CASE DESCRIPTION
A 32 year-old-man presents with concerns of 4 events (lasting ∼25 sec) of recently “acting out” his dreams, occurring 1–2 hours after sleep onset. The episodes are sudden, bizarre, purposeful, violent movements of jumping and running across the bed to protect his wife against an apparent intruder. The most recent event involved injury to his wife as he tried to forcefully grab her by the arms; during this episode, he also bit his tongue with residual bleeding. All events end with his wife grabbing him by the hands, at which time he is calm, confused with poor recollection of his actions, but with feelings of remorse. Although the patient denied hypersomnia, he did report inability to concentrate on days following the events.
Four years prior the patient had surgical correction of a left frontal lobe cavernous angioma. Postsurgical evolution and recent health status were uneventful. He has a regular sleep-wake schedule with 8 hours total sleep duration. Family history was notable for 2 uncles with chronic somnambulism. Physical exam was unremarkable.
- Which of the following would be the best next step?
- Sleep-deprived electroencephalography (EEG)
- Video polysomnography (PSG)
- Brain magnetic resonance imaging (MRI)
- Anticonvulsant therapy
- Cerebrospinal fluid analysis
Answer: B
DISCUSSION
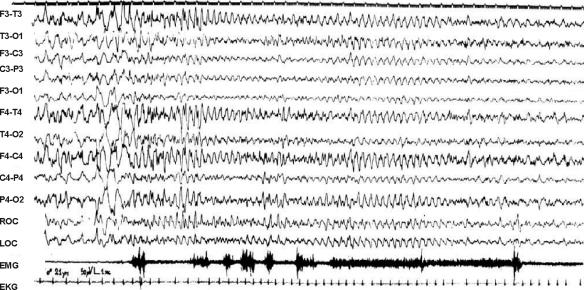
This patient has nocturnal frontal lobe epilepsy (NFLE) due to the location of the epileptic discharge noted in the PSG (Figure 1) and the complex “somnambulistic” behavior. NFLE should be suspected in the presence of frequent stereotyped paroxysmal nocturnal motor events arising or persisting into adulthood. Video-PSG is mandatory to confirm the diagnosis.1,2 Typically patients lack daytime seizures and are otherwise asymptomatic during wake states. Daytime symptoms expressed by this patient are likely explained by the nocturnal seizures leading to sleep architecture alteration and poor sleep quality.3
Key.
EMG (electromyography), EKG (electrocardiogram), LOC (left outer canthus), ROC (right outer canthus)
The timing of the events suggests occurrence during NREM sleep. NFLE is known to typically occur during NREM sleep, related to the hypersynchrony present during this stage of sleep that may facilitate the onset and/or spread of certain partial seizures.4
NFLE seizures appear most frequently between 14 and 20 years of age with predominant male predilection, but can affect any age and tend to increase in frequency during life.5 A few cases present with antecedents such as birth anoxia, febrile convulsions, or head injury. In this case, the previous brain surgery may be a factor.
Physical exam and MRI are typically nondiagnostic; however, in the familial form, brain positron emission tomography (PET) imaging may show hyperperfusion in epileptogenic foci.6 The familial form is characterized by an autosomal dominant transmission in chromosome 20 with altered acetylcholine receptors. This form of epilepsy is responsive to treatment with carbamazepine in up to a third of patients.7 Carbamazepine, likely due to acetylcholine sodium channel stabilization, remains the drug of choice with clinical effectiveness in up to two-thirds of patients.5,8 Patients who tolerate the seizures may elect no treatment. This form of epilepsy is usually clinically and biologically heterogeneous, which may account for the different presentations described in this patient's family.5
During the evaluation for suspected seizures, sleep-deprived EEG is widely used clinically to trigger epileptiform discharges. However, the reproducibility of this form of test has been questioned.9 Half of the patients with NFLE have normal interictal EEG tracings, and clinical history is the principal diagnostic tool. The other half may have some discrete changes during sleep EEG tracing.
It is often clinically difficult to distinguish this form of epilepsy from REM-sleep behavior disorder (RBD) as they may present similarly, however, the timing of the events early during the night suggests a NREM parasomnia. In addition, RBD typically occurs in older men. The lack of reported symptom-based autonomic activation speaks against nocturnal panic attacks and night terrors, although interestingly, autonomic activation such as increased heart rate is also frequently noted in NFLE.5
Footnotes
Disclosure Statement
This was not an industry supported study. Drs. Fahed and Mehra have indicated no financial conflicts of interest.
REFERENCES
- 1.Aldrich MS, Jahnke B. Diagnostic value of video-EEG polysomnography. Neurology. 1991;41:1060–6. doi: 10.1212/wnl.41.7.1060. [DOI] [PubMed] [Google Scholar]
- 2.Zucconi M, Ferini-Strambi L. NREM parasonmias: arousal disorders and differentiation from nocturnal frontal lobe epilepsy. Clin Neurophysiol. 2000;111(Suppl 2):S129–35. doi: 10.1016/s1388-2457(00)00413-2. [DOI] [PubMed] [Google Scholar]
- 3.Vignatelli L, Bisulli F, Naldi I, et al. Excessive daytime sleepiness and subjective sleep quality in patients with nocturnal frontal lobe epilepsy: a case-control study. Epilepsia. 2006;47(Suppl 5):73–7. doi: 10.1111/j.1528-1167.2006.00882.x. [DOI] [PubMed] [Google Scholar]
- 4.Park SA, Lee BI, Park SC, et al. Clinical courses of pure sleep epilepsies. Seizure. 1998;7:369–77. doi: 10.1016/s1059-1311(05)80005-6. [DOI] [PubMed] [Google Scholar]
- 5.Provini F, Plazzi G, Montagna P, Lugaresi E. The wide clinical spectrum of nocturnal frontal lobe epilepsy. Sleep Med Rev. 2000;4:375–86. doi: 10.1053/smrv.2000.0109. [DOI] [PubMed] [Google Scholar]
- 6.Hayman M, Scheffer IE, Chinvarun Y, Berlangieri SU, Berkovic SF. Autosomal dominant nocturnal frontal lobe epilepsy: demonstration of focal frontal onset and intrafamilial variation. Neurology. 1997;49:969–75. doi: 10.1212/wnl.49.4.969. [DOI] [PubMed] [Google Scholar]
- 7.Picard F, Bertrand S, Steinlein OK, Bertrand D. Mutated nicotinic receptors responsible for autosomal dominant nocturnal frontal lobe epilepsy are more sensitive to carbamazepine. Epilepsia. 1999;40:1198–209. doi: 10.1111/j.1528-1157.1999.tb00848.x. [DOI] [PubMed] [Google Scholar]
- 8.Post RM. Time course of clinical effects of carbamazepine: implications for mechanisms of action. J Clin Psychiatry. 1988;49(Suppl):35–48. [PubMed] [Google Scholar]
- 9.Malow BA, Passaro E, Milling C, Minecan DN, Levy K. Sleep deprivation does not affect seizure frequency during inpatient video-EEG monitoring. Neurology. 2002;59:1371–4. doi: 10.1212/01.wnl.0000031810.15811.9e. [DOI] [PubMed] [Google Scholar]