Reason for posting: Pioglitazone is an oral hypoglycemic agent widely used as monotherapy or combination therapy for type 2 diabetes mellitus. However, a recent analysis by the drug's manufacturer of several unpublished clinical trials in the company's database revealed an increased risk of bone fracture among pioglitazone users. Health Canada and the drug's manufacturer recently issued a letter warning health care professionals about this potential serious adverse effect.1
The drug: Pioglitazone is a thiazolidinedione (also known as a TZD, or “glitazone”). It binds to and activates peroxisome proliferator-activated receptors (PPAR), including the PPAR gamma and alpha subtypes. These receptors in turn increase glucose utilization and decrease glucose production by the liver, and increase insulin sensitivity in adipose and muscle tissue.
The Health Canada advisory1 was based on an unpublished, manufacturer-led review of double-blind randomized controlled trials of pioglitazone use in diabetic patients. Primary outcome measures in the trials included glycemic control, liver function and vascular events. The trials were not designed specifically to assess fracture risk, and fractures were recorded as adverse events. The doses of pioglitazone used are unclear. Participants in the comparison group were given either a placebo or another diabetic drug (metformin or a sulfonylurea).
Nineteen studies were included in the review. The durations varied from 16 weeks to 3.5 years. No clinically relevant demographic details about the participants were provided (e.g., age, risk factors for osteoporosis), and it is unclear whether the treatment and comparison groups were comparable. In total, 8157 patients received pioglitazone, and 7442 were in the comparison group.
There was no apparent increase in fracture risk among men, but the advisory did not state baseline fracture rates for the treatment or comparison groups. Among women, 2.6% of those in the pioglitazone group experienced fractures, as compared with only 1.7% in the comparison group. This translates to a number needed to harm of 111 patients. The fracture rate was 1.9 fractures per 100 patient-years in the pioglitazone treated group and 1.1 fractures per 100 patient-years in the comparison group. In other words, fractures occurred in 1 of 52 patients taking pioglitazone for a year, as compared with 1 of 90 patients taking either a placebo or another diabetes drug.
Most of the fractures occurred in distal upper and lower limbs and, to a lesser degree, in the hip and spine.2 The specific proportions involving each skeletal location was not stated in the advisory, nor was the severity or the mechanism of the fracture (i.e., trauma v. osteoporosis-related).
Thiazolidinediones have been found to cause bone loss in some rodent models. In humans, their effects may occur because of increased bone marrow adiposity, decreased osteoblast activity, or reduced aromatase activity leading to altered estrogen production and increased bone resorption.2 In a separate prospective observational study, 3075 community-dwelling adults in their 70s were followed for 4 years; thiazolidinedione use was associated with reduced bone mineral density in women but not in men.2
Prospective randomized trials of thiazolidinediones, including pioglitazone, that have bone density or fracture risk, or both, as outcome measures are lacking. It is unclear whether another thiazolidinedione, rosiglitazone, is associated with a similar risk of reduced bone mineral density.
What to do: Use of thiazolidinediones, specifically pioglitazone, may be associated with an increased risk of fracture in women. Women taking pioglitazone should be warned of this adverse event. It is unclear whether the risk of fracture can be mitigated by use of other agents (e.g., bisphosphanates, calcium or vitamin D), and unfortunately a lack of clinical details in the advisory does not allow clinicians to pinpoint women who may be at increased risk of this adverse event.
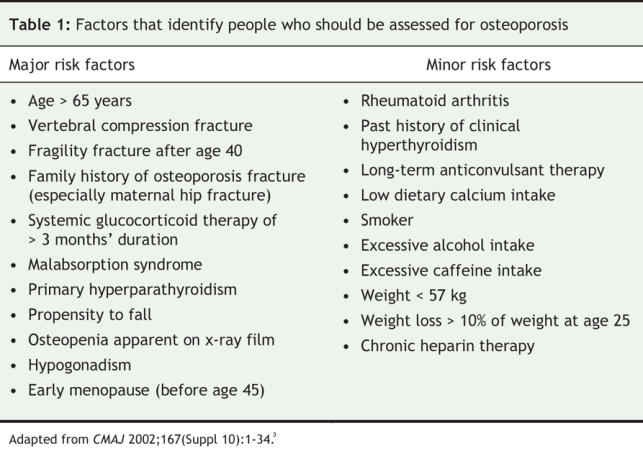
Pioglitazone use can be added to a growing list of risk factors for osteoporosis (Table 1). Close monitoring of bone mineral density in women taking the drug, particularly those with other known risk factors for osteoporosis, may be wise, and alternative therapies might be considered in these women.
Table 1
Reza Heidarpour Meymeh MD Resident Department of Family Medicine University of Ottawa Ottawa, Ont. Eric Wooltorton MD MSc Associate Editor, CMAJ
REFERENCES
- 1.Eli Lilly Canada Inc.; Health Canada. Increased incidence of fractures in female patients who received long-term treatment with ACTOS (pioglitazone hydrochloride) tablets for type 2 diabetes mellitus [letter]. Ottawa: Health Canada; 2007 Apr 18. Available: www.hc-sc.gc.ca/dhp-mps/medeff/advisories-avis/prof/2007/actos_hpc-cps_2_e.html (accessed 2007 20 Aug).
- 2.Schwartz AV, Sellmeyer DE, Vittinghoff E, et al. Thiazolidinedione use and bone loss in older diabetic adults. J Clin Endocrinol Metab 2006;91:3349-54. Epub 2006 Apr 11. [DOI] [PMC free article] [PubMed]
- 3.Brown JP, Josse RG, for the Scientific Advisory Council of the Osteoporosis Society of Canada. 2002 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada. CMAJ 2002;167(Suppl 10):1-34. [PMC free article] [PubMed]


