Abstract
Stress is a risk factor for a number of diseases and is an important predictor of health in general. Herbal medicines have been used as adaptogens to regulate and improve the stress response and there is evidence to support the use of herbal medicines for this purpose. We conducted an open-label longitudinal study on the natural health product, OCTA©, a compound mixture of eight herbs, to determine its effects on perceptions of stress. Eighteen participants were enrolled in the study and were followed over a period of 3 months. Primary endpoints included scores from four validated questionnaires (SF-36v2, PSS, STAI and BDI-II), serum DHEA, ALT, AST and creatinine all measured at 12 weeks. Seventeen patients completed the study. Except for the physical summary score of the SF36 questionnaire, all the subjective scores indicated a highly significant (P < 0.0001) improvement in the participants' ability to cope with stress. No adverse effects were reported and there was no evidence of damage to the liver or kidney based on serum markers. Initial evidence for this polyherbal compound supports its potential as an effective ‘adaptogenic’ aid in dealing with stress. Further research using a randomized controlled design is necessary to confirm the findings from this pilot study.
Keywords: adaptogen, CAM, clinical trial, complementary and alternative medicine, herbal medicine, stress
Introduction
Stress is an extremely broad term that serves to define a wide variety of phenomena that humans are exposed to throughout their lives. The facets of stress are essentially limitless; however, broad categories include physical exertion, emotional upset, persistent psychological pressure, existential crisis and the residual effects of emotional trauma. The 1993 World Labour Report by the UN's International Labour Organization claimed that stress had become one of the most serious health issues of the 20th century (1). Stress and its resultant comorbidity are responsible for a large proportion of disability worldwide. It has consistently been shown that individuals experiencing stress have impaired physical and mental functioning; more workdays lost, impairment at work and increased use of healthcare services. The disability caused by stress is just as great as the disability caused by workplace accidents or other common medical conditions such as hypertension, diabetes and arthritis (2). The World Health Organization (WHO) Global Burden of Disease Survey estimates that mental disease, including stress-related disorders, will be the second leading cause of disability by the year 2020 (3).
Since the characterization of the generalized adaptation syndrome (GAS) by Hans Selye, the issue of stress has come to be viewed as a risk factor in both the etiology and progression of a wide variety of diseases. Chronic and post-traumatic stress has been implicated in cardiovascular disease (4–6), gastrointestinal ulceration (7), inflammatory bowel disease (7), depression (8,9), anxiety (9), fibromyalgia (10), autoimmune disease (11) and schizophrenia (12). In addition, chronic stress clearly demonstrates the ability to negatively impact immune system function and can predispose a person toward infection (13–15). Evidence also demonstrates that stress very early in life, i.e. within the first few years of childhood, may be an etiological agent for the development of type 1 diabetes (16) and also potentially in the development and severity of asthma (17).
Normally the stress response is activated on an acute basis and the body is able to return to normal parasympathetic homeostasis. Stress becomes pathologic, however, when it is chronic or when the body acquires an inherent tendency towards activation of the sympathetic nervous system (15,18). Current therapies for dealing with ‘stress’ are extensive but perhaps not ideally targeted in most cases. Pharmacological approaches are principally focused on the treatment of depression and the manifestations of both acute and chronic anxiety disorders (19).
A potentially beneficial use of herbal medicine involves the use of herbs as ‘adaptogens’ in order to prevent stress-induced morbidity. From an herbalist's perspective, the therapeutic intent of an adaptogen is to promote an optimal physiological response to both internal and external stresses. Essentially the adaptogen supports the body's ability to ‘adapt’ ideally to its environment. These herbs are believed to have a bimodal function of action either by providing a stimulant effect or a sedative effect depending on the needs of the individual in a particular situation. Common examples of adaptogens include Asian ginseng (L. Panax ginseng), Siberian ginseng (Eleutherococcus senticosus), Ashwagandha root (Withania somnifera) and rhodiola (L. Rhodiola rosea) (20). Herbs are not the only potential adaptogens as other agents like vitamins and even amino acids have also exhibited this kind of activity (21).
In the 1950s, Russian scientists set out specific criteria that an herb had to incorporate in order to be considered an adaptogen. The criteria were that the herb must (i) only cause minimal disorders in physiological function; (ii) must increase resistance to external and internal stresses through a wide range of physical, chemical, and biochemical factors; and (iii) must have a normalizing effect, improving all types of conditions while aggravating none (22,23). Specific examples of how adaptogens have been taken to improve health include their usage to: reduce fatigue, regain or improve athletic performance, regain or improve mental acuity, increase appetite, relieve insomnia, improve mood and increase resistance against infection (15,23,24). For an intriguing discussion on how adaptogens may impact health, the reader is referred to a series of articles published by Olalde Rangel et al. in 2005 (25–28).
Relatively little clinical research has been conducted on the use of herbal adaptogens for stress, and still less on combinations of herbal medications. In this paper, we report on the results of an open-label uncontrolled longitudinal trial on the use of a proprietary herbal compound mixture, OCTA©, on subjective parameters of stress as well as objective measures.
Methods
Design and Participants
We conducted an open-label and uncontrolled clinical trial to evaluate the impact of OCTA© on known parameters of stress. We enrolled 18 participants between the ages of 21 and 58 years old (mean 39.5 years) with a relatively even sex distribution (8 males and 10 females). Self-reported stress levels at enrollment were initially evaluated using the Perceived Stress Level test. For inclusion, participants had to have experienced one or more illnesses potentially related to stress including anxiety, arthritis, chronic pain, depression, diabetes, eczema, headaches, heart attacks, heart disease, impotence, decreased libido, high blood pressure or peptic ulceration. Participants were excluded from enrollment if they were under 18 years old, were pregnant, planning to become pregnant or were taking any of the following medications: glucocorticoids, androgens, birth control pills, anti-seizure drugs, diuretics, barbiturates, sedatives or anxiolytics.
Participants were recruited through newspaper and radio advertisements run for a period of 2 weeks. The message conveyed was that we were looking for individuals adversely affected by stress. As compensation for their involvement, participants were offered a $50 gift certificate and a free nutritional consultation at the completion of the study. Participants were not required to be actively seeking treatment. Interested participants contacted the study coordinator (R.S.) and attended an information session that detailed the protocol. The timing, severity and history of the participants' complaints were not assessed. Only subjective questionnaires were used to measure changes in outcome but not with respect to the particular complaint or chief concern of the participants but rather to measure overall changes in quality of life.
We conducted a physical examination to rule out underlying pathology. Participants were advised to exclude any supplements designed to mitigate the effects of stress including any natural health products that weren't taken for general health. The only supplements consumed by any of the participants included multivitamins, flax oil and vitamin C. The participants were advised to continue their lifestyle, maintain their normal diet and vitamin consumption and change nothing except for the addition of the OCTA©. Participants were followed over a 3 month period and asked to come in for assessment at predefined time points including at baseline, 2 weeks, 4 weeks, 8 weeks, and 12 weeks. At each time point, the participants were administered self-reported standardized questionnaires, had their blood pressure monitored and had blood samples taken for specific laboratory tests. To be enrolled, participants had to sign an informed consent form and be assessed by a physician. Participants were permitted to ask questions at any time during the study.
Intervention
Participants were provided with the proprietary herbal compound OCTA©, an aqueous-based liquid herbal preparation consisting of eight herbs as follows: W. somnifera, Lagerstroemia speciosa, Bacopa monniera, Zizyphus jujuba, Morinda citrifolia, Punica granatum, Shisandrae chinensis and Lycium barbarum (listed in descending order according to respective concentrations). Participants were instructed to consume two tablespoons (30 ml) of the herbal compound per day each morning for a total period of 3 months.
The product has been through quality control testing and has demonstrated consistent concentrations of the herbal extracts. The two main ingredients are derived from standardized extracts (W. somnifera: 2.5% with anolides; and L. speciosa: 1% corosolic acid). OCTA© has been under review by Health Canada's Natural Health Products Directorate (NHPD) since 2004 but due to a backlog of requests has yet to be processed. The manufacturer adheres to GMP standards and is certified by Australia's Therapeutics Goods Administration (TGA), the Department of Health of the State of New Jersey, and has received an ‘A’ rating from the National Nutritional Foods Association (NNFA).
Outcome Measures
Study endpoints assessed and analyzed for each of the participants consisted of both objective and subjective measures. Aside from serum dehydroepiandrosterone (DHEA), the objective measures were not primary outcomes but were included in order to assess for patient safety and the potential for liver or kidney toxicity. Secondary objective measures included blood pressure, cholesterol levels, aspartate transaminase (AST), alanine transaminase (ALT) and urinary creatinine. Primary outcome measures consisted of subjective scores from four self-reported questionnaires including the perceived stress scale, the state/trait anxiety scale, the beck depression index and the SF36 Health Survey (Version 2) questionnaire. These questionnaires, described briefly below, were chosen because they have been validated and are widely accepted amongst healthcare professionals.
The SF36 Health Survey (SF-36v2) questionnaire is one of the most extensively used and validated quality of life measures. It is a self-administered, 36-item questionnaire that measures health-related quality of life in 8 domains that consist of both physical and mental-related issues. The physical and mental scores can be summarily added in order to obtain overall summaries of each of these two distinct areas. The reliability of the test is well documented with a Cronbach's alpha value greater than 0.85 (29).
The Perceived Stress Scale (PSS) is the most widely used psychological instrument for measuring the perception of stress. It is a self-reported, uni-dimensional instrument developed to measure a perceived stress in a person's life. It is a measure of the degree to which situations in one's life are appraised as stressful. The scale also includes a number of direct queries about current levels of experienced stress. Moreover, the questions are of a general nature and hence are relatively free of content specific to any subpopulation group.
The State-Trait Anxiety Inventory (STAI) was initially conceptualized as a research instrument for the study of anxiety in adults. It is a self-reported assessment device that includes separate measures of state and trait anxiety. According to the author of this tool, state anxiety reflects a ‘transitory emotional state or condition of the human organism that is characterized by subjective, consciously perceived feelings of tension and apprehension, and heightened autonomic nervous system activity’. State anxiety may fluctuate over time and can vary in intensity. In contrast, trait anxiety denotes ‘relatively stable individual differences in anxiety proneness…’ and refers to a general tendency to respond with anxiety to perceived threats in the environment (30).
The Beck Depression Inventory Second Edition (BDI-II) is a 21-item self-reporting instrument intended to assess the existence and severity of symptoms of depression as listed in the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM-IV; 1994). This new revised edition replaces the BDI and the BDI-1A, and includes items intending to index symptoms of severe depression, which would require hospitalization. Items have been changed to indicate increases or decreases in sleep and appetite, items labeled body image, work difficulty, weight loss and somatic preoccupation were replaced with items labeled as agitation, concentration difficulty and loss of energy. Many statements were reworded resulting in a substantial revision of the original BDI and BDI-1A. When presented with the BDI-II, a patient is asked to consider each statement as it relates to the way they have felt for the past 2 weeks, to more accurately correspond to the DSM-IV criteria.
Statistical Analyses
Results were analyzed using one-way ANOVA. Scores for each test as well as the objective samples were independently assessed and only in the case of the SF-36v2 was the test divided into physical and psychological summary categories.
Results
We enrolled 18 participants for the 12 week period. Seventeen participants completed the trial. One participant withdrew due to scheduling conflicts. Table 1 displays the overall effects of OCTA© on primary subjective outcomes. Table 2 reports results from the SF-36v2 Quality of Life results in all eight domains. Table 3 displays selected objective outcome measures including serum DHEA levels, urinary creatinine and levels of the liver enzymes AST and ALT. No significant changes in blood pressure and cholesterol were observed in any of the participants (data not shown). None of the participants reported self-perceived adverse events, nor were any observed by the monitoring physician.
Table 1.
Subjective score summaries of the self-reported questionnaires
| Perceived stress scale | State anxiety scale | Trait anxiety scale | Beck depression scale | SF-36 physical summary | SF-36 mental summary | |
|---|---|---|---|---|---|---|
| Initial | 25.11 | 53.44 | 53.33 | 23.94 | 46.75 | 27.57 |
| Week 2 | 20.29 | 44.65 | 50.18 | 16.65 | 50.29 | 34.25 |
| Week 4 | 18.25 | 40.69 | 45.25 | 12.38 | 49.10 | 39.56 |
| Week 8 | 15.88 | 35.94 | 42.82 | 10.35 | 51.84 | 41.78 |
| Week 12 | 13.53 | 32.24 | 39.71 | 7.82 | 51.09 | 47.50 |
| Change | 11.58 | 21.21 | 13.63 | 16.12 | 4.35 | 19.92 |
| % Change | 46.12 | 39.68 | 25.55 | 67.33 | 9.30 | 72.25 |
| F-value | 10.95 | 10.67 | 7.09 | 9.33 | 1.44 | 11.51 |
| P-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 | 0.23 | <0.0001 |
Table 2.
SF-36v2 Quality of life results: individual categories
| Physical function | Physical limitation | Body pain | General health | Vitality | Social function | Emotional limitation | Mental health | |
|---|---|---|---|---|---|---|---|---|
| Initial | 47.09 | 36.99 | 41.15 | 41.07 | 35.09 | 32.91 | 28.88 | 32.64 |
| Week 2 | 48.86 | 43.02 | 46.33 | 44.94 | 43.64 | 38.88 | 34.16 | 37.75 |
| Week 4 | 48.09 | 43.54 | 47.56 | 45.81 | 45.26 | 43.56 | 37.41 | 42.44 |
| Week 8 | 51.59 | 45.90 | 50.11 | 49.23 | 47.50 | 44.34 | 40.79 | 45.37 |
| Week 12 | 51.71 | 47.92 | 49.59 | 51.28 | 50.62 | 47.87 | 46.96 | 48.68 |
| Change | 4.61 | 10.93 | 8.44 | 10.21 | 15.53 | 14.95 | 18.08 | 16.04 |
| % Change | 9.80 | 29.56 | 20.50 | 24.86 | 44.25 | 45.44 | 62.58 | 49.14 |
Table 3.
Objective measures including toxicity data
| Serum DHEA (μmol l−1) | Aspartate transaminase (U l−1) | Alanine transaminase (U l−1) | Urinary creatinine (μmol l−1) | |
|---|---|---|---|---|
| Initial | 4.12 | 21.50 | 20.50 | 11.84 |
| Week 2 | 4.64 | 23.00 | 21.56 | 10.68 |
| Week 4 | 4.20 | 22.44 | 20.79 | 11.46 |
| Week 8 | 4.32 | 22.47 | 21.12 | 10.55 |
| Week 12 | 4.65 | 21.88 | 20.24 | 11.27 |
| Change | 0.54 | 0.38 | −0.26 | −0.58 |
| % | 13.03 | 1.78 | −1.29 | −4.86 |
| F-value | 0.118 | 0.155 | 0.087 | 0.254 |
| P-value | 0.97 | 0.96 | 0.99 | 0.91 |
For our primary outcomes, we observed a 46% improvement in self-perceived stress. The state and trait anxiety scale reported overall changes from baseline of 40 and 26%, respectively. The Beck Depression Index improved by 67%. For the SF-36 questionnaire, the mental summary score improved by 72%. Each of these results was statistically significant with P-values all <0.0001. The physical summary of the SF-36 demonstrated a modest improvement of 9%; however, this was not statistically significant (P = 0.228). ANOVA of serum DHEA demonstrated no change from baseline (P = 0.98).
Discussion
The findings of this trial should be of interest to physicians and patients alike. We found an overall improvement in perceptions of stress and quality of life due to changes associated with stress as monitored by valid stress and quality of life markers.
Limitations
There are several limitations to consider in our trial. As this is a pilot trial, we did not use a randomized controlled design, thus limiting the strength of inference. Additionally, we cannot determine the extent of any potential changes, benefit or harm, to internal organs apart from liver and renal function. It is also quite possible that even though acute adverse effects were not witnessed over the 3 month trial, a longer time period of consumption might lead to unforeseen side effects and possible organ toxicity.
Strengths
Several important strengths to this study deserve mention. Primarily, this trial is the first to assess this herbal combination on stress levels in a clinical setting. In addition, we used well-validated self-reporting tools and tested over an extended period of time. The participants were monitored for adverse effects and compliance through oral reporting and the use of a daily journal. Compliance as indicated by dosing times recorded in the journal was found to be excellent (>80%). To establish significance we used cut-offs (P ≤ 0.01) far beyond the standard significance threshold (P ≤ 0.05).
Complementary and alternative medicine (CAM) intervention research has often been based on a mind–body medicine approach with an emphasis on relaxation techniques like yoga, meditation and modified breathing techniques (31,32). Another approach in CAM which has not received as much attention is the use of ingested natural health products to provide a pharmacological action in order to provide an ‘adaptogenic’ or protective effect against stress. Our pilot study addresses some of this knowledge gap by assessing the effects of a combined herbal compound, OCTA©, on parameters of stress and its effects on the mental state of the individual. If the results of our trial are to be trusted and assumed to not solely be due to placebo, then we can infer that this polyherbal compound does have a specific effect and could be an effective aid in controlling at least some of the negative psychological manifestations of stress.
Stress Physiology and Adaptogenic Effect
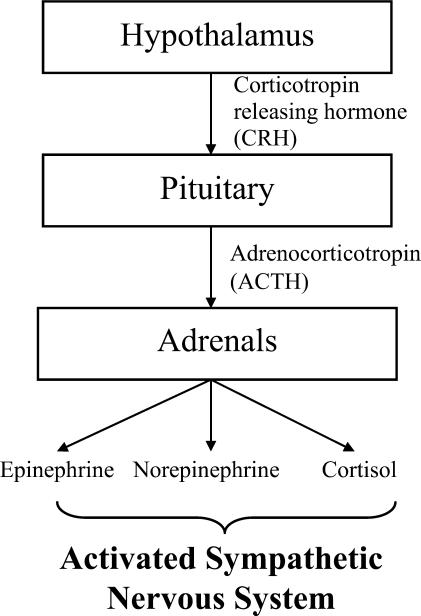
Exemplified in the relatively new field of psychoneuroimmunology, stress invariably leads to a systemic physiological response with implications for the maintenance of both health and predisposition towards disease (14,33). The physiology of stress has been well characterized with an emphasis on the hypothalamic–pituitary–adrenal axis. Briefly, we know that the immune system and the nervous system are in constant communication and are held in a subtle balance that can be distorted by the impact of stress. Three key players, the hypothalamus, pituitary gland and adrenal glands are considered principal effectors in transmitting and amplifying the stress signal (11). The hypothalamus releases corticotrophin-releasing hormone (CRH) that then stimulates the adjacent pituitary gland to secrete adrenocorticotropin hormone (ACTH). In turn, circulating ACTH stimulates the adrenal gland to secrete epinephrine, norepinephrine and ultimately cortisol into the bloodstream resulting in the classic symptoms of the fight or flight response (Fig. 1). It is important to note that many cytokines and inflammatory modulators feed into the stress signal at different physiological points and are also critical in their contribution to the overall picture.
Figure 1.
Principal endocrine axis of the sympathetic nervous system.
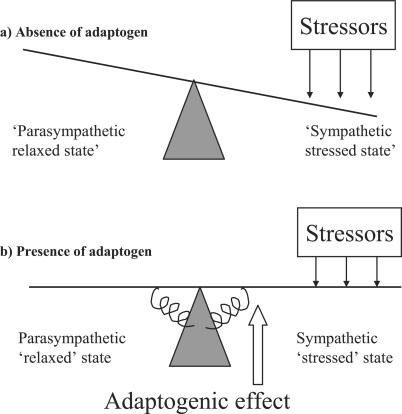
With such a complex system involved in the body's realization of stress, it is plausible that a compound mixture of herbs could have a modulatory and adaptogenic effect on the body's overall response to stress. An analogous representation of the effects of an adaptogen is depicted in the change of a system's tendency towards balance as shown in Fig. 2. This is represented by a simple fulcrum and balance beam. When an adaptogen is added to the system, (i.e. stabilizing damping springs) additional force has to be applied to deviate the balance beam from the horizontal thereby making the system less likely to become perturbed to one side or the other. In this scenario, the adaptogen effectively counteracts the effective ‘weight’ that a stressor has on the system and thus makes it less likely to ‘fall’ into the sympathetic stressed state.
Figure 2.
Counteractive adaptogenic effect against stress.
Whether the potential adaptogenic effect of this compound occurs in the mental state and personal perception of stress, or through the provision of a more direct physicochemical attenuating effect is not answerable by this study. An examination of the different changes in QOL measures, however, does have subtle implications. The fact that the score of mental components of the SF-36 showed dramatic improvements whereas the physical components score changed little implies that the effect may be more psychological than physical. In addition, a possible implication of a lack of a change in physical symptoms from the SF-36 questionnaire is that placebo may not actually account for the lion's share of the changes in the psychological domain. If placebo was indeed the principle effector, then changes should have been noticeable in both the physical and psychological domains and not just in the latter. These implications are purely theoretical however and should be tested in more mechanistic-based research.
Further Research
As well as conducting a controlled trial to eliminate the placebo effect, it would be interesting to conduct research that explores changes in important proinflammatory cytokines including IL-6, TNF and IL-1 as well as examining changes in lymphocyte and neutrophil counts. The use of antioxidants has been shown to reduce stress-induced lymphopenia (34) and it would be optimal to evaluate the impact of the herbs contained within OCTA© either individually or in combination on the immune system in further research.
Conclusion
The lack of adverse effects found in our study as well as an absence of changes in both liver and renal function tests tentatively supports the notion that this herbal mixture is non-toxic. Well-controlled and longer-term studies are needed, however, to establish the long-term effects of this mixture both with regards to efficacy and toxicity. In addition, the small number of participants in our pilot study does not preclude the possibility that serious side effects might occur. While inconclusive, the results from this study are encouraging. Albeit uncontrolled, the pilot study indicates that a polyherbal compound, OCTA©, provides a beneficial adaptogenic effect. The lack of overt and measurable toxicity in all participants is also encouraging and supports the need for more research to better evaluate this polyherbal compound.
Conflict of Interest
Dugald Seely has no conflict of interest to declare. Rana Singh was the clinician in charge of running the trial and was hired to do so by Destiny Health and Wellness the makers of the product OCTA©. Data analysis was conducted independently of the company sponsoring the trial. The sponsoring company, Destiny Health and Wellness, had no input in drafting the manuscript.
References
- 1.World Labour Report. Geneva. UN International Labour Organization; 1993. [Google Scholar]
- 2.Kalia M. Assessing the economic impact of stress—the modern day hidden epidemic. Metabolism. 2002;51(6 Suppl 1):49–53. doi: 10.1053/meta.2002.33193. [DOI] [PubMed] [Google Scholar]
- 3.Murray CJL, Lopez AD. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries and Risk Factors in 1990 and Projected to 2020. Report on Behalf of the WHO and World Bank. Cambridge, MA: Harvard University Press, 1996. [Google Scholar]
- 4.Kawachi I, Sparrow D, Kubzansky LD, Spiro A, 3rd, Vokonas PS. Weiss ST. Prospective study of a self-report type A scale and risk of coronary heart disease: test of the MMPI-2 type A scale. Circulation. 1998;98:405–12. doi: 10.1161/01.cir.98.5.405. [DOI] [PubMed] [Google Scholar]
- 5.Kubzansky LD, Kawachi I, Spiro A, 3rd, Weiss ST, Vokonas PS, Sparrow D. Is worrying bad for your heart? A prospective study of worry and coronary heart disease in the Normative Aging Study. Circulation. 1997;95:818–24. doi: 10.1161/01.cir.95.4.818. [DOI] [PubMed] [Google Scholar]
- 6.Allison TG, Williams DE, Miller TD, Patten CA, Bailey KR, Squires RV, Gau GT. Medical and economic costs of psychologic distress in patients with coronary artery disease. Mayo Clin Proc. 1995;70:734–42. doi: 10.4065/70.8.734. [DOI] [PubMed] [Google Scholar]
- 7.Levenstein S. Psychosocial factors in peptic ulcer and inflammatory bowel disease. J Consult Clin Psychol. 2002;70:739–50. doi: 10.1037//0022-006x.70.3.739. [DOI] [PubMed] [Google Scholar]
- 8.Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. Lancet. 2005;365:1309–14. doi: 10.1016/S0140-6736(05)61027-6. [DOI] [PubMed] [Google Scholar]
- 9.Faragher EB, Cass M, Cooper CL. The relationship between job satisfaction and health: a meta-analysis. Occup Environ Med. 2005;62:105–12. doi: 10.1136/oem.2002.006734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Torpy DJ, Papanicolaou DA, Lotsikas AJ, Wilder RL, Chrousos GP, Pillemer SR. Responses of the sympathetic nervous system and the hypothalamic–pituitary–adrenal axis to interleukin-6: a pilot study in fibromyalgia. Arthritis Rheum. 2000;43:872–80. doi: 10.1002/1529-0131(200004)43:4<872::AID-ANR19>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 11.Torpy DJ, Chrousos GP. The three-way interactions between the hypothalamic–pituitary–adrenal and gonadal axes and the immune system. Baillieres Clin Rheumatol. 1996;10:181–98. doi: 10.1016/s0950-3579(96)80014-8. [DOI] [PubMed] [Google Scholar]
- 12.Corcoran C, Gallitano A, Leitman D, Malaspina D. The neurobiology of the stress cascade and its potential relevance for schizophrenia. J Psychiatr Pract. 2001;7:3–14. doi: 10.1097/00131746-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Gomez-Merino D, Drogou C, Chennaoui M, Tiollier E, Mathieu J, Guezennec CY. Effects of combined stress during intense training on cellular immunity, hormones and respiratory infections. Neuroimmunomodulation. 2005;12:164–72. doi: 10.1159/000084849. [DOI] [PubMed] [Google Scholar]
- 14.Glaser R, Kiecolt-Glaser JK. Stress-induced immune dysfunction: implications for health. Nat Rev Immunol. 2005;5:243–51. doi: 10.1038/nri1571. [DOI] [PubMed] [Google Scholar]
- 15.Kelly GS. Nutritional and botanical interventions to assist with the adaptation to stress. Altern Med Rev. 1999;4:249–65. [PubMed] [Google Scholar]
- 16.Sepa A, Wahlberg J, Vaarala O, Frodi A, Ludvigsson J. Psychological stress may induce diabetes-related autoimmunity in infancy. Diabetes Care. 2005;28:290–5. doi: 10.2337/diacare.28.2.290. [DOI] [PubMed] [Google Scholar]
- 17.Klinnert MD, Nelson HS, Price MR, Adinoff AD, Leung DY, Mrazek DA. Onset and persistence of childhood asthma: predictors from infancy. Pediatrics. 2001;108:E69. doi: 10.1542/peds.108.4.e69. [DOI] [PubMed] [Google Scholar]
- 18.Makino S, Hashimoto K, Gold PW. Multiple feedback mechanisms activating corticotropin-releasing hormone system in the brain during stress. Pharmacol Biochem Behav. 2002;73:147–58. doi: 10.1016/s0091-3057(02)00791-8. [DOI] [PubMed] [Google Scholar]
- 19.Nutt DJ. Overview of diagnosis and drug treatments of anxiety disorders. CNS Spectr. 2005;10:49–56. doi: 10.1017/s1092852900009901. [DOI] [PubMed] [Google Scholar]
- 20.Rege NN, Thatte UM, Dahanukar SA. Adaptogenic properties of six rasayana herbs used in ayurvedic medicine. Phytother Res. 1999;13:275–91. doi: 10.1002/(SICI)1099-1573(199906)13:4<275::AID-PTR510>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 21.Gupta V, Gupta A, Saggu S, Divekar HM, Grover SK, Kumar R. Anti-stress and adaptogenic activity of l-arginine supplementation. Evid Based Complement Alternat Med. 2005;2:93–7. doi: 10.1093/ecam/neh054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saleeby JP. Wonder Herbs: A Guide to Three Adaptogens. Philadelphia: Xlibris Corporation; 2006. [Google Scholar]
- 23.Davydov M, Krikorian AD. Eleutherococcus senticosus (Rupr. & Maxim.) Maxim. (Araliaceae) as an adaptogen: a closer look. J Ethnopharmacol. 2000;72:345–93. doi: 10.1016/s0378-8741(00)00181-1. [DOI] [PubMed] [Google Scholar]
- 24.Kelly GS. Rhodiola rosea: a possible plant adaptogen. Altern Med Rev. 2001;6:293–302. [PubMed] [Google Scholar]
- 25.Olalde Rangel JA. The systemic theory of living systems and relevance to CAM: Part I: the theory. Evid Based Complement Alternat Med. 2005;2:13–8. doi: 10.1093/ecam/neh068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Olalde Rangel JA. The systemic theory of living systems and relevance to CAM: the theory (Part II) Evid Based Complement Alternat Med. 2005;2:129–37. doi: 10.1093/ecam/neh093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Olalde Rangel JA. The systemic theory of living systems and relevance to CAM: the theory (Part III) Evid Based Complement Alternat Med. 2005;2:267–75. doi: 10.1093/ecam/neh119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Olalde Rangel JA, Magarici M, Amendola F, del Castillo O. The systemic theory of living systems. Part IV: systemic medicine—the praxis. Evid Based Complement Alternat Med. 2005;2:429–39. doi: 10.1093/ecam/neh139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brazier JE, Harper R, Jones NM, O'Cathain A, Thomas KJ, Usherwood T, Westlake J. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. Br Med J. 1992;305:160–4. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spielberger CD, Gorusch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory (Self-Evaluation Questionnaire) Palo Alto, CA: Consulting Psychologist Press; 1970. [Google Scholar]
- 31.Monti DA, Yang J. Complementary medicine in chronic cancer care. Semin Oncol. 2005;32:225–31. doi: 10.1053/j.seminoncol.2004.11.026. [DOI] [PubMed] [Google Scholar]
- 32.Ray O. The revolutionary health science of psychoendoneuroimmunology: a new paradigm for understanding health and treating illness. Ann NY Acad Sci. 2004;1032:35–51. doi: 10.1196/annals.1314.004. [DOI] [PubMed] [Google Scholar]
- 33.Dantzer R. Somatization: a psychoneuroimmune perspective. Psychoneuroendocrinology. 2005;30:947–52. doi: 10.1016/j.psyneuen.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 34.Shi Y, Devadas S, Greeneltch KM, Yin D, Allan Mufson R, Zhou JN. Stressed to death: implication of lymphocyte apoptosis for psychoneuroimmunology. Brain Behav Immun. 2003;17(Suppl 1):S18–26. doi: 10.1016/s0889-1591(02)00062-4. [DOI] [PubMed] [Google Scholar]