Abstract
Background
Studies have shown patients who are delayed for surgical cardiac revascularization are faced with increased risks of symptom deterioration and death. This could explain the observation that operative mortality among persons undergoing coronary artery bypass surgery (CABG) is higher among women than men. However, in jurisdictions that employ priority wait lists to manage access to elective cardiac surgery, there is little information on whether women wait longer than men for CABG. It is therefore difficult to ascertain whether higher operative mortality among women is due to biological differences or to delayed access to elective CABG.
Methods
Using records from a population-based registry, we compared the wait-list time between women and men in British Columbia (BC) between 1990 and 2000. We compared the number of weeks from registration to surgery for equal proportions of women and men, after adjusting for priority, comorbidity and age.
Results
In BC in the 1990s, 9,167 patients aged 40 years and over were registered on wait lists for CABG and spent a total of 136,071 person-weeks waiting. At the time of registration for CABG, women were more likely to have a comorbid condition than men. We found little evidence to suggest that women waited longer than men for CABG after registration, after adjusting for comorbidity and age, either overall or within three priority groups.
Conclusion
Our findings support the hypothesis that higher operative mortality during elective CABG operations observed among women is not due to longer delays for the procedure.
Background
In publicly funded health care systems, priority wait lists are commonly used to manage access to elective cardiac surgery [1]. While queuing according to urgency of intervention is designed to facilitate access to surgery within a clinically appropriate time [2], patients who are delayed for surgical cardiac revascularization are faced with increased risks of worsening symptoms [3] and death [4,5]. The additional risks incurred by longer delays may be of particular concern for women with cardiovascular disease because, at presentation, women are more likely than men to have comorbid medical conditions such as hypertension, diabetes or obesity [6-11]. These comorbid medical conditions may increase the amount of time that women wait for CABG.
A number of studies have shown that the operative mortality among women undergoing CABG surgery is higher than that of men [12,13]. However, there is no information on whether women wait longer than men for CABG, after adjusting for age, severity of disease and comorbidity. It is therefore difficult to ascertain whether higher operative mortality may be due to delayed access to care in the pre-surgical period. Addressing this question is important for improving the care of persons with cardiovascular disease because, if differences are due to longer waiting times, it might be feasible to implement strategies to reduce waiting times among women.
The objective of this study was to compare the time from registration on the wait list to CABG between women and men, after adjusting for differences in age, severity of coronary artery disease, and comorbidity. To examine the consistency over time of any effects of sex on waiting times, comparisons were done across synthetic cohorts of patients defined by two-year periods of registration on the wait lists: 1991–92, 1993–94, 1995–96, 1997–98, or 1999–2000.
Methods
Data sources
The BC Cardiac Registries (BCCR) prospectively capture the occurrence and timing of registration, surgery, or removal from the wait lists without surgery, for all patients accepted for cardiac surgery procedures in the four heart-surgery centers delivering services in BC (population of four million) [14]. Registered patients were removed from the wait lists without surgery if they died, declined the operation, accepted surgery from another surgeon, moved away, or continued with medical management. Cardiac surgeons in BC have developed common guidelines for prioritizing patients and assigning the suggested waiting time for surgery based on angina symptoms, affected coronary anatomy, non-invasive test results, and left ventricular function impairment as described elsewhere [15]. Using those guidelines, each patient was classified by the surgeon into one of the following three groups: priority 1 if the suggested time to surgery was three days, priority 2 if the suggested time to surgery was six weeks, and priority 3 if the suggested time to surgery was 12 weeks.
Patients
There were 9,366 records of registration for isolated CABG added to the Registry between January 1991 and December 2000. We excluded 135 records of patients who were: emergency cases (30), removed on the registration date (101), and had missing operating room reports (4). All remaining 9,231 records had either the surgery date or the date and reason of removal from the list without surgery. We restricted the analyses to the first 52 weeks after registration so that 475 (5%) patients remaining on the lists at 12 months were censored. Of those, 167 eventually underwent surgery; seven died; 78 received medical treatment; 104 declined surgery; 17 were transferred to another surgeon or hospital; and 102 were removed for other reasons.
Comorbidity
To control for co-existing conditions, each patient was classified as (1) presenting with no co-existing conditions, (2) presenting with a major comorbid condition including congestive heart failure, diabetes, chronic obstructive pulmonary disease, cancer, or rheumatoid arthritis, or (3) presenting with a minor comorbid condition including other coexisting chronic conditions including peripheral vascular disease, cerebrovascular disease, dementia, peptic ulcer disease, hemiplegia, renal disease, or liver disease [16]. The first set of conditions were those originally used in a study on the appropriateness of coronary revascularization [17]. As we were concerned that there were other potential concomitant illnesses that could delay surgery, we added the other category that included conditions from Charlson comorbidity index [18]. We entered two indicator variables in the models to represent the three comorbidity categories.
Statistical methods
Waiting times were analyzed as prospective observations beginning at the time of registration. Each patient had a waiting time calculated in calendar weeks from registration to surgery or removal for other reasons. The cumulative probability of undergoing surgery as a function of waiting time was estimated using the Kaplan-Meier method [19]. Patients removed from the list for reasons other than surgery were treated as censored observations.
Primary comparisons were done across synthetic cohorts of patients defined by two-year periods of registration on the wait lists. Within each registration period, differences in the distributions of wait-list times between women and men were examined using the log rank-test [20].
The effect size for each period was estimated using hazard ratios for surgery derived from a Cox proportional hazards model [21] in which we stratified on age. The priority group and the comorbidity measures were included as independent variables in the Cox model to estimate adjusted effects. Hazard ratios (HR) for women evaluate the conditional probability of undergoing CABG relative to men at any week on the list. The weekly surgery rate was calculated by dividing the number of operations by the total number of patient-weeks on the list.
The Clinical Research Ethics Board of the University of British Columbia approved the study protocol in September, 2001. Individual consent was waived.
Results and discussion
In BC in the 1990s, 9,167 patients aged 40 years and over were registered on wait lists for CABG and spent a total of 136,071 person-weeks waiting. Of 9,167 persons aged 40 to 89 y who were registered for CABG in BC between 1991 and 2000, about 18% (1,629) were women (Table 1). At registration for CABG, among women, 19% were under age 60 y and 42% were over age 70 y, compared with 31% of men under age 60 y and 30% over age 70 y. There was a significant difference in the distribution of age between women and men (X2 = 128.3, df = 4, P < 0.0001). The number of women registered ranged from a low of 297 in 1993–1994 to a high of 379 in 1995–1996 (data not shown).
Table 1.
Characteristics of 9,167 patients registered for CABG surgery in British Columbia, 1991–2000
| Women (N = 1,629) | Men (N = 7,538) | |||
| Characteristic | N | (%) | N | (%) |
| Age Group (y) | ||||
| 40–49 | 68 | (4.2) | 600 | (8.0) |
| 50–59 | 241 | (14.8) | 1764 | (23.4) |
| 60–69 | 638 | (39.2) | 2892 | (38.4) |
| 70–79 | 633 | (38.9) | 2137 | (28.3) |
| 80–89 | 49 | (3.0) | 145 | (1.9) |
| Urgency at Registration | ||||
| Priority 1 | 123 | (7.6) | 534 | (7.1) |
| Priority 2 | 1116 | (68.5) | 5339 | (70.8) |
| Priority 3 | 377 | (23.1) | 1567 | (20.8) |
| Unknown | 13 | (0.8) | 98 | (1.3) |
| Comorbidity at Registration | ||||
| No comorbidity | 750 | (46.0) | 3985 | (52.9) |
| Major comorbidity (CHF, diabetes, COPD, rheumatism, cancer) | 463 | (28.4) | 1540 | (20.4) |
| Other conditions | 416 | (25.2) | 2013 | (26.7) |
| Registration Period | ||||
| 1991–1992 | 318 | (19.5) | 1394 | (18.5) |
| 1993–1994 | 297 | (18.2) | 1574 | (20.9) |
| 1995–1996 | 379 | (23.3) | 1619 | (21.5) |
| 1997–1998 | 350 | (21.5) | 1527 | (20.3) |
| 1999–2000 | 285 | (17.5) | 1424 | (18.9) |
Abbreviations: CABG = outpatient isolated coronary artery bypass surgery; CHF = congestive heart failure; COPD = chronic obstructive pulmonary disease
At registration, 46% of women had no comorbid conditions recorded, 25% had at least one minor comorbid medical condition and 28% had at least one major comorbid condition. Women were 20% less likely than men to have no comorbid conditions (OR = 0.8) and 50% more likely to have a major comorbid condition (OR = 1.5). There was a significant difference in the distribution of comorbid medical conditions between women and men (X2 = 51.9, df = 2, P < 0.0001). A similar proportion of women and men received the operation within the recommended waiting time (Table 2).
Table 2.
Outcomes of registration for CABG surgery in British Columbia 1991–2000 at 52 weeks
| Women (N = 1629) | Men (N = 7538) | |||
| Outcomes | N | (%) | N | (%) |
| Underwent Surgery* | ||||
| Within recommended time | 534 | (32.8) | 2393 | (31.7) |
| Beyond recommended time | 845 | (51.9) | 4120 | (54.7) |
| Between 1 and 12 weeks, priority unknown | 8 | (0.5) | 33 | (0.4) |
| Removed without surgery** | ||||
| Died while waiting | 9 | (0.6) | 81 | (1.1) |
| Medical treatment | 46 | (2.8) | 128 | (1.7) |
| Patient request | 42 | (2.6) | 145 | (1.9) |
| Transferred or moved | 12 | (0.7) | 87 | (1.2) |
| Other reason | 45 | (2.8) | 166 | (2.2) |
| Still on wait list at 52 weeks | 88 | (5.4) | 385 | (5.1) |
Abbreviation: CABG = outpatient isolated coronary artery bypass surgery
* χ2 = 2.0, df = 2, p = 0.36
** χ2 = 14.8, df = 4, p = 0.0052
Over all periods, at registration for CABG, approximately equal proportions of women and men were in priority group 1 (OR = 1.0, 95% CI: 0.8, 1.2 (adjusted for year and age)), a lower proportion of women was in priority group 2 (OR = 0.9, 95% CI: 0.8, 1.0 (adjusted for year and age)), and a higher proportion was in priority group 3 (OR = 1.2, 95% CI 1.0, 1.3 (adjusted for year and age)) (Table 3). There was a significant difference in the distribution of priority group among women and men (X2 = 7.72, df = 3, P = 0.0521).
Table 3.
Distribution of patients registered for CABG in British Columbia 1991–2000 by priority group and registration period
| Priority 1 | Priority 2 | Priority 3 | ||||
| Registration Period | N | (%) | N | (%) | N | (%) |
| Women | ||||||
| 1991–1992 | 27 | (8.5) | 224 | (70.4) | 65 | (20.4) |
| 1993–1994 | 21 | (7.1) | 210 | (70.7) | 64 | (21.5) |
| 1995–1996 | 47 | (12.4) | 248 | (65.4) | 81 | (21.4) |
| 1997–1998 | 25 | (7.1) | 238 | (68.0) | 83 | (23.7) |
| 1999–2000 | 3 | (1.1) | 196 | (68.8) | 84 | (29.5) |
| All periods* | 123 | (7.6) | 1116 | (68.5) | 377 | (23.1) |
| Men | ||||||
| 1991–1992 | 88 | (6.3) | 990 | (71.0) | 267 | (19.2) |
| 1993–1994 | 89 | (5.7) | 1160 | (73.7) | 317 | (20.1) |
| 1995–1996 | 202 | (12.5) | 1105 | (68.3) | 291 | (18.0) |
| 1997–1998 | 91 | (6.0) | 1083 | (70.9) | 341 | (22.3) |
| 1999–2000 | 64 | (4.5) | 1001 | (70.3) | 351 | (24.6) |
| All periods** | 534 | (7.1) | 5339 | (70.8) | 1567 | (20.8) |
Abbreviation: CABG = outpatient isolated coronary artery bypass surgery
*Excludes 13 patients with unknown priority
**Excludes 98 patients with unknown priority
Among women, the distribution of priority group at registration for CABG remained approximately constant during the first four periods; in the final period, there was a reduced proportion in priority group 1 and an increased proportion in the priority group 3. A similar pattern was observed among men, with a relatively constant distribution of priority groups during the first four periods and a shift in the last period to a reduced proportion in the most urgent priority group and an increased proportion in the least urgent priority group.
Among women and over all registration periods, the median wait list time for outpatient isolated CABG in BC was 11 weeks, ranging from 7 weeks in the earliest period to 16 weeks in the middle period (Table 4). Among men and over all registration periods, the median wait list time was also 11 weeks, ranging from 9 weeks in the earliest period to 14 weeks in the middle period. As measured by the interquartile range (IQR), the variability in wait list time over all periods was 1 week longer for women than men (18 weeks versus 17 weeks).
Table 4.
Percentiles of wait-list time (weeks) for women and men registered for CABG in British Columbia 1991–2000 by registration period
| Percentile | ||||||
| Registration Period | 10th | 25th | 50th | 75th | 90th | 90th – 50th |
| Women | ||||||
| 1991–1992 | 1 | 2 | 7 | 19 | 43 | 36 |
| 1993–1994 | 1 | 4 | 8 | 18 | 49 | 41 |
| 1995–1996 | 1 | 6 | 16 | 27 | 53 | 37 |
| 1997–1998 | 3 | 6 | 15 | 26 | 40 | 25 |
| 1999–2000 | 3 | 6 | 11 | 19 | 47 | 36 |
| All periods | 1 | 5 | 11 | 23 | 49 | 38 |
| Men | ||||||
| 1991–1992 | 1 | 3 | 9 | 19 | 44 | 25 |
| 1993–1994 | 2 | 4 | 9 | 18 | 44 | 25 |
| 1995–1996 | 1 | 6 | 14 | 26 | 46 | 32 |
| 1997–1998 | 2 | 6 | 13 | 24 | 43 | 30 |
| 1999–2000 | 3 | 6 | 10 | 19 | 39 | 29 |
| All periods | 2 | 5 | 11 | 22 | 43 | 32 |
Abbreviation: CABG = outpatient isolated coronary artery bypass surgery
One difference between women and men was observed for those patients with longer waiting times: the wait-list interval requiring 40% of operations in patients staying on the lists longer than the median time was 6 weeks longer among women than men, as measured by the differences between 90th and 50th percentiles. The differential between women and men reached a maximum 14 weeks in 1993–1994.
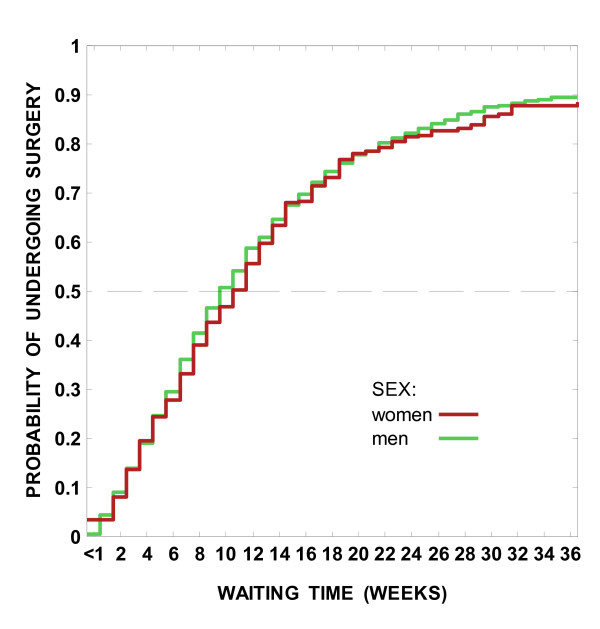
The differences in time spent on the wait lists were not significantly different between women and men in any calendar period of registration (P > 0.10 for all periods). The distributions of the estimated probability of undergoing CABG at each week on the wait list for the period 1999–2000 were overlapping for women and men over the first 36 weeks after registration (Figure 1).
Figure 1.
Characteristics of 9,167 patients registered for outpatient isolated coronary artery bypass surgery in British Columbia, 1991–2000.
For women, the average weekly rate of operations per 100 varied from 6.9 (6.1–7.7) in the 1991–1992 cohort to 4.7 (4.2–5.2) in the 1995–1996 cohort to 5.8 (5.1–6.6) in the 1999–2000 cohort (Table 5). At any week on the list, the conditional probability of undergoing surgery was reduced by 39% in 1995–1996 women, HR = 0.61 (0.51–0.72), and by 13% in 1999–2000 women, HR = 0.87 (0.73–1.05), relative to the period 1991–1992, after adjusting for priority, comorbidity, and age.
Table 5.
Average weekly rate of CABG in British Columbia, 1991–2000 and adjusted hazard ratios by registration period
| Registration Period | Number of operations | Total waiting time, weeks | Crude Rate, per 100 | SE | RR | 95% CI* |
| Women | ||||||
| 1991–1992 | 281 | 4094.0 | 6.9 | (0.4) | 1.00 | Referent |
| 1993–1994 | 260 | 3892.5 | 6.7 | (0.4) | 0.98 | (0.82, 1.17) |
| 1995–1996 | 313 | 6676.5 | 4.7 | (0.3) | 0.61 | (0.51, 0.72) |
| 1997–1998 | 293 | 5587.5 | 5.2 | (0.3) | 0.68 | (0.57, 0.81) |
| 1999–2000 | 240 | 4103.5 | 5.8 | (0.4) | 0.87 | (0.73, 1.05) |
| Men | ||||||
| 1991–1992 | 1211 | 18773.0 | 6.5 | (0.2) | 1.00 | Referent |
| 1993–1994 | 1370 | 21221.0 | 6.5 | (0.2) | 1.01 | (0.93, 1.09) |
| 1995–1996 | 1403 | 27353.0 | 5.1 | (0.1) | 0.72 | (0.66, 0.78) |
| 1997–1998 | 1311 | 24570.0 | 5.3 | (0.1) | 0.79 | (0.72, 0.85) |
| 1999–2000 | 1251 | 19799.5 | 6.3 | (0.2) | 0.93 | (0.86, 1.01) |
Abbreviations: CABG = outpatient isolated coronary artery bypass surgery; SE = standard error; HR = hazard ratio; 95% CI = 95% confidence interval
*adjusted for priority group and comorbidity; stratified by age.
0 patients were on the wait list on December 31, 2001
For men, the average weekly rate of operations per 100 varied from 6.5 (6.1–6.8) in the 1991–1992 cohort to 5.1 (4.9–5.4) in the 1995–1996 cohort to 6.3 (6.0–6.7) in the 1999–2000 cohort. At any week on the list, the conditional probability of undergoing surgery was reduced by 28% in 1995–1996 men, HR = 0.72 (0.66–0.78), and by 7% in 1999–2000 men, HR = 0.93 (0.86–1.01), relative to the period 1991–1992, after adjusting for priority, comorbidity, and age.
Within priority groups, there was little evidence that women waited longer than men for CABG after registration, after adjusting for comorbidity, age and sex (Table 6).
Table 6.
Rate Ratios* by sex and priority group for patients undergoing CABG in British Columbia 1991–2000
| Priority 1 | Priority 2 | Priority 3 | ||||
| Sex | RR | 95% CI | RR | 95% CI | RR | 95% CI |
| Men | 1.00 | Referent | 1.00 | Referent | 1.00 | Referent |
| Women | 0.88 | (0.69, 1.14) | 0.99 | (0.92, 1.06) | 1.01 | (0.88, 1.16) |
Abbreviations: CABG = outpatient isolated coronary artery bypass surgery; RR = rate ratio; 95% CI = 95% confidence interval
*adjusted for comorbidity; stratified by age and registration period
Conclusion
In this paper we found little evidence that women waited longer than men for elective CABG in BC during the 1990s. After adjusting for comorbidity and age, the time spent on CABG wait lists did not differ between women and men in any calendar period of registration or within any of the three priority groups. A similar proportion of women and men received the operation within the recommended waiting time.
The distribution of women undergoing CABG was lower than reported in other jurisdictions [6,8,22,23] and within the range reported in other Canadian provinces: a lower proportion (12%) of women was observed in Nova Scotia [3] and a higher proportion (30%) in Alberta [24].
The significance of our findings can be understood within the context that women have higher mortality after CABG [6,25-28]. This issue was addressed using the United States Society of Thoracic Surgeons National Cardiac Surgery Database to examine peri-operative survival among 344,913 patients undergoing CABG between 1994 and 1997 [6]. After adjustment for other risk factors, female sex remained an independent predictor of operative mortality in all but very high risk patients. The main finding in the current study – that waiting times did not differ between women and men in BC – supports the hypothesis that the higher operative mortality among women is due to biological differences. Studies from the Cleveland Clinic and the Northern New England Study Group have shown the impact of body size on peri-operative CABG mortality [29,30]. Women typically have a smaller body surface area than men which in turn is associated with smaller hearts and correspondingly diminutive coronary arteries. This is thought to increase the technical difficulty of CABG and contribute to poorer outcome [31]. Alternatively, the differences in operative mortality may be due to a delay in treatment or in referral to catheterization [32]. Other Canadian investigators found that the median duration between cardiac catheterization and surgery did differ between women and men waiting for CABG or aortic valve replacement in Nova Scotia [3].
We also found that, for one portion of the waiting time distribution that included patients who waited longer than the median waiting time as measured by the differences between 90th and 50th percentiles, the waiting time was six weeks longer among women than men. An explanation of this finding remains speculative and could serve as the basis of a future study.
As reported by other investigators [6-11], we found that women were significantly older and more likely to have a major comorbid medical conditions when registered for CABG. Part of this difference stems from women presenting with initial symptoms of cardiovascular disease at an older age. This may also be indicative of differences in health seeking behavior by women [33,34] or in referral patterns from a cardiologist to a cardiac surgeon for women with symptoms of cardiovascular disease [32].
Limitations
The internal validity of this study was high and it is unlikely that potential biases could have materially affected the results. Selection bias was minimized because the registry maintains a record for virtually every person assessed by a cardiac surgeon in BC and active follow-up is undertaken for all persons registered. Information bias was not a concern because there is no reason to believe that any coding or other errors occurred differentially among women and men. While there is always the possibility of confounding in an observational study, the likelihood of a major unknown confounder is small because it would need to have exerted a strong influence to substantially affecting the interpretation and results, and we are unaware of any powerful factor that affected waiting time.
The main question regarding the validity of the study is the generalizability of the results. A study examining whether the waiting time for CABG differs between women and men in another jurisdiction that employs priority wait lists for CABG would be valuable. It would also be of considerable interest to determine the impact of sex in health systems that use wait lists but have different types of reimbursement mechanisms.
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
ARL conceived and designed the study, acquired the data, interpreted the results, and drafted the manuscript. BGS conceived and designed the study, analysed the data, interpreted the results, and drafted the manuscript. LK analysed the data and interpreted the results. RH participated in the design of the study, helped acquire the data, and interpreted the results. SMM conceived and designed the study and interpreted the results. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
The authors gratefully acknowledge the contributions of Rita Sobolyeva and Laurie Kilburn.
The following cardiac surgeons are contributors to the BCCR Surgical Research Committee: Drs. James Abel, Richard Brownlee, Larry Burr, Anson Cheung, James Dutton, Guy Fradet, Virginia Gudas, Robert Hayden, Eric Jamieson, Michael Janusz, Shahzad Karim, Tim Latham, Jacques LeBlanc, Sam Lichtenstein, Hilton Ling, John Ofiesh, Michael Perchinsky, Peter Skarsgard and Frank Tyers.
This study received financial support from the: BC Research Institute of Women's and Children's Health, St Paul's Hospital Foundation (ARL), Vancouver Coastal Health Research Institute (BGS, JMF), Michael Smith Foundation for Health Research (ARL), Canada Foundation for Innovation (ARL, BGS), and Canada Research Chairs program (BGS).
Contributor Information
Adrian R Levy, Email: alevy@cheos.ubc.ca.
Boris G Sobolev, Email: sobolev@interchange.ubc.ca.
Lisa Kuramoto, Email: Lisa.Kuramoto@vch.ca.
Robert Hayden, Email: erh@telus.net.
Stuart M MacLeod, Email: smacleod@cw.bc.ca.
References
- Hurst J, Siciliani L. Tackling excessive waiting times for elective surgery: a comparison of policies in twelve OECD countries. Paris, Organisation for Economic Co-operation and Development; 2003. [Google Scholar]
- MacCormick AD, Collecutt WG, Parry BR. Prioritizing patients for elective surgery: a systematic review. ANZ J Surg. 2003;73:633–642. doi: 10.1046/j.1445-2197.2003.02605.x. [DOI] [PubMed] [Google Scholar]
- Ray AA, Buth KJ, Sullivan JA, Johnstone DE, Hirsch GM. Waiting for cardiac surgery: results of a risk-stratified queuing process. Circulation. 2001;104:I92–I98. [PubMed] [Google Scholar]
- Sobolev BG, Levy AR, Kuramoto L, Hayden R, Fitzgerald JM. Do longer delays for coronary artery bypass surgery contribute to preoperative mortality in less urgent patients? Med Care. 2006;44:680–686. doi: 10.1097/01.mlr.0000220257.81482.67. [DOI] [PubMed] [Google Scholar]
- Sobolev BG, Levy AR, Kuramoto L, Hayden R, Brophy JM, Fitzgerald JM. The risk of death associated with delayed coronary artery bypass surgery. BMC Health Serv Res. 2006;6:85. doi: 10.1186/1472-6963-6-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards FH, Carey JS, Grover FL, Bero JW, Hartz RS. Impact of gender on coronary bypass operative mortality. Ann Thorac Surg. 1998;66:125–131. doi: 10.1016/S0003-4975(98)00358-0. [DOI] [PubMed] [Google Scholar]
- Hassan A, Chiasson M, Buth K, Hirsch GM. Women have worse long-term outcomes after coronary artery bypass grafting than men. Canadian Journal of Cardiology. 2005;21:757–762. [PubMed] [Google Scholar]
- Vaccarino V, Abramson JL, Veledar E, Weintraub WS. Sex differences in hospital mortality after coronary artery bypass surgery - Evidence for a higher mortality in younger women. Circulation. 2002;105:1176–1181. doi: 10.1161/hc1002.105133. [DOI] [PubMed] [Google Scholar]
- Abramov D, Tamariz MG, Sever JY, Christakis GT, Bhatnagar G, Heenan AL, Goldman BS, Fremes SE. The influence of gender on the outcome of coronary artery bypass surgery. Ann Thorac Surg. 2000;70:800–805. doi: 10.1016/S0003-4975(00)01563-0. [DOI] [PubMed] [Google Scholar]
- Koch CG, Weng YS, Zhou SX, Savino JS, Mathew JP, Hsu PH, Saidman LJ, Mangano DT. Prevalence of risk factors, and not gender per se, determines short- and long-term survival after coronary artery bypass surgery. Journal of Cardiothoracic and Vascular Anesthesia. 2003;17:585–593. doi: 10.1016/S1053-0770(03)00201-5. [DOI] [PubMed] [Google Scholar]
- Koch CG, Higgins TL, Capdeville M, Maryland P, Leventhal M, Starr NJ. The risk of coronary artery surgery in women: A matched comparison using preoperative severity of illness scoring. Journal of Cardiothoracic and Vascular Anesthesia. 1996;10:839–843. doi: 10.1016/S1053-0770(96)80042-5. [DOI] [PubMed] [Google Scholar]
- Jaglal SB, Tu JV, Naylor CD. Higher in-hospital mortality in female patients following coronary artery bypass surgery: a population-based study. Provincial Adult Cardiac Care Network of Ontario. Clin Invest Med. 1995;18:99–107. [PubMed] [Google Scholar]
- Fisher LD, Kennedy JW, Davis KB, Maynard C, Fritz JK, Kaiser G, Myers WO. Association of sex, physical size, and operative mortality after coronary artery bypass in the Coronary Artery Surgery Study (CASS) J Thorac Cardiovasc Surg. 1982;84:334–341. [PubMed] [Google Scholar]
- Volk T, Hahn L, Hayden R, Abel J, Puterman ML, Tyers GF. Reliability audit of a regional cardiac surgery registry. J Thorac Cardiovasc Surg. 1997;114:903–910. doi: 10.1016/S0022-5223(97)70003-5. [DOI] [PubMed] [Google Scholar]
- Levy AR, Sobolev BG, Hayden R, Kiely M, Fitzgerald JM, Schechter MT. Time on wait lists for coronary bypass surgery in British Columbia, Canada, 1991-2000. BMC Health Serv Res. 2005;5:22. doi: 10.1186/1472-6963-5-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romano PS, Roos LL, Jollis JG. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol. 1993;46:1075–9; discussion 1081-9. doi: 10.1016/0895-4356(93)90103-8. [DOI] [PubMed] [Google Scholar]
- Naylor CD, Levinton CM, Baigrie RS. Adapting to waiting lists for coronary revascularization. Do Canadian specialists agree on which patients come first? Chest. 1992;101:715–722. doi: 10.1378/chest.101.3.715. [DOI] [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied Survival Analysis: regression modeling time to event data. New York, Wiley & Son; 1998. pp. 27–86. [Google Scholar]
- Klein JP, Moeschberger ML. Survival analysis: techniques for censored and truncated data. New York, Springer; 1997. Hypothesis testing; pp. 191–201. [Google Scholar]
- Cox DR. Regression models and life tables. J R Stat Soc B. 1972;34:387–404. [Google Scholar]
- Ayanian JZ, Epstein AM. Differences in the use of procedures between women and men hospitalized for coronary heart disease. N Engl J Med. 1991;325:221–225. doi: 10.1056/NEJM199107253250401. [DOI] [PubMed] [Google Scholar]
- Haglund B, Koster M, Nilsson T, Rosen M. Inequality in access to coronary revascularization in Sweden. Scand Cardiovasc J. 2004;38:334–339. doi: 10.1080/14017430410021516. [DOI] [PubMed] [Google Scholar]
- Ghali WA, Faris PD, Galbraith PD, Norris CM, Curtis MJ, Saunders LD, Dzavik V, Mitchell LB, Knudtson ML. Sex differences in access to coronary revascularization after cardiac catheterization: importance of detailed clinical data. Ann Intern Med. 2002;136:723–732. doi: 10.7326/0003-4819-136-10-200205210-00007. [DOI] [PubMed] [Google Scholar]
- Edwards FH, Ferraris VA, Shahian DM, Peterson E, Furnary AP, Haan CK, Bridges CR. Gender-specific practice guidelines for coronary artery bypass surgery: Perioperative management. Ann Thorac Surg. 2005;79:2189–2194. doi: 10.1016/j.athoracsur.2005.02.065. [DOI] [PubMed] [Google Scholar]
- Hammar N, Sandberg E, Larsen FF, Ivert T. Comparison of early and late mortality in men and women after isolated coronary artery bypass graft surgery in Stockholm, Sweden, 1980 to 1989. J Am Coll Cardiol. 1997;29:659–664. doi: 10.1016/S0735-1097(96)00531-1. [DOI] [PubMed] [Google Scholar]
- Carey JS, Cukingnan RA, Singer LKM. Health-Status After Myocardial Revascularization - Inferior Results in Women. Ann Thorac Surg. 1995;59:112–117. doi: 10.1016/0003-4975(94)00702-9. [DOI] [PubMed] [Google Scholar]
- Edwards FH, Clark RE, Schwartz M. Coronary-Artery Bypass-Grafting - the Society-Of-Thoracic-Surgeons National Database Experience. Ann Thorac Surg. 1994;57:12–19. doi: 10.1016/0003-4975(94)90358-1. [DOI] [PubMed] [Google Scholar]
- Loop FD, Golding LR, MacMillan JP, Cosgrove DM, Lytle BW, Sheldon WC. Coronary artery surgery in women compared with men: analyses of risks and long-term results. J Am Coll Cardiol. 1983;1:383–390. doi: 10.1016/s0735-1097(83)80064-3. [DOI] [PubMed] [Google Scholar]
- O'Connor GT, Morton JR, Diehl MJ, Olmstead EM, Coffin LH, Levy DG, Maloney CT, Plume SK, Nugent W, Malenka DJ, . Differences between men and women in hospital mortality associated with coronary artery bypass graft surgery. The Northern New England Cardiovascular Disease Study Group. Circulation. 1993;88:2104–2110. doi: 10.1161/01.cir.88.5.2104. [DOI] [PubMed] [Google Scholar]
- McLarty A, Mann N, Lawson WE, Foster A. Womens heart health series: a mini-symposium. Med Sci Monit. 2003;9:RA103–RA110. [PubMed] [Google Scholar]
- Sheifer SE, Escarce JJ, Schulman KA. Race and sex differences in the management of coronary artery disease. Am Heart J. 2000;139:848–857. doi: 10.1016/S0002-8703(00)90017-6. [DOI] [PubMed] [Google Scholar]
- Gibler WB, Armstrong PW, Ohman EM, Weaver WD, Stebbins AL, Gore JM, Newby LK, Califf RM, Topol EJ. Persistence of delays in presentation and treatment for patients with acute myocardial infarction: The GUSTO-I and GUSTO-III experience. Annals of Emergency Medicine. 2002;39:123–130. doi: 10.1067/mem.2002.121402. [DOI] [PubMed] [Google Scholar]
- Rosenfeld AG. Women's risk of decision delay in acute myocardial infarction: Implications for research and practice. AACN clinical issues. 2001;12:29–39. doi: 10.1097/00044067-200102000-00005. [DOI] [PubMed] [Google Scholar]