Abstract
Background
Prenatal exposure to diethylstilboestrol (DES) may induce neurodevelopmental disturbances potentially mediating an increased risk of psychiatric disorders in exposed subjects. Most findings of an increased prevalence of psychiatric disorders in men and women prenatally exposed to DES are not easy to interpret because of selection biases.
Method
Information on hormonal treatment during pregnancy and on offspring’s medical outcome was collected from women participating in the Etude Epidemiologique de Femmes de la Mutuelle Générale de l’Education Nationale (E3N) prospective cohort who completed consecutive postal questionnaires on a range of medical events since 1990. Information on hormonal treatment during pregnancy was collected in 1992 and on offspring’s medical outcome in 2004. The psychiatric outcome of subjects prenatally exposed to DES was compared to that of their unexposed siblings.
Results
A total of 1352 mothers with DES treatment for at least one pregnancy provided information on 1680 exposed children and 1447 unexposed siblings. After adjustment for duration of follow-up, educational level, history of obstetric complication, prenatal exposure to progestagen drugs or other hormones and parental history of psychiatric hospitalization, no association was found between prenatal exposure to DES and occurrence of strictly defined serious psychiatric outcome (suicide or psychiatric hospitalization) [adjusted odds ratio (OR) 0.8, 95% confidence interval (CI) 0.5–1.2], or of broadly defined serious psychiatric outcome (same events plus psychiatric or psychological consultation) (adjusted OR 1.0, 95% CI 0.8–1.2).
Conclusions
These findings suggest that the impact of prenatal DES exposure on foetal brain development, if any, is unlikely to increase the risk of serious psychiatric disorders.
INTRODUCTION
There is accumulating evidence that subjects with perinatal exposure to environmental events disturbing neurodevelopment are at increased risk of psychiatric disorders (Murray & Lewis, 1987; Cannon et al. 2003; Verdoux, 2004). Few studies have investigated the impact of prenatal exposure to synthetic hormones on psychiatric outcome. However, intra-uterine levels of oestrogens affect foetal brain development, particularly cerebral lateralization (Geschwind & Galaburda, 1985). Synthetic oestrogens (or xeno-oestrogens) have a non-steroidal structure and do not bind to peripheral alphafoetoprotein, a mechanism preventing entry into the foetal central nervous system; unlike endogenous oestrogens, they do not convert to oestrone, a metabolite of low oestrogenic activity (Schachter, 1994). Hence, high concentrations of active xeno-oestrogens reach the foetal brain with potential deleterious consequences on brain development (Slikker et al. 1982). Animal studies have shown that rodents prenatally exposed to xeno-oestrogens such as diethylstilboestrol (DES) or ethynyloestradiol present with a range of behavioural abnormalities (Porrini et al. 2005). Human studies suggest that DES may impact on the neurodevelopmental lateralization process. An excess of left-handedness in women with prenatal exposure to DES has been reported by several studies (Schachter, 1994; Scheirs & Vingerhoets, 1995; Smith & Hines, 2000), although this finding was not supported by others (Titus-Ernstoff et al. 2003); yet other studies found an excess of left-handedness in men with prenatal exposure to DES (Reinisch & Sanders, 1992; Titus-Ernstoff et al. 2003).
Considering that abnormal lateralization may be implicated in the pathophysiology of psychiatric disorders (Crow et al. 1996; Orr et al. 1999), DES-induced neurodevelopmental disturbances may potentially mediate an increased risk of psychiatric disorders in exposed subjects. Contradictory findings have been reported by previous studies exploring this issue (Vessey et al. 1983; Meyer-Bahlburg et al. 1985; Ehrhardt et al. 1987; Fried-Cassorla et al. 1987; Gustavson et al. 1991; Pillard et al. 1993; Titus-Ernstoff et al. 2003).
Although DES is no longer prescribed, its impact on psychiatric outcome should be clarified, considering the numerous subjects prenatally exposed to DES up to the 1970s (around 8 000 in UK, more than 150 000 in the Netherlands and in France and nearly 5 million in the USA; Palmlund et al. 1993). Furthermore, because of the persisting risk of prenatal exposure to environmental xeno-oestrogens (Newbold, 2004), DES studies are of value as a model of exposure to these substances. We investigated, in the French prospective cohort Etude Epidemiologique de Femmes de la Mutuelle Générale de l’Education Nationale (E3N), whether psychiatric outcome differed between subjects prenatally exposed to DES and their unexposed siblings.
METHOD
Sample
Participants were mothers of a subgroup of the E3N cohort who completed questionnaires about their children for the present study. The E3N was initiated in 1990 to study risk factors for cancer in women (Clavel-Chapelon, 2002; Romieu et al. 2003; Fournier et al. 2005; Tehard et al. 2005). At baseline, the cohort included 97 995 women fulfilling the following inclusion criteria: (i) born between 1925 and 1950; (ii) covered by the national health insurance plan for French teachers (MGEN); and (iii) giving written informed consent to participate in the investigation. Information on a range of medical events is collected using postal questionnaires approximately every 24 months since 1990.
The process for subject selection included in the present study is presented in Fig. 1. Information on hormonal treatments during pregnancy was collected in the 1992 questionnaire sent to the whole cohort and completed by 87.9% of the women included at baseline. From this initial pool, we identified all women still alive who reported giving birth to at least one child exposed to DES in utero. They were sent a postal questionnaire in 2004. The cover letter mentioned only that the aim of the survey was to explore the impact of perinatal events on children’s health. The hypothesis addressed in the present study and the fact that women had been selected on the basis of their prior answer to the DES item were not specified.
FIG. 1.
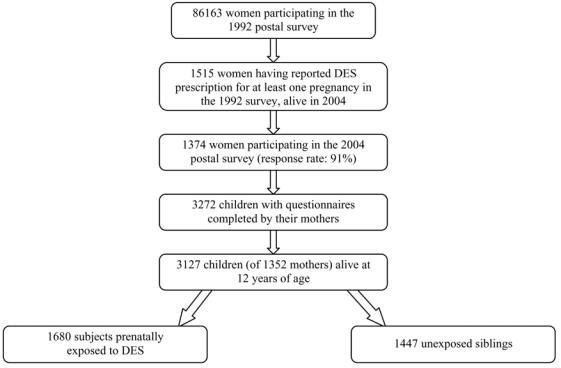
Selection of the subjects prenatally exposed to DES and their unexposed siblings.
Assessment of prenatal exposure to DES and other hormones
According to the information reported by the mother in the 1992 questionnaire, three variables were derived for each child: prenatal exposure to (i) DES; (ii) progestagen drugs; (iii) other hormones. To facilitate accurate recall, a leaflet with colour photographs of the hormonal treatments marketed in France accompanied the questionnaire. The presence or absence of hormonal treatment was recorded, without further information on motive for prescription, dose, duration or stage of pregnancy.
Assessment of child’s outcome
In 2004, the women were asked to complete a questionnaire for each biological child born alive (up to five). Information collected included (i) history of obstetric complications using questions (see Table 1) derived from the Lewis and Murray scale (this scale has been widely used to explore the association between obstetric complications and psychiatric outcome in studies based upon maternal recall; Lewis & Murray, 1987; Verdoux et al. 1997); (ii) demographic characteristics, including cause of death; (iii) reproductive status: parity, history of miscarriage and of difficulties to conceive; if the answer was positive to the latter item, the mother was asked to specify if, to her knowledge, these difficulties were attributable to her child, to her partner, or of unknown origin; nulliparity and difficulties to conceive attributable to her child were categorized as ‘infertility strictly defined’, nulliparity and difficulties to conceive not attributable to the child or of unknown origin were categorized as ‘infertility broadly defined’; (iv) lifetime medical history of hospitalization or consultation with specialists, and age at first hospitalization: women were proposed a list of 15 possible reasons for hospitalization (including psychiatric hospitalization) and a similar list of speciality names (including consultation with a psychiatrist or a psychologist). We defined two categories of psychiatric outcome: (i) lifetime history of strictly defined serious psychiatric outcome if the mother reported that her son or daughter committed suicide or had been hospitalized in psychiatry; and (ii) lifetime history of broadly defined serious psychiatric outcome including the previous events or a history of consultation with a psychiatrist or a psychologist.
Table 1.
Characteristics of subjects prenatally exposed to DES and their unexposed siblings
| Subjects with prenatal DES exposure n (%) or mean (S.D.) (n=1680) | Siblings without prenatal DES exposure n (%) or mean (S.D.) (n=1447) | |
|---|---|---|
| Demographic characteristics | ||
| Duration of follow-up (years)a | 36.8 (7.4) | 36.5 (5.5) |
| Male gender | 751 (44.7)) | 781 (54.0 |
| Educational level >14 years | 1189 (71.8) | 952 (67.2) |
| Obstetric history | ||
| Definite obstetric complicationb | 1331 (79.2) | 561 (38.8) |
| Prenatal exposure to progestagen | 632 (37.6) | 281 (19.4) |
| Prenatal exposure to other hormones | 87 (5.2) | 75 (5.2) |
| History of maternal or paternal psychiatric hospitalization | 74 (4.4) | 61 (4.2) |
DES, Diethylstilboestrol; S.D., standard deviation.
Age of the children still alive in 2004, or age at the time of death.
At least one definite obstetric complication according to the Lewis and Murray scale (Lewis & Murray, 1987): threatened abortion; antepartum bleeding; severe hypertension requiring hospitalization; caesarean for emergency delivery; breech presentation; premature birth >3 weeks; postmature birth >2 weeks; birthweight <2000 g; incubator used >4 weeks.
In addition, history of hospitalization in the first- and second-degree biological relatives of each child was collected. The above list of medical motives was used. In the present study only information on psychiatric hospitalization was used as a proxy measure of family history of psychiatric disorder. We applied a narrow definition of positive family history of psychiatric disorder, restricted to history of psychiatric hospitalization in the mother or in the biological father.
Statistical methods
We investigated the relationship between exposure to DES and psychiatric outcome overall and after stratification by gender. We also explored the relationship between DES exposure and reproductive status in daughters (history of miscarriage, nulliparity and infertility) to serve as a tool to validate maternal information, as the increased frequency of such events in DES-daughter has been largely documented elsewhere (Kaufman et al. 2000). Finally, we performed a sensitivity analysis to check that removing non-significant variables or modifying correlation structure did not modify the other estimates (results available on request).
Characteristics of the exposed and unexposed children were compared statistically using the χ2 test. Multivariate analyses were performed to assess associations between each outcome of interest and exposure to DES, progestagen drugs or other hormones. The models were adjusted for follow-up duration (calculated as the age for children still alive in 2004 or the age at death), sex, educational level (dichotomized as above or below 14 years), history of obstetric complications and family history of psychiatric hospitalization. All variables except follow-up were treated as binary. Because of the large sample size, model selection was unnecessary, thereby limiting the risk of bias. Separate models were generated for strictly and broadly defined serious psychiatric outcomes. All variables included in the models were specified in the analysis plan blind to the data.
To take into account intra-family correlation, a hierarchical two-level logistic model was used (Watier et al. 1997). The child’s level was embedded in the family level, making it possible to estimate and to take into account correlation between siblings. An exchangeable correlation structure assuming common correlation among all siblings was used. The generalized estimating equations (GEE) approach provided estimates and 95% confidence intervals (CIs). Adjusted odds ratios (aORs) are reported. All tests were two-tailed. Statistical analyses were performed with SAS version 9.1 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Characteristics of the sample
Numbers of respondents and children included in the study are given in Fig. 1. Few data were missing for most items of the questionnaire, limiting a posteriori loss of power; obstetrical complications variables had the highest frequency of missing data (around 10%) but sensitivity analyses with different imputation strategies led to the same results. The mean age of the mothers was 65 years (S.D.=5.8, range 54–80). Only children alive at 12 years of age and without history of psychiatric hospitalization before age 12 were considered, in order to exclude subjects with severe infancy or childhood psychiatric disorders such as mental retardation or pervasive development disorders, because inclusion of these subjects may have contributed to increase the heterogeneity of the spectrum of disorders considered in the psychiatric outcome. The mean duration of follow-up was 36 years (S.D.=6.4, range 12–57) and was 30 years and over for most (90%) children.
The characteristics of the subjects with prenatal DES exposure and of their unexposed siblings are given in Table 1. Irrespective of exposure status, most subjects had a high educational level. Nearly four out of five children prenatally exposed to DES had a history of definite obstetric complications, the most frequent being threatened abortion (69.7% of DES-exposed subjects; 21.4% of unexposed siblings) and antepartum bleeding (41.8% of DES-exposed subjects; 13.5% of unexposed siblings). Statistical tests indicate that both groups are not significantly different for all characteristics except for sex, progestagen exposure and obstetrical complications. These two latter differences were expected because DES was given to pregnant women with a history of prior complicated pregnancy and was often co-prescribed with progestagens.
Prenatal hormonal exposure and psychiatric outcome
In the overall sample, subjects (n=16) who committed suicide had a median age of 27 years [interquartile range (IQR) 23–31, range 18–43]. The median age at first psychiatric hospitalization was 24 years (IQR 20–32, range 13–47). The comparison of psychiatric outcome according to prenatal DES exposure status is given in Table 2.
Table 2.
Psychiatric outcome of subjects prenatally exposed to DES and their unexposed siblings
| Subjects with prenatal DES exposure n (%) | Siblings without prenatal DES exposure n (%) | Adjusted OR (95% CI)a | |
|---|---|---|---|
| Suicide | 9 (0.5) | 7 (0.5) | |
| Psychiatric hospitalization | 60 (3.6) | 55 (3.8) | |
| Strictly defined serious psychiatric outcomeb | 60 (3.6) | 58 (4) | 0.8 (0.5–1.2), p = 0.22 |
| Consultation with a psychiatrist | 194 (11.6) | 147 (10.2) | |
| Consultation with a psychologist | 199 (11.9) | 162 (11.2) | |
| Broadly defined serious psychiatric outcomec | 330 (19.6) | 267 (18.5) | 1.0 (0.8–1.2), p = 0.86 |
DES, Diethylstilboestrol; OR, odds ratio; CI, confidence interval.
Adjusted for duration of follow-up, educational level, history of at least one definite obstetric complication according to the Lewis and Murray scale (Lewis & Murray, 1987) (see Table 1), prenatal exposure to progestagen drugs or other hormones, paternal or maternal history of psychiatric hospitalization.
Suicide or psychiatric hospitalization.
Suicide, psychiatric hospitalization or consultation with a psychiatrist or a psychologist.
Subjects prenatally exposed to DES were not at increased risk of presenting with a lifetime history of suicide or psychiatric hospitalization compared to their unexposed siblings. No association was found between prenatal DES exposure and serious psychiatric outcome broadly defined. Similar findings were obtained in analyses stratified by gender: the occurrence of strictly defined serious psychiatric outcome did not differ between women prenatally exposed to DES and their unexposed sisters (aOR 0.8, 95% CI 0.5–1.4, p = 0.49) or between men exposed to DES and their unexposed brothers (aOR 0.80, 95% CI 0.37–1.67, p = 0.56).
In the model adjusted for DES exposure and other potential confounding factors (see Table 1), no association was found between (i) prenatal exposure to progestagen drugs and serious psychiatric outcome (strictly defined: aOR 1.2, 95% CI 0.8–1.9, p=0.33; broadly defined: aOR 1, 95% CI 0.8–1.2, p = 0.99); (ii) prenatal exposure to other hormones and serious psychiatric outcome (strictly defined: aOR 0.8, 95% CI 0.3–1.8, p = 0.57; broadly defined: aOR 1.2, 95% CI 0.8–1.7, p = 0.41).
Prenatal exposure to hormones and daughters’ obstetrical outcome during adulthood
The frequency of nulliparity did not differ between daughters prenatally exposed to DES compared to their unexposed sisters [n = 229 (27.1%) v. n = 156 (26.6%), aOR 1.1, 95% CI 0.8–1.4, p = 0.52]. A history of miscarriage was more frequently reported in daughters prenatally exposed to DES compared to their unexposed sisters [n = 189 (22.3%) v. n = 97 (16.5%), aOR 1.4, 95% CI 1.1–1.9, p = 0.01]. Significant associations were found between prenatal DES exposure and infertility strictly defined [exposed daughters n = 79 (9.4%) v. unexposed sisters n = 16 (1.7%), aOR 3.4, 95% CI 2.0–6.0, p = 0.0001] or infertility broadly defined [exposed daughters n = 110 (13.1%) v. unexposed sisters n = 42 (7.2%), aOR 2.1, 95% CI 1.4–3.1, p = 0.0001]. No association was found between prenatal exposure to progestagen drugs and nulliparity (aOR 1.1, 95% CI 0.8–1.4, p = 0.55), history of miscarriage (aOR 0.9, 95% CI 0.7–1.2, p = 0.52), and infertility strictly (aOR 1.4, 95% CI 0.9–2.2, p = 0.18) or broadly (aOR 1.2, 95% CI 0.8–1.7, p = 0.36) defined. No association was found between prenatal exposure to other hormones and nulliparity (aOR 1.0, 95% CI 0.6–1.6, p = 0.90), history of miscarriage (aOR 1.1, 95% CI 0.6–2.1, p = 0.77), and infertility strictly (aOR 0.6, 95% CI 0.2–1.8, p = 0.31) or broadly (aOR 1.1, 95% CI 0.5–2.3, p = 0.84) defined.
DISCUSSION
Serious psychiatric outcome did not differ between subjects prenatally exposed to DES and their unexposed siblings. A history of miscarriage and of infertility was more frequent in women prenatally exposed to DES compared to their unexposed sisters.
Strengths and weaknesses
First, memory bias may limit the validity of maternal recall on pregnancy events, particularly medications prescribed during pregnancy. As we have little reason to suspect that this bias differed systematically according to offspring’s psychiatric outcome, such a misclassification may have contributed to reduce the strength of the association. However, information on DES exposure was collected 14 years before the present survey, the mothers were not informed about the aim of this study, and their report of DES impact on their daughters’ obstetric outcome at adulthood was in accordance with the documented genital consequences of DES (Kaufman et al. 2000). Second, mothers may not be fully informed about the psychiatric outcome of their children, such as psychiatric consultation, but it is unlikely that they were not aware of events such as suicide or psychiatric hospitalization, or that they systematically under-reported psychiatric events for DES-exposed subjects compared to their unexposed siblings. However, we cannot exclude a nonsystematic misclassification of broadly defined serious psychiatric outcome that may have attenuated the strengths of the associations. Third, mothers and children were not representative of the general population with regard to educational level, but is it unlikely that educational level modifies the neurodevelopmental impact of prenatal DES exposure. Fourth, no information was available on duration, dose and time of DES exposure during pregnancy, which may have attenuated the strength of the association if these characteristics modify the impact of DES exposure on psychiatric outcome. However, such information was no more available in prior studies reporting an association between DES exposure and increased risk of psychiatric disorders.
The major strengths of the study are the high response rate, the large sample size limiting the risk of type II error, and the fact that most offspring had passed beyond the age of peak incidence of major psychiatric disorders. In particular, for a prevalence of psychiatric disorders around 10% and an intra-family correlation between 0% and 50%, the study had a 80% power to detect a non-adjusted OR between 1.3 and 1.1 respectively.
Interpretation of findings
Studies have reported that the prevalence of psychiatric disorders, particularly depression or eating disorders, is increased in women or men prenatally exposed to DES (Vessey et al. 1983; Meyer-Bahlburg et al. 1985; Gustavson et al. 1991; Pillard et al. 1993). Most of these studies were hampered by selection biases, the sampling procedure selecting, for example, women recruited in DES specialized centres or members of users’ associations (Verdoux, 2002). The only exception was the study by Vessey (1983) using data from a randomized controlled trial performed in the 1950s comparing DES to placebo in 1000 women. Information on the medical outcome of their 660 children was provided in 1977–1982 by their general practitioners (GPs) blind to the exposure status. Subjects prenatally exposed to DES were twice as likely to present with psychiatric disorders, mostly anxiety and depression, compared to their unexposed siblings. Other studies did not report such an association (Ehrhardt et al. 1987; Fried-Cassorla et al. 1987; Titus-Ernstoff et al. 2003). The discrepancy between our findings and those of previous studies showing an excess of psychiatric disorders in subjects prenatally exposed to DES may be explained by the selection biases present in most prior studies. As psychiatric outcome was restricted in the present study to suicide or treatment by mental health professionals, we did not consider most common mental disorders treated at a primary care level, which may explain the difference between our findings and those reported in the study by Vessey et al. 1983.
Compared to prior studies carried out in selected populations or those that did not differentiate psychiatric outcome according to severity level or need for care, the major contribution of the present study is to provide strong evidence that prenatal exposure to DES is not associated with an increased risk of major psychiatric disorder requiring hospitalization or at least consultation with a mental health specialist. Our findings suggest that prenatal DES exposure is unlikely to have a major impact on the development of foetal brain structures implicated in the pathophysiology of serious psychiatric disorders. Nevertheless, this reassuring finding should not obscure the fact that DES-exposed subjects, particularly DES daughters, too often have to cope daily with the psychological distress induced by cancer or the consequences of genital malformations (infertility, foetal loss), and have to be provided with adequate psychological support.
Acknowledgments
We are grateful to the users’ association Union Nationale des Amis et Familles de Malades Psychiques (UNAFAM) for supporting the study logistically. We thank the French League against Cancer, the European Community, the 3M Company, the Mutuelle Générale de l’Education Nationale, and the French Drugs Regulatory Agency (Agence Française de Sécurité Sanitaire des Produits de Santé) for supporting the E3N study financially. We thank Lyan Hoang for collecting the data and for managing the database and Ray Cooke for supervising the English of this manuscript. We acknowledge the reviewers of a prior version of the manuscript for their thoughtful comments.
Contributor Information
Hélène Verdoux, Pharmacoepidemiologie et Evaluation de l'Impact des Produits de Sante Sur les Populations INSERM : U657, Université Victor Segalen - Bordeaux II, Universite Victor Segalen BORDEAUX 178, Rue Leo Saignat 33076 BORDEAUX ,FR.
Jacques Ropers, Agence Française de Sécurité Sanitaire des Produits de Santé AFSSAPS, St Denis,FR.
Dominique Costagliola, Epidémiologie Clinique et Traitement de l'Infection à VIH INSERM : U720, Université Pierre et Marie Curie - Paris VI, Centre de Recherche Inserm PARIS VI 56, Boulevard Vincent Auriol 75625 PARIS CEDEX 13,FR.
Françoise Clavel-Chapelon, Nutrition, hormones et cancer: épidémiologie et prévention INSERM : ERI20, IFR69, Université Paris Sud - Paris XI, EA4045, Institut Gustave-Roussy 39 rue Camille Desmoulins 94805 Villejuif CEDEX,FR.
Xavier Paoletti, Modèles et méthodes de l'évaluation thérapeutique des maladies chroniques INSERM : U738, Université Denis Diderot - Paris VII, Faculté de médecine Paris 7 16, Rue Henri Huchard 75018 Paris,FR.
References
- Cannon M, Kendell R, Susser E, Jones P. Prenatal and perinatal risk factors for schizophrenia. In: Murray R, Jones P, Susser E, Van Os J, Cannon M, editors. The Epidemiology of Schizophrenia. Cambridge University Press; Cambridge: 2003. pp. 74–99. [Google Scholar]
- Clavel-Chapelon F. Differential effects of reproductive factors on the risk of pre- and postmenopausal breast cancer. Results from a large cohort of French women. British Journal of Cancer. 2002;86:723–727. doi: 10.1038/sj.bjc.6600124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crow TJ, Done DJ, Sacker A. Cerebral lateralization is delayed in children who later develop schizophrenia. Schizophrenia Research. 1996;22:181–185. doi: 10.1016/s0920-9964(96)00068-0. [DOI] [PubMed] [Google Scholar]
- Ehrhardt AA, Feldman JF, Rosen LR, Meyer-Bahlburg HF, Gruen R, Veridiano NP, Endicott J, Cohen P. Psychopathology in prenatally DES-exposed females: current and lifetime adjustment. Psychosomatic Medicine. 1987;49:183–196. doi: 10.1097/00006842-198703000-00008. [DOI] [PubMed] [Google Scholar]
- Fournier A, Berrino F, Riboli E, Avenel V, Clavel-Chapelon F. Breast cancer risk in relation to different types of hormone replacement therapy in the E3N-EPIC cohort. International Journal of Cancer. 2005;114:448–454. doi: 10.1002/ijc.20710. [DOI] [PubMed] [Google Scholar]
- Fried-Cassorla M, Scholl T, Borow L, Strassman H, Bowers E. Depression and diethylstilbestrol exposure in women. Journal of Reproductive Medicine. 1987;32:847–850. [PubMed] [Google Scholar]
- Geschwind N, Galaburda A. Cerebral lateralization. Biological mechanisms, associations, and pathology: II. A hypothesis and program for research. Archives of Neurology. 1985;42:521–552. doi: 10.1001/archneur.1985.04060060019009. [DOI] [PubMed] [Google Scholar]
- Gustavson CR, Gustavson JC, Noller KL, O’Brien PC, Melton LJ, Pumariega AJ, Kaufman RH, Colton T. Increased risk of profound weight loss among women exposed to diethylstilbestrol in utero. Behavioral and Neural Biology. 1991;55:307–312. doi: 10.1016/0163-1047(91)90645-7. [DOI] [PubMed] [Google Scholar]
- Kaufman RH, Adam E, Hatch EE, Noller K, Herbst AL, Palmer JR, Hoover RN. Continued follow-up of pregnancy outcomes in diethylstilbestrol-exposed offspring. Obstetrics and Gynecology. 2000;96:483–489. doi: 10.1016/s0029-7844(00)00959-5. [DOI] [PubMed] [Google Scholar]
- Lewis S, Murray R. Obstetric complications, neurodevelopmental deviance, and risk of schizophrenia. Journal of Psychiatry Research. 1987;21:413–421. doi: 10.1016/0022-3956(87)90088-4. [DOI] [PubMed] [Google Scholar]
- Meyer-Bahlburg HF, Ehrhardt AA, Feldman JF, Rosen LR, Veridiano NP, Zimmerman I. Sexual activity level and sexual functioning in women prenatally exposed to diethylstilbestrol. Psychosomatic Medicine. 1985;47:497–511. doi: 10.1097/00006842-198511000-00001. [DOI] [PubMed] [Google Scholar]
- Murray R, Lewis SW. Is schizophrenia a neurodevelopmental disorder? British Medical Journal. 1987;295:681–682. doi: 10.1136/bmj.295.6600.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newbold RR. Lessons learned from perinatal exposure to diethylstilbestrol. Toxicology and Applied Pharmacology. 2004;199:142–150. doi: 10.1016/j.taap.2003.11.033. [DOI] [PubMed] [Google Scholar]
- Orr KG, Cannon M, Gilvarry CM, Jones PB, Murray RM. Schizophrenic patients and their first-degree relatives show an excess of mixed-handedness. Schizophrenia Research. 1999;39:167–176. doi: 10.1016/s0920-9964(99)00071-7. [DOI] [PubMed] [Google Scholar]
- Palmlund I, Apfel R, Buitendijk S, Cabau A, Forsberg JG. Effects of diethylstilbestrol (DES) medication during pregnancy: report from a symposium at the 10th International Congress of ISPOG. Journal of Psychosomatic Obstetrics and Gynecology. 1993;14:71–89. doi: 10.3109/01674829309084432. [DOI] [PubMed] [Google Scholar]
- Pillard RC, Rosen LR, Meyer-Bahlburg H, Weinrich JD, Feldman JF, Gruen R, Ehrhardt AA. Psychopathology and social functioning in men prenatally exposed to diethylstilbestrol (DES) Psychosomatic Medicine. 1993;55:485–491. doi: 10.1097/00006842-199311000-00003. [DOI] [PubMed] [Google Scholar]
- Porrini S, Belloni V, Della Seta D, Farabollini F, Giannelli G, Dessi-Fulgheri F. Early exposure to a low dose of bisphenol A affects socio-sexual behavior of juvenile female rats. Brain Research Bulletin. 2005;65:261–266. doi: 10.1016/j.brainresbull.2004.11.014. [DOI] [PubMed] [Google Scholar]
- Reinisch JM, Sanders SA. Effects of prenatal exposure to diethylstilbestrol (DES) on hemispheric laterality and spatial ability in human males. Hormones and Behavior. 1992;26:62–75. doi: 10.1016/0018-506x(92)90032-q. [DOI] [PubMed] [Google Scholar]
- Romieu I, Avenel V, Leynaert B, Kauffmann F, Clavel-Chapelon F. Body mass index, change in body silhouette, and risk of asthma in the E3N cohort study. American Journal of Epidemiology. 2003;158:165–174. doi: 10.1093/aje/kwg131. [DOI] [PubMed] [Google Scholar]
- Schachter S. Handedness in women with intrauterine exposure to diethystilbestrol. Neuropsychologia. 1994;32:619–623. doi: 10.1016/0028-3932(94)90149-x. [DOI] [PubMed] [Google Scholar]
- Scheirs JG, Vingerhoets AJ. Handedness and other laterality indices in women prenatally exposed to DES. Journal of Clinical and Experimental Neurophysiology. 1995;17:725–730. doi: 10.1080/01688639508405162. [DOI] [PubMed] [Google Scholar]
- Slikker W, Jr, Bailey JR, Newport D, Lipe GW, Hill DE. Placental transfer and metabolism of 17 alphaethynylestradiol-17 beta and estradiol-17 beta in the rhesus monkey. Journal of Pharmacology and Experimental Therapeutics. 1982;223:483–489. [PubMed] [Google Scholar]
- Smith LL, Hines M. Language lateralization and handedness in women prenatally exposed to diethylstilbestrol (DES) Psychoneuroendocrinology. 2000;25:497–512. doi: 10.1016/s0306-4530(00)00005-6. [DOI] [PubMed] [Google Scholar]
- Tehard B, Kaaks R, Clavel-Chapelon F. Body silhouette, menstrual function at adolescence and breast cancer risk in the E3N cohort study. British Journal of Cancer. 2005;92:2042–2048. doi: 10.1038/sj.bjc.6602620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titus-Ernstoff L, Perez K, Hatch EE, Troisi R, Palmer JR, Hartge P, Hyer M, Kaufman R, Adam E, Strohsnitter W, Noller K, Pickett KE, Hoover R. Psychosexual characteristics of men and women exposed prenatally to diethylstilbestrol. Epidemiology. 2003;14:155–160. doi: 10.1097/01.EDE.0000039059.38824.B2. [DOI] [PubMed] [Google Scholar]
- Verdoux H. Long-term psychiatric and behavioural consequences of prenatal exposure to psychoactive drugs [in French] Therapie. 2002;57:181–185. [PubMed] [Google Scholar]
- Verdoux H. Perinatal risk factors for schizophrenia: how specific are they? Current Psychiatry Reports. 2004;6:162–167. doi: 10.1007/s11920-004-0060-6. [DOI] [PubMed] [Google Scholar]
- Verdoux H, Geddes J, Takei N, Lawrie S, Bovet P, Eagles J, Heun R, McCreadie R, McNeil T, O’Callaghan E, Stöber G, Willinger U, Wright P, Murray R. Obstetric complications and age at onset in schizophrenia. An international collaborative meta-analysis of individual patient data. American Journal of Psychiatry. 1997;154:1220–1227. doi: 10.1176/ajp.154.9.1220. [DOI] [PubMed] [Google Scholar]
- Vessey MP, Fairweather DV, Norman-Smith B, Buckley J. A randomized double-blind controlled trial of the value of stilboestrol therapy in pregnancy: long-term follow-up of mothers and their offspring. British Journal of Obstetrics and Gynaecology. 1983;90:1007–1017. doi: 10.1111/j.1471-0528.1983.tb06438.x. [DOI] [PubMed] [Google Scholar]
- Watier L, Richardson S, Hemon D. Accounting for pregnancy dependence in epidemiologic studies of reproductive outcomes. Epidemiology. 1997;8:629–636. doi: 10.1097/00001648-199710000-00003. [DOI] [PubMed] [Google Scholar]


