Abstract
Study Objectives:
To gain some insight into how various behavioral (lifestyle) factors influence sleep duration, by investigation of the relationship of sleep time to waking activities using the American Time Use Survey (ATUS).
Design:
Cross-sectional data from ATUS, an annual telephone survey of a population sample of US citizens who are interviewed regarding how they spent their time during a 24-hour period between 04:00 on the previous day and 04:00 on the interview day.
Participants:
Data were pooled from the 2003, 2004, and 2005 ATUS databases involving N=47,731 respondents older than 14 years of age.
Interventions:
N/A
Results:
Adjusted multiple linear regression models showed that the largest reciprocal relationship to sleep was found for work time, followed by travel time, which included commute time. Only shorter than average sleepers (<7.5 h) spent more time socializing, relaxing, and engaging in leisure activities, while both short (<5.5 h) and long sleepers (≥8.5 h) watched more TV than the average sleeper. The extent to which sleep time was exchanged for waking activities was also shown to depend on age and gender. Sleep time was minimal while work time was maximal in the age group 45–54 yr, and sleep time increased both with lower and higher age.
Conclusions:
Work time, travel time, and time for socializing, relaxing, and leisure are the primary activities reciprocally related to sleep time among Americans. These activities may be confounding the frequently observed association between short and long sleep on one hand and morbidity and mortality on the other hand and should be controlled for in future studies.
Citation:
Basner M; Fomberstein KM; Razavi FM; Banks S; William JH; Rosa RR; Dinges DF. American time use survey: sleep time and its relationship to waking activities. SLEEP 2007;30(9):1085-1095.
Keywords: time use, sleep time, work, travel, television, mortality, morbidity
INTRODUCTION
BOTH SHORT AND LONG HABITUAL SLEEP TIME WERE FOUND TO BE ASSOCIATED WITH INCREASED RISKS OF MORTALITY AND MORBIDITY OR WITH DISEASE promoting risk factors. While the first report appeared more than 40 years ago,1 the number of studies on this topic has increased markedly since 2000.
A systematic review of the literature (Simpson et al,2 in press) identified 18 studies examining the relationship of sleep duration to mortality. In total, these studies suggest that self-reported sleep duration is associated with all-cause mortality. Of the 18 published studies, 12 found some relationship (median sample size 9126) between sleep duration and mortality, and 6 studies did not (median sample size 3022). The relationship was found more often in men than women, and more often for both short (<7 hours) and long sleep (≥8 hours) than for either alone.
Other than mortality, short habitual sleep time has been associated with elevated body mass index (BMI),3–7 self-rated poor health,8 low blood levels of leptin and high blood levels of ghrelin,4 while associations with both short and long habitual sleep durations have been found for hypertension,9,10 diabetes,11–13 and impaired glucose tolerance.12
However, 2 factors complicate the interpretation of the observed association between sleep time and morbidity and mortality. First, it is impossible to establish a causal link between short or long habitual sleep duration and mortality and morbidity on the basis of observational studies alone. Sleep is one of the basic human needs that both affects and is affected by numerous lifestyle, socioeconomic, and health related factors.14,15 Therefore, causality is likely to flow in both directions. Prospective randomization of sleep duration would be necessary to confirm a causal link between sleep time and morbidity and mortality.30
Second, numerous factors may be related to both short or long habitual sleep time and morbidity or mortality, potentially confounding their association. Some epidemiological studies1,16 did not adjust for confounding at all (besides age), while others adjusted for up to 32 confounders.3 Factors often adjusted for across studies were demographic characteristics (e.g., age, gender, race, education, martial status), health behaviors (e.g., smoking habits, exercise level, diet), and prior health conditions (e.g., BMI, history of heart disease, diabetes, hypertension). Nevertheless, there may still be residual but important confounding factors that have not yet been identified. In a recent publication, Patel et al.14 investigated the association of psychiatric, lifestyle, socioeconomic, and medical factors with short and long sleep duration. They found that a large number of the studied factors had a U-shaped distribution with respect to sleep duration, whereby both short and long sleepers were more likely to have characteristics associated with poor health. They pointed out that potential confounders not only need to be associated with prolonged or short sleep times, but they also need to be prevalent to explain the associations between sleep time and mortality. Conversely, overadjustment may also play a role in epidemiological studies2 (e.g., if short or long sleep causes heart disease, then correcting for history of heart disease might obscure an underlying effect of sleep duration).
In this paper we investigate another factor that complicates drawing conclusions on the causal relationship between short and long sleep times and morbidity and mortality. Both short and long habitual sleep times are necessarily paired with greater or lesser amounts of waking activity. Therefore, it may not be reduced or increased sleep times per se that lead to higher risks of morbidity and mortality, but rather the associated changes in waking activity. Although it has been reported that short sleepers and long sleepers differ from average sleepers in psychological characteristics17 and health,14 there is limited knowledge about differences in waking activities between subjects with habitual sleep times below and above the average. Modern humans frequently alter the timing and duration of sleep in exchange for other activities. This appears to be especially the case in current industrialized societies, where the biological imperative to sleep sometimes opposes the cultural imperative to be awake.18 Here, sleep may be perceived as a flexible commodity that is traded for other activities considered more pressing or of greater value.19 Although there are many candidate waking activities that could have a reciprocal relationship to sleep among Americans, there have been no systematic data presented on this topic. This study used data from the publicly available American Time Use Surveys (ATUS) conducted in the years 2003, 2004, and 2005, on a representative population sample of U.S. citizens, to investigate sleep time and its relationship to waking activities. Age, gender, day of the week, and other potentially important variables were considered in the analysis.
METHODS
ATUS Survey
ATUS is a federally administered, continuous survey on time use in the United States sponsored by the Bureau of Labor Statistics and conducted by the U.S. Census Bureau. The goal of the survey is to measure how people divide their time among life's activities in a nationally representative sample. ATUS participants are randomly selected from a subset of the households that complete their eighth and final month interviews for the Current Population Survey (CPS). Demographic information—including sex, race, age, educational attainment, occupation, income, marital status, and the presence of children in the household—is available from the CPS, but only some of those variables are updated during the ATUS interview. ATUS contains no information on BMI or any health-related factors.
For the present analyses, ATUS databases for the years 2003, 2004, and 2005 were merged. In 2003, 3375 households leaving the CPS sample were selected for the ATUS sample each month. Because of budgetary cutbacks beginning in December 2003, the monthly ATUS sample was reduced by 35% to 2194 per month. To ensure reliable measures of time spent on weekdays and weekend days, 10% of the sample was allocated to each weekday, and 25% to each weekend day.
Section 9 of Title 13, United States Code, ensures that all respondent and household information obtained via ATUS remains confidential. The U.S. Office of Management and Budget (OMB) approved the survey.
Participants
ATUS covers all residents living in the 105 million households in the United States ≥15 years of age, with the exception of active military personnel and people residing in institutions such as nursing homes and prisons. ATUS involves a stratified, 3-stage sample. In the first stage of selection, the CPS over-sample in less-populous states was reduced. In the second stage of selection, households were stratified based on the following characteristics: race/ethnicity of the householder, presence and age of children, and number of adults in adults-only households. In the third stage of selection, an eligible person from each household selected in the second stage was randomly selected to be the designated person for the ATUS interview.
Survey Administration
ATUS involves a telephone survey in which people are interviewed once for 15–20 minutes on a preselected day (days are selected to ensure that the survey captures activities every day in the year) about how they spent their time between 04:00 on the previous day and 04:00 on the interview day, including where they were and whom they were with. Therefore, Sunday covers the period from 04:00 Sunday morning until 04:00 Monday morning. Monday covers the period from 04:00 Monday morning until 04:00 Tuesday morning, etc. All ATUS interviews were conducted from the U.S. Census Bureau's telephone center at the National Processing Center in Jeffersonville, IN. The interviewers attempted calls in 4-call blocks throughout the day and were required to make at least one call in each call block until contact was made with each household. Once a household was contacted and the designated person agreed to participate, the interview was conducted using computer-assisted telephone interviewing (CATI) software. Subjects were compensated $40 for completing the survey. During processing, cases with poor quality (defined as those containing <5 activities, those for which refusals or “don't remember” responses account for ≥3 hours of the 24-hour day, or both) were removed from the database, thus lowering final annual average response rates by 1 to 3 percentage points to 51.2% (2003), 53.1% (2004), and 49.5% (2005).
ATUS Coding
Responses were codified using the ATUS coding lexicon, or activity classification system, a 3-tiered system, with 17 major (first-tier) categories, each having 2 additional levels (tiers) of detail. Each third-tier activity category contains a list of examples of activities that fall into that category. For the 17 different broad categories of activity, the second tier coding is given in the Appendix. “Sleeping” is codified as 01 (1st tier) personal care, 01 (2nd tier) sleeping, with 3 third-order tiers: 01.01.01 “sleeping” (examples: sleeping, falling asleep, dozing off, napping, getting up, waking up, dreaming, catnapping, getting some shut-eye, dozing); 01.01.02 “sleeplessness” (examples: insomnia, tossing and turning, lying awake, counting sheep); and 01.01.99 “sleeping not elsewhere classified.” Categories 01.01.01, 01.01.02, and 01.01.99 were combined for most of the analyses presented below, because people usually either tried to sleep or actually slept in all the situations described in the examples, and because sleeplessness is typically overestimated in insomnia. For convenience, the phrase sleep time is used throughout the paper. However, it is emphasized that, as defined, sleep time captures all sleep periods (including daytime naps) and some activities that describe sleepiness or transitions in or out of sleep rather than sleep itself (e.g., dozing or getting up). Category 01.01.99 (sleep not elsewhere classified) was used in only 4 out of 47,731 respondents.
With 2 exceptions, the 17 ATUS categories were analyzed on the first-tier level. The exceptions were “commuting” (17.05.01), which was extracted from the “travel” category for a subanalysis, and “watching TV” (12.03.03 and 12.03.04), which was extracted from the “socializing, relaxing, leisure” category. If respondents could not remember which activity they pursued during a certain time of the day, this time was allocated to a category called “data code.”
Statistical Analyses
The first part of the analyses was mainly descriptive. Stratified analyses were performed focusing on the relationship of age, gender, and weekday to sleep time, work time, and reported sleeplessness. The Bureau of Labor Statistics and the Census Bureau provide weights for calculating estimates that correct for oversampling of some demographic groups, oversampling of weekend days, and differing response rates across demographic groups and days of the week. These weights (variable TU04FWGT for the 2003 dataset and variable TUFINLWGT for 2004 and 2005 datasets) were used to calculate representative estimates of average time spent sleeping and working per day. Standard errors were calculated with the replicate variance method described in detail in chapter 7 of the ATUS User's Guide.20 In the text, means ± standard errors are reported. Interviews on holidays (N=843) were generally excluded from analyses. Two sample t-tests (SPSS 14.0, SPSS Inc.) were used to investigate differences in sleep times on different days of the week. Age and gender differences in the proportion of respondents who reported any “sleeplessness” during the 24-h period were investigated with univariable logistic regression models using SAS PROC LOGISTIC (version 9.1, SAS Corp.).
The second part of the analyses concentrated on the covariation of sleep time with other waking activities. More specifically, we sought to determine how short and long sleepers differed from respondents with average sleep time in terms of waking activities. For this purpose, 18 linear regression models were evaluated using SAS PROC REG (version 9.1, SAS Corp.). In each model, one of the 18 waking activities served as the dependent variable, while sleep time always served as the independent variable of primary interest. To account for nonlinear relationships and to increase comparability to epidemiological studies, sleep time was divided into 9 categories: <4.5 h, 4.5 h to <5.5 h, 5.5 h to <6.5 h, 6.5 h to <7.5 h, 7.5 h to <8.5 h, 8.5 h to <9.5 h, 9.5 h to <10.5 h, 10.5 h to <11.5 h, and ≥11.5 h. The 7.5 h to <8.5 h sleep time category was chosen as a reference because most of the respondents fell into this category on weekdays. Indicator variables were constructed for the remaining 8 categories. Each model was further adjusted for age and its quadratic (continuous variable centered at age 45), gender, race (white only, black only, other), weekly pay (none; low ≤$430; medium >$430 but ≤$830; and high >$830), educational attainment (< high school, high school, college graduate, graduate school), children present in household (no child present, one or more children present), and spouse or unmarried partner present (for definitions of income and children present in household refer to the ATUS User's Guide20). In this setting, the intercept in our regression models represents average waking activity time for the reference categories (7.5 h to <8.5 h sleep time, age 45 years, female, race white, medium weekly pay, high school degree, no child present in household, and spouse or unmarried partner present in household). Sleep time category regression coefficients express how much a respondent's waking activity time deviated from that observed in respondents with average sleep time, adjusted for the remaining variables in the model. A single regression model with sleep time as the dependent variable was not appropriate, because sleep time and waking activities summed to 24 hours, resulting in regression coefficients of −1 for each waking activity variable (i.e., a waking activity that increased by 1 minute when adjusted for all other waking activities, would necessarily result in sleep time decreasing by 1 minute).
Results
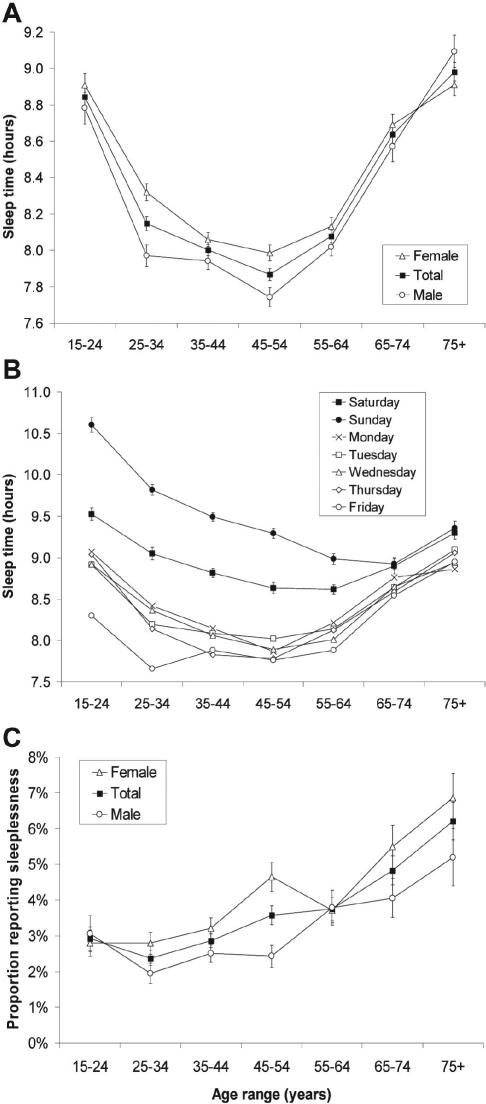
Table 1 summarizes relevant information for the 2003, 2004, and 2005 samples. Figure 1A shows average sleep time on weekdays with respect to age and gender. The relationship between age and sleep time was U-shaped with average sleep time at a minimum at age 45–54 y (7.87 ± 0.03 h) and increasing both with lower and higher age. Maximum sleep time occurred at age 75+y (8.98 ± 0.05 h), i.e., people in this age group slept on average 1 h more than people at age 45–54 y. Except for age group 75+, women slept longer than men in all age groups. The difference in sleep time (which includes all reported sleep) between women and men was prominent up to the age group 45–54 y, and was maximum at 25–34 y with a delta of 21 min. It was markedly decreased in people aged ≥55 y.
Table 1.
Composition of the 2003, 2004 and 2005 ATUS Databases
| ATUS Sample N |
Responder in Database N (%) |
Female (%) |
Mon–Fri N |
Sat+Sun N |
|
|---|---|---|---|---|---|
| 2003 | 40,500 | 20,720 (51.2%) | 56.3% | 10,223 | 10,497 |
| 2004 | 26,328 | 13,973 (53.1%) | 56.2% | 6,950 | 7,023 |
| 2005 | 26,328 | 13,038 (49.5%) | 57.1% | 6,544 | 6,494 |
| All | 93,156 | 47,731 (51.2%) | 56.5% | 23,717 | 24,014 |
Figure 1.
A. Average weekday (Mon–Fri) sleep time depending on age range and gender (Nmale=10,137, Nfemale=13,188). Sleep time includes ATUS tiers 01.01.01 “sleeping,” 01.01.02 “sleeplessness,” and 01.01.99 “sleeping not elsewhere classified” (for examples see Methods). B. Average sleep time depending on age range and day of the week (N=46,888). Each day covers a period from 04:00 on the same day to 04:00 on the next day (e.g., Sunday covers Sunday morning 04:00 to Monday morning 04:00.). Error bars are only shown for weekend days for clarity. C. Proportion of respondents reporting sleeplessness (ATUS category 01.01.02) depending on age range and gender (Nmale=20,393, Nfemale=26,495). The ATUS User's Guide20 gives the following examples for the category “sleeplessness”: insomnia, tossing and turning, lying awake, counting sheep. Error bars in a, b, and c represent standard errors calculated with the replicate variance method described in the ATUS User's Guide.
Figure 1B shows average sleep time with respect to age and day of the week. The U-shaped relationship between age and sleep time that was observed during weekdays in Figure 1A was observed for Saturday and Sunday as well. Average sleep time reached its minimum on weekend days at age ≥55 and on weekdays at age <55. Average sleep time across age groups was highest on Sunday (9.59 ± 0.03 h) followed by Saturday (8.97 ± 0.03 h). It was markedly lower during the week, where it gradually decreased from Monday to Friday (Monday 8.41 ± 0.04 h, Tuesday 8.37 ± 0.03 h, Wednesday 8.34 ± 0.04 h, Thursday 8.28 ± 0.03 h, Friday 8.03 ± 0.04 h). The differences between weekdays (Mon–Fri) were minor compared to the differences between weekdays and weekend days. Pair-wise t-tests indicated that sleep times differed significantly (P <0.05) between all days of the week except for Tuesday and Wednesday (P = 0.998), Tuesday and Thursday (P = 0.119), and Wednesday and Thursday (P = 0.117). However, people ≤34y slept markedly less on Friday compared with the rest of the week (Mon–Thu, P all <0.0001 based on 2 sample t-tests).
Figure 1C shows the proportion of respondents who reported any “sleeplessness” during the 24-h period, as a function of age and gender. Reports of sleeplessness increased with age (P <0.0001) and were more frequent in women compared to men (P <0.0001) except for age groups 15–24 y and 55–64 y. Across all age groups, 3.0% of males and 4.2% of females reported sleeplessness. As shown in Table 2 reports of sleeplessness tended to increase with sleep time, reaching a maximum among respondents reporting sleep times of 11.5 h or more.
Table 2.
Percentage of ATUS Respondents Falling in One of Nine Sleep Time Categories Depending on Day of the Week (Mon–Fri, Sat+Sun) and Gender
| Sleep time category (hours) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| < 4.5 | 4.5 < 5.5 | 5.5 < 6.5 | 6.5 < 7.5 | 7.5 < 8.5 | 8.5 < 9.5 | 9.5 < 10.5 | 10.5 < 11.5 | 11.5 + | Average (SE) | ||
| Mon – Fri | All | 2.5% | 3.4% | 8.5% | 18.2% | 24.3% | 19.3% | 10.9% | 5.9% | 7.1% | 8.28 h (0.02 h) |
| Men | 3.0% | 4.0% | 9.0% | 19.2% | 23.8% | 18.0% | 10.2% | 5.8% | 6.9% | 8.19 h (0.03 h) | |
| Women | 2.0% | 2.8% | 8.1% | 17.2% | 24.7% | 20.5% | 11.5% | 5.9% | 7.2% | 8.37 h (0.02 h) | |
| Sat + Sun | All | 1.8% | 2.1% | 4.6% | 9.3% | 16.2% | 21.0% | 17.6% | 11.9% | 15.5% | 9.27 h (0.02 h) |
| Men | 2.1% | 2.3% | 5.0% | 9.7% | 16.2% | 20.7% | 16.5% | 11.5% | 15.8% | 9.23 h (0.03 h) | |
| Women | 1.5% | 1.9% | 4.1% | 8.8% | 16.2% | 21.3% | 18.6% | 12.4% | 15.2% | 9.33 h (0.02 h) | |
| Pr(Sleeplessness) | 2.9% | 2.8% | 2.4% | 3.2% | 3.4% | 3.1% | 3.5% | 3.9% | 5.4% | 3.4% (0.1%) | |
| Pr(Work = 0) | 34.3% | 31.3% | 31.3% | 34.7% | 44.2% | 58.5% | 70.5% | 76.0% | 85.0% | 53.6% (0.3%) | |
The last two rows show the proportion of respondents reporting sleeplessness (Pr[Sleeplessness]) and the proportion of respondents reporting not to have worked on the day before the interview day (Pr[Work = 0]) depending on sleep time category. SE refers to the standard error calculated with the replicate variance method described in the ATUS User's Guide.20
Table 2 displays average sleep times and the percentage of respondents falling in the nine sleep time categories used for regression analyses with respect to gender and day of the week. If sleep periods initiated between 19:00 and 04:00 are defined as nighttime sleep and those initiated after 04:00 and before 19:00 are defined as daytime sleep; nighttime sleep accounts for 93.5% (7.75 h) of sleep time on weekdays and for 93.3% (8.66 h) of sleep time on weekends, daytime sleep accounts for 5.9% (0.49 h) of sleep time on weekdays and for 6.2% (0.57 h) of sleep time on weekends, and sleeplessness (tier 01.01.02) accounts for only 0.6% (0.05 h) of sleep time on weekdays and for 0.5% (0.04 h) of sleep time on weekends.
The bottom of the table displays the percentage of respondents who reported no compensated work time within each sleep time group. “Compensated work time” is defined by ATUS 1st tier category 05 as “working or work related activities” (see Appendix). These percentages increased with increases in reported sleep time.
Table 3 (weekdays) and Table 4 (weekend) present intercepts of the regression models (corresponding to activity time in respondents sleeping 7.5 h to <8.5 h) together with coefficient estimates for 8 indicator variables representing 8 distinct sleep time ranges. The correlation of sleep time and waking activities is given as Pearson's Rho. As expected, most waking activities were inversely related to sleep time, i.e., they increased when sleep time decreased and vice versa. For some variables, a pronounced increase or decrease was only seen either in short or in long sleepers (so-called J-shaped relationships; see e.g., categories “Education” and “Socializing, Relaxing, Leisure” on weekdays or “Household Activities” and “Volunteer Activities” on weekends). U-shaped relationships were observed for categories “Professional and Personal Care Services” and “Watching TV” on weekdays, “Religion” and “Consumer Purchases” on weekends, and “Eating and Drinking” on both weekdays and weekends.
Table 3.
Results of 18 Multiple Linear Regression Models for Weekdays (N=23,325) Adjusted for Age, Gender, Ethnicity, Educational Attainment, Income, Presence of Partner, and Presence of Children
| Monday – Friday | Reference (min) | Sleep time category (change compared to reference category in min with standard errors) |
rPearson (P-value) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 7.5 < 8.5 | < 4.5 | 4.5 < 5.5 | 5.5 < 6.5 | 6.5 < 7.5 | 8.5 < 9.5 | 9.5 < 10.5 | 10.5 < 11.5 | 11.5 + | ||
| Work | 421.4 (4.5) | +91.7 (8.5) | +68.0 (7.2) | +51.9 (4.9) | +35.9 (3.8) | −37.1 (3.8) | −83.0 (4.6) | −97.8 (5.9) | −131.1 (5.6) | −0.363 (<.0001) |
| Socializing, relaxing, leisure w/o TV | 58.2 (2.9) | +58.7 (5.5) | +27.6 (4.7) | +23.1 (3.2) | +8.2 (2.5) | −0.4 (2.5) | −1.5 (3.0) | −4.3 (3.8) | −22.5 (3.7) | −0.023 (0.0004) |
| Travel | 72.8 (1.7) | +46.6 (3.2) | +22.3 (2.7) | +15.9 (1.9) | +7.3 (1.5) | −6.9 (1.5) | −12.3 (1.8) | −15.5 (2.2) | −29.2 (2.2) | −0.209 (<.0001) |
| Personal care w/o sleep | 55.6 (1.4) | +20.4 (2.7) | +11.1 (2.3) | +6.5 (1.6) | +3.6 (1.2) | −3.7 (1.2) | −4.3 (1.5) | −6.0 (1.9) | −7.4 (1.8) | −0.075 (<.0001) |
| Watching TV | 115.3 (3.3) | +14.0 (6.3) | +13.8 (5.3) | −1.7 (3.6) | −3.9 (2.8) | +6.6 (2.8) | +15.7 (3.4) | +24.8 (4.3) | +11.6 (4.2) | +0.092 (<.0001) |
| Care for non-household members | 14.7 (1.1) | +9.3 (2.1) | +2.8 (1.8) | +0.7 (1.2) | −0.2 (1.0) | −0.9 (1.0) | −2.5 (1.2) | −2.4 (1.5) | −4.6 (1.4) | −0.024 (<.0002) |
| Care for household members | 16.9 (1.7) | +9.2 (3.2) | +2.6 (2.7) | +4.0 (1.9) | +0.9 (1.4) | −1.2 (1.4) | −3.0 (1.8) | −5.6 (2.2) | −11.6 (2.1) | −0.071 (<.0001) |
| Volunteer activities | 1.9 (1.1) | +7.1 (2.0) | +4.2 (1.7) | +3.7 (1.2) | +2.3 (0.9) | −1.4 (0.9) | −1.5 (1.1) | −6.5 (1.4) | −6.7 (1.4) | −0.051 (<.0001) |
| Household activities | 121.6 (2.9) | +6.8 (5.4) | +7.3 (4.6) | +2.1 (3.1) | −1.8 (2.4) | −1.6 (2.4) | +1.9 (3.0) | −15.8 (3.8) | −30.2 (3.6) | −0.011 (0.0886) |
| Phone | 5.5 (0.6) | +6.0 (1.1) | +2.6 (1.0) | +1.6 (0.7) | +0.6 (0.5) | −0.7 (0.5) | −1.5 (0.6) | −2.2 (0.8) | −2.8 (0.8) | −0.024 (0.0003) |
| Prof. and personal care services | 6.0 (0.7) | +4.0 (1.3) | +2.6 (1.1) | −0.1 (0.8) | +0.4 (0.6) | +0.6 (0.6) | +1.9 (0.7) | +1.1 (0.9) | +1.8 (0.9) | +0.016 (0.0179) |
| Sports | 5.9 (1.2) | +3.4 (2.2) | +0.7 (1.9) | +3.2 (1.3) | +1.4 (1.0) | −0.9 (1.0) | −2.3 (1.2) | −5.7 (1.5) | −6.9 (1.5) | −0.029 (<.0001) |
| Consumer purchases | 22.2 (1.0) | +3.1 (2.0) | +1.8 (1.7) | +0.8 (1.1) | −0.4 (0.9) | −0.6 (0.9) | −0.4 (1.1) | +1.3 (1.4) | −4.7 (1.3) | −0.009 (0.1491) |
| Education | −24.0 (2.1) | +2.6 (3.9) | +9.7 (3.3) | +5.8 (2.3) | +3.6 (1.8) | −5.8 (1.8) | −17.9 (2.1) | −31.7 (2.7) | −48.2 (2.6) | −0.033 (<.0001) |
| Household services | +1.2 (0.3) | +1.1 (0.6) | +0.5 (0.5) | −0.3 (0.4) | −0.2 (0.3) | −0.2 (0.3) | −0.3 (0.3) | −0.6 (0.4) | −0.7 (0.4) | −0.010 (0.1098) |
| Religion | 1.9 (0.5) | +0.2 (0.9) | +0.5 (0.7) | +0.7 (0.5) | +0.5 (0.4) | −0.4 (0.4) | −0.8 (0.5) | −0.6 (0.6) | −1.9 (0.6) | −0.013 (0.0427) |
| Government services | 0.4 (0.2) | −0.3 (0.4) | 0.0 (0.3) | −0.1 (0.2) | 0.0 (0.2) | −0.1 (0.2) | −0.1 (0.2) | −0.2 (0.3) | −0.3 (0.2) | −0.002 (0.7606) |
| Eating and drinking | 65.0 (1.1) | −7.2 (2.0) | −2.3 (1.7) | −4.3 (1.2) | −1.0 (0.9) | −2.9 (0.9) | −5.2 (1.1) | −8.2 (1.4) | −14.5 (1.3) | −0.059 (<.0001) |
The intercept of the regression models is shown in the “Reference” column, and represents average waking activity time for the reference categories (7.5 h to <8.5 h sleep time, age 45 years, female, race white, medium weekly pay, high school degree, no child present in household, and spouse or unmarried partner present in household), and the indicator variables for sleep time express how much a respondent's activity time in any given sleep category deviates from the activity time observed in respondents with average sleep time, adjusted for the remaining variables in the model. The last column shows Pearson's moment correlation coefficients of sleep time and the respective waking activity time.
Table 4.
Results of 18 Multiple Linear Regression Models for Weekends (N=23,563) Adjusted for Age, Gender, Ethnicity, Educational Attainment, Income, Presence of Partner, and Presence of Children
| Saturday and Sunday | Reference (min) | Sleep time category (change compared to reference category in min with standard errors) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 7.5 < 8.5 | < 4.5 | 4.5 < 5.5 | 5.5 < 6.5 | 6.5 < 7.5 | 8.5 < 9.5 | 9.5 < 10.5 | 10.5 < 11.5 | 11.5 + | rPearson (P−value) | |
| Work | 110.0 (4.1) | +115.9 (8.3) | +105.9 (7.6) | +75.2 (5.5) | +37.6 (4.2) | −31.1 (3.4) | −50.3 (3.5) | −62.2 (4.0) | −70.9 (3.9) | −0.248 (<.0001) |
| Socializing, relaxing, leisure w/o TV | 138.6 (3.9) | +82.9 (8.1) | +24.0 (7.4) | +25.5 (5.3) | +12.0 (4.1) | −5.2 (3.3) | −17.4 (3.4) | −28.7 (3.9) | −55.9 (3.8) | −0.152 (<.0001) |
| Travel | 89.8 (2.1) | +37.7 (4.3) | +18.2 (3.9) | +20.8 (2.8) | +11.4 (2.2) | −8.2 (1.7) | −17.5 (1.8) | −23.7 (2.1) | −38.1 (2.0) | −0.197 (<.0001) |
| Personal care w/o sleep | 52.1 (1.6) | +40.6 (3.2) | +16.3 (2.9) | +5.3 (2.1) | +3.4 (1.6) | −2.1 (1.3) | −5.7 (1.4) | −6.8 (1.5) | −10.9 (1.5) | −0.102 (<.0001) |
| Watching TV | 156.7 (4.2) | −10.2 (8.7) | −9.4 (7.9) | −14.6 (5.7) | −13.6 (4.4) | +6.2 (3.5) | +13.7 (3.7) | +19.9 (4.1) | +4.8 (4.0) | −0.023 (0.0005) |
| Care for non-household members | 22.5 (1.4) | +9.3 (2.9) | +6.0 (2.6) | −1.1 (1.9) | +2.4 (1.5) | +0.7 (1.2) | −2.1 (1.2) | −4.4 (1.4) | −7.8 (1.4) | −0.059 (<.0001) |
| Care for household members | 17.8 (1.8) | +8.5 (3.7) | +5.0 (3.4) | +3.3 (2.4) | +0.1 (1.9) | −2.6 (1.5) | −8.5 (1.6) | −11.6 (1.8) | −18.6 (1.7) | −0.084 (<.0001) |
| Volunteer activities | 10.0 (1.3) | +1.8 (2.7) | +8.5 (2.4) | +0.3 (1.8) | +4.5 (1.4) | −2.2 (1.1) | −5.1 (1.1) | −6.9 (1.3) | −8.4 (1.2) | +0.136 (<.0001) |
| Household activities | 188.8 (3.7) | +0.2 (7.5) | +4.6 (6.8) | −5.4 (4.9) | −1.5 (3.8) | −2.2 (3.0) | −3.6 (3.2) | −14.7 (3.6) | −36.0 (3.5) | −0.109 (<.0001) |
| Phone | 6.6 (0.7) | +2.7 (1.3) | +1.8 (1.2) | +1.0 (0.9) | +0.2 (0.7) | −1.2 (0.5) | −1.4 (0.6) | −2.7 (0.6) | −4.3 (0.6) | −0.045 (<.0001) |
| Prof. and personal care services | 3.7 (0.5) | +5.7 (1.1) | +0.9 (1.0) | +0.7 (0.7) | +1.0 (0.6) | −0.2 (0.4) | −0.3 (0.5) | −0.5 (0.5) | −0.9 (0.5) | −0.032 (<.0001) |
| Sports | 15.3 (1.8) | +8.3 (3.7) | +5.8 (3.4) | +10.7 (2.4) | +4.3 (1.9) | −3.7 (1.5) | −7.0 (1.6) | −9.6 (1.8) | −11.9 (1.7) | −0.067 (<.0001) |
| Consumer purchases | 50.7 (1.6) | −3.9 (3.3) | −5.5 (3.0) | +0.4 (2.2) | +1.1 (1.7) | −1.4 (1.3) | −0.3 (1.4) | −4.6 (1.6) | −11.0 (1.5) | −0.051 (<.0001) |
| Education | 3.7 (1.3) | −3.3 (2.6) | +4.2 (2.3) | +1.7 (1.7) | −2.2 (1.3) | −2.9 (1.0) | −3.3 (1.1) | −4.2 (1.2) | −4.4 (1.2) | +0.000 (0.9633) |
| Household services | 0.4 (0.2) | −0.7 (0.5) | 0.0 (0.5) | +0.7 (0.3) | −0.2 (0.3) | 0.2 (0.2) | −0.2 (0.2) | −0.5 (0.2) | −0.2 (0.2) | −0.014 (0.0336) |
| Religion | 16.7 (1.4) | −7.3 (3.0) | −4.6 (2.7) | −4.2 (1.9) | −1.6 (1.5) | +1.2 (1.2) | −1.1 (1.3) | −3.7 (1.4) | −8.0 (1.4) | −0.019 (0.0030) |
| Government services | 0.1 (0.1) | 0.0 (0.1) | +0.1 (0.1) | +0.2 (0.1) | +0.1 (0.1) | 0.0 (0.1) | 0.0 (0.1) | ¬−0.1 (0.1) | 0.0 (0.1) | −0.018 (0.0072) |
| Eating and drinking | 74.9 (1.4) | −2.5 (2.9) | −4.0 (2.6) | −1.9 (1.9) | +0.2 (1.4) | ¬−2.4 (1.2) | −4.0 (1.2) | −7.4 (1.4) | −15.1 (1.3) | −0.109 (<.0001) |
The intercept of the regression models is shown in the “Reference” column, and represents average waking activity time for the reference categories (7.5 h to <8.5 h sleep time, age 45 years, female, race white, medium weekly pay, high school degree, no child present in household, and spouse or unmarried partner present in household), and the indicator variables for sleep time express how much a respondent's activity time in any given sleep category deviates from the activity time observed in respondents with average sleep time, adjusted for the remaining variables in the model. The last column shows Pearson's moment correlation coefficients of sleep time and the respective waking activity time.
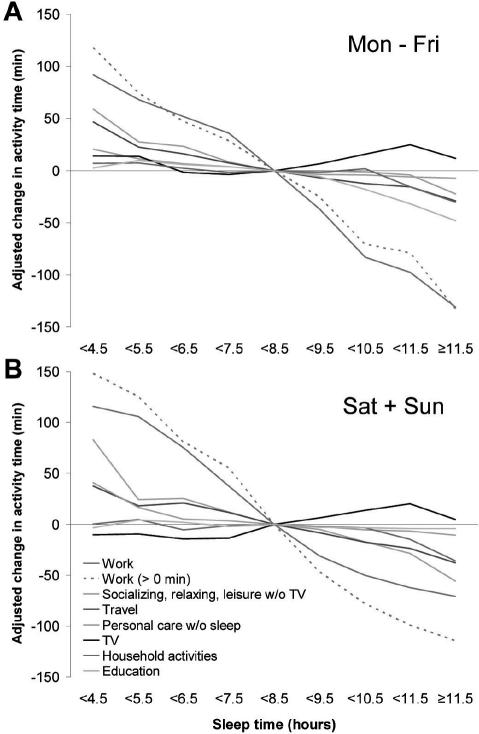
In Figure 2A, adjusted changes in waking activity time with respect to sleep time are shown for 7 categories that exceeded 20 min change in at least one of the sleep categories on weekdays. Work time was the waking activity predominantly exchanged for sleep time across all sleep time categories on both weekdays (r = −0.363, P <0.0001) and weekends (r = −0.248, P <0.0001). Respondents who slept ≤4.5 h worked an average of 93 min more on weekdays (P <0.0001) and 118 min more on weekends (P <0.0001) than the average sleeper, while respondents who slept ≥11.5 h worked an average of 143 min less on weekdays (P <0.0001) and 71 min less on weekends (P <0.0001) than the average sleeper. Additionally, reports of not having worked on the day preceding the interview day increased with increasing sleep time, where 34.3% of respondents sleeping <4.5 h and 85.0% of respondents sleeping >11.5 h reported not having worked (see Table 2). Restricting the analysis to respondents who worked on the day preceding the interview day (work >0, dashed lines in Figures 2A and 2B) did not change the results on weekdays and intensified the inverse relationship between sleep time and work time on weekends. Short sleep was also moderately related to higher amounts of travel time on both weekdays (rPearson = −0.209, P <0.0001) and weekends (rPearson = −0.197, P <0.0001), and time spent for socializing, relaxing, and leisure on weekends (rPearson = −0.152, P <0.0001). Short sleepers also spent more time engaged in education, personal care without sleep, household activities and, for very short sleepers, watching TV. Except for time spent watching TV, which increased with longer sleep times, all waking activities shown in Figure 2A decreased with increasing sleep time.
Figure 2.
A. Average change in weekday (Mon–Fri) waking activity time depending on sleep time category (N=23,325) based on multiple linear regression models adjusting for age, gender, ethnicity, educational attainment, income, presence of partner, and presence of children. The 7.5 h to <8.5 h sleep time category served as reference. Upper boundaries of 1 h sleep time ranges are shown on the abscissa, except for the lowest and highest category, which extend to minimum and maximum sleep time. For work time, separate models were run for the whole group (Work) and restricting data to those who worked on the interview day (Work > 0 min).B. Average change in weekend (Sat+Sun) waking activity time depending on sleep time category (N=23,563).
In Figure 2B, adjusted changes in waking activity time on weekends are shown with respect to sleep time for the 7 categories presented in Figure 2A. As with weekdays, work time was the waking activity predominantly exchanged for sleep time across all sleep time categories on weekends. The differences between weekday and weekend results were minor, except for 2 activities. Short sleepers spent less time watching TV than respondents with average sleep times on weekends in all sleep categories; and long sleepers spent less time in socializing, relaxing, and leisure activities than respondents with average sleep times.
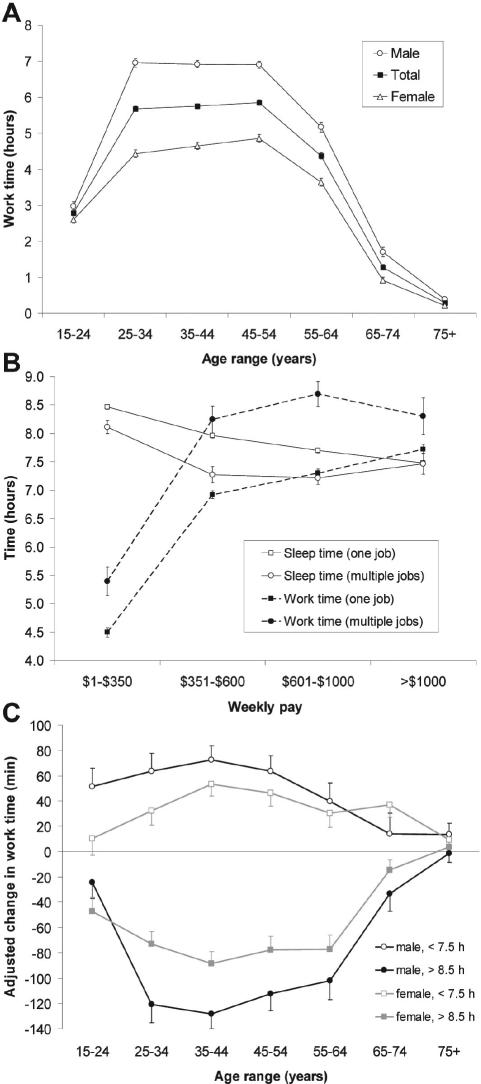
Figure 3A shows average hours of compensated work time of all respondents (regardless of whether they worked) on weekdays, as a function of age and gender. The relationship between age and work time has an inverse U-shape; average work time reached its maximum at age 45–54 y (5.86 ± 0.07 hours), decreased both with lower and higher age, and reached its minimum at age 75+ y. On average, men spent more time in compensated work than women in all age groups. The difference in work time of women and men reached its maximum of 2.5 h at 25–34 y and was markedly lower in 15 to 24-year-olds and people ≥55 y.
Figure 3.
A. Average weekday (Mon–Fri) work time depending on age range and gender (Nmale=10,137, Nfemale=13,188). Work time includes ATUS tier 05: All “working and work related activities” (see Appendix). Error bars represent standard errors calculated with the replicate variance method described in the ATUS User's Guide.20 B. Average sleep time and work time depending on quartile of weekly pay and multiple job status for weekdays (Mon–Fri). Of the 13,130 respondents with income, 9.3% reported work in multiple jobs. Error bars represent standard errors calculated with the replicate variance method described in the ATUS User's Guide.20 C. Average change in weekday (Mon–Fri) work time depending on age range and gender for below average (<7.5 h) and above average (> 8.5 h) sleepers (N=23,325) based on multiple linear regression models adjusting for age, gender, ethnicity, educational attainment, income, presence of partner, and presence of children. The 7.5 h to <8.5 h sleep time category served as reference. Error bars represent standard errors.
Figure 3B shows average sleep and work time on weekdays depending on income quartiles and multiple job status for those who reported to have income. 9.3% of respondents with income reported working in multiple jobs. Work time increased while sleep time decreased with increasing weekly pay. People working in multiple jobs worked longer and slept less to earn the same amount of money as people with one job. Both phenomena were observed across all salary categories. Respondents who reported to have no income slept 8.7 h on average, i.e., 19 min longer than respondents in the lowest income quartile and 75 min longer than respondents in the highest income quartile.
The results shown in Figures 2A and 2B were adjusted for age and gender. Obviously, the extent that waking activities are exchanged for sleep time depends both on age and gender. This is exemplified for work time on weekdays in Figure 3C. Here, the change in work time, adjusted for income, race, educational attainment, and presence of partner and children, is shown for shorter than average sleepers (<7.5 h) and longer than average sleepers (>8.5 h) depending on age group and gender. Women exchanged less compensated work time for sleep time across age groups than men. Work time was predominantly exchanged for sleep time between ages 25 and 64 y, and, as would be expected, almost negligibly in respondents ≥75 y.
DISCUSSION
Representative time use data collected on 47,731 respondents between 2003 and 2005 were used to investigate the relationship of sleep time and waking activities. Sleep time was shown to be shorter in men, especially between the age of 25 and 64 years. Sleep time reached its minimum at age 45–54 y, when compensated work time reached its maximum. Sleep time was maximal in the oldest age group, but it is unclear to what extent reported long sleep durations correspond to actual physiologic sleep.21 One recent study documented greater self-reported sleep durations compared to sleep durations determined by actigraphy, suggesting that there is at least some degree of error variance in the estimation of self-reported sleep duration.22
Even if restricted to nighttime sleep, average ATUS sleep times were longer than those reported in other population-based studies.3,23,24 If compared to the National Sleep Foundation's (NSF) 2005 Sleep in America poll,23 average ATUS nighttime sleep times exceeded average NSF sleep times by 0.9 h (+13.2%) on weekdays and by 1.2 h (+16%) on weekends. Given that the “sleep” category for ATUS included a wide range of terms that may not involve physiological sleep (e.g., falling asleep, dozing off, napping, getting up, waking up), it is certain that the ATUS sleep times are overestimates of actual physiological sleep obtained by respondents per 24 h. This may have contributed to the longer estimated sleep durations obtained in this study compared to other population-based studies.3,23,24 As explained above, both sleeplessness and daytime sleep were captured in addition to nighttime sleep with our definition of sleep time. It would have been possible to treat nighttime sleep, daytime sleep, and sleeplessness as 3 different outcome variables. However, it is unlikely that the relationships between sleep time and waking activities observed in our present analysis would have changed substantially. This applies especially to nighttime sleep, as nighttime sleep represented 93.5% of sleep time on weekdays and 93.3% of sleep time on weekends.
Sleep time on Saturdays and especially on Sundays was markedly higher than weekdays, especially in those <65 y (Figure 1B). This pattern is consistent with weekend sleep duration reflecting an opportunity to recover from weekday sleep restriction for those < 65 y. Respondents aged ≥65 years averaged the longest weekday sleep times, while those <35 y averaged the longest weekend sleep times (especially on Sunday). The former likely reflects retirement and the reduced competing demands on sleep time. The latter may reflect the ability of adolescents and young adults to extend sleep duration following a sleep debt. The marked increase in sleep duration on weekends relative to weekdays in those <65 y also suggests that the use of a single subjective estimate of sleep duration—as commonly used in epidemiological studies—may obscure the large differences found between sleep times on weekends versus weekdays in the ATUS database. The data also remind us that despite the likely importance of sleep timing to health25 and its demonstrated importance to cognitive alertness26 and safety,27,28 the United States still lacks population-based estimates of physiological sleep duration as a function of gender, ethnicity, age, compensated work schedules, domestic responsibilities, health-related behaviors, and health status. Moreover, since ATUS does not include medical information (even height and weight), it is not possible to evaluate how time used for sleep, work, and other activities relate to BMI and morbidity.
The proportion of people reporting sleeplessness (defined by terms that included “insomnia, tossing and turning, lying awake, counting sheep”), was found to be slightly higher in women (4.2%) than men (3.0%), and to increase with age (especially >64 y), which is consistent with other studies.29 Depending on the study and the definition prevalence estimates of insomnia vary widely between 5% and 50%.29,30 Therefore, the prevalence of sleeplessness in the ATUS databases is comparatively low. Most of this discrepancy may be attributed to the fact that estimates of insomnia are usually based on weekly or monthly estimates of insomnia symptoms, whereas ATUS only covers a 24-h period (i.e., a point estimate). Additionally, respondents were not specifically asked for symptoms of sleeplessness in ATUS, but rather, they had to bring up those symptoms themselves.
The primary focus of the study was to identify the relationships between sleep duration and all other waking activity categories in the ATUS database. Controlling for age, gender, educational attainment, race, income, and the presence of children and partners; time used for monetarily compensated work and work-related activities was consistently associated with sleep time, such that work time increased as sleep time decreased. This reciprocal relationship was apparent both when all respondents were included (regardless of whether they worked for compensation), and when the analysis was restricted only to those who worked for pay and slept on the day of the interview. The relationship was also evident on weekend days, and evident in the finding that the percentage of people who did not work on the interview day increased with increasing sleep time. These cross-sectional results in a nationally representative sample suggest that compensated work time is the most potent determinant of sleep time, in which case work time should be considered an important factor when evaluating the relationship between sleep time and morbidity and mortality.
The few time use studies examining sleeping and working are consistent with our findings. Hale31 used data of Time Use Studies performed in the United States in 1965, 1975, 1985, and 1999, and reported that people working more than 50 h/wk were more likely to be short sleepers (<6.5 h, OR = 1.45) and less likely to be long sleepers (> 8.5 h sleep, OR = 0.75) compared to people who worked <35 h a week. She also showed that retirement and having no job both increased the probability of sleeping longer than average on weekdays. Biddle and Hamermesh19 analyzed time use data sampled in 1519 U.S. households between 1975 and 1976. Their multivariable linear regression models, which did not allow for nonlinear relationships, suggested that each additional hour of work costs 7 to 10 min of sleep. They concluded that “[t]ime spent sleeping is inversely related to both the wage and time spent in the labor market. In short, sleep is subject to consumer choice and is affected by the same economic variables that affect choices about other uses of time.”
Our analyses of the 2003–2005 ATUS data—collected nearly 30 years after the Biddle and Hamermesh data19—confirm the preeminent reciprocal relationship between compensated work time and sleep time. Further support for economic factors influencing sleep time comes from Patel et al.14 who found that measures of low socioeconomic status, such as lack of employment or low household income, were strongly associated with long sleep. The magnitude of the confounding rate ratio was comparable to that found for depression,14 suggesting that low socioeconomic status might contribute to, or confound, the positive association between long sleep and mortality observed in previous studies.2
While work time was expected to have a negative relationship to sleep time, travel time (composed of work commute time and all other travel time) was an unexpected second-place factor reciprocally related to sleep time. Commute time accounted for 26.8% of travel time on weekdays in all respondents and for 44.7% of travel time in those who worked on the interview day. These data suggest avenues for further research, such as how sleep time may be squeezed by work commutes that are starting earlier in the morning (to work) and/or later in the day (to home), or commutes that are getting longer due to such factors as urban sprawl (i.e., people living further from work) or traffic volume growing faster than transport capacity. Our findings also highlight how little we know about how non-commute travel, such as to shop, to schools, to religious and social events, or long distance travel might be reducing sleep time.
Four other ATUS tier 1 categories were associated with sleep time, defined as activity time increased or decreased by 20 min or more in at least one of the sleep time categories compared to average sleepers on weekdays (see Figures 2A and 2B). Time spent for personal care showed a reciprocal relationship to sleep time that was less pronounced than either work time or travel time. The socializing, relaxing, and leisure time category was negatively related to sleep time, but this relationship was primarily evident for short sleepers (<7.5 h). Surprisingly, the subcategory watching TV was increased in both short and long sleepers on weekdays relative to the reference group (7.5 h to <8.5 h), although short sleepers watched less TV than reference sleepers on weekends. Watching TV was the only waking activity that increased in all long-sleeper categories. Only respondents sleeping >10.5 h spent significantly less time in household activities. Likewise, time spent for education was significantly lower for those sleeping ≥9.5 h. Consequently, long sleepers worked less, spent less time on education and household activities, and watched television more, suggesting a relatively sedentary life style.
Although some of the other 11 ATUS tier 1 categories also showed reciprocal associations with sleep time, they were much less pronounced. This may be partially due to the relative temporal infrequency or lower duration of time people devoted to these other activities. That is, more focused analyses on people who reported activities that were less frequent (e.g., caring for and helping household members; volunteer activities; consumer purchases; religious and spiritual activities), may reveal stronger reciprocal relationships between these activities and sleep time. However, these 11 other ATUS activity categories were inconsequential in the larger cohort compared to the 6 factors most associated with reduced sleep time (i.e., work time; travel time; socializing, relaxing, leisure time [including watching television]; personal care; household activities; and education).
The association between sleep time and morbidity and mortality often has a U-shape, i.e., morbidity and mortality increase in both short and long sleepers. Therefore, waking activities simultaneously increasing or simultaneously decreasing in short and long sleepers are candidates for confounding the association between sleep time and morbidity and mortality. Only 2 activities are both prevalent and show U-shaped relationships (see Table 3). First, time used for “eating and drinking” was lower in both short and long sleepers. If quick meals are associated with unhealthy diets, this may lead to higher morbidity and mortality. Second, watching TV increased in both short and long sleepers on weekdays. Watching TV was found to be associated with obesity,5 which is known to be associated with higher rates of morbidity and mortality.
U-shaped associations are not a prerequisite for a waking activity confounding the association of sleep time and morbidity and mortality. Similar to the association of poor health with other health-related factors (e.g., exercise, caloric intake), moderate amounts are optimal, whereas low or high levels can be harmful.21 Of course, short sleepers generally have more time to spend for other waking activities, but our analyses showed that it is predominantly exchanged for work time, travel time, and socializing, relaxing, and leisure. John et al.32 showed in a cross-sectional survey on 4075 subjects aged 18–64 that participants sleeping ≤5 h had significantly increased odds ratios for nicotine (OR 1.9) and alcohol (OR 2.6) dependence, depressive disorder (OR 3.0) and anxiety disorder (OR 2.1) compared to average sleepers (7–8 h). These factors were not available in the ATUS database.
Long sleepers were much more likely not to work, or, if they did, to work shorter hours than short sleepers. Most of the other activities were decreased in favor of sleep, except for watching TV. Here, long sleepers watched more TV than average sleepers. More sleep, more TV, and less work means that long sleepers might be at risk for interacting less with other people, which is consistent with the findings of Hartman et al,17 who showed that short sleepers were characterized as ambitious, active, energetic, slightly hypomanic, and saw sleep as an unfortunate obstacle in life's pursuit, whereas long sleepers were shy, introverted, anxious, mildly depressed, less energetic, and tended to use sleep as an escape from life's pressures.
Limitations
While attempts have been made to collect the most accurate data possible, the ATUS data do have limitations. With the exception of childcare, information on secondary activities (activities that are done at the same time as the primary activity) is not collected. This could lead to underestimates of the amount of time people spend doing activities that are frequently done in combination with other activities (e.g., listening to music). Additionally, survey estimates are subject to nonsampling errors, such as an inability to obtain information from all households in the sample, data entry errors, coding errors, and misinterpretation of definitions. Errors also could occur if nonresponse is correlated with time use. Nonsampling errors were not measured. However, the Census Bureau uses quality assurance procedures to minimize nonsampling data entry and coding errors in the survey estimates.
Weights provided by the Bureau of Labor Statistics and the Census Bureau were used to correct for oversampling of some demographic groups, oversampling of weekend days, and differing response rates across demographic groups and days of the week. Nevertheless, the overall response rate of 51.2% is relatively low, which may be partly explained by response fatigue, as ATUS respondents were drawn from households that completed their eighth and final month interviews for the CPS. The extent to which nonresponse influenced the representativeness of the sample is discussed in greater detail in Abraham et al.33
The cross-sectional nature of the data limits conclusions of causality. We cannot be certain that sleep time is reduced deliberately to increase work time or vice versa. It is possible that survey respondents were reporting sleep as a reflection of their biological sleep need, and that the increased time we observed for work, travel, and other activities was purely at their discretion (i.e., all waking activities are equally valued). We doubt this interpretation is correct because of the relatively few waking activities that were reciprocally related to sleep time across the full range of sleep times, and because there is ample evidence that people can and do engage in lifestyles that result in sleep restriction and its adverse consequences for neurobehavioral functions, safety, and health.
It was shown that the extent to which waking activities were exchanged for sleep time depended on age and gender. In spite of this, we chose not to incorporate any interaction terms between age, gender, or any of the other variables and sleep time in the regression models for 2 reasons. First, sleep time indicator variables would have lost their favorable interpretation of “change in activity time relative to respondents with average sleep time.” Second, because of the large sample size, which was not based on sample size calculations but rather on the available data, many of the interactions would have been found significant without being relevant. To elaborate the complex interactions between sleep time and other factors confounding the relationship between sleep and waking activities will be an important task for future in depth analyses that would have gone beyond the scope of this publication.
Conclusions
Our analyses suggest that time spent working is the primary candidate for a waking activity confounding the relationship between short and long sleep durations and morbidity and mortality. Astonishingly, none of the 18 epidemiological studies investigating this association considered adjusting for hours worked, although some adjusted for occupational status.2 In studies gathering sleep time data, it would not be difficult to gather data on usual hours on the job at the same time. In future sleep studies, work time should be considered as a potential confounder, as it was shown to be associated with sleep time and was shown to be associated with mental and physical health as well.15 This suggestion is consistent with the suggestion by Tamakoshi et al.24 who speculated that work related social factors may be confounding the association of sleep time and health, as the increased mortality risk associated with short sleep times disappeared in their study in men but not in women after covariate adjustment. Considerably more research is required to identify how these and other factors influence sleep timing, duration, and quality. It is especially important to determine at what point the exchanges people make between sleep time and time for other activities can result in adverse consequences for health and safety.
ACKNOWLEDGMENTS
Supported by NIH grant NR-04281, by the National Space Biomedical Research Institute through NASA cooperative agreement NCC 9–58 and by the Institute for Experimental Psychiatry Research Foundation.
APPENDIX
ATUS coding for the first (underlined) and the second tier are replicated here. Codes were taken from the 2003 ATUS Activity Lexicon. There were some minor and even a few major coding changes in the 2004 and 2005 surveys. Information about differences in coding and the coding manuals themselves can be obtained online at www.bls.gov/tus/lexicons.htm.
-
01 Personal Care
01 Sleeping; 02 Grooming; 03 Health-related Self Care; 04 Personal Activities; 05 Personal Care Emergencies; 99 Personal Care not elsewhere classified (n.e.c.)
-
02 Household Activities
01 Housework; 02 Food and Drink Preparation, Presentation, and Clean-up; 03 Interior Maintenance, Repair, and Decoration; 04 Exterior Maintenance, Repair, and Decoration; 05 Lawn, Garden, and Houseplants; 06 Animals and Pets; 07 Vehicles; 08 Appliances and Tools; 09 Household Management; 99 Household Activities n.e.c.
-
03 Caring For and Helping Household Members
01 Caring For and Helping Household Children; 02 Activities Related to household Children's Education; 03 Activities Related to household Children's Health; 04 Caring For Household Adults; 05 Helping Household Adults; 99 Caring For and Helping household Members n.e.c.
-
04 Caring For and Helping Non-household Members
01 Caring For and Helping Non-household Children; 02 Activities Related to Non-household Children's Education; 03 Activities Related to Non-household Children's Health; 04 Caring for Non-household Adults; 05 Helping Non-household Adults; 99 Caring For and Helping Non-household Members n.e.c.
-
05 Working and Work-Related Activities
01 Working; 02 Work-Related Activities; 03 Other Income-generating Activities; 04 Job Search and Interviewing; 99 Work and Work-Related Activities n.e.c.
-
06 Education
01 Taking Class; 02 Extracurricular School Activities—Except Sports; 03 Research/Homework; 04 Registration/Administrative activities; 99 Education n.e.c.
-
07 Consumer Purchases
01 Shopping—Store, Telephone, Internet; 02 Researching Purchases; 03 Security Procedures Related to Consumer Purchases; 99 Consumer Purchases n.e.c.
-
08 Professional and Personal Care Services
01 Childcare Services; 02 Financial Services and Banking; 03 Legal Services; 04 Medical and Care Services; 05 Personal Care Services; 06 Real Estate; 07 Veterinary Services; 08 Security Procedures Related to Professional/Personal Services; 99 Professional and Personal Services n.e.c.
-
09 Household Services
01 Household Services (not done by self); 02 Home Maintenance, Repair, Decoration, and Construction (not done by self); 03 Pet Services (not done by self, not vet); 04 Lawn and Garden Services (not done by self); 05 Vehicle Maintenance and Repair Services (not done by self); 99 Household Services n.e.c.
-
10 Government Services and Civic Obligations
01 Using Government Services; 02 Civic Obligations and Participation; 03 Waiting Associated with Government Services or Civic Obligations; 04 Security Procedures Related to Government Services/Civic Obligations; 99 Government Services n.e.c.
-
11 Eating and Drinking
01 Eating and Drinking; 99 Eating and Drinking n.e.c.
-
12 Socializing, Relaxing, and Leisure
01 Socializing and Communicating; 02 Attending or Hosting Social Events; 03 Relaxing and Leisure; 04 Arts and Entertainment other than sports; 05 Waiting Associated with Socializing, Relaxing, and Leisure; 99 Socializing, Relaxing, and Leisure n.e.c.
-
13 Sports, Exercise, and Recreation
01 Participating in Sports, Exercise, or Recreation; 02 Attending Sporting/Recreational Events; 03 Waiting Associated with Sports, Exercise, and Recreation; 04 Security Procedures Related to Sports, Exercise, and Recreation; 99 Sports, Exercise, and Recreation n.e.c.
-
14 Religious and Spiritual Activities
01 Religious/Spiritual Practices; 99 Religious and Spiritual Activities n.e.c.
-
15 Volunteer Activities
01 Administrative and Support Activities; 02 Social Service and Care Activities (Except Medical); 03 Indoor and Outdoor Maintenance, Building, and Clean-up Activities; 04 Participating in Performance and Cultural Activities; 05 Attending Meetings, Conferences, and Training; 06 Public Health and Safety Activities; 99 Volunteer Activities n.e.c.
-
16 Telephone Calls
01 Telephone Calls; 99 Telephone Calls n.e.c.
-
17 Traveling
01 Travel Related to Personal Care; 02 Travel Related to Household Activities; 03 Travel Related to Caring For and Helping household Members; 04 Travel Related to Caring For and Helping Non-household Members; 05 Travel Related to Work; 06 Travel Related to Education; 07 Travel Related to Consumer Purchases; 08 Travel Related to Using Professional and Personal Care Services; 09 Travel Related to Using Household Services; 10 Travel Related to Using Government Services and Civic Obligations; 11 Travel Related to Eating and Drinking; 12 Travel Related to Socializing, Relaxing, and Leisure; 13 Travel Related to Sports, Exercise, and Recreation; 14 Travel Related to Religious/Spiritual Activities; 15 Travel Related to Volunteer Activities; 16 Travel Related to Telephone Calls; 17 Security Procedures Related to Traveling; 99 Traveling n.e.c.
Footnotes
Disclosure Statement
This was not an industry supported study. Dr. Rosa is an employee of a granting agency – National Institute for Occupational Safety and Health. Dr. Dinges has received research support from Cephalon; has participated in speaking engagements for Cephalon and Jazz; and has consulted for Cephalon, Merck, Novartis, Pfizer, GlaxoSmithKline, Mars Masterfoods, and Proctor & Gamble. Dr. Basner, Dr. Banks, Mr. Fomberstein, Mr. Razavi, and Mr. William have indicated no financial conflicts of interest.
REFERENCES
- 1.Hammond EC. Am J Public Health Nations Health. 1964. Some preliminary findings on physical complaints from a prospective study of 1,064,004 men and women; pp. 11–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simpson NS, Punjabi NM, Dinges DF. Sleep and mortality. In: Chokroverty SM, Montagna P, editors. Handbook of clinical neurology. Elsevier; (in press) [Google Scholar]
- 3.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;2:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 4.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;3:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vioque J, Torres A, Quiles J. Time spent watching television, sleep duration and obesity in adults living in Valencia, Spain. Int J Obes Relat Metab Disord. 2000;12:1683–8. doi: 10.1038/sj.ijo.0801434. [DOI] [PubMed] [Google Scholar]
- 6.Hasler G, Buysse DJ, Klaghofer R, et al. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep. 2004;4:661–6. doi: 10.1093/sleep/27.4.661. [DOI] [PubMed] [Google Scholar]
- 7.Vorona RD, Winn MP, Babineau TW, Eng BP, Feldman HR, Ware JC. Overweight and obese patients in a primary care population report less sleep than patients with a normal body mass index. Arch Intern Med. 2005;1:25–30. doi: 10.1001/archinte.165.1.25. [DOI] [PubMed] [Google Scholar]
- 8.Steptoe A, Peacey V, Wardle J. Sleep duration and health in young adults. Arch Intern Med. 2006;16:1689–92. doi: 10.1001/archinte.166.16.1689. [DOI] [PubMed] [Google Scholar]
- 9.Gottlieb DJ, Redline S, Nieto FJ, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006;8:1009–14. doi: 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- 10.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;5:833–9. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- 11.Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;2:205–9. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 12.Gottlieb DJ, Punjabi NM, Newman AB, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;8:863–7. doi: 10.1001/archinte.165.8.863. [DOI] [PubMed] [Google Scholar]
- 13.Yaggi HK, Araujo AB, McKinlay JB. Sleep duration as a risk factor for the development of type 2 diabetes. Diabetes Care. 2006;3:657–61. doi: 10.2337/diacare.29.03.06.dc05-0879. [DOI] [PubMed] [Google Scholar]
- 14.Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep. 2006;7:881–9. doi: 10.1093/sleep/29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moore PJ, Adler NE, Williams DR, Jackson JS. Socioeconomic status and health: the role of sleep. Psychosom Med. 2002;2:337–44. doi: 10.1097/00006842-200203000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Breslow L, Enstrom JE. Persistence of health habits and their relationship to mortality. Prev Med. 1980;4:469–83. doi: 10.1016/0091-7435(80)90042-0. [DOI] [PubMed] [Google Scholar]
- 17.Hartmann E, Baekeland F, Zwilling GR. Psychological differences between long and short sleepers. Arch Gen Psychiatry. 1972;5:463–68. doi: 10.1001/archpsyc.1972.01750230073014. [DOI] [PubMed] [Google Scholar]
- 18.Foster RG, Wulff K. The rhythm of rest and excess. Nat Rev Neurosci. 2005;5:407–14. doi: 10.1038/nrn1670. [DOI] [PubMed] [Google Scholar]
- 19.Biddle JE, Hamermesh DS. Sleep and the allocation of time. J Political Econ. 1990;5(Pt. 1):922–43. [Google Scholar]
- 20.U.S. Bureau of Labor Statistics and U.S. Census Bureau. American Time Use Survey User's Guide - Understanding ATUS 2003, 2004, and 2005. 2007 Accessed through http://www.bls.gov/tus/atususersguide.pdf on 03/13/2007).
- 21.Youngstedt SD, Kripke DF. Long sleep and mortality: rationale for sleep restriction. Sleep Med Rev. 2004;3:159–74. doi: 10.1016/j.smrv.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 22.Lauderdale DS, Knutson KL, Yan LL, et al. Objectively measured sleep characteristics among early-middle-aged adults: The CARDIA Study. Am J Epidemiol. 2006;1:5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 23.National Sleep Foundation. 2005 Sleep in America Poll. Washington D.C: 2005. Accessed through www.sleepfoundation.org on 03/28/2007. [Google Scholar]
- 24.Tamakoshi A, Ohno Y. Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep. 2004;1:51–54. [PubMed] [Google Scholar]
- 25.Comittee on Sleep Medicine and Research. Washington, DC: The National Academic Press; 2006. Sleep disorders and sleep deprivation: an unmet public health problem. [PubMed] [Google Scholar]
- 26.Durmer JS, Dinges DF. Neurocognitive consequences of sleep deprivation. Semin Neurol. 2005;1:117–29. doi: 10.1055/s-2005-867080. [DOI] [PubMed] [Google Scholar]
- 27.Dinges DF. An overview of sleepiness and accidents. J Sleep Res. 1995;S2:4–14. doi: 10.1111/j.1365-2869.1995.tb00220.x. [DOI] [PubMed] [Google Scholar]
- 28.Walsh JW, Dement C, Dinges DF. Sleep medicine, public policy and health. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. Philadelphia, PA: W.B. Saunders; 2005. pp. 648–56. [Google Scholar]
- 29.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;2:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 30.Becker PM. Insomnia: prevalence, impact, pathogenesis, differential diagnosis, and evaluation. Psychiatr Clin North Am. 2006;4:855–70. doi: 10.1016/j.psc.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 31.Hale L. Who has time to sleep? J Public Health (Oxf) 2005;2:205–11. doi: 10.1093/pubmed/fdi004. [DOI] [PubMed] [Google Scholar]
- 32.John U, Meyer C, Rumpf HJ, Hapke U. Relationships of psychiatric disorders with sleep duration in an adult general population sample. J Psychiatr Res. 2005;6:577–83. doi: 10.1016/j.jpsychires.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 33.Abraham K, Maitland A, Bianchi SM. Nonresponse in the American Time Use Survey. Public Opinion Quarterly. 2006;5:676–703. [Google Scholar]