Abstract
Stathmin (Oncoprotein18), a signal transduction regulatory factor, plays an important role in cell division and malignant tumor development. Stathmin is a ubiquitous intracellular phosphoprotein that is overexpressed in a variety of human malignancies, including osteosarcoma. To investigate the potential use of stathmin as a therapeutic target for human osteosarcomas, we employed RNA interference [small interfering RNA (siRNA)] to reduce stathmin expression in human osteosarcoma cell lines and analyzed their phenotypic changes. Results showed that the downregulation of stathmin expression in human osteosarcoma cells significantly inhibited cell proliferation in vitro and tumorigenicity in vivo. The specific downregulation induced cell arrest in the G2/M phase of cell cycle and eventually apoptotic cell death. Taxanes are a group of effective chemotherapeutic agents whose activity is mediated through stabilization of the microtubules of the mitotic spindle. In the present study, we also observed a synergistic enhancement of the cytotoxicity effect by combination use of taxanes and RNA interference-mediated stathmin downregulation. All these experimental data indicate that stathmin downregulation can lead to potent antitumor activity and chemosensitizing activity to taxanes in human osteosarcomas.
INTRODUCTION
Osteosarcomas, malignant tumors derived from bone tissues, are the most frequently occurring type of bone tumor and are characterized by aggressive invasion, early metastasis, and resistance to existing chemotherapeutic agents (1). To improve the formidable prognosis of osteosarcoma, it is essential to find novel approaches for both diagnosis and treatment that are far more efficient than currently available methods (2). Osteosarcoma employs complex signal transduction systems, some of which remain unclear. Stathmin family phosphoproteins (stathmin, SCG10, SCLIP, RB3/RB3′/RB3″) are important signal transduction molecules and regulators of microtubule dynamics (3). Recent studies have shown that stathmin is expressed at high levels in human osteosarcoma (4). Overexpression of this gene occurs in a number of other human malignancies such as leukemia and lymphoma, prostate carcinoma, ovarian carcinoma, Wilms tumor, breast carcinoma, and adenoid cystic carcinoma of the salivary glands, suggesting the existence of an important oncogene that plays a critical role in maintenance of malignant phenotypes in various human cancers (5–7).
Stathmin was first identified as a 17-kDa cytosolic protein that was rapidly phosphorylated when HL60 leukemic cells underwent terminal differentiation and ceased to proliferate (8). Also known as oncoprotein 18, prosolin, p19, 19K, p18, and op18, stathmin is a conserved cytosolic protein that plays a critical role in mitosis and possibly other cellular processes (9,10). Stathmin has been shown to regulate the dynamics of the microtubules that make up the mitotic spindle, a role associated with carcinogenesis that indicates stathmin is one of the fundamental cancer-associated genes and a potential target for diagnosis and treatment (11,12). Previous studies have shown that manipulations which increase or decrease the level of stathmin expression can interfere with the orderly progression of leukemic cells through the cell cycle (13). Recent studies also demonstrated that stathmin inhibition decreases the rate of proliferation of tumor cells, accumulation in the G2/M phase of the cell cycle, and synergistic interaction with Taxol (14–16). In a previous study, we found that RNA interference (RNAi)-mediated stathmin inhibition could reverse malignant phenotypes of tumor cells (17). In addition, stathmin inhibition has shown tumor-suppressor function in breast cancer cell lines (18) and therapeutic interactions with chemotherapeutic agents in prostate cancer (19). Thus, we believe that stathmin may provide an attractive molecular target for disrupting the mitotic apparatus and arresting the proliferation of malignant cells. In the present study, we employed small interfering RNA targeting stathmin to explore the potential of new therapeutic targets in the treatment of human osteosarcomas. Moreover, we analyzed the synergistic effects on both in vitro and in vivo proliferation of osteosarcoma cells by combined use of taxanes and RNAi-mediated stathmin downregulation. Such synergistic interaction might be relevant for the treatment of osteosarcoma because taxanes and RNAi targeting stathmin are two of the most effective treatment methods for this disease. Thus, this combination may provide a novel strategy of osteosarcoma therapy that avoids toxicities associated with the use of multiple chemotherapeutic agents at full therapeutic doses.
MATERIALS AND METHODS
Maintenance of Cell Lines
Two human osteosarcoma cell lines (Saos-2 and MG63) were cultured in Dulbecco’s modified Eagle’s medium (Invitrogen, Carlsbad, CA, USA) supplemented with 10% fetal bovine serum (Sijiqing, Hangzhou, China), 100 U/mL penicillin, and 100 μg/mL streptomycin. All cells were maintained in an atmosphere of 5% CO2 with humidity at 37 °C.
SiRNA Synthesis
We designed and synthesized double-strand siRNAs in vitro for the stathmin gene with two thymidine residues(dTdT) at the 3′ end of the sequence extending between amino acid residues 398 and 417 (sense, 5′-GAAACGAGAGCACGAGAAA-3′) (15) (AuGCT Biotechnology, Beijing, PRC). We also synthesized a nonspecific siRNA as a control (sense, 5′-GCAAAAGAGCGAAAAG-3′). According to a BLAST database search, the scrambled sequences did not show significant homology to any human mRNA. These RNAs were dissolved in Tris-Cl (pH 8.0) and 1 mM EDTA as 200 μM solutions. Double-strand siRNAs were generated by mixing the corresponding pair of sense and anti-sense RNA oligonucleotides at a concentration of 20 μM in 5 × annealing buffer [30 mM HEPES-KOH (pH 7.4), 100 mM KCl, 2 mM MgCl2, and 50 mM NH4AC]. The reaction mixture was heated to 90 °C for 1 min, gradually cooled down to 37 °C for 60 min, and then aliquoted and stored at −20 °C.
Transient Transfection of siRNA
Two human osteosarcoma cell lines (Saos-2 and MG63) were plated in 10-cm tissue culture plates at approximately 1.0 × 106 cells per well, respectively, and cultured overnight to give 50%–70% confluence prior to transfection. In vitro transfection of RNA oligonucleotides resulting in various RNA concentrations was performed using Lipofectamine2000 transfection reagent (Invitrogen). The cells were harvested at different time points for RT-PCR and Western blot analyses.
Quantitative Real-Time PCR
Total RNA was extracted from cultured cells using Trizol reagent (Invitrogen). RNA of 2 μL (1μg/μL) was used to synthesize cDNA using a Superscript First-Strand Synthesis Kit (Promega, Madison, Wisconsin, USA) following the manufacturer protocols. Expression of stathmin mRNA was detected with the ABI 7700 Sequence Detection System (PE Applied-Biosystems) using specific primers: sense 5′-ATGGCTTCTTCTGATATCCAG-3′ and antisense 5′-TTAGTCAGCTTCAGTCTCGTC-3′. Relative gene expression was quantified, using β-actin as an internal standard.
Western Blot Analysis
A total of 2.0 × 106 cells were harvested and rinsed three times with phosphate-buffered saline (PBS). Cell extracts were prepared with lysis buffer (1 mM dithio-threitol, 0.125 mM EDTA, 5% glycerol, 1 mM phenylmethylsulfonylfluoride, 1 μg/mL leupeptin, 1 μg/mL pepstatin, 1 μg/mL aprotinin, and 1% Triton X-100 in 12.5 mM Tris-HCl buffer, pH7.0) at 4°C for about 30 min. An equal volume of lysate was electrophoresed with SDS polyacrylamide gel electrophoresis (12%). The separated proteins in the gel were transferred to the nitrocellulose membrane. The membranes were blocked for one hour with Tris-buffered saline plus 0.1% Tween-20 (TTBS) containing 5% nonfat milk and then incubated for two hours with the appropriate primary antibodies [anti-stathmin (Santa Cruz Biotechnology, Santa Cruz, CA, USA); anti-β-actin (Sigma, St Louis, MO, USA)] in TTBS containing 5% nonfat milk, followed by incubation for 45 min with horseradish peroxidase-conjugated antimouse immunoglobulin antibodies (Sigma). The immunocomplexes were visualized by enhanced chemoluminescence using an ECL™ kit (Amersham, Piscataway, NJ, USA), followed by exposure to x-ray films.
Cell Proliferation Assay
A total of approximately 6.0 × 103 osteosarcoma cells in 100 μL of the medium were plated in 96-well plates and allowed to attach for 48 h, then treated daily for two days with indicated concentrations of siRNA. After 48 hours of incubation, the medium was replaced with 100 μL of 0.05% 3-[4,5-dimethyl-2-thiazolyl]-2, then 5-diphenyl-2H-tetra-zolium bromide (5 mg/mL) was added to each well and the plate was incubated for four hours at 37 °C. After the incubation, the reaction was stopped by the addition of 150 μL/well of DMSO for 10 min. The absorbance was measured using a VersaMax Tunable Microplate Reader (Molecular Devices, Sunnyvale, CA, USA) with a test wavelength of 570 nm and a reference wavelength of 630 nm; all experiments were performed in triplicate. The cell proliferation curve was plotted using the absorbance at each time point.
Soft Agar Colony Assays
Forty-eight hours after siRNA transfection, the cells were mixed with cell culture medium containing 0.6% agar to a final concentration of 0.4%. We immediately plated 1 mL of this cell suspension in 6-well plates coated with 0.6% agar (1 mL per well) in cell culture medium. The colonies were counted in triplicate 15 d after plating, and the number of colonies per 103 cells was calculated.
Plasmid Constructions
The DNA oligonucleotides coding for the short hairpin short hairpin (sh)stathmin and a nonspecific shRNA negative control (shControl) were designed and synthesized as follows: shstathmin: (5′-GATCCGAAACGAGAGCACGAGAAATTCAAGAGATTTCTCGTGCTCTCGTTTCAGA-3′) and shControl: (5′-GATCCGCAAAAGAGCGAAAAGTTCAAGAGATTTTCGCTCTTTTGCAGA-3′). All these sequences were inserted between BamHI and HindIII restriction sites of pSi-lencer4.1-CMVneo (pSC) vectors (Ambion, Austin, TX, USA). Name designation of the recombinant plasmid was pSC-shstathmin and pSC-shControl. The recombinant vectors were confirmed by the digestion analysis of restriction endonuclease and all inserted sequences were verified by DNA sequencing by TaKaRa Biotech Company using ABI PRISM SigDyeTM Terminator Cycle Sequencing Ready Reaction Kit with AmpliTaq DNA Polymerase FS (Perkin Elmer, Waltham, MA, USA).
Stable Transfection of Plasmids and Selection
Human osteosarcoma cell lines (Saos-2 and MG63) were seeded in 6-well plates at 2.0 × 104 cells/well, respectively, and cultured overnight to about 90% confluence prior to transfection. Then, transfection was performed using Lipofectamine2000 transfection reagent (Invitrogen) following the manufacturer’s specifications. Forty-eight hours after transfection, stable cell lines were selected with G418 (800 μg/mL). Three stably transfected osteosarcoma cell lines (transfected with pSC-shstathmin, pSC-shControl, or pSC-CMVneo parental vector) were established.
Flow Cytometry Analysis of Cell Cycle and Apoptosis
The cells were harvested with trypsinization, fixed with cold 70% ethanol, and stored at 4°C until analyzed. The fixed cells were pelleted and resuspended in PBS containing 20 μg/mL propidium iodide (PI) and RNase A and then analyzed for PI fluorescence intensity by flow cytometry to assess cellular DNA content. The relative proportions of cells in the G1, S, and G2/M phases of the cell cycle were determined from the flow cytometry data. The percentage of apoptotic cells was determined by the sub-G1 proportion. Apoptosis of stable transfectants was also measured with an annexin V-fluorescein isothiocyanate apoptosis detection kit (Zymed; Invitrogen) that was used to detect the cell apoptosis of stable transfectants.
Tumor Formation Assay in Nude Mice
Mouse studies were performed according to institutional guidelines and a protocol improved by the animal research committee. The effect of stathmin downregulation on the tumorigenic capacity was assessed by subcutaneous injection of pSC-shstathmin, pSC-shControl, or pSC-neo parental vector- transfected and untransfected Saos-2 cells into athymic nude mice. Approximately 1.0 × 106 stably transfected cells were injected into eight-week-old female BALB/c nude mice, which were maintained under pathogen-free conditions. The inoculations were performed in 10 mice for one group. Tumor growth from days 7 to 28 after inoculation was monitored, and tumor diameters were measured with a caliper. Tumor volumes (mm3) were calculated by the following formula: V = 1/2 × L2 × W (L, tumor length; W, tumor width). At 28 d after inoculation, all mice were killed, and subcutaneous tumors were resected. Survival tests were made using groups of mice (n = 10) treated as above and monitored daily until all the mice died.
Chemosensitivity Assay
First, cell chemosensitivity in vitro to taxanes (Taxol and Docetaxel; Sigma) was evaluated by MTT analysis; then, 72 hours after transfection, the cells (Saos-2 and MG63) in the 96 wells were treated with various concentrations of Taxol (at 0, 5, 15, 20, and 25 nM) and Docetaxel (at 0, 3, 6, 9, 12, and 15 nM). Cell viability was detected 48 hours later, as described above, and the in vivo tumor sensitivity to taxanes was evaluated in the mouse model. Mice were implanted with 1.0 × 106 Saos-2 cells. Two weeks after implantation, subcutaneous tumors were formed, mice were allocated to 5 groups (10 mice/group), and mice in each group were treated as described in Table 1 (siRNA in 60 μL PBS by tail vein injection and taxanes in 100 μL PBS by intraperitoneal injection thrice weekly). After 10 weeks of treatment, all mice were killed, and subcutaneous tumors were resected. Tumor growth was evaluated by the average volume and the average weight of tumors. The tumor volume was calculated as already described and tumors were weighed. All the animal experiments were performed in accordance with institutional guidelines of the Fourth Military Medical University.
Table 1.
Thrice weekly in vivo chemotherapy regimen (n = 10/group).
| Group Treatment |
|---|
|
Statistical Analysis
All experiments were performed at least in triplicate and all statistical analyses were performed with SPSS10.0. Comparisons among all groups were performed with the one-way analysis of variance (ANOVA) test and Student Newman Keuls method. Values of P < 0.05 were considered significant.
RESULTS
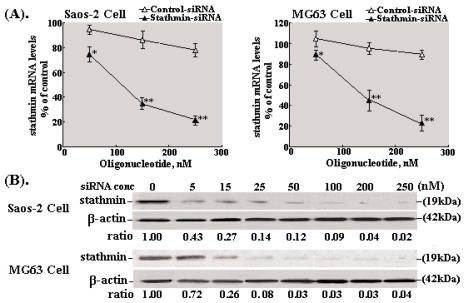
Downregulation of Stathmin Expression by Transient siRNA in Osteosarcoma Cells
We in vitro synthesized 21-mer oligori-bonucleotide targeting stathmin (nucleotide 398–417) and transiently transfected two osteosarcoma cells (Saos-2 and MG63). Real-time RT-PCR (Figure 1A) and Western blot analyses (Figure 1B) were used to determine the effect of treatment with siRNA on stathmin expression at the mRNA and protein levels in osteosarcoma cell lines. As shown in Figure 1A, daily treatment of osteosarcoma cells with 50, 150, and 250 nM stathmin-siRNA for two days reduced stathmin mRNA levels by 16.2%, 53.6%, or 64.3% in Saos-2 cells and by 15.0%, 50.2%, or 78.2% in MG63 cells. As shown in Figure 1B, stathmin protein levels were reduced in a dose-dependent manner, and partial to complete inhibitions were observed with increasing concentrations of the siRNA oligonucleotides.
Figure 1.
Specific downregulation of stathmin mRNA and protein expression by stathmin-siRNA. (A) Cells were transfected daily with 50, 150, or 250 nM Control-siRNA or stathmin-siRNA for 48 hours, and mRNA levels were quantified by real-time PCR analysis. Data were normalized by using β-actin as an internal standard. *P < 0.05 and **P < 0.01 vs. Control-siRNA. (B) Cells were treated daily with various concentrations ranging from 0 to 250 nM for 48 hours. Cells were harvested, and stathmin protein levels were detected by Western blot analysis. β-Actin expression was monitored as the control. The ratio of stathmin/β-actin was calculated by using densitometry, and values were normalized by dividing by the ratio at no treatment (0 nmol/L). *P < 0.05 vs. control-siRNA.
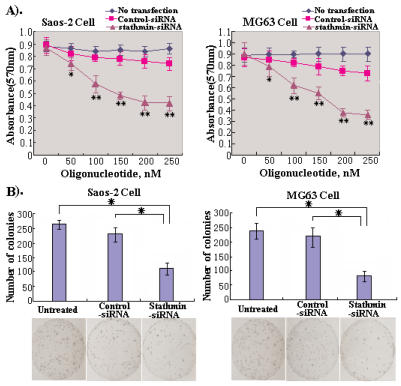
Effects of Stathmin-siRNA on Cell Proliferation and Colony Formation In Vitro
To analyze phenotypic changes, we first investigated the effects of transient stathmin-siRNA on celluar proliferation of osteosarcoma cells. Cell proliferation was evaluated by MTT assay daily for various concentrations of stathmin-siRNA. As shown in Figure 2A, treatment of Saos-2 and MG63 cells with stathmin-siRNA resulted in a dose-dependent inhibition of the proliferation of two osteosarcoma cells and reduced cell proliferation by 51.2% and 61.0% at 250 nM, respectively. Next, we explored whether stathmin-siRNA affected colony formation of osteosarcoma cells in soft agar assays. Cells were transfected with stathmin-siRNA or control-siRNA, and at 48 hours after transfection, the cells were plated into medium with soft agar. Colony formation was assayed at 15 days. As shown in Figure 2B, colony formation was significantly inhibited in the presence of stathmin-siRNA compared with that seen with unteatment or Control-siRNA treatment. All these results showed that RNAi-mediated transient stathmin downregulation resulted in marked inhibition of osteosarcoma cell proliferation in vitro.
Figure 2.
Effects of stathmin-siRNA on the cell proliferation and colony formation in vitro. (A) Cell proliferation assay. Human osteosarcoma cells (Saos-2 and MG63) were transfected with Control-siRNA or stathmin-siRNA (250 nM) for 24 h. Cell viability was evaluated by MTT assay. The data in each time point are averaged values from four replicates. These experiments were performed in triplicate. *P < 0.05 and **P < 0.01 vs. Control-siRNA. (B) Colony formation assay. Compared with that seen in the untransfected group, the number of colonies was significantly reduced in the stathmin-siRNA-transfected group but not in the Control-siRNA-transfected group. These experiments were performed in triplicate. *P < 0.05.
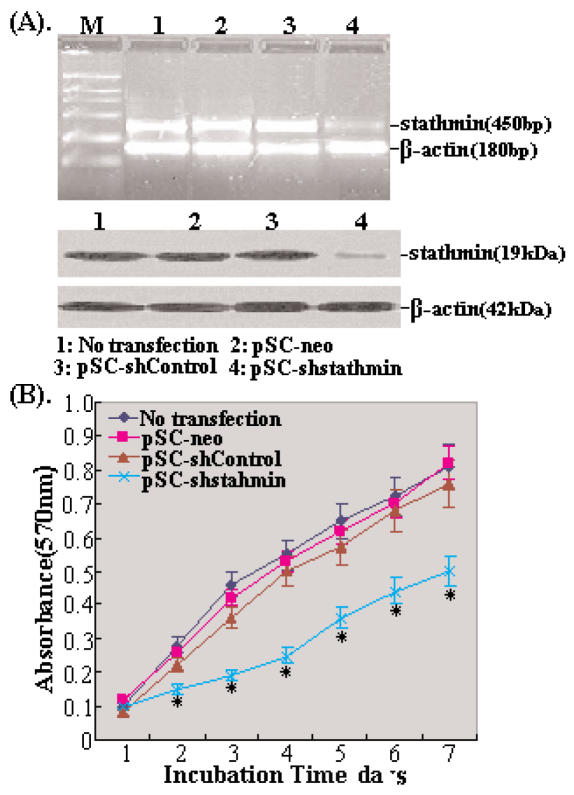
Effects of Vector-Mediated shRNA on Stathmin Expression and Cell Proliferation
First, we established stable transfectants of Saos-2 cells (transfected with pSC-shstathmin, pSC-shControl, or pSC-neo parental vector). In those stable transfectants expressing shstathmin, RT-PCR and Western blot analysis results showed that the levels of stathmin mRNA and protein expression were reduced by 64.7% and 75.5%, respectively (Figure 3A). We then tested the in vitro proliferation of these stably transfected cells by MTT assay daily for seven days. The cell proliferation curve showed that the stably transfected Saos-2 cells expressing shstathmin showed incomplete inhibition but moderate proliferation retardation, and the highest inhibitory rate was 38.3 ± 1.46% on day seven (P < 0.05, Figure 3B).
Figure 3.
Vector-mediated shstathmin inhibited its expression and induced proliferation retardation. (A) The levels of stathmin mRNA and protein expression were detected in the stably transfected Saos-2 cells. Compared with untransfected cells, the levels of stathmin mRNA and protein expression in pSC-shstathmin transfected Saos-2 cells were reduced by 64.7% and 75.5%, respectively (P < 0.05), but there were no obvious changes among other transfected Saos-2 cells (P > 0.05). (B) Stably transfected Saos-2 cell proliferation in vitro evaluated by MTT assay. These experiments were performed in triplicate. *P < 0.05 (significant differences among no transfection, pSC-neo, pSC-shControl, and pSC-shstathmin transfectants).
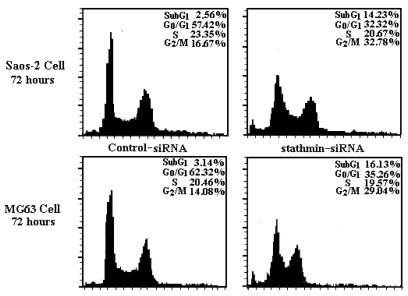
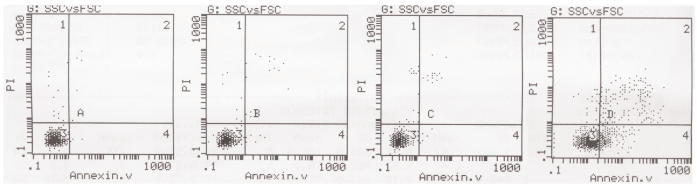
Effects of RNA Interference Targeting Stathmin on Cell Cycle and Apoptosis
The proliferation inhibition of osteosarcoma cells by knockdown of stathmin expression was caused by disrupting the cell cycle and affecting microtubule assembly shown in other types of mammalian cells (16,17). To reveal the mechanisms underlying RNAi-mediated proliferation inhibition, we used flow cytometric analysis to detect changes in the cell cycle and quantify apoptotic rates in osteosarcoma cells. We first analyzed the DNA contents of cell populations after transient transfection of stathmin-siRNA at the concentration of 250 nM into Saos-2 and MG63 cells. In both Saos-2 and MG63 cells 72 hours after stathmin-siRNA treatment, the population of G2/M phase was significantly increased and the population of G1/G0 phase was obviously decreased (P < 0.05), and a marked increase in the sub-G1 population was also detected (Figure 4, Table 2).
Figure 4.
The changes of cell cycle detected by flow cytometry. Cells were harvested 72 hours after siRNA transfection at 250 nM and subsequently analyzed for their DNA content by flow cytometry. Representative results are shown. These experiments were performed in triplicate. *P < 0.05.
Table 2.
Changes of population in cell cycle of transfected osteosarcoma cells.
| Saos-2 cell (72h after treatment)
|
MG63 cell (72 h after treatment)
|
|||
|---|---|---|---|---|
| Cell phase | Control-siRNA (%) | stathmin-siRNA (%) | Control-siRNA (%) | stathmin-siRNA (%) |
| SubG1 | 2.56 ± 0.35 | *14.23 ± 0.88 | 3.14 ± 0.74 | *16.13 ± 1.35 |
| G0/G1 | 57.42 ± 3.16 | *32.32 ± 2.03 | 62.32 ± 2.64 | *35.26 ± 2.83 |
| S | 23.35 ± 1.14 | 20.67 ± 1.55 | 20.46 ± 2.13 | 19.57 ± 1.46 |
| G2/M | 16.67 ± 1.76 | *32.78 ± 2.43 | 14.08 ± 1.17 | *29.04 ± 2.23 |
P < 0.05 compared with Control-siRNA.
Next, an annexin V-fluorescein isothiocyanate apoptosis detection kit (Zymed) was used to detect cell apoptosis of stably transfected Saos-2 cells. Cell apoptosis analysis by flow cytometry showed that compared with untransfected Saos-2 cells, the apoptosis rate of pSC-shstathmin transfected Saos-2 cells significantly increased by 22.6% ± 2.1% (P < 0.05, Figure 5), whereas there were no obvious changes among other stably transfected Saos-2 cells(transfected with pSC-shControl or pSC-neo vector). All above results suggested that RNAi-mediated transient or stable downregulation of stathmin expression in osteosarcoma cells could induce cell accumulation in the G2/M phase and final apoptosis.
Figure 5.
Cell apoptosis of stable transfectants detected by flow cytometry. The apoptotic rate of pSC-shstathmin transfected Saos-2 cells obviously increased by 22.6 ± −2.1% (P < 0.05), whereas there were no significant differences in cell apoptosis among untransfected, pSC-neo, or pSC-shControl transfected Saos-2 cells (P > 0.05).
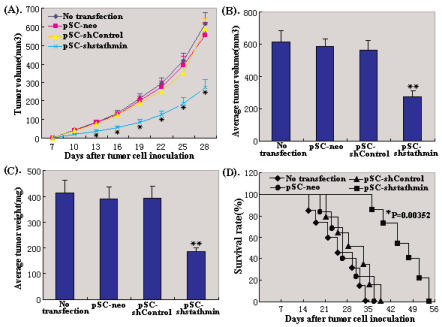
Inhibition of In Vivo Tumor Growth by Stathmin Downregulation
With the above findings of the effects of stathmin-siRNA in vitro, we next explore whether stathmin plays a critical role in tumor formation in vivo, and whether it can be used in clinical gene therapy. We subcutaneously injected aliquots of 1.0 × 107 stably transfected Saos-2 cells into 4 groups of mice and monitored tumor growth. As shown in Figure 6A, the growth of tumors formed from the pSC-shstathmin xenografts was significantly inhibited compared with tumors formed from other control xenografts. At 28 days after inoculation, the average tumor volume and tumor weight of the mice was decreased by 55.1% and 52.0% in pSC-shstathmin xenografts compared with untreated xenografts. (P < 0.01, Figure 6B and Figure 6C). Figure 6D shows the survival time of the mice. Stathmin downregulation prolonged the lifespan of mice bearing Saos-2 tumor cells (P = .00352). These results indicated that RNAi-mediated stathmin downregulation exerted a strong growth-suppressive effect on osteosarcoma in vivo.
Figure 6.
Effects of stathmin downregulation on tumor growth in vivo. (A) The growth in mice of tumors developed from untransfected and stably transfected Saos-2 cells (transfected with pSC-neo, pSC-shControl or pSC-shstathmin vector). The inoculation was performed in four groups (n = 10). (B) The average tumor volume at day 28 after inoculation of the above cells; **P < 0.01. (C) The average tumor weight at day 28 after inoculation of the above cells; **P < 0.01. (D) Survival curve of mice (n = 10) inoculated with untransfected and stably transfected Saos-2 cells (transfected with pSC-neo, pSC-shControl, or pSC-shstathmin vector). Results were evaluated by the Kaplan-Meier method. The differences between pSC-shstathmin treatment group and other control groups were statistically significant, *P < 0.01.
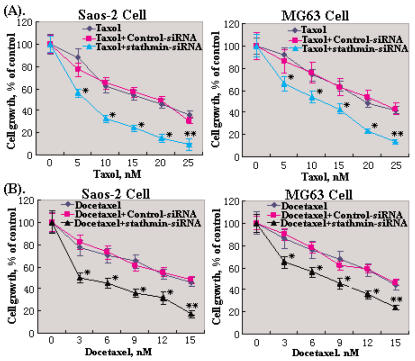
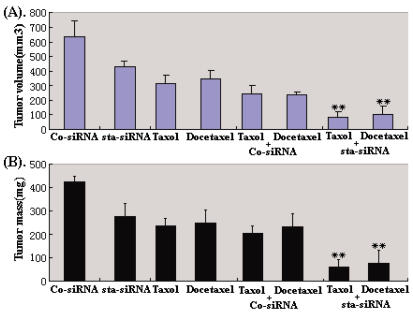
Stathmin-siRNA Synergistically Enhances Taxane-Induced Cytotoxicity In Vitro and In Vivo
Stathmin can disrupt the microtubule structure and destabilize microtubules through its phosphorylation. Taxanes, a family of chemotherapeutic agents, impair disassembly of microtubules that is essential for the normal segregation of chromosomes during mitosis of eukaryotic cells. Thus, we conclude that RNAi-mediated stathmin downregulation may synergistically enhance the cytotoxicity of taxanes, because taxanes can accumulate cells in the G2/M phase where stathmin plays important roles. To determine whether stathmin-siRNA enhanced the cytotoxicity of taxanes (Taxol and Docetaxel), osteosarcoma cells (Saos-2 and MG63) were treated with 100 nM Control-siRNA or stathmin-siRNA daily for three days, and incubated with indicated concentrations of each chemotherapeutic agent for two days. As shown in Figure 7, stathmin-siRNA significantly enhanced the chemosensitivity of these agents, decreasing the 50% inhibitory concentration of Taxol by 54.2 (or 47.3%) and Docetaxel by 78.5% (or 53.6%). Considering these findings in vitro, we next investigated the efficacy of stathmin-siRNA as an in vivo chemosensitizing strategy in a nude mouse xenograft model. After mice were treated with Control-siRNA and stathmin-siRNA, alone and in combination with Taxol or Docetaxel for 10 weeks, the average tumor volume (mm3) and tumor mass (mg) were detected. The average tumor volume and average tumor mass of mice treated with Taxol or Docetaxel in combination with stathmin-siRNA were 87.5 mm3 and 64 mg, respectively. Compared with other groups of mice, the tumor growth in this group of mice treated with Taxol or Docetaxel in combination with stathmin-siRNA was significantly inhibited (P < 0.05, Figure 8). All above results showed that the downregulation of stathmin expression mediated by siRNA can synergistically enhance the chemosensitivity of human osteosarcoma cells to taxanes both in vivo and in vitro.
Figure 7.
Stathmin-siRNA synergistically enhanced the cytotoxicity effect of taxanes in vitro. Saos-2 or MG63 Cells were treated daily with 100 nM stathmin-siRNA or Control-siRNA for three days, followed by the indicated concentrations of (A) Taxol and (B) Docetaxel. After 72 hours of incubation, cell growth was evaluated by MTT assay. *P < 0.05 and **P < 0.01 vs. Control-siRNA.
Figure 8.
Stathmin-siRNA synergistically enhanced the cytotoxicity effect of taxanes in vivo. (A) Tumor mass, (B) tumor volume following treatment with Taxol or Docetaxel, alone and in combination with Control-siRNA or with stathmin-siRNA. **P < 0.01 vs. Control-siRNA.
DISCUSSION
Stathmin (Op18), a cytosolic phosphoprotein, is the founding member of a family of microtubule-destabilizing proteins that regulate the dynamics of microtubule polymerization and depolymerization (20,21). Stathmin is overexpressed in various types of human cancers, including osteosarcoma, and its high expression levels could affect the distribution of cells throughout the cell cycle (22,23). To explore the possibility of stathmin as an effective therapeutic target, we employed an RNA interference technique to silence endogenous stathmin expression in osteosarcoma cells and analyzed phenotypic changes of transiently or stably transfected osteosarcoma cells. In our study, we achieved almost complete downregulation of stathmin expression by using an siRNA treatment strategy in osteosarcoma cell lines. Experimental data showed that transient stathmin downregulation led to significant inhibition of in vitro proliferation and colony formation, accumulation of G2/M phase, and final apoptosis of osteosarcoma cells. We established stably transfected osteosarcoma cells expressing shstathmin and observed that stable stathmin downregulation in osteosarcoma cells induced incomplete proliferation inhibition but moderate proliferation retardation. We also detected increased apoptosis rates of pSC-shstathmin transfectants, and the stable transfectants almost completely suppressed tumorigenecity in a mouse xenograft model. All these results suggest that stathmin is an important molecule of proliferation of tumor cells and a potential target for suppressing proliferation and triggering apoptosis, which can be explained by its key roles in mitosis. Thus, we have reasons to believe that stathmin may provide an excellent molecular target for osteosarcoma therapy.
Taxanes, a family of chemotherapeutic drugs that exert antitumor effects by interacting with microtubules and interfering with their dynamic equilibrium, induce cell accumulation in the G2/M phase of the cell cycle (24). The antimitotic effects of taxanes are exerted by promoting microtubulins to stable microtubules and suppressing their breakdown by combining with free microtubules, which are essential for the segregation of chromosomes during mitosis of eukaryotic cells. This action interferes with the normal regulation of the mitotic spindle and leads to mitotic arrest (25,26). After exposure to taxanes, some of the mitotically arrested cells undergo apoptosis, whereas others complete the division cycle, producing aneuploid cells that undergo apoptosis during subsequent cell cycles (27). Although taxanes significantly inhibit proliferation and induce apoptosis of osteosarcoma cells in vitro (28–30), their clinical uses as single chemotherapeutic agents are very limited because of the toxic effects related to long-term administration at high doses. Thus strategies to target mitosis will help to enhance the cytotoxicity effects of taxanes while reducing toxicity (or side effects) caused by high doses.
In the present study, we observed that RNAi-mediated stathmin downregulation in combination with taxanes could synergistically enhance the cytotoxicity effects both in vitro and in vivo. Taxanes and stathmin downregulation both interfere with the regulation of microtubules that make up the mitotic spindle, so it is not surprising that the combined use of two interventions would induce a synergistic interaction. In fact, RNAi-mediated stathmin inhibition and taxane exposure target different steps in the same mitotic pathway, so the simultaneous effects of both of these methods will increase tumor cell cytotoxicity. These results are consistent with other studies that showed synergistic inhibition of tumor cell proliferation associated with stathmin inhibition and taxol exposure (31,32). Much evidence has demonstrated that stathmin deficiency can decrease the rate of destruction and sequestration of tubulin molecules, thereby disrupting the equilibrium between polymerized and unpolymerized tubulin in favor of polymerized tubulin (33,34). Taxanes, on the other hand, make microtubules stable by binding to polymerized tubulin (35). Thus, once the stathmin-downregulated cells are exposed to taxanes, cells affected by stathmin deficiency will fail to depolymerize the microtubules, and the polymerized microtubules will be further stabilized by taxane binding. Therefore, the combine use of stathmin downregulation and taxanes will lead to stronger impairment of G2/M phase progression and synergistic induction of apoptosis. This result may be attributable, at least in part, to the mechanism by which RNAi-mediated stathmin downregulation synergizes with taxane exposure to exert more potent antiproliferative and antitumor effects. These results are also consistent with our previous reports and those of others that the overexpression of stathmin increased resistance to chemotherapy by decreasing microtubule polymer mass (36,37). The exact molecular mechanism that accounts for the observed synergistic interaction between stathmin inhibition and taxanes appears complex and remains to be further clarified.
RNA interference is characterized by high efficiency, high specificity, and low toxicity (38,39). This novel technology is becoming a conventional application for in vivo cancer therapy (40–42). In our study, we presented a proof of principle for the use of novel RNA interference technology to target candidate oncogenes in osteosarcoma cells and thereby exert antitumor effects at multiple levels. RNAi-mediated stathmin downregulation effectively inhibited cell proliferation in vitro and tumorigenicity in vivo, induced cell accumulation in the G2/M phase, led to apoptotic cell death, and enhanced chemosensitivity in human ostesosarcoma cells. All these findings suggest that stathmin may be a pivotal determinant for tumorigenesis and chemosensitivity, so it is expected to be a potential therapeutic target for the treatment of osteosarcomas.
ACKNOWLEDGMENTS
We thank the Department of Clinical Diagnosis for their technical support. This work was supported by a grant from Natural Science Foundation of Shaanxi Province (2003K10G44).
Footnotes
Online address: http://www.molmed.org
REFERENCES
- 1.Wittig JC, Bickels J, Priebat D, et al. Osteosarcoma: a multidisciplinary approach to diagnosis and treatment. Am Fam Physician. 2002;65:1123–32. [PubMed] [Google Scholar]
- 2.Bacci G, Longhi A, Versari M, Mercuri M, Briccoli A, Picci P. Prognostic factors for osteosarcoma of the extremity treated with neoadjuvant chemotherapy: 15-year experience in 789 patients treated at a single institution. Cancer. 2006;106:1154–61. doi: 10.1002/cncr.21724. [DOI] [PubMed] [Google Scholar]
- 3.Charbaut E, Curmi PA, Ozon S, Lachkar S, Redeker V, Sobel A. Stathmin family proteins display specific molecular and tubulin binding properties. J Biol Chem. 2001;276:16146–54. doi: 10.1074/jbc.M010637200. [DOI] [PubMed] [Google Scholar]
- 4.Zhang HZ, Gao P, Yan L, Lin F. Significance of stathmin gene overexpression in osteosarcoma cells. Ai Zheng. 2004;23:493–6. [PubMed] [Google Scholar]
- 5.Price DK, Ball JR, Bahrani-Mostafavi Z, et al. The phosphoprotein Op18/stathmin is differentially expressed in ovarian cancer. Cancer Invest. 2000;18:722–30. doi: 10.3109/07357900009012204. [DOI] [PubMed] [Google Scholar]
- 6.Roos G, Brattsand G, Landberg G, Marklund U, Gullberg M. Expression of oncoprotein 18 in human leukemias and lymphomas. Leukemia. 1993;7:1538–46. [PubMed] [Google Scholar]
- 7.Hanash SM, Strahler JR, Kuick R, Chu EHY, Nichols D. Identification of a polypeptide associated with the malignant phenotype in acute leukemia. J Biol Chem. 1998;263:12813–5. [PubMed] [Google Scholar]
- 8.Feuerstein N, Cooper HL. Rapid phosphorylation induced by phorbol ester in HL-60 cells. J Biol Chem. 1983;258:10786–93. [PubMed] [Google Scholar]
- 9.Belmont LD, Mitchison TJ. Identification of a protein that interacts with tubulin dimers and increases the catastrophe rate of microtubules. Cell. 1996;84:623–31. doi: 10.1016/s0092-8674(00)81037-5. [DOI] [PubMed] [Google Scholar]
- 10.Laird AD, Shalloway D. Oncoprotein signaling and mitosis. Cell Signal. 1997;9:249–55. doi: 10.1016/s0898-6568(96)00176-3. [DOI] [PubMed] [Google Scholar]
- 11.Murphy ME, Cassimeris L. A novel cancer therapy approach targeting microtubule function. Cancer Biol Ther. 2006;5:1721–3. doi: 10.4161/cbt.5.12.3736. [DOI] [PubMed] [Google Scholar]
- 12.Mistry SJ, Atweh GF. Role of stathmin in the regulation of the mitotic spindle: potential applications in cancer therapy. Mt Sinai J Med. 2002;69:299–304. [PubMed] [Google Scholar]
- 13.Luo XN, Mookerjee B, Ferrari A, Mistry S, Atweh GF. Regulation of phosphoprotein p18 in leukemic cells. Cell cycle regulated phosphorylation by p34cdc2 kinase. J Biol Chem. 1994;269:10312–8. [PubMed] [Google Scholar]
- 14.Jeha S, Luo XN, Beran M, Kantarjian H, Atweh GF. Antisense RNA inhibition of phosphoprotein p18 expression abrogates the transformed phenotype of leukemic cells. Cancer Res. 1996;56:1445–50. [PubMed] [Google Scholar]
- 15.Fan XM, Zhang HZ, Zhang MH, Fan QY. Inhibitory effects of AS-ODN of Stathmin gene on cultured osteosarcoma cell lines. J Fourth Mil Med Univ. 2002;23:469–71. [Google Scholar]
- 16.Gao P, Lin F. Inhibitory effects of stathmin gene SiRNA on cultured HeLa cell lines. J Modern Oncol. 2006;2:210–2. [Google Scholar]
- 17.Zhang HZ, et al. Silencing stathmin gene expression by survivin promoter-driven siRNA vector to reverse malignant phenotype of tumor cells. Cancer Biol Ther. 2006;5:1457–61. doi: 10.4161/cbt.5.11.3272. [DOI] [PubMed] [Google Scholar]
- 18.Alli E, Yang JM, Hait WN. Silencing of stathmin induces tumor-suppressor function in breast cancer cell lines harboring mutant p53. Oncogene. 2007;26:1003–12. doi: 10.1038/sj.onc.1209864. [DOI] [PubMed] [Google Scholar]
- 19.Mistry SJ, Atweh GF. Therapeutic interactions between stathmin inhibition and chemotherapeutic agents in prostate cancer. Mol Cancer Ther. 2006;5:3248–57. doi: 10.1158/1535-7163.MCT-06-0227. [DOI] [PubMed] [Google Scholar]
- 20.Melhem RF, Strahler JR, Hailat N, Zhu XX, Hanash SM. Involvement of OP18 in cell proliferation. Biochem Biophys Res Commun. 1991;179:1649–55. doi: 10.1016/0006-291x(91)91764-4. [DOI] [PubMed] [Google Scholar]
- 21.Curmi PA, et al. Stathmin and its phosphoprotein family: general properties, biochemical and functional interaction with tubulin. Cell Struct Funct. 1999;24:345–57. doi: 10.1247/csf.24.345. [DOI] [PubMed] [Google Scholar]
- 22.Niethammer P, Bastiaens P, Karsenti E. Stathmin-tubulin interaction gradients in motile and mitotic cells. Science. 2004;303:1862–6. doi: 10.1126/science.1094108. [DOI] [PubMed] [Google Scholar]
- 23.Rubin CI, Atweh GF. The role of stathmin in the regulation of the cell cycle. J Cell Biochem. 2004;93:242–50. doi: 10.1002/jcb.20187. [DOI] [PubMed] [Google Scholar]
- 24.Rowinsky EK. The development and clinical utility of the taxane class of antimicrotubule chemotherapy agents. Ann Rev Med. 1997;48:353–74. doi: 10.1146/annurev.med.48.1.353. [DOI] [PubMed] [Google Scholar]
- 25.Yvon AM, Wadsworth P, Jordan MA. Taxol suppresses dynamics of individual microtubules in living human tumor cells. Mol Biol Cell. 1999;10:947–59. doi: 10.1091/mbc.10.4.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jordan MA, Toso RJ, Thrower D, Wilson L. Mechanism of mitotic block and inhibition of cell proliferation by Taxol at low concentrations. Proc Natl Acad Sci USA. 1993;90:9552–6. doi: 10.1073/pnas.90.20.9552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rowinsky EK, Donehower RC, Jones RJ, Tucker RW. Microtubule changes and cytotoxicity in leukemic cell lines treated with Taxol. Cancer Res. 1988;48:4093–100. [PubMed] [Google Scholar]
- 28.Guo W, Zeng C, Dong FQ, Lei W. Paclitaxel-induced apoptosis in osteosarcoma cell line U-2 OS. Chin Med J (Engl) 2002;115:1796–801. [PubMed] [Google Scholar]
- 29.Xu XT, Wu XF, Zhang YQ. Experimental study of paclitaxel against human osteosarcoma. Cancer Research on Prevention and Treatment. 2005;32:333–5. [Google Scholar]
- 30.Tao H, Cai L, Song J. Proliferation inhibition effect of docetaxel combined with cisplatin on osteosarcoma cells. Medical Journal of Wuhan University. 2006;23:756–8. doi: 10.1007/s12032-009-9240-x. [DOI] [PubMed] [Google Scholar]
- 31.Iancu C, Mistry SJ, Arkin S, Atweh GF. Taxol and anti-stathmin therapy: a synergistic combination that targets the mitotic spindle. Cancer Res. 2000;60:3537–41. [PubMed] [Google Scholar]
- 32.Mistry SJ, Atweh GF. Therapeutic interactions between stathmin inhibition and chemotherapeutic agents in prostate cancer. Mol Cancer Ther. 2006;5:3248–57. doi: 10.1158/1535-7163.MCT-06-0227. [DOI] [PubMed] [Google Scholar]
- 33.Mistry SJ, Atweh GF. Stathmin inhibition enhances okadaic acidinduced mitotic arrest: a potential role for stathmin in mitotic exit. J Biol Chem. 2001;276:31209–15. doi: 10.1074/jbc.M011654200. [DOI] [PubMed] [Google Scholar]
- 34.Howell B, Deacon H, Cassimeris L. Decreasing oncoprotein 18/stathmin levels reduces microtubule catastrophes and increases microtubule polymer in vivo. J Cell Sci. 1999;112:3713–22. doi: 10.1242/jcs.112.21.3713. [DOI] [PubMed] [Google Scholar]
- 35.Parness J, Horwitz SB. Taxol binds to polymerized tubulin in vitro. J Biol Chem. 1981;91:479–87. doi: 10.1083/jcb.91.2.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jing X-R, Liu L, Zhao H, Zhang H-Z. Relationship between expression of Stathm in gene in cancer cells and its sensitivity to chemotherapeutic drugs. J Fourth Mil Med Univ. 2005;26:784–8. [Google Scholar]
- 37.Nishio K, Nakamura T, Koh Y, Kanzawa F, Tamura T, Saijo N. Oncoprotein 18 over-expression increases the sensitivity to vindesine in the human lung carcinoma cells. Cancer. 2001;91:1494–9. doi: 10.1002/1097-0142(20010415)91:8<1494::aid-cncr1157>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 38.Elbashir SM, Lendeckel W, Tuschl T. RNA interference is mediated by 21- and 22-nucleotide RNAs. Genes Dev. 2001;15:188–200. doi: 10.1101/gad.862301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tomari Y, Matranga C, Haley B, Martinez N, Zamore PD. A protein sensor for siRNA asymmetry. Science. 2004;306:1377–80. doi: 10.1126/science.1102755. [DOI] [PubMed] [Google Scholar]
- 40.Hingorani SR, Jacobetz MA, Robertson GP, Herlyn M, Tuveson DA. Suppression of BRAF(V599E) in human melanoma abrogates transformation. Cancer Res. 2003;63:5198–202. [PubMed] [Google Scholar]
- 41.Brummelkamp TR, Bernards R, Agami R. Stable suppression of tumorigenicity by virus-mediated RNA interference. Cancer Cell. 2002;2:243–7. doi: 10.1016/s1535-6108(02)00122-8. [DOI] [PubMed] [Google Scholar]
- 42.Takei Y, Kadomatsu K, Yuzawa Y, Matsuo S, Muramatsu T. A small interfering RNA targeting vascular endothelial growth factor as cancer therapeutics. Cancer Res. 2004;64:3365–70. doi: 10.1158/0008-5472.CAN-03-2682. [DOI] [PubMed] [Google Scholar]