Abstract
Objective To detect any change in exposure to secondhand smoke among primary schoolchildren after implementation of smoke-free legislation in Scotland in March 2006.
Design Comparison of nationally representative, cross sectional, class based surveys carried out in the same schools before and after legislation.
Setting Scotland.
Participants 2559 primary schoolchildren (primary 7; mean age 11.4 years) surveyed in January 2006 (before smoke-free legislation) and 2424 in January 2007 (after legislation).
Outcome measures Salivary cotinine concentrations, reports of parental smoking, and exposure to tobacco smoke in public and private places before and after legislation.
Results The geometric mean salivary cotinine concentration in non-smoking children fell from 0.36 (95% confidence interval 0.32 to 0.40) ng/ml to 0.22 (0.19 to 0.25) ng/ml after the introduction of smoke-free legislation in Scotland—a 39% reduction. The extent of the fall in cotinine concentration varied according to the number of parent figures in the home who smoked but was statistically significant only among pupils living in households in which neither parent figure smoked (51% fall, from 0.14 (0.13 to 0.16) ng/ml to 0.07 (0.06 to 0.08) ng/ml) and among pupils living in households in which only the father figure smoked (44% fall, from 0.57 (0.47 to 0.70) ng/ml to 0.32 (0.25 to 0.42) ng/ml). Little change occurred in reported exposure to secondhand smoke in pupils' own homes or in cars, but a small decrease in exposure in other people's homes was reported. Pupils reported lower exposure in cafes and restaurants and in public transport after legislation.
Conclusions The Scottish smoke-free legislation has reduced exposure to secondhand smoke among young people in Scotland, particularly among groups with lower exposure in the home. We found no evidence of increased secondhand smoke exposure in young people associated with displacement of parental smoking into the home. The Scottish smoke-free legislation has thus had a positive short term impact on young people's health, but further efforts are needed to promote both smoke-free homes and smoking cessation.
Introduction
Children and young people are particularly vulnerable to the health effects of passive smoking.1 2 3 4 5 Children have smaller airways and greater oxygen demands than adults and therefore higher respiratory rates, coupled with less mature immune,6 nervous, and respiratory systems.5 The main source of exposure to secondhand smoke among children is domestic, usually in the home or the car7 8; the levels of exposure correlate with the prevalence of parental smoking, particularly maternal smoking.9 10 In the home, protection can arise only from voluntary family based restrictions by adults that are likely to be beyond the control of children. However, like adults, children can also be exposed in other contexts, including public places where smoking is allowed,8 yet this is a little studied area.
On 26 March 2006 Scotland followed in the footsteps of the Republic of Ireland, Norway, Malta, Sweden, Italy, Spain, New Zealand, Uruguay, and parts of the United States and Canada and introduced legislation that prohibited smoking in most enclosed public places.11 12 Studies using objective measures, such as salivary cotinine and air quality measures, have found that smoke-free legislation is an effective strategy for reducing secondhand smoke exposure in adults,13 14 15 with associated health benefits such as improvement in respiratory symptoms.16 17 An unintended consequence of smoke-free legislation might be displacement of adult smoking from public places into the home,18 19 thus increasing exposure to secondhand smoke among children living with adults who smoke. Evidence from elsewhere, however, does not support this supposition, as smoke-free legislation has been shown to be associated with an increase in smoke-free homes, a tendency to smoke less, and more successful cessation attempts among adults.20 21 22 We might, therefore, predict a reduction in secondhand smoke exposure among children, especially those who live with parents who smoke. Previous studies have examined the association between children's cotinine concentrations and parental smoking.9 10 23 24 25 26 However, to our knowledge no studies have assessed the impact of smoke-free legislation on children's exposure to secondhand smoke both inside and outside the home.
Here we report results from the changes in child exposure to environmental tobacco smoke (CHETS) study, which is part of a national evaluation of the health, behavioural, sociocultural, and economic impacts of the Scottish smoke-free legislation.27 We examined the impact of the smoke-free legislation on children's exposure to secondhand smoke at a population level. The primary outcome was salivary cotinine concentration as a biomarker of secondhand smoke exposure before and after legislation. Secondary outcomes were children's reports of parental smoking and self reported exposure to secondhand smoke in both public and private locations before and after legislation. In addition, we examined whether any evidence exists for increased parental smoking in the home associated with implementation of the Scottish smoke-free legislation.
Methods
The changes in child exposure to environmental tobacco smoke study has a repeat cross sectional design with objective and self reported measures of exposure to secondhand smoke. Two nationally representative class based surveys of children in their final year of primary school in Scotland (primary 7) were done in the same schools one year apart, before (January 2006) and after (January 2007) smoke-free legislation, to assess changes in exposure to secondhand smoke. The sample size was chosen to have 80% power to detect a 20% difference in mean cotinine concentrations between the survey years. All mainstream local authority and independent primary schools on mainland Scotland were included in the sample frame. The sample frame was proportionally stratified by school type (independent and local authority), mainland education authority, and school size, with implicit stratification by proportion of free school meals (as a proxy for socioeconomic characteristics). We used the same schools in both survey sweeps to reduce variation in outcome variables attributable to sources other than the implementation of the legislation (such as changes in socioeconomic characteristics or urban/rural make up of the sample between years). At around 11 years children have sufficient maturity to be able to complete the necessary questionnaire, but very few (less than 2%) are themselves active smokers,28 29 and they are therefore also unlikely to be exposed to secondhand smoke through peer smoking.
Directors of education in each local education authority gave permission to approach schools. We then approached head teachers to enrol schools. We asked each participating school to select one primary 7 class to take part. Pupils in the selected classes received opt-out parental consent letters before the survey. (In a single school opt-in forms were issued for 2006 and 2007. For one class in 2007 opt-out consent letters were issued after the survey, and post-survey retrospective consent was obtained; two questionnaires were destroyed when consent was not obtained.) We gave all pupils information about the study and the option to withdraw on the day of the survey.
Trained researchers administered the survey in the classroom. Pupils completed an anonymous and confidential questionnaire that included questions on their own smoking status and that of their friends and “parent figures” (defined as parents or step parents who the children reported living with all or most of the time) and recent exposure to tobacco smoke in various public and private locations (full details of questions are in the appendix on www.education.ed.ac.uk/CAHRU/publications.html—follow link to CHETS journal articles). They were not asked about the smoking status of other household members. Children were also asked to provide a saliva sample for testing for cotinine. Under supervision, pupils were asked to place a dental roll in their mouths without touching it with their hands (to reduce the risk of contamination) and hold it between their cheek and gum for at least three minutes, to ensure the collection of a sufficient volume of saliva. Supervising researchers were non-smokers, and samples were stored in a smoke-free environment before analysis.
Cotinine is a major metabolite of nicotine and is a sensitive indicator of the absorption of smoke products.30 Cotinine has a half life of approximately 20 hours, is stable with temperature change, and has high specificity and sensitivity as a biomarker for exposure to nicotine from secondhand smoke.31 We used a salivary cotinine assay to assess secondhand smoke exposure as it has a simple collection procedure, has a longer half life than nicotine, and is specific to tobacco.32 We determined the concentration of salivary cotinine by using capillary gas chromatography with a specific nitrogen/phosphorus detector from a 100 µl sample.33 The assay had a detection limit of 0.1 ng/ml. We excluded pupils who reported being current smokers or who had cotinine concentrations above 15 ng/ml, the accepted cut-off point for active smoking.34
We classified parent figures described by their children as smoking “every day” or “sometimes” as smokers. We restricted analyses involving parental figures' smoking status to pupils who lived in two parent, step parent, or single parent families. We derived the number of smoker parent figures each child lived with (none, one (father figure only), one (mother figure only) or two) on the basis of family structure and reported parental figures' smoking status. Measures for determining family structure and parental figures' smoking status are detailed in the appendix.
We used the family affluence scale to measure socioeconomic status.35 36 The family affluence scale comprises family car ownership, bedroom occupancy, family holidays, and computer ownership. We calculated a final family affluence scale score for each pupil and then split the sample into thirds corresponding to those living in low, medium, and high affluence families.37
Statistical analysis
We used log transformed cotinine values for all analyses, as the distribution of cotinine values was positively skewed. We assigned cotinine values below the limit of detection (0.1 ng/ml) an imputed value randomly sampled from the left tail of a truncated log normal distribution. We report geometric mean cotinine concentrations and their 95% confidence intervals. As individual children within a school class may be more similar with respect to secondhand smoke exposure or other measures than randomly selected children, standard methods of variance estimation (and hence confidence intervals) may underestimate the true variance in the population. Appropriate analyses take account of the complex survey design (stratification and clustering) to produce robust variance estimates. In our analyses, the effect of the survey design was to increase the standard error of estimates by 5-13%. All analyses reported here take account of the survey design and used the survey data analysis option of Intercooled Stata version 9.2.
Univariate analyses to test differences in means or proportions used (design adjusted) t tests or χ2 tests as appropriate. Changes in exposure to secondhand smoke in private and public locations were based on the number of pupils reporting someone smoking in a location versus all other responses (including missing). We used linear regression (taking account of the survey design) to assess the differences in mean cotinine concentrations between survey years, adjusting for age and family affluence. We did a separate linear regression analysis to assess the differences in mean cotinine concentrations before and after legislation by number of parent figures who smoked, again adjusting for age and family affluence, on the basis of a reduced subset of pupils for whom information on smoking status of parent figures was available. In each model we tested possible interaction effects and retained those significant at P<0.05.
Results
Response rates
In total, 116 (68%) of 170 approached schools agreed to take part in the study before the legislation; 111 of the original 116 schools also participated at follow-up in 2007 (65% of originally approached schools). A total of 2559/2991 (86%) pupils completed the self report questionnaire in 2006, and 2424/2836 (85%) pupils completed the questionnaire in 2007. We excluded cases in which information on sex was missing or the pupil was in primary 6 (part of a mixed primary 6/primary 7 class) (27 cases in 2006 and 35 cases in 2007). The final data sets contained 2532 pupil questionnaires and 2403 saliva samples in 2006 and 2389 pupil questionnaires and 2270 saliva samples in 2007. One per cent (n=24) of children surveyed in 2006 and 2% (n=42) in 2007 did not provide a saliva sample. We did not seek reasons for this. Less than one tenth (9.6% in 2006 and 8.3% in 2007) of pupils were absent on the day of the survey. Most absences were due to illness or authorised absence (8.3% in 2006 and 7.1% in 2007), and just over 1% (1.3% in 2006 and 1.2% in 2007) were due to truancy or exclusion. Schools that declined to participate did not have significantly different distributions from participating schools with respect to denomination, urban/rural classification, school size, and proportion of pupils receiving free school meals (used as a school level indicator of socioeconomic deprivation). In each survey, participating schools were representative of Scottish schools with respect to these indicators.
Sample characteristics
Table 1 details the characteristics of the samples. The mean age of pupils, proportion of boys and girls, and proportion of pupils living in each family structure and in each family affluence group were not significantly different before and after legislation. Most pupils in both survey years were classified as non-smokers on the basis of self report and cotinine concentrations below 15 ng/ml.
Table 1.
Description of sample before and after smoke-free legislation in Scotland. Values are numbers (percentages) unless stated otherwise
| Characteristic | 2006 (n=2532) | 2007 (n=2389) |
|---|---|---|
| Mean age (years) | 11.5 | 11.4 |
| Boys | 1289 (50.9) | 1227 (51.4) |
| Family affluence scale*: | (n=2445) | (n=2258) |
| Low | 803 (32.8) | 739 (32.7) |
| Medium | 825 (33.7) | 763 (33.8) |
| High | 817 (33.4) | 756 (33.5) |
| Cotinine confirmed smoking status†: | ||
| Non-smokers | 2339 (92.3) | 2217 (92.8) |
| Smokers | 46 (1.8) | 35 (1.5) |
| Missing‡ | 147 (5.8) | 137 (5.7) |
| Family structure (parent figures that sample lives with): | ||
| Both parents | 1723 (68.0) | 1602 (67.1) |
| Parent and step parent | 240 (9.5) | 229 (9.6) |
| Single mother | 453 (17.9) | 432 (18.1) |
| Single father | 45 (1.8) | 41 (1.7) |
| Other§ | 36 (1.4) | 35 (1.5) |
| Unclassifiable | 17 (0.7) | 33 (1.4) |
| Missing | 18 (0.7) | 17 (0.7) |
*Pupils who reported living in both parent, step, or single parent families only.
†Non-smokers=self reported non-smokers with cotinine concentrations <15 ng/ml; smokers=cotinine concentrations >15 mg/ml regardless of self reported smoking status.
‡Pupils who did not answer the smoking question or have a cotinine concentration assigned to them by the laboratory.
§Pupils who reported to be living in a foster home or children's home or some other arrangement.
Population change in secondhand smoke exposure
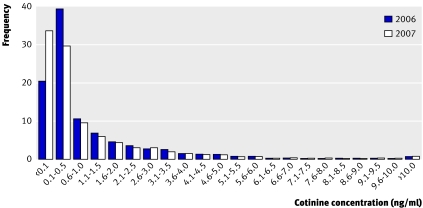
Figure 1 illustrates the distribution of cotinine concentrations before and after legislation. Median cotinine concentration fell from 0.3 ng/ml to 0.2 ng/ml after legislation. The proportion of pupils with cotinine concentration below the limit of detection increased from 20% to 34% after legislation. However, the proportion of pupils with higher cotinine concentrations did not change substantially; for example, the proportion of pupils with cotinine concentrations greater than 1.7 ng/ml changed only slightly from 20% before legislation to 19% after legislation (table 2). We modelled the statistical significance of difference in cotinine concentration before and after legislation by linear regression analysis, adjusting for age and family affluence. The adjusted mean cotinine concentration fell by 39% from 0.36 (95% confidence interval 0.32 to 0.40) ng/ml in 2006 to 0.22 (0.19 to 0.25) ng/ml in 2007.
Fig 1 Distribution of cotinine concentration before and after smoke-free legislation in Scotland (all pupils)
Table 2.
Cotinine concentration distribution and proportion of pupils above each cut-off point before and after smoke-free legislation in Scotland
| Measurement | 2006 (n=2339) | 2007 (n=2217) | Ratio (95% CI) 2007:2006 |
|---|---|---|---|
| Median cotinine concentration (ng/ml) | 0.3 | 0.2 | – |
| Percentage below level of detection (0.1 ng/ml) | 20.5 | 33.9 | – |
| Percentage above cotinine concentration (ng/ml): | |||
| 0.2* | 55.9 | 45.3 | – |
| 0.5 | 40.1 | 36.4 | – |
| 1 | 29.5 | 26.8 | – |
| 1.7* | 20.4 | 19.1 | – |
| 2 | 17.8 | 16.4 | – |
| 3 | 11.3 | 10.1 | – |
| Unadjusted geometric mean (95% CI) cotinine concentration (ng/ml) | 0.35 (0.31 to 0.41) | 0.22 (0.19 to 0.26) | – |
| Geometric mean cotinine (95% CI) concentration (ng/ml) adjusted for age and family affluence | 0.36 (0.32 to 0.40) | 0.22 (0.19 to 0.25) | 0.61 (0.51 to 0.73) |
*Cut-offs used by Kallio et al (2007).40
Table 3 shows reported exposure to secondhand smoke in private and public locations before and after legislation. Self reported exposure to secondhand smoke was higher in private locations than in public locations both before and after legislation. Exposure in pupils' own homes, the most reported location (27.8% in 2006 and 27.4% in 2007), or in a car (6.7% in 2006 and 6.5% in 2007) were similar before and after legislation. In contrast, reported exposure in someone else's home fell after legislation (11.6% in 2006 v 9.5% in 2007, P=0.029). Exposure to secondhand smoke in public places was reported by relatively few pupils before and after legislation, but a decline in exposure between survey years was reported in cafes or restaurants (3.2% in 2006 v 0.9% in 2007, P<0.001) and on buses or trains (1.5% in 2006 v 0.6% in 2007, P=0.015). The small proportion of pupils reporting people smoking in an indoor leisure facility was lower after legislation (2.6% in 2006 v 1.9% in 2007), but the difference was not statistically significant.
Table 3.
Exposure to secondhand smoke in private and public locations before and after smoke-free legislation in Scotland. Values are numbers (percentages)
| Location | Yes, someone was smoking there | No-one was smoking there | I wasn't in this location yesterday | Don't know | Total |
|---|---|---|---|---|---|
| Home (P=0.747*) | |||||
| 2006 | 668 (27.8) | 1550 (64.5) | 27 (1.1) | 159 (6.6) | 2404 |
| 2007 | 622 (27.4) | 1461 (64.3) | 19 (0.8) | 170 (7.5) | 2272 |
| Car (P=0.817*) | |||||
| 2006 | 155 (6.7) | 1448 (62.1) | 678 (29.1) | 49 (2.1) | 2330 |
| 2007 | 144 (6.5) | 1364 (61.3) | 669 (30.1) | 47 (2.1) | 2224 |
| Someone else's home (P=0.029*) | |||||
| 2006 | 266 (11.6) | 599 (26.1) | 1319 (57.5) | 111 (4.8) | 2295 |
| 2007 | 208 (9.5) | 632 (28.9) | 1236 (56.4) | 114 (5.2) | 2190 |
| Cafe or restaurant (P<0.001*) | |||||
| 2006 | 74 (3.2) | 96 (4.1) | 2125 (91.2) | 35 (1.5) | 2330 |
| 2007 | 21 (0.9) | 183 (8.2) | 1982 (89.3) | 33 (1.5) | 2219 |
| Bus or train (P=0.015*) | |||||
| 2006 | 36 (1.5) | 175 (7.4) | 2122 (89.7) | 33 (1.4) | 2366 |
| 2007 | 13 (0.6) | 211 (9.5) | 1972 (88.6) | 30 (1.3) | 2226 |
| Indoor leisure facility (P=0.102*) | |||||
| 2006 | 60 (2.6) | 445 (19.0) | 1709 (73.1) | 124 (5.3) | 2338 |
| 2007 | 41 (1.9) | 487 (22.1) | 1560 (70.8) | 115 (5.2) | 2203 |
*Tests for changes between survey years based on number of pupils reporting someone smoking in a location versus all other responses (including missing); significance levels for design adjusted χ2 analyses shown.
Displacement of parental smoking into the home
In each survey year more than 40% of pupils reported living with a parent figure who smoked. Similar proportions of pupils were in each of the four groups of parental smoking status in each survey year (P=0.314) (table 4).
Table 4.
Geometric mean cotinine concentrations and 95% confidence intervals by number of parent figures who smoke, adjusted for age and family affluence, before and after smoke-free legislation in Scotland
| Parental smoking status | 2006 | 2007 | Ratio (95% CI) of mean cotinine concentration 2007:2006 | P value | |||
|---|---|---|---|---|---|---|---|
| Mean (95% CI) cotinine concentration (ng/ml) | No (%) | Mean (95% CI) cotinine concentration (ng/ml) | No (%) | ||||
| Neither parent figure smokes | 0.14 (0.13 to 0.16) | 1240 (59.6) | 0.07 (0.06 to 0.08) | 1140 (58.3) | 0.49 (0.42 to 0.56) | <0.001 | |
| Father figure only smokes | 0.57 (0.47 to 0.70) | 218 (10.5) | 0.32 (0.25 to 0.42) | 226 (11.6) | 0.56 (0.41 to 0.77) | <0.001 | |
| Mother figure only smokes | 1.38 (1.18 to 1.62) | 309 (14.9) | 1.23 (1.03 to 1.48) | 301 (15.4) | 0.89 (0.71 to 1.13) | 0.314 | |
| Two parent figures smoke | 1.94 (1.71 to 2.21) | 312 (15.0) | 1.74 (1.51 to 2.00) | 287 (14.7) | 0.89 (0.74 to 1.08) | 0.173 | |
| Total | 0.35 (0.32 to 0.38) | 2079 | 0.21 (0.19 to 0.23) | 1954 | 0.60 (0.53 to 0.68) | <0.001 | |
Cotinine confirmed non-smokers.
We used linear regression to assess any differences in mean cotinine concentrations before and after legislation by number of parent figures who smoked (adjusted for age and family affluence). Geometric mean cotinine concentration decreased significantly between survey years, as when all pupils were included (adjusted geometric mean cotinine concentration 0.35 (0.32 to 0.38) ng/ml in 2006 and 0.21 (0.19 to 0.23) ng/ml in 2007, P<0.001), and increased significantly across groups (P<0.001) as the number of parent figures who smoked increased. The only interaction term that reached significance was that between survey year and parent figures in the home who smoked, indicating that the change in cotinine concentrations between years was not equivalent in all groups. Table 4 and figure 2 show the modelled estimates for geometric mean cotinine concentration before and after legislation in each group. Within each of the groups, a fall in geometric mean cotinine concentration occurred after legislation. However, this drop was statistically significant only among groups with lower levels of secondhand smoke exposure. Among pupils of non-smoking parent figures, geometric mean cotinine concentration fell 51% from 0.14 (0.13 to 0.16) ng/ml to 0.07 (0.06 to 0.08) ng/ml. Among pupils with only a father figure who smoked, mean cotinine concentration fell 44% from 0.57 (0.47 to 0.70) ng/ml to 0.32 (0.25 to 0.42) ng/ml. Among pupils living in households with only a mother who smoked or with both parents who smoked, geometric mean cotinine concentration fell 11%, but this was not statistically significant. Use of parental socioeconomic status as an alternative to family affluence in the linear models did not alter the conclusions from the analyses.
Fig 2 Geometric mean cotinine concentrations and 95% confidence intervals before and after implementation of smoke-free legislation in Scotland by number of parental smoking figures, adjusted for age and family affluence (cotinine confirmed non-smokers)
Discussion
Main findings
Our study provides evidence of a population level change in exposure to secondhand smoke among children in their final year of primary school (primary 7) in Scotland after the introduction of smoke-free legislation in March 2006. Overall, secondhand smoke exposure fell by 39% between January 2006 and January 2007, as shown by a significant fall in geometric mean cotinine concentration among children with cotinine confirmed non-smoking status. The extent of this reduction was not equivalent in all groups but differed depending on the smoking status of parent figures in the household. The greatest proportional reduction occurred among pupils living in households with lower levels of secondhand smoke exposure. Although a reduction occurred among pupils with higher levels of secondhand smoke exposure at home, this was relatively small and not statistically significant. For children with no parents who smoke, we conclude that this reduction must be largely due to lower secondhand smoke exposure in public places outside the home.
Using self report data, we found evidence of a reduction in secondhand smoke exposure in public places covered by the legislation, including cafes or restaurants and buses or trains. The fact that some children reported exposure to smoke in these places after legislation does not necessarily imply a breach of the law. Children may simply have seen smoking in the outdoor areas of venues, where smoking would still have been permitted under the legislation.
Among the private locations where pupils are likely to spend time, a fall in reported secondhand smoke exposure when visiting other people's homes occurred after legislation. This finding suggests some modification of smoking behaviour in front of non-family members after the legislation. This could be due to an increased awareness of the health risks associated with exposing others to tobacco smoke or to changing social norms about smoking behaviour. Previous studies have also found that the adoption of smoke-free public places stimulated the adoption of smoke-free homes by adult smokers, increased the frequency of quit attempts, and increased the proportion of successful quit attempts.18 20
However, in this study we found little evidence of a change between survey years in reported exposure in pupils' own homes or in cars. As children were only asked to report on whether smoking took place in the home, rather than the extent of smoking, more subtle changes in smoking levels or practices would not be recorded. The study also found little evidence of differences in the reported prevalence of parental smoking between the two survey years.
This study provides no evidence that the smoke-free legislation has led to displacement of adult smoking from public places into the home and thus increased exposure to secondhand smoke among children who live with adults who smoke.17 18 We found little difference in the reported proportion of parents who smoke or exposure in pupils' own homes and, regardless of parental smoking status, no evidence of an increase in secondhand smoke exposure as measured by cotinine concentration. Instead, we saw a reduction in exposure in all groups, regardless of the number of parent figures in the home who smoked, but this fall was only significant among children who had lower levels of exposure—those with non-smoking parent figures and those with only a father figure who smoked.
Information on secular changes in cotinine concentrations in this age group before legislation is limited. The Scottish health survey collects cotinine data from young people, but findings are based on small numbers in the 11 year old age group.28 In addition, data on cotinine concentrations are aggregated across smokers and non-smokers. However, findings are available for non-smoking 11-15 year olds in England.25 26 For this group overall, mean cotinine concentration fell by 52% over a 15 year period between 1988 and 2003. Most of this decline occurred in the period up to 1996, with a slowdown thereafter. Although a secular change in cotinine concentration was seen in England, perhaps owing to a de-normalising of smoking in public and possibly private places, the change in levels in our study, a 39% fall in cotinine concentration in a single year, is an order of magnitude higher than the average annual change seen in the English studies. This change in Scotland can arguably be attributed to the introduction of the Scottish smoke-free legislation. Our data are also consistent with a study of changes in adult non-smokers' exposure to secondhand smoke associated with the Scottish smoke-free legislation, which has also reported an overall 39% reduction in exposure. As in our study, by far the largest reduction in secondhand smoke exposure occurred in non-smokers living in non-smoking households.38 Similar findings in a US study of non-smoking adults show reductions in serum cotinine concentrations at a national level as states and municipalities have implemented smoke-free legislation.14
Strengths of the study
This study evaluates national legislation and is based on a large nationally representative sample, which permits population level inference. We used an objective measure, salivary cotinine concentration, which is a good indicator of secondhand smoke exposure. This study provides a reliable description of the smoking status of parent figures, making the distinction between absent and lived with fathers, for example. Basing the survey in schools may also have encouraged more honest reporting of parental smoking than if the survey had been done at home with parent figures present in the house.28
Limitations of the study
A longitudinal study design with repeat measures is generally regarded as being more robust, but we chose a repeat cross sectional design, as with a longitudinal design the effects of the smoke-free legislation could not have been disentangled from changes in the likelihood of secondhand smoke exposure associated with behavioural changes owing to pupils maturing. Use of the same schools before and after legislation minimised the variation between years in pupils' characteristics.
The school take-up at baseline was lower than expected given response rates in another national survey among this age group in Scotland.35 This perhaps reflects the different content of the changes in child exposure to environmental tobacco smoke (CHETS) study and the requirement to collect saliva samples. However, we detected no systematic bias in the final sample of schools arising from non-participation.
This study included only children who attended school on the day of the survey in mainstream schools across mainland Scotland. Children who are truanting or excluded from school have a higher likelihood of participating in risky behaviours (such as drinking, drug misuse, and smoking).39 They may also have higher secondhand smoke exposure. However, they represent a small proportion of children in this sample, and our results are based on non-smoking pupils. This small group of children would therefore be unlikely to cause substantive change in the conclusions drawn.
Children were asked only to report secondhand smoke exposure on the day before the survey. Compared with our cotinine validated measures, which reflect secondhand smoke exposure in the previous three to five days, the self report data may underestimate secondhand smoke exposure. However, children's recall of secondhand smoke exposure over a period longer than the previous day is potentially much less reliable.
The study was not designed to measure changes in the number of cigarettes smoked by parental figures, so we cannot ascertain whether this has altered after legislation. However, the observed decrease in geometric mean cotinine concentration among all groups of pupils, regardless of the number of parent figures in the home who smoked, suggests that any increase in the number of cigarettes smoked in the home cannot have been great, as we did not detect an increase in exposure to secondhand smoke among children.
Conclusions
Our study provides evidence that the Scottish smoke-free legislation has made initial and rapid progress towards achieving one of its primary aims—that of promoting health in children by reducing exposure to secondhand smoke—within one year of implementation. Nevertheless, little impact has been made on the higher levels of exposure in the home experienced by children whose mother figure or both parent figures smoke. Although the absolute cotinine concentrations reported here are low relative to those of smokers, for example, health risks are associated with low level exposure to secondhand smoke. Recent research has found that even modest levels of exposure to secondhand smoke (ranging from 0.2 ng/ml to 1.6 ng/ml and from 1.7 ng/ml to 6.8 ng/ml) are associated with only partially reversible arterial abnormalities in children in a dose response manner.40 Nineteen per cent of children in our sample were still exposed to secondhand smoke at a level (≥1.7 ng/ml) that has been shown to be harmful to arterial health. Exposure of children to secondhand smoke thus remains an outstanding public health concern, and our findings underline the importance of continuing to raise awareness of the health risks of passive smoking; supporting adults, especially those living in smoking households, to implement smoke-free policies in their homes and cars; and promoting smoking cessation, particularly among adults who live in households with children. Communication to adults that even low levels of secondhand smoke exposure can pose substantial health risk to children of all ages is particularly important. After implementation of smoke-free legislation, a need now exists to explore approaches to preventing exposure of children to secondhand smoke in the home. This will benefit children's health and help to maximise the potential impacts of the smoke-free legislation.
Further research should explore the longer term impact of the smoke-free legislation on secondhand smoke exposure among children. This should monitor population level changes in exposure to secondhand smoke, as well as observing how exposure changes among children who live with smoking and non-smoking parent figures. Further research should also determine if there are measurable improvements in the health of children after implementation of smoke-free legislation.
What is already known on this topic
Passive smoking poses a significant health risk to adults and children
Smoke-free legislation has been shown to be effective in improving the health and wellbeing of adults
What this study adds
Exposure to secondhand smoke among children in their final year of primary school in Scotland fell after the introduction of smoke-free legislation
This reduction occurred particularly among groups with lower secondhand smoke exposure in the home
No evidence of increased secondhand smoke exposure in young people associated with displacement of parental smoking into the home was found
We thank ABS Labs, London, who analysed salivary cotinine; MVA Consultancy for managing the fieldwork; Scottish local education authorities for granting permission to approach schools under their authority; pupils and teachers of all participating schools; Emily Healy, research administrator, Child and Adolescent Health Research Unit (CAHRU) for providing assistance with this paper; Kate Levin (CAHRU), Joanna Todd (CAHRU), and Rebecca Smith (CAHRU) for providing useful comments on drafts of this paper; and independent reviewers for providing comments on this paper.
Contributors: PCA participated in research design, managed the CHETS survey, prepared study materials, analysed the data, interpreted the data analysis, and led the preparation of drafts of the manuscript. DBC participated in research design, data analysis, interpretation of data analysis, and preparation of drafts of the manuscript. CEC, as principal investigator, is the guarantor. She participated in research design, interpretation of data analysis, and preparation of drafts of the manuscript. SJH participated in research design and preparation of drafts of the manuscript.
Funding: NHS Health Scotland and the Scottish Executive. The study design was developed in discussion with an advisory group that included SJH (NHS Health Scotland). The timing of submission of this paper was agreed with the sponsor, as it would form part of a portfolio of other papers submitted simultaneously. SJH contributed to preparation of the manuscript, but this did not create any conflicts of interest.
Competing interests: None declared.
Ethical approval: School of Education Ethics Committee, University of Edinburgh.
Provenance and peer review: Non-commissioned; externally peer reviewed.
References
- 1.Pattenden S, Antova T, Neuberger M, Nikiforov B, De Sario M, Grize L, et al. Parental smoking and children's respiratory health: independent effects of prenatal and postnatal exposure. Tob Control 2006;15(4). [DOI] [PMC free article] [PubMed]
- 2.Greenberg D, Givon-Lavi N, Broides A, Blancovich I, Peled N, Dagan R. The contribution of smoking and exposure to tobacco smoke to streptococcus pneumoniae and Haemophilus influenzae carriage in children and their mothers. Clin Infect Dis 2006;42:897-903. [DOI] [PubMed] [Google Scholar]
- 3.Weitzman M, Cook S., Auinger P, Florin TA, Daniels S, Nguyen M, et al. Tobacco smoke exposure in associated with the metabolic syndrome in adolescents. Circulation 2005;112:862-9. [DOI] [PubMed] [Google Scholar]
- 4.Yolton K, Dietrich K, Auinger P, Lanphear BP, Hornung R. Exposure to environmental tobacco smoke and cognitive abilities among U.S. children and adolescents. Environ Health Perspect 2005;113:98-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Polanska K, Hanke W, Ronchetti R, Van den Hazel P, Zuurbier M, Kippe JG, et al. Environmental tobacco smoke exposure and children's health. Acta Paediatr 2006;95(suppl 453):86-92. [DOI] [PubMed] [Google Scholar]
- 6.Rees VC, Connolly GN. Measuring air quality to protect children from secondhand smoke in cars. Am J Prev Med 2006;31:363-8. [DOI] [PubMed] [Google Scholar]
- 7.Thaqi A, Franke K, Merkel G, Wichmann H-E, Heinrich J. Biomarkers of exposure to passive smoking of school children: frequency and determinants. Indoor Air 2005;15:302-10. [DOI] [PubMed] [Google Scholar]
- 8.GTTS Collaborative Group. A cross country comparison of exposure to secondhand smoke among youth. Tob Control 2006;15:4-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cook DG, Whincup PH, Jarvis MJ, Strachan DP, Pap Acosta O, Bryant A. Passive exposure to tobacco smoke in children aged 5-7 years—individual, family, and community factors. BMJ 1994;308:384-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jarvis MJ, Russell MAH, Feyerabend C, Eiser JR, Morgan M, Gammage P, et al. Passive exposure to tobacco smoke—saliva cotinine concentrations in a representative population-sample of non-smoking schoolchildren. BMJ 1985;291:927-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Edinburgh: Stationery Office, 2005. Available at Smoking health and social care (Scotland) act 2005. Part 1. Smoking: prohibition and control www.opsi.gov.uk/legislation/scotland/acts2005/20050013.htm
- 12.ASH Scotland. Smoke-free legislation around the world. (accessed 27 Aug 2007).www.ashscotland.org.uk/ash/4264.html
- 13.Semple S, Creely KS, Naji A, Miller BJ, Ayres JG. Secondhand smoke levels in Scottish pubs: the effect of the smoke-free legislation. Tob Control 2007;16:127-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pickett M, Schober SE, Brody DJ, Curtin LR, Giovino GA. Smoke-free laws and secondhand smoke exposure in US non-smoking adults, 1999-2002. Tob Control 2006;15:302-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Allwright S, Paul G, Greiner B, Mullally BJ, Pursell L, Kelly A, et al. Legislation for smoke-free workplaces and health of bar workers in Ireland: before and after study. BMJ 2005;331:1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eagan T, Hetland J, Aarø LE. Decline in respiratory symptoms in service workers five months after a public smoking ban. Tob Control 2006;15:242-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hetland J, Aarø LE. Smokefree restaurants and pubs: air quality, self reported health and job satisfaction. Evaluation of smoking control policies in Norway, 2003-2007 HEMIL/SIRUS report No 4, 2005
- 18.O'Dowd A. Smoking ban in public places also cuts smoking at home. BMJ 2005;331:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hinchliffe D. The government's public health white paper (Cm 6374): minutes of evidence. London: UK Parliament House of Commons Health Committee, 2005. (accessed 22 June 2007).www.parliament.the-stationery-office.co.uk/pa/cm200405/cmselect/cmhealth/358/5022301.htm
- 20.Borland R, Yong H-H, Cummings KM, Hyland A, Anderson S, Fong GT. Determinants and consequences of smoke-free homes: findings from the International Tobacco Control (ITC) four country survey. Tob Control 2006;15:42-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fong G, Hyland A, Borland R, Hammond D, Hastings G, McNeil A, et al. Reductions in tobacco smoke pollution and increases in support for smoke-free public places following the implementation of comprehensive smoke-free workplace legislation in the Republic of Ireland: findings from the ITC Ireland/UK survey. Tob Control 2006;15:51-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Royal College of Physicians. Going smoke-free: the medical case for clean air in the home, at work and in public places. A report on passive smoking by the Tobacco Advisory Group of the Royal College of Physicians London: RCP, 2005 [DOI] [PMC free article] [PubMed]
- 23.Willers S, Axmon A, Feyerabend C, Nielsen J, Skarping G, Skerfving S. Assessment of environmental tobacco smoke exposure in children with asthmatic symptoms by questionnaire and cotinine concentrations in plasma, saliva, and urine. J Clin Epidemiol 2000;53:715-21. [DOI] [PubMed] [Google Scholar]
- 24.Jarvis MJ, Strachan DP, Feyerabend C. Determinants of passive smoking in children in Edinburgh, Scotland. Am J Public Health 1992;82:1225-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jarvis MJ, Goddard E, Higgins V, Feyerabend C, Bryant A, Cook DG. Children's exposure to passive smoking in England since the 1980s: cotinine evidence from population surveys. BMJ 2000;321:343-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Department of Health. Health survey for England. (accessed 22 June 2007).www.dh.gov.uk/en/Publicationsandstatistics/PublishedSurvey/HealthSurveyForEngland/index.htm
- 27.Haw S, Gruer L, Amos A, Currie C, Fischbacher C, Fong GT, et al. Legislation on smoking in enclosed public places in Scotland: how will we evaluate the impact? J Public Health (Oxf) 28(1):24-30. [DOI] [PubMed]
- 28.Bromley C, Sproston K, Shelton N. The Scottish health survey 2003. Volume 3: children. Edinburgh: Scottish Executive, 2005. Available at .www.scotland.gov.uk/Resource/Doc/76169/0019732.pdf
- 29.Godeau E, Rahav G, Hublet A. Tobacco smoking. In: Currie CE, Roberts C, Morgan A, Smith R, Settertobulte W, Samdal O, et al, eds. Young people's health in context: health policy for children and adolescents No 4 Copenhagen, Denmark: WHO Regional Office for Europe, 2004:63-72.
- 30.Jarvis MJ. Application of biochemical intake markers to passive smoking measurement and risk estimation. Mutat Res 1989;222:101-10. [DOI] [PubMed] [Google Scholar]
- 31.Benowitz NL. Cotinine as a biomarker of environmental tobacco smoke exposure. Epidemiol Rev 1996;18:188-204. [DOI] [PubMed] [Google Scholar]
- 32.Jarvis M, Tunstall-Pedoe H, Feyerabend C, Vesey C, Salloojee Y. Biochemical markers of smoke absorption and self reported exposure to passive smoking. J Epidemiol Community Health 1984;38:335-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Feyerabend C, Russell MAH. A rapid gas-liquid chromatographic method for the determination of cotinine and nicotine in biological fluids. J Pharm Pharmacol 1990;42:450-2. [DOI] [PubMed] [Google Scholar]
- 34.Jarvis MJ, Primatesta P, Erens B, Feyerabend C, Bryant A. Measuring nicotine intake in population surveys: comparability of saliva cotinine and plasma cotinine estimates. Nicotine Tob Res 2003;5:349-55. [DOI] [PubMed] [Google Scholar]
- 35.Currie C, Elton RA, Todd J, Platt S. Indicators of socioeconomic status for adolescents: the WHO health behaviour in school-aged children survey. Health Educ Res 1997;12:385-97. [DOI] [PubMed] [Google Scholar]
- 36.Boyce W, Dallago L. Socioeconomic inequality. In: Currie CE, Roberts C, Morgan A, Smith R, Settertobulte W, Samdal O, et al, eds. Young people's health in context: health policy for children and adolescents No 4 Copenhagen, Denmark: WHO Regional Office for Europe, 2004:13-25.
- 37.Batista-Foguet JM, Fortiana J, Currie C, Villalbi JR. Socioeconomic indexes in surveys for comparisons between countries: an applied comparison using the family affluence scale. Soc Indic Res 2004;67:315-32. [Google Scholar]
- 38.Haw SJ, Gruer L. Changes in exposure of adult non-smokers to secondhand smoke after implementation of smoke-free legislation in Scotland: national cross sectional survey. BMJ 2007;doi: 10.1136/bmj.39315.670208.47 [DOI] [PMC free article] [PubMed]
- 39.McAra L. Truancy, school exclusion and substance misuse. Edinburgh Study of Youth Transitions and Crime No 4, University of Edinburgh. (accessed 25 July 2007).www.law.ed.ac.uk/cls/esytc
- 40.Kallio K, Jokinen E, Raitakari OT, Hämäläinen M, Siltala M, Volanenn I, et al. Circulation 2007;115:3205-12. [DOI] [PubMed] [Google Scholar]