]. Respondents rated how often (on a five-point scale with 0 = never and 4 = often) they experienced each of nine symptoms of depression in the last month, such as feeling sad or blue; feeling guilty, worthless, or down; thoughts about death or suicide (alpha at baseline = 0.92). To assess social functioning we asked participants about how many friends they had, as defined by close friends, membership in a circle of close friends, and friends who could be counted on for help when needed.
Life context and coping was assessed by standardized summary measures of chronic stressors and social resources in several life domains, such as spouse/partner, other relatives, finances and work (average alphas at baseline = 0.75 and 0.76 for stressors and resources, respectively). Each of these domains was assessed by several four- or five-point items drawn from the Life Stressors and Social Resources Inventory (LISRES [46]). We also obtained measures of the number out of 38 negative life events and 13 positive life events that had occurred in the last year. Coping was assessed by two six-item subscales, which measured problem solving and avoidance coping (alphas at baseline = 0.75 and 0.59, respectively). The subscales were composed of four-point items ranging from ‘no’ to ‘fairly often’ drawn primarily from the Coping Responses Inventory (CRI [47]). We used a four-point item to tap the individual’s tendency to drink to reduce tension as a coping strategy.
Analytical plan
We employed χ2 analyses to compare the proportion of individuals who attained 3-year remission in the no help versus the helped groups, and to compare subsequent relapse rates among initially remitted individuals. χ2 analyses were also employed to examine whether participation in treatment or AA in years 2 and 3 was associated with 3-year remission and whether such participation in years 4–8 was associated with relapse after remission. We did not examine participation in these modalities of help between 9 and 16 years in order to avoid the possibility of including help received subsequent to relapse, which might have occurred by the 8-year follow-up. To identify predictors of 3-year remission, we conducted two-way analyses of variance (ANOVAs) to examine differences in demographic and life-history factors, and in baseline drinking, functioning and life context and coping indices between helped and non-helped individuals and remitted and non-remitted individuals. We also focused on interactions between the help status and remission status groups.
To identify predictors of 16-year relapse among initially remitted individuals, we conducted two-way ANOVAs to examine differences in demographic, life history and 3-year follow-up indices between individuals in the helped versus no help groups and stably remitted and relapsed individuals. In addition, we examined interactions between the help status and relapse status groups.
We also conducted partial correlation and logistic regression analyses, controlling for help group, to identify independent predictors of 3-year remission and of 16-year relapse among initially remitted individuals. We used a regression-based estimation model [48] and information from baseline and completed follow-ups to impute missing values; as noted earlier, more than 90% of participants completed at least two of the four follow-ups.
RESULTS
Rates of short-term remission and subsequent relapse
By the 3-year follow-up, 62.4% of individuals in the helped group were remitted, compared with only 43.4% of individuals in the no help group (χ2 = 11.54; df = 1; P < 0.01). In the no help group, the proportion of remitted (23.3%) and non-remitted (35.7%) individuals who delayed entry but then participated in treatment and/or AA in years 2 and 3 did not differ significantly (χ2= 2.79; df = 1; NS). Similarly, in the helped group, there was no significant difference in the proportion of remitted (63.3%) and non-remitted (62.5%) individuals who were involved in treatment and/or AA in years 2 and 3 (χ2 < 1; df = 1; NS). Thus, the receipt of treatment or AA subsequent to the first year was not associated with remission.
By the 16-year follow-up, 60.5% of the 3-year remitted individuals in the no help group had relapsed, compared with 42.9% of 3-year remitted individuals in the helped group (χ2 = 4.48; df = 1; P < 0.05). In the no help group, only 3.8% of relapsed individuals and 5.0% of continuously remitted individuals participated in treatment and/or AA in years 4–8 (χ2 < 1; df = 1; NS). In the helped group, 13.4% of relapsed individuals and 12.4% of continuously remitted individuals had some additional involvement in treatment and/or AA in years 4–8 (χ2 < 1; df = 1; NS).
Predictors of short-term remission
Compared to individuals who did not achieve remission by the 3-year follow-up, those who did were more likely to be women and to be married, were older and had more education and were older when they first recognized their drinking problem. At baseline, they consumed alcohol less heavily, had fewer current drinking problems and reported more self-efficacy and less avoidance coping (Table 1).
Table 1.
Demographic and life history, alcohol-related functioning, and social context and coping indices at baseline for help and 3-year remission groups.
| No help group | Helped group | ||||||
|---|---|---|---|---|---|---|---|
| Index | Remit
(n = 43) |
Non-remit
(n = 56) |
Remit
(n = 226) |
Non-remit
(n = 136) |
Help
group |
Remit
group |
Interaction |
| Demographic factors | |||||||
| Gender (% female) | 53.5 | 28.6 | 57.1 | 47.1 | 4.03* | 7.97** | 1.72 |
| Age (years) | 35.9 | 30.1 | 34.4 | 32.7 | < 1 | 9.68** | 4.17* |
| Education (years) | 13.1 | 12.4 | 13.4 | 13.0 | 2.86 | 4.70* | < 1 |
| Married (%) | 34.9 | 12.5 | 25.7 | 21.3 | < 1 | 4.26* | 3.44 |
| Employed (%) | 51.2 | 44.6 | 40.7 | 47.8 | < 1 | < 1 | 1.42 |
| Life history | |||||||
| Age recognized drinking problem | 29.0 | 24.4 | 28.0 | 26.7 | < 1 | 6.39* | 2.93 |
| Lifetime drinking problems | 10.0 | 11.8 | 15.8 | 14.5 | 21.21** | < 1 | 3.16 |
| Tried to cut down (%) | 44.2 | 41.1 | 62.4 | 53.7 | 7.28** | 2.51 | < 1 |
| Drinking patterns/problems | |||||||
| Alcohol consumption (frequency) | 5.1 | 5.5 | 5.0 | 5.4 | < 1 | 3.47 | < 1 |
| Alcohol consumption (maximum oz.) | 8.0 | 13.7 | 12.0 | 14.2 | 2.98 | 8.14** | 1.77 |
| Current drinking problems (0–9) | 3.3 | 5.1 | 4.8 | 5.1 | 6.88** | 6.77** | 7.76** |
| Drinking a significant problem (%) | 53.5 | 61.1 | 83.1 | 80.1 | 25.79** | < 1 | 1.24 |
| Psychological/social | |||||||
| Self-efficacy (0–10) | 6.9 | 5.1 | 5.2 | 4.8 | 5.69* | 4.61* | 2.74 |
| Depression (0–36) | 18.0 | 20.5 | 21.6 | 21.2 | 4.36* | < 1 | 2.01 |
| Social functioning (0–11) | 4.6 | 4.5 | 4.0 | 3.9 | 3.23 | < 1 | < 1 |
| Context and coping | |||||||
| Chronic stressors | 48.8 | 49.9 | 50.1 | 50.6 | 1.64 | < 1 | < 1 |
| Negative events (0–38) | 3.5 | 5.3 | 5.0 | 5.1 | 3.87* | 2.94 | 6.20* |
| Social resources | 51.4 | 49.5 | 49.6 | 49.6 | 1.28 | < 1 | 1.74 |
| Positive events (0–13) | 2.1 | 2.1 | 1.8 | 2.0 | < 1 | < 1 | < 1 |
| Problem solving (0–18) | 9.6 | 10.0 | 9.7 | 9.5 | < 1 | < 1 | < 1 |
| Avoidance (0–18) | 6.8 | 10.2 | 8.9 | 9.0 | < 1 | 4.44* | 14.98** |
| DrInk to reduce tension (%) | 69.8 | 98.2 | 81.8 | 86.7 | < 1 | 8.53** | 7.97** |
Chronic stressors and social resources are standardized indices with mean = 50 and SD = 10.
P < 0.05;
P < 0.01.
There were some interactions between the help groups and the baseline variables in predicting remission (Table 1). Less severe problems (fewer current drinking problems and fewer negative life events) and better coping skills (less avoidance coping and drinking to reduce tension) were more predictive of remission in the no help than in the helped group. Moreover, compared to individuals who remitted with help, individuals who remitted without help had fewer problems or more resources on each of these indices.
Predictors of relapse after remission
Compared to individuals who remained remitted, those who relapsed by the 16-year follow-up had less education, were less likely to have been employed, had more life-time drinking problems and were less likely to have previously tried to reduce their drinking (Table 2). At the 3-year follow-up, the then-remitted individuals who subsequently relapsed consumed alcohol more frequently and heavily, were less likely to see their drinking as a significant problem, had less self-efficacy to resist alcohol consumption and were more likely to drink to reduce tension (Table 2).
Table 2.
Demographic and life history, alcohol-related functioning, and social context and coping indices at 3-year follow-up for help and 16-year relapse groups.
| No help group | Helped group | ||||||
|---|---|---|---|---|---|---|---|
| Index | Remit
(n = 17) |
Relapse
(n = 26) |
Remit
(n = 129) |
Relapse
(n = 97) |
Help
group |
Relapse
group |
Interaction |
| Demographic factors | |||||||
| Gender (% female) | 41.2 | 61.5 | 59.7 | 53.6 | < 1 | < 1 | 2.46 |
| Age (years) | 38.2 | 34.3 | 34.9 | 33.7 | 1.32 | 2.19 | < 1 |
| Education (years) | 13.7 | 12.8 | 13.6 | 13.0 | < 1 | 5.54* | < 1 |
| Married (%) | 47.1 | 26.9 | 24.8 | 26.8 | 1.61 | < 1 | 2.15 |
| Employed (%) | 64.7 | 42.3 | 47.3 | 32.0 | 2.64 | 7.40** | < 1 |
| Life history | |||||||
| Age recognized drinking problem | 31.9 | 27.0 | 28.3 | 27.5 | < 1 | 1.67 | 1.67 |
| Life-time drinking problems | 9.7 | 10.1 | 18.3 | 12.5 | 16.36** | 27.89** | 5.98* |
| Tried to cut down (%) | 35.3 | 50.0 | 75.2 | 45.4 | 3.24 | 15.54** | 7.79** |
| Drinking patterns/problems | |||||||
| Alcohol consumption (frequency) | 0.9 | 2.6 | 0.4 | 1.3 | 11.26** | 23.15** | 2.31 |
| Alcohol consumption (maximum oz.) | 0.5 | 2.1 | 0.7 | 1.6 | < 1 | 7.05** | < 1 |
| Drinking a significant problem (%) | 17.6 | 23.1 | 57.4 | 39.2 | 10.37** | 5.92* | 2.08 |
| Psychological/social | |||||||
| Self-efficacy (0–10) | 9.5 | 8.4 | 9.3 | 8.7 | < 1 | 7.43** | < 1 |
| Depression (0–36) | 9.3 | 10.4 | 12.0 | 12.3 | 3.45 | < 1 | < 1 |
| Social functioning (0– 11) | 4.4 | 4.1 | 5.4 | 4.7 | 2.39 | 2.93 | < 1 |
| Context and coping | |||||||
| Chronic stressors | 49.3 | 48.8 | 49.3 | 49.6 | < 1 | < 1 | < 1 |
| Negative events (0–38) | 3.1 | 3.6 | 3.0 | 2.8 | 1.72 | < 1 | < 1 |
| Social resources | 51.9 | 51.1 | 50.9 | 49.5 | 1.81 | 3.17 | < 1 |
| Positive events (0–13) | 2.6 | 2.3 | 2.7 | 2.6 | < 1 | < 1 | < 1 |
| Problem solving (0–18) | 11.3 | 12.5 | 11.9 | 11.5 | < 1 | < 1 | 1.63 |
| Avoidance (0–18) | 3.6 | 4.4 | 4.9 | 4.9 | 2.70 | < 1 | < 1 |
| DrInk to reduce tension (%) | 5.9 | 30.8 | 10.1 | 23.7 | < 1 | 11.55** | < 1 |
Chronic stressors and social resources are standardized indices with overall mean = 50 and SD = 10.
P < 0.05;
P < 0.01.
There were two significant interactions: in the help group, compared to individuals who remained remitted, individuals who relapsed had fewer life-time drinking problems and were less likely to have tried to reduce their drinking before. In the no help group, compared to remitted individuals, relapsed individuals had somewhat more drinking problems and were more likely to have previously tried to reduce their drinking.
Independent predictors of 3-year remission and relapse after remission
To identify independent predictors of remission, we conducted logistic regression analyses using help group status and the indices significantly associated with 3-year remission as predictors (see Table 1). Female gender, older age and less reliance on drinking to reduce tension were independent predictors and accounted for 12% of the variance in remission (Table 3). Controlling for whether or not individuals obtained some help (treatment and/or AA) in years 2 and 3 did not alter these findings.
Table 3.
Alcohol-related functioning and social context and coping predictors of 3-year remission (n = 461) and of 16-year relapse (n = 276).
| 3-Year remission | 16-Year relapse | ||||
|---|---|---|---|---|---|
| Characteristic | Partial corr | Betas | Partial corr | Betas | |
| Help group (1=helped) | – | 0.68** | – | –0.06 | |
| Demographics and life history | |||||
| Gender (1=female) | 0.13** | 0.75** | –0.02 | – | |
| Age | 0.14** | 0.04** | –0.09 | – | |
| Education (years) | 0.10* | – | –0.14** | –0.15** | |
| Employed (1 = yes) | –0.04 | – | –0.17** | –0.71* | |
| Drinking patterns | |||||
| Lifetime Drinking problems | –0.04 | – | –0.31** | –0.08* | |
| Alcohol use (freq) | –0.09 | – | 0.28** | 0.26** | |
| Alcohol use (max) | –0.14** | – | 0.16** | – | |
| Coping | |||||
| Drink to reduce tension | –0.13** | –0.86* | 0.20** | – | |
| Constant | –1.16 | 3.09 | |||
| Nagelkerke R2 | 0.12 | 0.27 | |||
P < 0.05;
P < 0.01.
We conducted comparable logistic regression analyses using help group status and the indices significantly associated with relapse (see Table 2) to identify independent predictors of relapse subsequent to remission. Less education, unemployed status, fewer life-time drinking problems and more frequent alcohol consumption at the 3-year follow-up were independent predictors and accounted for 27% of the variance in relapse (Table 3). When taken by itself, membership in the helped group predicted a lower likelihood of relapse (beta = ;0.71; P < 0.01); however, in the context of the other predictors it was no longer significant. Controlling for whether or not individuals obtained some help (treatment and/or AA) in years 2–8 did not alter these findings.
To find out how well 16-year relapse could be predicted, we constructed a risk for relapse index based on the four risk factors identified in the regression. As shown in Fig. 1, remitted individuals with no risk factors had a 22% likelihood of relapse. The likelihood of relapse rose to 45% for individuals with one risk factor, 70% for individuals with two risk factors and 86% for individuals with three or four risk factors.
Figure 1.
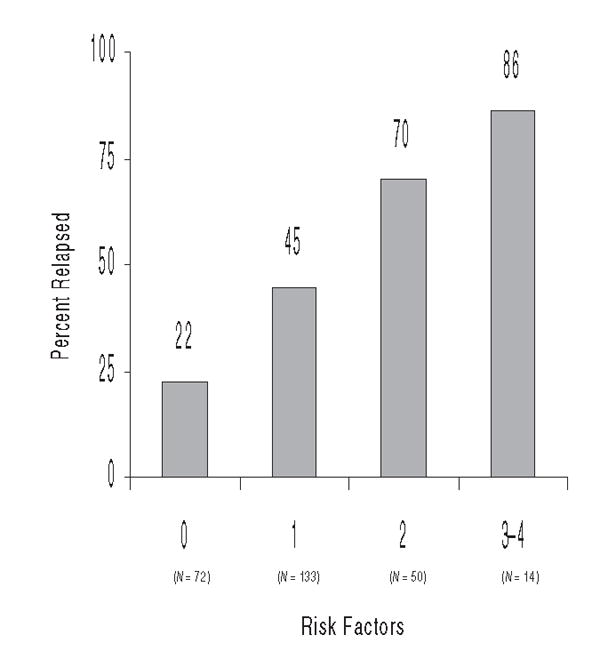
Percentage of initially remitted patients who relapsed by the number of risk factors for relapse
DISCUSSION
Rates of remission and relapse
Consistent with previous research [2,7,8,11], we found lower short-term remission rates among individuals with alcohol use problems who did not participate in treatment or AA soon after initiating help-seeking than among those who did. These results add to growing evidence that participation in treatment and/or AA contributes to better short-term alcohol-related outcomes.
The 62% remission rate in the helped sample is comparable to the 57% that Haver, Dahlgren & Willander [49] found among initially untreated women with alcohol use disorders, but is somewhat higher than the 20–50% rate shown typically in treated samples [1,2]. This finding probably reflects the fact that our sample was composed of individuals who had never been in treatment before and were at a relatively early stage in their alcoholism careers. The 43% remission rate among individuals who did not obtain help quickly is consistent with the rates obtained in prior studies of individuals who were aware of their alcohol problem and sought but did not obtain treatment [3,4].
Compared with individuals who remitted after obtaining help, individuals who remitted without help were more likely to relapse subsequently and, in fact, the relapse rate among these individuals was 60%. This is comparable to but somewhat higher than the 50% rate Klingemann & Aeberhard [50] identified in 7- and 14-year follow-ups of untreated remitted individuals with alcohol use disorders. These findings indicate that the remission rates identified in cross-sectional studies of untreated individuals should be viewed with caution. The relapse rate of just over 40% for individuals who had obtained help and initially remitted is consistent with prior estimates of relapse rates in treated samples [9,10]. Overall, individuals who recognize that they have an alcohol use problem and initiate help-seeking but do not obtain help quickly are at a double disadvantage: they are less likely to achieve remission and, once having achieved remission, may be more likely to relapse.
About 30% of the individuals who did not obtain help in the first year subsequently participated in professional treatment and/or AA. However, consistent with earlier findings on this sample [11,51], obtaining help in a delayed manner was not associated with a higher likelihood of remission or less chance of relapse. Moreover, for individuals who participated in treatment and/or AA in the first year, obtaining additional help later was not associated with altered remission or relapse outcomes. These findings probably reflect a needs-based selection process in which individuals with poorer short-term outcomes are more likely to obtain additional treatment [52].
Predictors of short-term remission
Short-term remission was associated with female gender and older age, and with more personal and social resources such as married status, education and self-efficacy, less severe and chronic alcohol-related involvement and less reliance on avoidance coping. These findings are consistent with previous work on both treated and untreated samples, and indicate that individuals with more ‘social capital’ are likely to show better short-term alcohol-related outcomes [3,13,16,53]. More social pressure to abstain or reduce drinking was associated with a lower likelihood of short-term remission, which may reflect the link between more severe drinking problems and greater social pressure for change [15,20].
Compared to individuals who remitted with help, individuals who remitted without help experienced fewer current drinking problems and negative life events and relied less on avoidance coping and drinking to reduce tension. These findings are consistent with the idea that individuals who improve without formal help have more personal resources and fewer alcohol-related deficits, and that professional treatment and/or AA may provide a compensatory source of support for individuals who lack social capital [18,19,23].
Predictors of relapse after remission
Compared to continuously remitted individuals, four key risk factors characterized initially remitted individuals who later relapsed: less education and a lower likelihood of employed status, more life-time drinking problems and more frequent consumption of alcohol when remitted. A risk factor score composed of these indicators could serve as an early warning sign of the potential for relapse after remission and perhaps trigger preventive or more intensive continuing care. Individuals who relapsed also were less likely to see their drinking as a significant problem, reported less self-efficacy and relied more on drinking to reduce tension. Similarly, in previous studies of treated and untreated individuals, fewer personal resources, such as lack of self-efficacy and coping skills, have been associated with relapse [21,36-38]. These findings support the idea that the likelihood of relapse rises in the absence of personal and social resources that reflect maintenance factors for stable remission [18,34,35].
Fewer life-time drinking problems and no prior attempts to cut down on drinking were associated with a higher likelihood of relapse for individuals in the helped group, but were not associated with relapse for individuals in the no help group. Individuals who have experienced more drinking problems and tried previously to reduce their drinking without success may be more motivated and ready to learn coping skills imparted in treatment and AA that raise the likelihood of achieving a good outcome.
Limitations and future directions
Some limitations of this work should be noted. We conducted a naturalistic study in which individuals selfselected into treatment and AA. Thus, in part, the benefits of help we identified are due to self-selection and motivation to obtain help, as well as to obtaining help per se. We also focused on individuals who had already recognized their alcohol-related problems and initiated a search for help. Accordingly, our findings on lower remission and higher relapse rates among individuals who do not obtain help quickly may not generalize to individuals who have alcohol-related problems but have not sought help. These individuals may have less severe problems and/or more personal and social resources that can help them initiate and sustain natural recovery.
Another limitation is that we obtained information on only 6-month windows of alcohol-related outcomes at each follow-up and thus cannot trace the complete drinking status of respondents over the initial 3-year or the entire 16-year interval. In addition, our data were based on self-report. We obtained some evidence for the validity of respondents’ self-reports at baseline, but did not gather subsequent information from collaterals. However, both treated and untreated individuals’ self-reported alcohol-related outcomes appear to be reasonably valid [54-56]. There also is some support for the reliability of reports of social context factors associated with remission [17,56].
Our findings on the benefits of relatively rapid entry into treatment and/or AA support the value of strengthening the referral process for individuals who recognize their alcohol problems and initiate help-seeking. Assessment of help-seekers’ motivation and readiness for change may help target high-risk individuals for interventions to enhance and maintain participation in treatment [57]. In addition, identification of risk factors for relapse after either treated or untreated remission can help providers target tertiary prevention efforts.
A priority for future research is to find out why individuals who recognize their alcohol problems and initiate help seeking do not obtain timely help. Access to convenient, low intensity interventions [58] could enhance the self-change process and enable such individuals to achieve and maintain remission. Other issues to address include closer examination of the role of prior attempts at self-change in help-seeking and the remission/relapse process, and clarification of whether individuals’ attributions about triggering and maintenance factors for help-seeking and reduced alcohol consumption play more than an epiphenomenal role in treated and natural remission.
Acknowledgments
Preparation of this manuscript was supported in part by NIAAA grant AA12718 and by the Department of Veterans Affairs Health Services Research and Development Service. We thank Bianca Frogner, Ilana Mabel and Christine Stansbury for their help in data collection and Mark Ilgen, John McKellar, Kathleen Schutte and Christine Timko for their helpful comments on an earlier draft of the manuscript. Opinions expressed herein are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
References
- 1.Miller WR, Walters ST, Bennett ME. How effective is alcoholism treatment in the United States? J Stud Alcohol. 2001;62:211–20. doi: 10.15288/jsa.2001.62.211. [DOI] [PubMed] [Google Scholar]
- 2.Monahan S, Finney J. Explaining abstinence rates following treatment for alcohol abuse. A quantitative synthesis of patient, research design, and treatment effects. Addiction. 1996;91:787–805. doi: 10.1046/j.1360-0443.1996.9167876.x. [DOI] [PubMed] [Google Scholar]
- 3.Armor DJ, Meshkoff JE. Remission among treated and untreated alcoholics. Adv Subst Abuse. 1983;3:239–69. [Google Scholar]
- 4.Roizen R, Cahalan D, Shanks P. ‘Spontaneous remission’ among untreated problem drinkers. In: Kandel DB, editor. Longitudinal research on drug use: empirical findings and methodological issues. Washington, DC: Hemisphere; 1978. pp. 197–221. [Google Scholar]
- 5.Blomqvist J. Paths to recovery from substance misuse. change of lifestyle and the role of treatment. Subst Use Misuse. 1996;31:1807–52. doi: 10.3109/10826089609064002. [DOI] [PubMed] [Google Scholar]
- 6.Cunningham JA. Resolving alcohol-related problems with and without treatment: the effects of different problem criteria. J Stud Alcohol. 1999;60:463–6. doi: 10.15288/jsa.1999.60.463. [DOI] [PubMed] [Google Scholar]
- 7.Moyer A, Finney JW. Outcomes for untreated individuals involved in randomized trials of alcohol treatment. J Subst Abuse Treat. 2002;23:247–52. doi: 10.1016/s0740-5472(02)00264-7. [DOI] [PubMed] [Google Scholar]
- 8.Weisner C, Matzger H, Kaskutas LA. How important is treatment? One-year outcomes of treated and untreated alcohol-dependent individuals. Addiction. 2003;98:901–11. doi: 10.1046/j.1360-0443.2003.00438.x. [DOI] [PubMed] [Google Scholar]
- 9.Finney J, Moos R, Timko C. The course of treated and untreated substance use disorders: remission and resolution, relapse and mortality. In: McCrady B, Epstein E, editors. Addictions: a comprehensive guidebook. New York: Oxford University Press; 1999. pp. 30–49. [Google Scholar]
- 10.Jin H, Rourke SB, Patterson TL, Taylor MJ, Grant I. Predictors of relapse in long-term abstinent alcoholics. J Stud Alcohol. 1998;59:640–6. doi: 10.15288/jsa.1998.59.640. [DOI] [PubMed] [Google Scholar]
- 11.Timko C, Finney J, Moos B. Short-term treatment careers and outcomes of previously untreated alcoholics. J Stud Alcohol. 1995;56:597–610. doi: 10.15288/jsa.1995.56.597. [DOI] [PubMed] [Google Scholar]
- 12.Jarvis TJ. Implications of gender for alcohol treatment research: a quantitative and qualitative review. Br J Addict. 1992;87:1249–61. doi: 10.1111/j.1360-0443.1992.tb02734.x. [DOI] [PubMed] [Google Scholar]
- 13.McLellan AT, Alterman AI, Metzger DS, Grissom GR, Woody GE, Luborsky L, et al. Similarity of outcome predictors across opiate, cocaine, and alcohol treatments: Role of treatment services. J Consult Clin Psychol. 1994;62:1141–58. doi: 10.1037//0022-006x.62.6.1141. [DOI] [PubMed] [Google Scholar]
- 14.Ornstein P, Cherepon JA. Demographic variables as predictors of alcoholism treatment outcome. J Stud Alcohol. 1985;46:425–32. doi: 10.15288/jsa.1985.46.425. [DOI] [PubMed] [Google Scholar]
- 15.Bischof G, Rumpf HJ, Hapke U, Meyer C, John U. Factors influencing remission from alcohol dependence without formal help in a representative population sample. Addiction. 2001;96:1327–36. doi: 10.1046/j.1360-0443.2001.969132712.x. [DOI] [PubMed] [Google Scholar]
- 16.Booth BM, Curran GM, Han X. Predictors of short-term course of drinking in untreated rural and urban at-risk drinkers: effects of gender, illegal drug use, and psychiatric comorbidity. J Stud Alcohol. 2004;65:63–73. doi: 10.15288/jsa.2004.65.63. [DOI] [PubMed] [Google Scholar]
- 17.Tucker JA, Vuchinich RE, Gladsjo JA. Environmental events surrounding natural recovery from alcohol-related problems. J Stud Alcohol. 1994;55:401–11. doi: 10.15288/jsa.1994.55.401. [DOI] [PubMed] [Google Scholar]
- 18.Blomqvist J. Treated and untreated recovery from alcohol misuse: environmental influences and perceived reasons for change. Subst Use Misuse. 1999;34:1371–406. doi: 10.3109/10826089909029389. [DOI] [PubMed] [Google Scholar]
- 19.Sobell LC, Cunningham JA, Sobell MB. Recovery from alcohol problems with and without treatment: prevalence in two population surveys. Am J Public Health. 1996;86:966–72. doi: 10.2105/ajph.86.7.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Russell M, Peirce RS, Chan AW, Wieczorek WF, Moscato BS, Nochajski TH. Natural recovery in a community-based sample of alcoholics: study design and descriptive data. Subst Use Misuse. 2001;36:1417–41. doi: 10.1081/ja-100106958. [DOI] [PubMed] [Google Scholar]
- 21.Rychtarik RG, Prue DM, Rapp SR, King AC. Self-efficacy, aftercare, and relapse in a treatment program for alcoholics. J Stud Alcohol. 1992;53:435–40. doi: 10.15288/jsa.1992.53.435. [DOI] [PubMed] [Google Scholar]
- 22.Solomon KE, Annis HM. Outcome and efficacy expectancy in the prediction of post-treatment drinking behavior. Addiction. 1990;85:659–65. doi: 10.1111/j.1360-0443.1990.tb03528.x. [DOI] [PubMed] [Google Scholar]
- 23.Cunningham JA, Lin E, Ross HE, Walsh GW. Factors associated with untreated remissions from alcohol abuse or dependence. Addict Behav. 2000;25:317–21. doi: 10.1016/s0306-4603(98)00130-0. [DOI] [PubMed] [Google Scholar]
- 24.Sobell LC, Sobell MB, Toneatto T. Recovery from alcohol problems without treatment. In: Heather N, Miller N, Greeley J, editors. Self control and the addictive behaviors. New York: Maxwell Macmillan; 1992. pp. 99–242. [Google Scholar]
- 25.Gordon AJ, Zrull M. Social networks and recovery: one year after inpatient treatment. J Subst Abuse Treat. 1991;8:143–52. doi: 10.1016/0740-5472(91)90005-u. [DOI] [PubMed] [Google Scholar]
- 26.Tucker JA, Vuchinich RE, Pukish MM. Molar environmental contexts surrounding recovery from alcohol problems by treated and untreated problem drinkers. Exp Clin Psychopharmacol. 1995;3:195–204. [Google Scholar]
- 27.Chung T, Langenbucher J, Labouvie E, Pandina R, Moos R. Changes in alcoholic patients’ coping responses predict l2-month treatment outcomes. J Consult Clin Psychol. 2001;69:92–100. doi: 10.1037//0022-006x.69.1.92. [DOI] [PubMed] [Google Scholar]
- 28.Moggi F, Ouimette P, Finney J, Moos R. Dual diagnosis patients in substance abuse treatment: relationships among general coping and substance-specific coping and one-year outcomes. Addiction. 1999;94:1805–16. doi: 10.1046/j.1360-0443.1999.941218056.x. [DOI] [PubMed] [Google Scholar]
- 29.Moser AE, Annis HM. The role of coping in relapse crisis outcome: a prospective study of treated alcoholics. Addiction. 1996;91:1101–13. doi: 10.1046/j.1360-0443.1996.91811013.x. [DOI] [PubMed] [Google Scholar]
- 30.Bischof G, Rumpf HJ, Hapke U, Meyer C, John U. Remission from alcohol dependence without help: how restrictive should our definition of treatment be? J Stud Alcohol. 2002;63:229–36. doi: 10.15288/jsa.2002.63.229. [DOI] [PubMed] [Google Scholar]
- 31.Moos R, Moos B. Risk factors for nonremission among initially untreated individuals with alcohol use disorders. J Stud Alcohol. 2003;64:555–63. doi: 10.15288/jsa.2003.64.555. [DOI] [PubMed] [Google Scholar]
- 32.King MP, Tucker JA. Natural resolution of alcohol problems without treatment: environmental contexts surrounding the initiation and maintenance of stable abstinence or moderation drinking. Addict Behav. 1998;23:537–41. doi: 10.1016/s0306-4603(97)00072-5. [DOI] [PubMed] [Google Scholar]
- 33.Rumpf HJ, Bischof G, Hapke U, Meyer C, John U. The role of family and partnership in recovery from alcohol dependence: comparison of individuals remitting with and without formal help. Eur Addict Res. 2002;8:122–7. doi: 10.1159/000059381. [DOI] [PubMed] [Google Scholar]
- 34.Tuchfeld BS. Spontaneous remission in alcoholics: empirical observations and theoretical implications. J Stud Alcohol. 1981;42:626–41. doi: 10.15288/jsa.1981.42.626. [DOI] [PubMed] [Google Scholar]
- 35.Tucker JA. Natural resolution of alcohol-related problems. In: Galanter M, editor. Recent developments in alcoholism, vol. XVI. Research on alcoholism treatment. New York: Kluwer; 2002. pp. 77–90. [DOI] [PubMed] [Google Scholar]
- 36.Brown SA, Vik PW, Patterson TL, Grant I, Schuckit MA. Stress, vulnerability, and alcohol relapse. J Stud Alcohol. 1995;56:538–45. doi: 10.15288/jsa.1995.56.538. [DOI] [PubMed] [Google Scholar]
- 37.Connors GJ, Maisto SA, Zywiak WH. Understanding relapse in the broader context of post-treatment functioning. Addiction. 1996;91:S173–89. [PubMed] [Google Scholar]
- 38.Miller WR, Westerberg VS, Harris RJ, Tonigan JS. What predicts relapse? Prospective testing of antecedent models. Addiction. 1996;91:S155–71. [PubMed] [Google Scholar]
- 39.Yates WR, Booth BM, Reed DA, Brown K, Masterson BJ. Descriptive and predictive validity of a high-risk alcoholism relapse model. J Stud Alcohol. 1993;54:645–51. doi: 10.15288/jsa.1993.54.645. [DOI] [PubMed] [Google Scholar]
- 40.Marlatt GA, Gordon JR, editors. Relapse prevention. New York: Guilford Press; 1985. [Google Scholar]
- 41.Finney J, Moos R. Entering treatment for alcohol abuse: a stress and coping model. Addiction. 1995;90:1223–40. doi: 10.1046/j.1360-0443.1995.90912237.x. [DOI] [PubMed] [Google Scholar]
- 42.Moos R, Moos B. Sixteen-year changes and stable remission among treated and untreated individuals with alcohol use disorders. Drug Alcohol Depend. doi: 10.1016/j.drugalcdep.2005.05.001. in press. [DOI] [PubMed] [Google Scholar]
- 43.Schutte K, Nichols K, Brennan P, Moos R. A 10-year follow-up of older former problem drinkers: risk of relapse and implications of successfully sustained remission. J Stud Alcohol. 2003;64:367–74. doi: 10.15288/jsa.2003.64.367. [DOI] [PubMed] [Google Scholar]
- 44.Moos R, Cronkite R, Finney J. Health and daily living form manual. 2. Palo Alto, CA: Mind Garden; 1992. [Google Scholar]
- 45.Annis HM, Graham JM. Situational confidence questionnaire user’s guide. Toronto: Addiction Research Foundation; 1988. [Google Scholar]
- 46.Moos R, Moos B. Life stressors and social resources inventory: adult form manual. Odessa, FL: Psychological Assessment Resources; 1994. [Google Scholar]
- 47.Moos R. Coping responses inventory: adult form manual. Odessa, FL: Psychological Assessment Resources; 1993. [Google Scholar]
- 48.Hill M. SPSS missing value analysis, version 7.5. Chicago, IL: SPSS; 1997. [Google Scholar]
- 49.Haver B, Dahlgren L, Willander A. A 2-year follow-up of 120 Swedish female alcoholics treated early in their drinking career: Prediction of drinking outcome. Alcohol Clin Exp Res. 2001;25:1586–93. [PubMed] [Google Scholar]
- 50.Klingemann H, Aeberhard M. Biographie und suchtkarrieren 1988;2002. Longitudinale fallanalysen von alcohol-und heroinselbstheiler/innen und -heilern. [[Biographies and addiction careers 1988;2002. Longitudanal case analyses on male and female self-healers]]. Abhaengigkeiten. 2004;2:52–63. [Google Scholar]
- 51.Timko C, Moos R, Finney J, Moos B, Kaplowitz M. Long-term treatment careers and outcomes of previously untreated alcoholics. J Stud Alcohol. 1999;60:437–47. doi: 10.15288/jsa.1999.60.437. [DOI] [PubMed] [Google Scholar]
- 52.Moos R, Moos B. The interplay between help-seeking and alcohol-related outcomes: divergent processes for professional treatment and self-help groups. Drug Alcohol Depend. 2004;75:155–64. doi: 10.1016/j.drugalcdep.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 53.Granfield R, Cloud W. Social context and ‘natural recovery’: the role of social capital in the resolution of drug-associated problems. Subst Use Misuse. 2001;36:1543–70. doi: 10.1081/ja-100106963. [DOI] [PubMed] [Google Scholar]
- 54.Babor TF, Stephens RS, Marlatt A. Verbal report methods in clinical research on alcoholism: response bias and its minimization. J Stud Alcohol. 1987;48:410–24. doi: 10.15288/jsa.1987.48.410. [DOI] [PubMed] [Google Scholar]
- 55.Babor TF, Steinberg K, Anton R, Del Boca F. Talk is cheap: measuring drinking outcomes in clinical trials. J Stud Alcohol. 2000;61:55–63. doi: 10.15288/jsa.2000.61.55. [DOI] [PubMed] [Google Scholar]
- 56.Gladsjo JA, Tucker JA, Hawkins JL, Vuchinich RE. Adequacy of recall of drinking patterns and event occurrences associated with natural recovery from alcohol problems. Addict Behav. 1992;17:347–58. doi: 10.1016/0306-4603(92)90040-3. [DOI] [PubMed] [Google Scholar]
- 57.Marlowe DB, Merikle EP, Kirby KC, Festinger DS, McLellan AT. Multidimensional assessment of perceived treatmententry pressures among substance abusers. Psychol Addict Behav. 2001;15:97–108. doi: 10.1037//0893-164x.15.2.97. [DOI] [PubMed] [Google Scholar]
- 58.Sobell LC, Sobell MB, Leo GI, Agrawal S, Johnson-Young L, Cunningham JA. Promoting self-change with alcohol abusers: a community-level mail intervention based on natural recovery studies. Alcohol Clin Exp Res. 2002;26:936–48. [PubMed] [Google Scholar]


