Abstract
CAM therapies have become increasingly popular in pediatric populations. Yet, little is known about children's preferences for CAM. This study examined treatment preferences in chronic pediatric pain patients offered a choice of CAM therapies for their pain. Participants were 129 children (94 girls) (mean age = 14.5 years ± 2.4; range = 8–18 years) presenting at a multidisciplinary, tertiary clinic specializing in pediatric chronic pain. Bivariate and multivariate analyses were used to examine the relationships between CAM treatment preferences and patient's sociodemographic and clinical characteristics, as well as their self-reported level of functioning. Over 60% of patients elected to try at least one CAM approach for pain. The most popular CAM therapies were biofeedback, yoga and hypnosis; the least popular were art therapy and energy healing, with craniosacral, acupuncture and massage being intermediate. Patients with a diagnosis of fibromyalgia (80%) were the most likely to try CAM versus those with other pain diagnoses. In multivariate analyses, pain duration emerged as a significant predictor of CAM preferences. For mind-based approaches (i.e. hypnosis, biofeedback and art therapy), pain duration and limitations in family activities were both significant predictors. When given a choice of CAM therapies, this sample of children with chronic pain, irrespective of pain diagnosis, preferred non-invasive approaches that enhanced relaxation and increased somatic control. Longer duration of pain and greater impairment in functioning, particularly during family activities increased the likelihood that such patients agreed to engage in CAM treatments, especially those that were categorized as mind-based modalities.
Keywords: functional impairment, mind–body approaches, pain management, pediatric pain, quality of life
Introduction
Recent work suggests that the use of CAM in pediatric populations is increasing substantially (1). Several studies have reported estimated rates of CAM use in various pediatric populations (2–18). However, these estimates vary widely from as low as 2% in the general pediatric population (3) to as high as 73% in a sample of children with cancer (10). Comparisons across studies are complicated by numerous factors including a lack of consensus regarding the definition of CAM, examination of different pediatric populations and variations in survey methodology. Moreover, existing studies have been conducted across several different countries, where attitudes and availability of CAM therapies may differ. In the United States (US), a recent population-based study representative of the general population of children under age 18 years estimated CAM use at only 1.8% (3). However, this study only included respondents who had consulted a CAM practitioner. Previous research suggests that nearly half of US adults who used CAM did so without consulting a practitioner (19) (for example, taking herbal supplements on one's own), and thus some have suggested that this study likely underestimated use of CAM among children in the US (20,21).
In the general US adult population, chronic pain is one of the main conditions for which CAM is used (22–24). No existing population-based studies have delineated specific conditions for which CAM is used in children. Nevertheless, it is recognized that children with chronic conditions that may not respond to conventional medicine have especially high rates of CAM use (25). Several reports indicate increased prevalence of CAM use among pediatric patients with cancer (31–73%) (5,9,10,14,26), juvenile rheumatoid arthritis (70%) (16) and cystic fibrosis (66%) (27). A recent study found that children with chronic illnesses (i.e. cancer, cerebral palsy and inflammatory bowel disease) were three times more likely to use CAM than healthy children (8). In many of these chronic conditions, pain may be a significant problem.
Despite the high prevalence of CAM use in children with chronic illnesses, little is known regarding patient preferences for specific CAM therapies. A recent randomized trial of adults with low back pain found that patients who expected to receive greater benefit from acupuncture than from massage were more likely to demonstrate better clinical outcomes with acupuncture than with massage, and vice versa (28). These findings point to the importance of assessing patient expectations and preferences for specific CAM approaches. We recently examined the expected benefits of CAM and conventional therapies in children and their parents presenting for treatment at a multidisciplinary clinic specializing in the treatment of chronic pediatric pain (29). We found that both parents and children expected relaxation and medication to be more beneficial for pain than hypnosis, massage, acupuncture or yoga. However, in this earlier study we did not assess which specific CAM therapies patients actually preferred when offered their choice of CAM approaches as part of a multimodal treatment package. Thus, the purpose of the current study was to examine patients' preferences for individual CAM therapies for chronic pediatric pain. In addition, we examined the relationship between CAM preferences and patient's sociodemographic and clinical characteristics, as well as their self-reported level of functioning across a variety of domains. Impairments in functioning constitute a major factor in lower health-related quality of life (HRQOL) among children with chronic pain (30).
Methods
Participants
Participants were 129 children (94 girls, 72.9%) with a mean age of 14.5 years (SD = 2.4, range = 8–18 years). Children were patients presenting for treatment at a multidisciplinary, tertiary clinic specializing in pediatric chronic pain. Presenting pain diagnoses were (note that percentages sum to more than 100% due to multiple pain diagnoses) 50.4% functional neurovisceral pain disorder (functional bowel, uterine or bladder disorder), 43.4% headaches (migraines; myofascial, vascular, tension, stress-related or other type of headaches), 38.8% myofascial pain (of any part of the body excluding headaches), 12.4% fibromyalgia, 11.6% complex regional pain syndrome, type 1 or type 2 (CRPS-I; CRPS-II) and 1.6% arthritis. Multiple pain diagnoses were evident in 42.6% (n = 55) of the sample. Average duration of symptoms was 46.1 months (SD = 51.8, range = 2–215). Ethnic composition was 70.3% Caucasian, 9.4% Hispanic, 3.1% African-American, 0.8% Asian American/Pacific Islander and 16.4% Other. Parents (115 mothers, 92%) had a mean age of 45.8 years (SD = 6.4, range = 27–67 years). Highest level of parent education was less than 8th grade 0.8%, some high school 3.2%, high school diploma 7.2%, some college or associates degree 31.2%, college degree 24.0% and postgraduate degree 32.8%. Institutional Review Board approved written informed consent forms were completed by parents, and children provided written assent (see below for additional details).
Procedure
A detailed description of the procedures for the administration of the questionnaire data used in this study is available elsewhere (29,31). In brief, prior to patients' initial clinic intake interview, two baseline questionnaire packets, one for the child and one for a parent, were mailed to the home following verbal consent from a parent obtained over the telephone. Written informed consent from parents and written assent from children were obtained either at the initial clinic appointment or prior to an in-home interview for those families who agreed to be interviewed. The questionnaire packets contained instructions that parents and children were to complete them separately, without consulting each other. The questionnaire responses of parents and children provided valuable clinical information and were administered to all patients attending the clinic as part of routine clinical practice. All questionnaire responses were thus reviewed by a research assistant and by the evaluating physician at the time of the initial clinic assessment to clarify ambiguous or missing responses; questions regarding these measures were also answered at this time. The questionnaires assessed demographic and general health information including measures of the child's pain, anxiety and functioning. Only those measures relevant to the current study are discussed below.
Families were offered CAM therapies in the following manner. At the end of the initial clinical evaluation, after the diagnosis (or diagnoses) was explained to the patient and parents by the evaluating physician, the approach to treatment within the biopsychosocial model was described. In addition to medication (if needed) and physical therapy, other non-pharmacological therapies were described. Specifically, the patient and parents were provided with a list of the pain program CAM clinicians, with the type of CAM therapy and therapists' contact information. In addition to providing referrals to psychotherapy and physical therapy, the clinic provides referrals to the following CAM treatments: biofeedback, hypnotherapy, Reiki, acupuncture, Iyengar yoga, art therapy, and craniosacral and massage therapy. The clinical team, including the CAM practitioners, met weekly with the clinic physicians to discuss the progress of each patient. Each practitioner is certified by a recognized national organization in his or her field, and most have been in practice for more than 10 years, often specializing in the treatment of children.
A brief description of each of the CAM therapies was provided by the evaluating physician. Patients and their parents were informed that all of the CAM approaches could be helpful for the child's pain, and to select what they thought would be most useful and that the child wanted to do. The patient and parents were asked to choose at least one therapy from the list, although they were urged to choose more than that if possible. General instructions were provided to select, if possible, at least one primarily mind-based (e.g. hypnosis) and one primarily body-based (e.g. yoga) therapy, although they were informed that all of the therapies likely had impact on both the mind and body. Specifically, patients were told: ‘Here is a list of different complementary therapies. All of them involve the mind and the body. However, some involve work you do with your mind, like hypnotherapy or biofeedback, and some involve work that you do or is done to your body, like yoga, acupuncture or massage, as examples. While they all can be helpful, I want you to choose at least one that primarily focuses on your mind and one on your body.’ Questions that remained about any of the CAM therapies were then answered.
Questionnaire Measures
Pain intensity. A 10 cm visual analogue scale (VAS) was used to represent a continuum from no pain to unendurable pain. The VAS has been established and widely used as a reliable and valid measure of pain intensity with children. This method measured the ‘usual’ level of pain currently experienced by the child.
Demographics. Locally developed questionnaires completed by the parent assessed demographic information for children and parents including age, sex, ethnicity and education.
Child Health Questionnaire (CHQ CF-87) (32). The CHQ CF-87 is a child self-report questionnaire designed to measure the physical and psychosocial well-being of children with and without chronic conditions. It is among the most widely used and well-validated measures for children. Reliability and validity testing have been extensive (32). In a representative sample of US children, the minimum criteria for item internal consistency (≥0.40) was exceeded on average by 94% of all item tests performed, and the average success rate for tests of item discriminant validity was 92% (32). The CHQ child form is comprised of 11 subscales as follows: general health; physical functioning; family cohesion; limitations in school work and activities with friends due to physical problems (physical role functioning); limitations in school work and activities with friends due to emotional difficulties (emotional role functioning); limitations in school work and activities with friends due to behavioral difficulties (behavior role functioning); behavior; mental health; self-esteem; limitations in family activities; bodily pain. Higher scores on the CHQ subscales indicate better functioning. Because the CHQ bodily pain subscale was significantly correlated with the VAS pain intensity ratings (r = −0.47, P < 0.001), our analyses did not include the CHQ bodily pain subscale.
Results
Statistical Analysis
To determine whether the number or type of CAM therapies selected differed between girls and boys, independent t-tests and chi-square tests were used for continuous and categorical data, respectively. These tests were also used to compare sociodemographic and clinical characteristics between patients who selected at least one CAM therapy and those who did not. Pooled-variance t-tests were employed if Levene's tests indicated unequal variance across groups. Differences in preferences for individual CAM approaches in the total sample were examined using Friedman's Rank test (non-parametric equivalent of one-sample repeated measures test). Pearson correlations were conducted to examine the relationship between CAM preferences and sociodemographic [child age, child sex (boys and girls coded as ‘0’ and ‘1’, respectively), parent race/ethnicity (Caucasian versus non-Caucasian), parent education], clinical [pain intensity, pain duration, multiple pain diagnoses (yes/no)] characteristics and functioning (CHQ subscale scores) measures. Correlations were computed for the following: the overall number of CAM therapies chosen; the selection of any CAM (yes/no); the number of mind-based approaches chosen; the number of body-based approaches chosen; the selection (yes/no) of any mind-based and body-based approaches. Mind-based approaches included hypnosis, biofeedback and art therapy. Body-based approaches included yoga, acupuncture, craniosacral and massage. Energy healing was not included in either the mind-based or body-based categories.
Significant bivariate correlates of the CAM preference variables were then subjected to multivariate analysis. Multiple linear regression was used to evaluate the relationship between the independent variable number of CAM approaches selected and the dependent variables identified in the bivariate analyses. To evaluate the predictors of selecting at least one CAM therapy [i.e. any CAM (yes/no)], logistic regression analysis was used including the variables identified in the bivariate analyses. For all multivariate analyses, the predictor variables were entered simultaneously. A standard probability level of 0.05 was used for all analyses.
Descriptive Findings: CAM Preferences
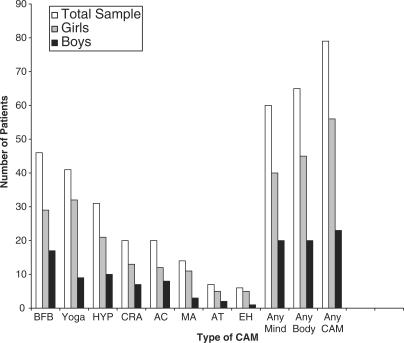
Figure 1 shows the frequency of CAM approaches selected by the total sample and by boys and girls separately. In the total sample, the individual CAM therapies selected were (in order from most to least) as follows: biofeedback (35.7%), yoga (31.8%), hypnosis (24%), acupuncture and craniosacral (tied, both 15.5%), massage (10.9%), art therapy (5.4%) and energy healing (4.7%). The two most frequently chosen CAM modalities (biofeedback and yoga) did not differ from each other but biofeedback (ranked first) was selected significantly more frequently than the third most popular approach, hypnosis (P < 0.05) and the remaining therapies (P < 0.01). Yoga and hypnosis (ranked second and third, respectively) did not differ from each other but both were chosen significantly more frequently than the two fourth ranked approaches, acupuncture and craniosacral (P < 0.01), as well as the remaining modalities (P < 0.01). Acupuncture and craniosacral (both ranked fourth) did not differ from massage, ranked fifth, but were significantly more popular than art therapy and energy healing, ranked sixth and seventh, respectively (P < 0.01). Massage (ranked fifth) did not differ from art therapy or energy healing.
Figure 1.
Frequencies of CAM therapies chosen by patients in the total sample (N = 129) and for girls (n = 94) and boys (n = 35). BFB, biofeedback; HYP, hypnosis; CRA, craniosacral; AC, acupuncture; MA, massage; AT, art therapy; EH, energy healing; Any Mind, at least one mind-based therapy; Any Body, at least one body-based therapy; Any CAM, at least one CAM therapy.
A majority of the total sample (61.2%) agreed to try at least one CAM approach. The mean number of CAM modalities chosen in the total sample was 1.5 (SD = 1.6; range = 0–10). Girls and boys did not differ in the likelihood of selecting any individual CAM therapy, nor did they differ in the likelihood of choosing at least one CAM approach. The number of CAM modalities chosen also did not differ between girls (M = 1.4; SD = 1.7) and boys (M = 1.7; SD = 1.5). Similarly, there were no sex differences in the number of mind-based or body-based therapies selected, or in the likelihood of choosing at least one mind-based or at least one body-based approach.
Comparisons between patients who selected at least one CAM therapy to those who did not choose any CAM interventions revealed that those who chose CAM reported longer pain duration [t(114.8) = −2.2, P < 0.05)], worse physical functioning [t(109.9) = 2.8, P < 0.01)] and worse physical role functioning [t(112) = 2.4, P < 0.05)]. However, there were no group differences in sex, parent race/ethnicity, parent education, presence of multiple diagnoses, pain intensity or the other CHQ subscale scores.
Pain Diagnosis and CAM Preferences
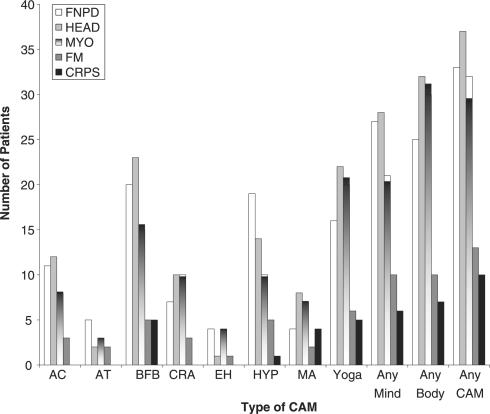
Figure 2 displays the frequency of preferences for each individual CAM approach and for any CAM as well as any mind-/body-based approach by pain diagnosis. Frequencies for the two patients with a diagnosis of arthritis are not shown in the table; these patients elected to try acupuncture, hypnosis and craniosacral. The figure shows that over 80% of patients diagnosed with fibromyalgia chose at least one CAM therapy, the highest proportion of any diagnosis. In contrast, roughly 50% of patients with a diagnosis of functional neurovisceral pain disorder opted to try at least one CAM approach, the lowest proportion of any diagnosis. Approximately two-thirds of patients with diagnoses of headaches, myofascial pain and complex regional pain syndrome (CRPS) selected at least one CAM therapy. As indicated above, over 42% of the sample had more than one diagnosis and thus statistical comparisons of CAM preferences between diagnoses were not conducted. However, as shown in Fig. 2, yoga and biofeedback were the most popular approaches among all the diagnoses. Hypnosis was also among the top therapies selected for all diagnoses except CRPS. On the other hand, art therapy and energy healing were the least popular modalities across all diagnoses.
Figure 2.
Frequencies of CAM preferences by pain diagnosis. FNPD, functional neurovisceral pain disorder (n = 65); HEAD, headaches (n = 56); MYO, myofascial pain (n = 50); FM, fibromyalgia (n =16) CRPS, complex regional pain syndrome, Type 1 or Type 2 (n = 15).
Correlates of CAM Preference
Sociodemographic and Clinical Characteristics
Table 1 shows the bivariate correlations between the sociodemographic and clinical variables and the CAM preference variables. As displayed in the table, all of the CAM preference variables were significantly positively correlated with duration of pain. Thus, longer duration of pain was associated with an increased likelihood of choosing at least one CAM/mind-/body-based therapy, and with selecting a greater number of these therapies. Child age was also positively correlated with selecting at least one body-based approach indicating that older children were more likely to choose these types of therapies.
Table 1.
Bivariate correlations between patient preferences for CAM and sociodemographic and clinical variables
| Child age | Child sex | Parent ethnicity | Parent education | Pain intensity | Pain duration | Multiple diagnoses (yes/no) | |
|---|---|---|---|---|---|---|---|
| Number of CAM | 0.07 | −0.07 | −0.03 | −0.02 | 0.11 | 0.30** | −0.09 |
| Any CAM | 0.12 | −0.06 | −0.07 | −0.01 | 0.14 | 0.19* | −0.08 |
| Number of Mind | 0.02 | −0.14 | 0.02 | −0.01 | 0.13 | 0.24** | −0.04 |
| Any Mind | 0.03 | −0.13 | −0.05 | −0.01 | 0.17 | 0.21* | −0.05 |
| Number of Body | 0.09 | −0.01 | −0.06 | −0.01 | 0.07 | 0.28** | −0.11 |
| Any Body | 0.18* | −0.08 | 0.03 | 0.03 | 0.09 | 0.21* | −0.07 |
Number of CAM, number of CAM therapies selected; Number of Mind, number of mind-based therapies selected; Number of Body, number of body-based therapies selected; Ethnicity, Caucasian versus non-Caucasian; Pain intensity, child self-ratings of pain intensity (0–10); Multiple diagnoses, multiple pain diagnoses (yes/no); **P < 0.01, *P < 0.05.
Child Functioning Scores
Table 2 shows the bivariate correlations between the CAM preference variables and the CHQ subscale scores. As shown in the table, physical functioning and physical role functioning were significantly inversely correlated with choosing any CAM and any mind-based therapy, as well as the number of mind-based approaches. In addition, family activities scores were significantly negatively associated with selecting any mind-based approach as well as the number of these modalities. Thus, greater impairment in functioning across these domains was associated with an increased likelihood of choosing at least one CAM and at least one mind-based therapy, as well as a greater number of mind-based interventions.
Table 2.
Bivariate correlations between patient preferences for CAM and child self-reported functioning (CHQ subscales)
| GH | PF | FC | ERF | BRF | PRF | BE | MH | SE | FA | |
|---|---|---|---|---|---|---|---|---|---|---|
| Number of CAM | −0.02 | −0.17 | −0.04 | 0.01 | −0.13 | −0.13 | −0.08 | −0.03 | 0.04 | −0.15 |
| Any CAM | −0.05 | −0.25** | −0.03 | 0.01 | −0.09 | −0.22* | −0.07 | −0.03 | −0.01 | −0.17 |
| Number of Mind | −0.07 | −0.24* | −0.07 | −0.01 | −0.12 | −0.19* | −0.17 | −0.10 | −0.06 | −0.26** |
| Any Mind | 0.01 | −0.23* | −0.06 | −0.03 | −0.08 | −0.21* | −0.14 | −0.08 | −0.05 | −0.22* |
| Number of Body | 0.03 | −0.09 | −0.02 | 0.01 | −0.10 | −0.08 | 0.01 | 0.03 | 0.12 | −0.03 |
| Any Body | −0.04 | −0.08 | −0.06 | 0.03 | −0.14 | −0.14 | −0.03 | −0.03 | 0.05 | −0.07 |
CHQ, child health questionnaire; GH, general health; PF, physical functioning; FC, family cohesion; ERF, emotional role functioning; BRF, behavior role functioning; PRF, physical role functioning; BE, behavior; MH, mental health; SE, self-esteem; FA, family activities; **P < 0.01, *P < 0.05.
Multivariate Results: Predictors of CAM Preferences
Based on the bivariate findings, the following predictors were examined in multivariate analyses: pain duration, physical functioning scores, physical role functioning scores and family activities scores. Multivariate analyses were not conducted on the number of body-based approaches selected or the selection of at least one body-based modality as pain duration was the only significant correlate identified in the bivariate analyses.
Number of CAM and Number of Mind–Body Therapies
Results of the multiple linear regression analysis examining the number of CAM and number of mind-based approaches selected are shown in Table 3. The model significantly predicted the number of CAM modalities chosen, explaining 14% (10% adjusted) of the variance. However, only the beta coefficient for pain duration was significantly different from zero (P < 0.01). Pain duration accounted for 10% of unique variance in the prediction of the number of CAM therapies selected. Also shown in Table 3, the model significantly predicted the number of mind–body approaches selected, explaining 14% (10% of the variance). The beta coefficients for pain duration and family activities scores were both significantly different form zero (P < 0.05), accounting for 5 and 4%, respectively, of unique variance.
Table 3.
Multiple linear regression of pain duration and functioning scores on the number of CAM and mind-based approaches selected
| Dependent variable | Variables entered | β | Model R2 | Adjusted R2 |
|---|---|---|---|---|
| Number of CAM | Pain duration | 0.32** | 0.14 | 0.10 |
| Physical functioning | −0.15 | |||
| Physical role functioning | 0.06 | |||
| Family activities | −0.13 | |||
| Number of mind-based | Pain duration | 0.22* | 0.14 | 0.10 |
| Physical functioning | −0.16 | |||
| Physical role functioning | 0.08 | |||
| Family activities | −0.25* |
β, standardized regression coefficient; Model R2, coefficient of determination (goodness of fit) for overall regression model after entry of each independent variable; change in R2, incremental contribution of an independent variable to R2 in the total set of independent variables; **P < 0.01, *P < 0.05.
Selection of Any CAM and Any Mind–Body Therapy
Table 4 displays the results of the logistic regression analysis examining the predictors of selecting at least one CAM approach. The overall model explained 13% of the variance in choosing any CAM (Cox and Snell R2). The significant odds ratio (OR) in Table 4 indicates that a 1 unit increase in pain duration increased the likelihood of choosing any CAM by 1.02 units. The overall classification rate for the model with all predictors included was 61.0%, with 75.0% of patients who selected any CAM and 39.0% of patients who did not select any CAM, correctly classified. Also shown in Table 4 are the results of the logistic regression for selecting at least one mind-based therapy. The complete model accounted for 11% of the variance in choosing any mind-based approach (Cox and Snell R2). A significant OR was found for pain duration, indicating that a 1 unit increase in pain duration increased the likelihood of choosing any mind-based therapy by 1.01 units. The overall classification rate for the model with all predictors included was 67.9%, with 50.0% of patients who selected any mind-based approach and 81.7% of patients who did not select any mind-based approach, correctly classified.
Table 4.
Logistic regression of pain duration and functioning scores on selection of any CAM and of any mind-based approach
| Dependent variable | Predictor variable | B | Odds ratio | 95% CI |
|---|---|---|---|---|
| Any CAM | Pain duration | 0.02 | 1.02* | 1.00–1.03 |
| Physical functioning | −0.02 | 0.98 | 0.96–1.00 | |
| Physical role functioning | −0.01 | 1.00 | 0.98–1.01 | |
| Family activities | −0.01 | 1.00 | 0.97–1.02 | |
| Any mind | Pain duration | 0.01 | 1.01* | 1.00–1.02 |
| Physical functioning | −0.01 | 0.99 | 0.97–1.01 | |
| Physical role functioning | −0.01 | 1.00 | 0.99–1.01 | |
| Family activities | −0.02 | 0.98 | 0.96–1.01 |
B, unstandardized regression coefficient; CI, confidence interval; *P < 0.05, **P < 0.01.
Discussion
Our findings indicate that when given a choice of a wide range of CAM therapies, over 60% of patients presenting to a tertiary pediatric pain clinic elect to try at least one CAM approach for pain. In this sample, boys and girls exhibited similar preferences for such therapies. However, our bivariate findings revealed that older children were more likely to select body-based modalities (i.e. yoga, acupuncture, craniosacral, massage and energy healing) than younger children although preferences for mind-based approaches (i.e. hypnosis, biofeedback and art therapy) did not vary by age. The most popular CAM therapies were biofeedback, yoga and hypnosis, and the least popular were art therapy and energy healing; craniosacral, acupuncture and massage were intermediate (see Fig. 1). Examination of CAM preferences by pain diagnosis revealed that more than 80% of patients diagnosed with fibromyalgia opted to try at least one CAM approach, compared to 50% of patients with a functional neurovisceral pain disorder and roughly two-thirds of patients with headaches, myofascial pain or CRPS (see Fig. 2). It should be noted that more than 40% of the current sample presented with more than one pain diagnosis.
Additional bivariate findings indicated that increased pain duration was positively associated with selecting at least one CAM therapy and at least one mind-based and body-based approach, as well as selecting a greater number of these therapies (see Table 1). Our bivariate results also revealed that greater child-reported impairments in physical functioning, school work and activities with friends due to physical problems, and family activities were associated with an increased likelihood of selecting any mind-based therapy, as well as selecting a greater number of mind-based approaches (see Table 2). Similar results were obtained for the selection of any CAM therapy. Multivariate analyses revealed that pain duration was a significant predictor of the number of CAM approaches selected, accounting for 10% of unique variance (see Table 3). In logistic regression analyses, pain duration emerged as the only significant predictor of the likelihood of selecting any CAM and any mind-based approach (see Table 4). Multivariate analysis examining the number of mind-based approaches chosen revealed that pain duration and limitations in family activities were both significant predictors, accounting for 5 and 4%, respectively, of unique variance (see Table 3). Thus, longer duration of pain and greater impairment in family activities were both associated with selecting a greater number of mind-based therapies for pain.
CAM Preferences and Children's Functional Ability
The above findings suggest that pediatric chronic pain patients' decisions regarding the use of CAM may be influenced by both clinical aspects (e.g. pain duration), as well as children's functional abilities across an array of settings including the home and school. The finding that longer duration of pain is strongly predictive of an increased willingness to try CAM approaches is not surprising in light of previous work reporting that pediatric CAM use is highest in children with chronic conditions such as cancer (5,9,10,14,26) and cystic fibrosis (27) in which pain may be a prominent feature. Since it is parents who typically transport the child to the CAM treatment site and pay for the treatments (or complete insurance forms) they may play a significant role in the choices of CAM interventions for children with chronic pain. Thus, duration of pain may become a salient factor in seeking CAM therapies because, after pain persists despite multiple medications and many visits to specialist physicians, parents might be more inclined to ‘try something else’.
To our knowledge, no prior studies have examined the relationship between children's functional ability and preferences for CAM. Impaired functioning has been shown to contribute substantially to lower HRQOL in children with chronic pain (30). Our multivariate findings suggest that the greater children's perceived limitations in their ability to participate in family activities, the more likely they are to try a greater number of mind-based approaches for their pain. It is possible that the impact of the child's pain on disruption of family activities might add further impetus for parents to have their child seek care from a CAM clinician. The finding that children's functional impairment showed a stronger relationship to preferences for mind-based versus body-based CAM modalities may be due to lower feelings of self-efficacy in carrying out body-based interventions, or the interest of parents and children in learning some new skill that involves less physical effort to cope with the pain. Future studies using qualitative methods to analyze patient's reasons for selecting individual CAM modalities may shed light on this issue.
Study Limitations
Caveats to our findings should be mentioned. When the CAM therapies were presented to families, they were urged to choose at least one mainly mind-based and one mainly body-based therapy. It is possible that categorizing the CAM therapies in this way by the clinic physicians when presenting the list of therapies may have influenced families' decision-making. Nevertheless, patients were informed that all of the approaches would likely impact both the mind and the body. Future studies may examine the extent to which patients understand such categorization and the extent to which these classifications impact patients' preferences for CAM therapies. Relatedly, some families may have been unfamiliar with CAM approaches and asked questions about the therapies. Whereas this additional discussion regarding the CAM therapies may have influenced physicians' descriptions of the therapies as well as patients' ultimate decisions regarding which approaches to engage in, it should be noted that this process closely resembles the way in which treatment decisions are made in clinical practice. That is, clinicians typically describe to patients the range of possible treatment options and patients' decisions regarding which approaches to try are based on this information as well as patients' requests for additional information. Future studies may investigate the extent to which patients' familiarity with CAM therapies might influence treatment preferences for CAM.
Other limitations concern our sample composition. Our sample was predominantly white (over 70%) and highly educated (over 56% with college or postgraduate degree), and therefore the present findings may be limited in their generalizability. On the other hand, the demographic profile of our sample is typical of specialty pediatric pain clinics. It should be noted that the restricted range of demographic characteristics in the present sample likely accounts for the lack of significant associations between the CAM preference variables and parent education and race/ethnicity (Caucasian versus non-Caucasian). Previous research in adults indicates that higher education and higher income are associated with greater CAM use (33). This latter finding may relate to the limited CAM modalities covered by most health insurance, thus requiring out of pocket expenses. Although we did not assess insurance status, it is unclear the extent to which insurance status would have impacted choice of CAM given that most CAM treatments are not covered. Moreover, it is likely that insurance status would not have varied substantially given the overall high socioeconomic status (e.g. more than 50% with college degree or higher) of this sample.
CAM and Pediatric Pain Management
Another potential limitation is that our clinic offered only certain types of CAM therapies and thus our findings may not be applicable to all pediatric pain clinics. However, Lin et al. (34) recently examined the provision of CAM in 43 major, accredited pediatric anesthesia centers in the US. Of these, 38 (86%) provided one or more CAM therapies for pediatric pain management. The prevalence of CAM treatments offered were as follows: biofeedback (65%), guided imagery (49%), hypnosis (44%), massage (35%), relaxation therapy (33%), acupuncture (33%), art therapy (21%), meditation (21%), therapeutic touch (21%), music therapy (19%), self-help groups (7%), herbal remedies (5%), yoga (4%), tai-chi (4%) and chiropractic (2%). None of the institutions provided spiritual healing or homeopathic remedies for their pediatric pain patients. It is notable that the CAM therapies offered by our clinic are largely consistent with those provided by these 38 centers.
The study by Lin et al. (34) indicates that CAM interventions are now being integrated into pediatric pain management services throughout the US, although the availability of individual CAM therapies appears to vary across institutions. Our present findings suggest that for children with chronic pain complaints, non-invasive approaches that enhance relaxation and increase somatic control (i.e. biofeedback, Iyengar yoga and hypnosis) are the most frequently chosen, irrespective of pain diagnosis. In addition, patients with widespread, diffuse pain (i.e. fibromyalgia) are more likely to engage in CAM modalities than those with more localized pain complaints. Longer duration of pain and greater impairment in functioning, particularly during family activities, increases the likelihood that such patients are willing to engage in CAM treatments, especially those that were classified as mind-based modalities (i.e. hypnosis, biofeedback and art therapy). Future studies should examine the extent to which patient preferences for specific CAM interventions ‘cluster’ together—that is, do patients who choose a particular intervention (e.g. yoga) also tend to choose other specific modalities (e.g. acupuncture)? Additional studies may also investigate whether there are any clear patterns of CAM preferences among pediatric pain patients that differ according to pain diagnosis or other patient characteristic(s). The growing interest in CAM therapies for pain in pediatric populations has focused increased attention on questions of safety and efficacy (35). These considerations should be addressed in rigorous, randomized controlled trials in order to establish those CAM modalities that hold the most promise for the treatment of chronic pediatric pain.
Acknowledgments
This study was supported by 1R01MH063779, awarded by the National Institute of Mental Health (PI; M.C.J.).
References
- 1.Ottolini MC, Hamburger EK, Loprieato JO, Coleman RH, Sachs HC, Madden R, et al. Complementary and alternative medicine use among children in the Washington, DC area. Ambul Pediatr. 2001;1:122–5. doi: 10.1367/1539-4409(2001)001<0122:caamua>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 2.Braganza S, Ozuah PO, Sharif I. The use of complementary therapies in inner-city asthmatic children. J Asthma. 2003;40:823–7. doi: 10.1081/jas-120023574. [DOI] [PubMed] [Google Scholar]
- 3.Davis MP, Darden PM. Use of complementary and alternative medicine by children in the United States. Arch Pediatr Adolesc Med. 2003;157:393–6. doi: 10.1001/archpedi.157.4.393. [DOI] [PubMed] [Google Scholar]
- 4.Faw C, Ballentine R, Ballentine L, van Eys J. Unproved cancer remedies. A survey of use in pediatric outpatients. JAMA. 1977;238:1536–8. doi: 10.1001/jama.238.14.1536. [DOI] [PubMed] [Google Scholar]
- 5.Friedman T, Slayton WB, Allen LS, Pollock BH, Dumont-Driscoll M, Mehta P, et al. Use of alternative therapies for children with cancer. Pediatrics. 1997;100:E1. doi: 10.1542/peds.100.6.e1. [DOI] [PubMed] [Google Scholar]
- 6.Jensen P. Use of alternative medicine by patients with atopic dermatitis and psoriasis. Acta Derm Venereol. 1990;70:421–4. [PubMed] [Google Scholar]
- 7.Lim A, Cranswick N, Skull S, South M. Survey of complementary and alternative medicine use at a tertiary children's hospital. J Paediatr Child Health. 2005;41:424–7. doi: 10.1111/j.1440-1754.2005.00659.x. [DOI] [PubMed] [Google Scholar]
- 8.McCann LJ, Newell SJ. Survey of paediatric complementary and alternative medicine use in health and chronic illness. Arch Dis Child. 2006;91:173–174. doi: 10.1136/adc.2004.052514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mottonen M, Uhari M. Use of micronutrients and alternative drugs by children with acute lymphoblastic leukemia. Med Pediatr Oncol. 1997;28:205–8. doi: 10.1002/(sici)1096-911x(199703)28:3<205::aid-mpo10>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 10.Neuhouser ML, Patterson RE, Schwartz SM, Hedderson MM, Bowen DJ, Standish LJ. Use of alternative medicine by children with cancer in Washington state. Prev Med. 2001;33:347–54. doi: 10.1006/pmed.2001.0911. [DOI] [PubMed] [Google Scholar]
- 11.Pendergrass TW, Davis S. Knowledge and use of “alternative” cancer therapies in children. Am J Pediatr Hematol Oncol. 1981;3:339–45. [PubMed] [Google Scholar]
- 12.Reznik M, Ozuah PO, Franco K, Cohen R, Motlow F. Use of complementary therapy by adolescents with asthma. Arch Pediatr Adolesc Med. 2002;156:1042–4. doi: 10.1001/archpedi.156.10.1042. [DOI] [PubMed] [Google Scholar]
- 13.Sawni-Sikand A, Schubiner H, Thomas RL. Use of complementary/alternative therapies among children in primary care pediatrics. Ambul Pediatr. 2002;2:99–103. doi: 10.1367/1539-4409(2002)002<0099:uocata>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 14.Sawyer MG, Gannoni AF, Toogood IR, Antoniou G, Rice M. The use of alternative therapies by children with cancer. Med J Aust. 1994;160:320–2. [PubMed] [Google Scholar]
- 15.Simpson N, Roman K. Complementary medicine use in children: extent and reasons. A population-based study. Br J Gen Pract. 2001;51:914–6. [PMC free article] [PubMed] [Google Scholar]
- 16.Southwood TR, Malleson PN, Roberts-Thomson PJ, Mahy M. Unconventional remedies used for patients with juvenile arthritis. Pediatrics. 1990;85:150–4. [PubMed] [Google Scholar]
- 17.Thomas KJ, Carr J, Westlake L, Williams BT. Use of non-orthodox and conventional health care in Great Britain. Br Med J. 1991;302:207–10. doi: 10.1136/bmj.302.6770.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Verhoef MJ, Russell ML, Love EJ. Alternative medicine use in rural Alberta. Can J Public Health. 1994;85:308–9. [PubMed] [Google Scholar]
- 19.Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States: prevalence, costs, and patterns of use. N Engl J Med. 1993;328:246–252. doi: 10.1056/NEJM199301283280406. [DOI] [PubMed] [Google Scholar]
- 20.Ente G. Prevalence of complementary and alternative medicine use in US children. Arch Pediatr Adolesc Med. 2004;158:292. doi: 10.1001/archpedi.158.3.292. [DOI] [PubMed] [Google Scholar]
- 21.Rosen LD. Complementary and alternative medicine use in children is underestimated. Arch Pediatr Adolesc Med. 2004;158:291. doi: 10.1001/archpedi.158.3.291-c. [DOI] [PubMed] [Google Scholar]
- 22.Astin JA. Why patients use alternative medicine: results of a national study. JAMA. 1998;279:1548–53. doi: 10.1001/jama.279.19.1548. [DOI] [PubMed] [Google Scholar]
- 23.Bausell RB, Lee W, Berman BM. Demographic and health-related correlates of visits to complementary and alternative medical providers. Med Care. 2001;39:190–196. doi: 10.1097/00005650-200102000-00009. [DOI] [PubMed] [Google Scholar]
- 24.Eisenbeg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, et al. Trends in alternative medicine use in the United States, 1990–1997. JAMA. 1998;280:1569–75. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 25.Ernst E. Prevalence of complementary/alternative medicine for children: a systematic review. Eur J Pediatr. 1999;158:7–11. doi: 10.1007/s004310051000. [DOI] [PubMed] [Google Scholar]
- 26.Grootenhuis MA, Last BF, de Graaf-Nijkerk JH, van der Wel M. Use of alternative treatment in pediatric oncology. Cancer Nurs. 1998;21:282–8. doi: 10.1097/00002820-199808000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Stern RC, Canda ER, Doershuk CF. Use of nonmedical treatment by cystic fibrosis patients. J Adolesc Health. 1992;13:612–5. doi: 10.1016/1054-139x(92)90376-m. [DOI] [PubMed] [Google Scholar]
- 28.Kalauokalani D, Cherkin DC, Sherman KJ, Koepsell TD, Deyo RA. Lessons from a trial of acupuncture and massage for low back pain: patient expectations and treatment effects. Spine. 2001;26:1418–24. doi: 10.1097/00007632-200107010-00005. [DOI] [PubMed] [Google Scholar]
- 29.Tsao JCI, Meldrum M, Bursch B, Jacob MC, Kim SC, Zeltzer LK. Treatment expectations for CAM interventions in pediatric chronic pain patients and their parents. Evid Based Complement Alternat Med. 2005;2:521–7. doi: 10.1093/ecam/neh132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Palermo TM. Impact of recurrent and chronic pain on child and family daily functioning: A critical review of the literature. J Dev Behav Pediatr. 2000;21:58–69. doi: 10.1097/00004703-200002000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Bursch B, Tsao JCI, Meldrum M, Zeltzer LK. Preliminary validation of a self-efficacy scale for child functioning despite chronic pain (child and parent versions) Pain. 2006;125:35–42. doi: 10.1016/j.pain.2006.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Landgraf JM, Abetz L, Ware JE. Boston, MA: The Health Institute; 1999. The CHQ: A User's Manual (2nd printing). HealthAct (1st printing) [Google Scholar]
- 33.Foltz V, St Pierre Y, Rozenberg S, Rossignol M, Bourgeois P, Joseph L, et al. Use of complementary and alternative therapies by patients with self-reported chronic back pain: a nationwide survey in Canada. Joint Bone Spine. 2005;72:571–7. doi: 10.1016/j.jbspin.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 34.Lin YC, Lee AC, Kemper KJ, Berde CB. Use of complementary and alternative medicine in pediatric pain management service: a survey. Pain Med. 2005;6:452–8. doi: 10.1111/j.1526-4637.2005.00071.x. [DOI] [PubMed] [Google Scholar]
- 35.Tsao JC, Zeltzer LK. Complementary and alternative medicine approaches for pediatric pain: a review of the state-of-the-science. Evid Based Complement Alternat Med. 2005;2:149–59. doi: 10.1093/ecam/neh092. [DOI] [PMC free article] [PubMed] [Google Scholar]