Abstract
Objective: To critically review evidence for the effectiveness of eccentric exercise to treat lower extremity tendinoses.
Data Sources: Databases used to locate randomized controlled trials (RCTs) included PubMed (1980–2006), CINAHL (1982–2006), Web of Science (1995–2006), SPORT Discus (1980–2006), Physiotherapy Evidence Database (PEDro), and the Cochrane Collaboration Database. Key words included tendon, tendonitis, tendinosis, tendinopathy, exercise, eccentric, rehabilitation, and therapy.
Study Selection: The criteria for trial selection were (1) the literature was written in English, (2) the research design was an RCT, (3) the study participants were adults with a clinical diagnosis of tendinosis, (4) the outcome measures included pain or strength, and (5) eccentric exercise was used to treat lower extremity tendinosis.
Data Extraction: Specific data were abstracted from the RCTs, including eccentric exercise protocol, adjunctive treatments, concurrent physical activity, and treatment outcome.
Data Synthesis: The calculated post hoc statistical power of the selected studies (n = 11) was low, and the average methodologic score was 5.3/10 based on PEDro criteria. Eccentric exercise was compared with no treatment (n = 1), concentric exercise (n = 5), an alternative eccentric exercise protocol (n = 1), stretching (n = 2), night splinting (n = 1), and physical agents (n = 1). In most trials, tendinosis-related pain was reduced with eccentric exercise over time, but only in 3 studies did eccentric exercise decrease pain relative to the control treatment. Similarly, the RCTs demonstrated that strength-related measures improved over time, but none revealed significant differences relative to the control treatment. Based on the best evidence available, it appears that eccentric exercise may reduce pain and improve strength in lower extremity tendinoses, but whether eccentric exercise is more effective than other forms of therapeutic exercise for the resolution of tendinosis symptoms remains questionable.
Keywords: rehabilitation, Achilles tendon, patellar tendon, tendon
Key Points
Eccentric exercise is likely a useful treatment for lower extremity tendinosis, but whether it is more or less effective than other forms of therapeutic exercise is unclear.
Eccentric exercise may be more effective in treating lower extremity tendinosis than splinting or some physical agents, but it may need to be combined with a prolonged period of rest from stressful activities for the best outcome.
Future investigators should recruit sufficient numbers of subjects and use valid, reliable, and patient-oriented outcome measures to evaluate the role of eccentric exercise in treating lower extremity tendinoses.
Prolonged musculoskeletal stresses are necessary for the development of symptomatic tendinosis 1; as a result, certified athletic trainers are likely to see these disorders frequently. In 2003, the Bureau of Labor Statistics reported more than 11 000 cases of chronic tendon injury that resulted in days away from work in the United States. 2 Sporting activities may impose even greater stresses on tendons than occupational activities. The prevalence of Achilles tendinosis has been estimated to be between 11% and 24% in runners, 3, 4 whereas the prevalence rates for patellar tendinosis in basketball and volleyball players have been recorded as high as 32% and 45%, respectively. 5 These estimates clearly indicate that tendinosis is a very common problem.
Lower extremity tendinoses have proven difficult to manage. Symptomatic Achilles and patellar tendinoses may preclude participation in physical activity, 6 prematurely terminate athletic careers, 7 and structurally weaken the tendon to the point of rupture. 8 Approximately 25% to 33% of athletes with lower extremity tendinoses demonstrate poor outcomes with conservative therapy, necessitating surgery. 6, 9 Of the surgical candidates, only 46% to 64% are able to successfully return to sports after a recovery period of 6 to 12 months. 6, 10, 11 Although the intensity of symptoms associated with tendinosis is greatest during periods of overuse, symptoms persist long after the end of an athletic career. 7
The foundation of conservative management for lower extremity tendinoses has traditionally included cessation or reduction of the offending activity, therapeutic modalities, nonsteroidal anti-inflammatory medication, and corticosteroid injections. 12 Unfortunately, the effectiveness of these treatment modes is limited because they primarily focus on decreasing inflammation, 12 which is absent in tendinosis. 13 Limited clinical effectiveness has forced clinicians to look to alternate means of treatment, such as eccentric exercise.
During the 1980s, Curwin and Stanish, 14 Fyfe and Stanish, 15 and Stanish et al 16 published several reports documenting their use of progressive eccentric exercise as part of a program to reduce the symptoms associated with tendinosis. Although this treatment method has existed for 2 decades, research studying the effectiveness of this intervention has been scant until recently.
The purposes of this manuscript are to (1) identify randomized controlled trials (RCTs) investigating the effect of eccentric exercise on lower extremity tendinosis, (2) present the treatments used with these exercise protocols, (3) describe the supplemental forms of treatment used in combination with eccentric exercise protocols in the treatment of tendinosis, (4) evaluate the strength of evidence supporting the use of eccentric exercise to treat tendinosis, and (5) make recommendations for future research.
METHODS
Data Sources
We performed a literature search using PubMed (1980– 2006), CINAHL (1982–2006), Web of Science (1995–2006), SPORT Discus (1980–2006), Physiotherapy Evidence Database (PEDro), and the Cochrane Collaboration Database to gather information relating to the treatment of tendinosis with eccentric exercise. The search terms included tendon, tendonitis, tendinosis, tendinopathy, exercise, eccentric, rehabilitation, and therapy.
Study Selection
The criteria for trial selection were (1) the literature was written in English, (2) the research design was an RCT, (3) the study participants were adults with a clinical diagnosis of tendinosis, (4) the outcome measures included pain or strength, and (5) eccentric exercise was used to treat lower extremity tendinosis. Using the aforementioned inclusion criteria, we filtered the retrieved citations from each database for relevance by reading only the title and abstract. Only if it could be clearly determined from the title and abstract that the study did not meet the criteria was it excluded. All other studies were obtained in full text to determine the appropriateness for inclusion in this systematic review.
We independently examined the trials and listed all of the studies that met the criteria for inclusion. If there were inconsistencies in the lists, a re-examination of each trial in question was warranted. Our consensus determined the final decision for study inclusion or exclusion.
Quality Assessment
The PEDro criteria were used to rate the trials for quality. Content validity of the PEDro criteria was developed by a consensus of experts in the area of methodologic quality. 17 The scored portion of the PEDro scale assesses 8 items pertaining to internal validity and 2 items added to ensure that the statistical results would be interpretable to the reader. 18 For each item on the PEDro scale, a yes or no response was obtained. A yes response earned 1 point, whereas a no received zero points, for a possible cumulative score of 10 points. The closer the score was to 10, the better the quality of the study. The cumulative PEDro score demonstrates high intertester reliability (intraclass correlation = .91), with κ scores for individual items ranging from .45 to 1.00. 19 Methodologic quality of each trial was independently assessed by each of us, and a consensus decision was later used to resolve any differences in PEDro scores.
Data Extraction
We independently extracted and recorded data from the RCTs on a data extraction form. Specific data extracted included pain and strength outcomes; characteristics of the treatments that were performed concomitant with the eccentric exercise; the amount of physical activity allowed during the rehabilitation period; and the variables in the eccentric exercise protocol, such as sets, repetitions, load, velocity of movement, equipment used, how the load was returned to the starting position, and frequency of treatments. Other information obtained included the anatomic location and length of symptoms. Group sizes, group means, and SDs of continuous data and frequencies of dichotomous data were extracted when feasible. Effect size (Hedges g) with a 95% confidence interval 20 and post hoc power 21 were calculated for continuous data. Relative risk and 95% confidence intervals were calculated for dichotomous data. 22 We then compared the independently extracted data for consistency and reached a consensus for any discrepancies in the data.
RESULTS
The database search identified 879 citations specific to the search terms used. After screening the citations by title and abstract, 27 trials remained that used eccentric exercise to treat tendinosis. Each of the 27 trials was obtained in full text and examined for inclusion. After full-text review, several more trials were excluded based on the following criteria: not written in English (n = 1), groups not randomly assigned (n = 3), lacking a control group of participants with the same injury (n = 9), no assessment of appropriate outcomes (n = 2), and tendinosis not located in the lower extremity (n = 1). Ultimately, 11 RCTs met the criteria for inclusion in this systematic review. The selection process is reflected in the Quality of Reporting of Meta-Analyses (QUOROM) 23 flow diagram in the Figure.
Quality of Reporting of Meta-Analyses (QUORUM) flow diagram demonstrating trial selection. 23 .
Study Quality
The mean PEDro score for the 11 studies was 5.3/10, with a range from 4 to 7. Overall, these scores are relatively good, considering that the intervention of eccentric exercise does not allow for blinding of the subject or therapist. Thus, the highest achievable score was 8/10.
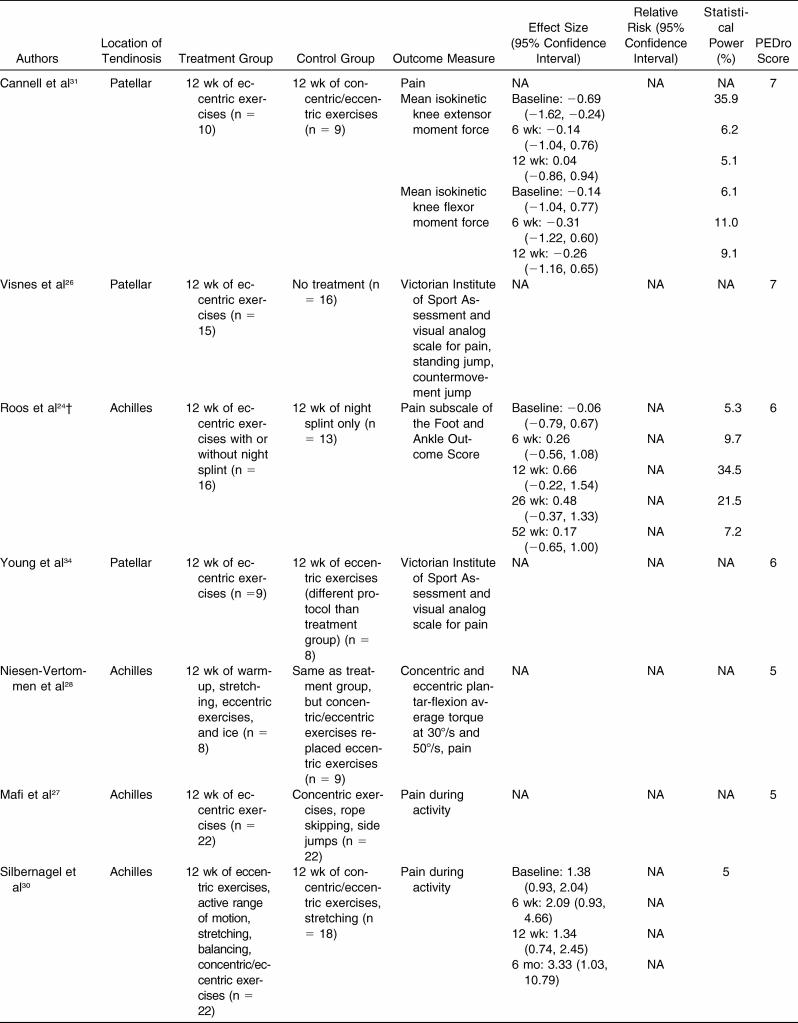
A methodologic factor that is not assessed by the PEDro scale, statistical power, is of particular importance in this review. Authors of only 3 studies 24–26 conducted an a priori power analysis, and only 1 group 26 achieved a sufficient final sample size to adequately ensure a priori power to detect differences in their outcome measures. However, the number of participants needed for sufficient statistical power (15 per group) in this study was based on an unusually large effect size (1.14). 26 Because most of the selected studies were underpowered (<80%), it is advisable to refer to Table 1, which presents effect size and relative risk for all of the available between-groups comparisons for continuous and dichotomous data, respectively.
Table 1. Efficacy of Eccentric Exercise for Tendinosis*.
Data Synthesis
The 11 selected studies included a total of 289 participants with clinical diagnoses of Achilles (n = 165) 24, 27–30 or patellar tendinosis (n =124). 25, 26, 31–34 The average number of participants in each trial was 26.3 (range = 12–44, eccentric group mean = 13.3, control group mean = 11.5), and the mean duration of symptoms at baseline ranged from 3.1 to 79 months. Pain was measured in all studies; however, strength outcomes were assessed in only 5 of 11 trials.
Eccentric Exercise Treatments
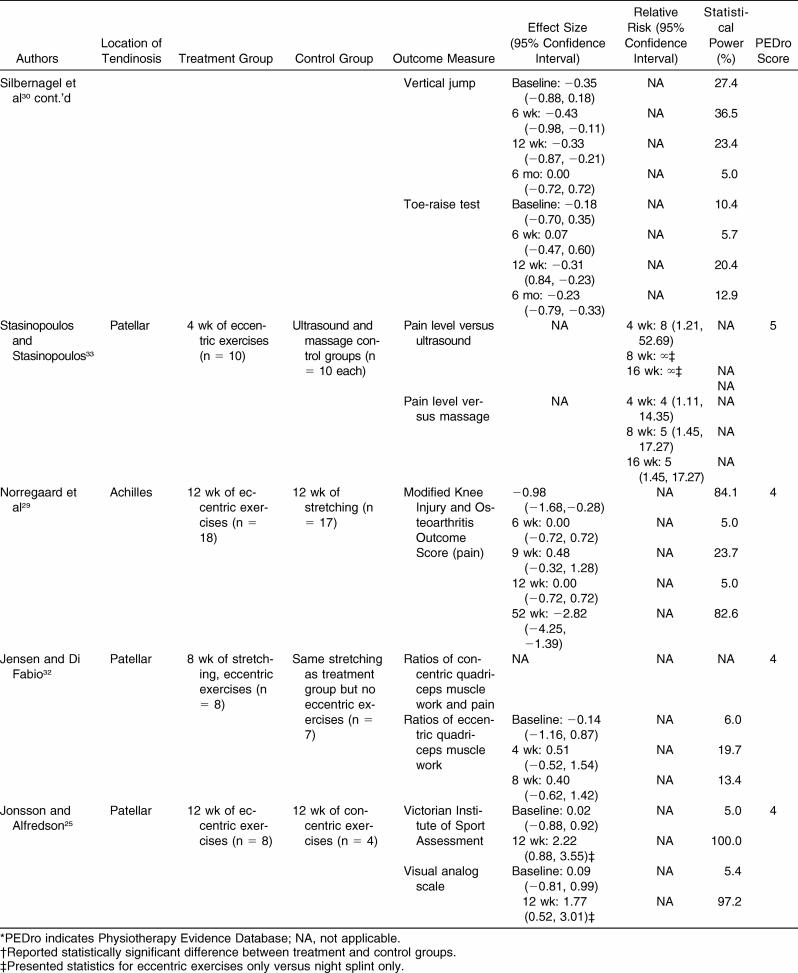
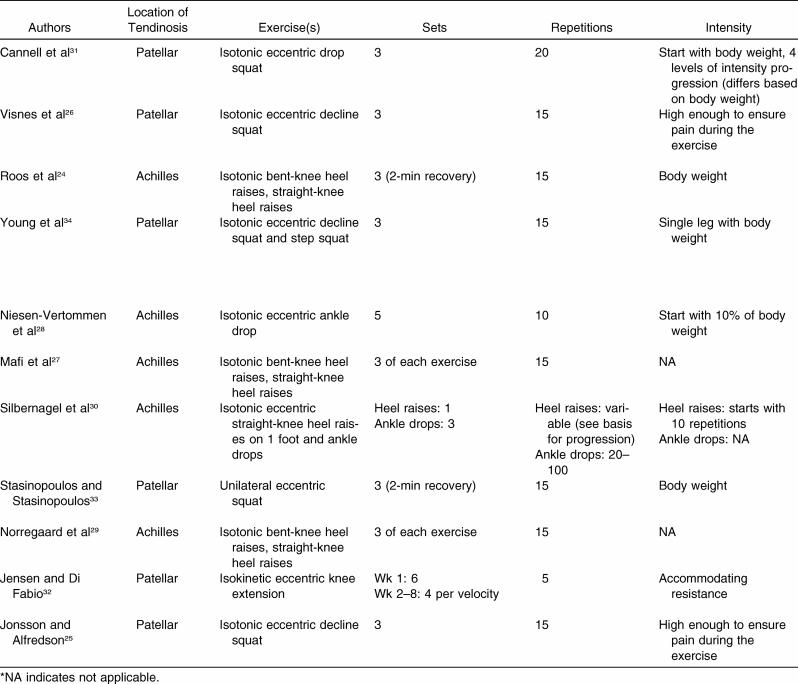
Therapeutic exercise protocols may be manipulated to maximize the effectiveness of the treatment. Table 2 lists the treatment variables used by authors treating Achilles and patellar tendinosis. The most common treatment protocols among the studies were established by Alfredson et al, 35 which consisted of 3 sets of 15 repetitions performed twice daily. Authors of most other RCTs did not deviate far from these protocols. 28, 30–32 However, the number of sets and repetitions per exercise ranged upward to 12 sets 32 and 100 repetitions. 30
Table 2. Eccentric Exercise Protocols for Tendinosis*.
Table 2. Extended*.
Eccentric exercise factors that were more inconsistent among studies included the velocity of the movement, pain ratings during exercise, and basis for progressive overload. Six exercise protocols indicated a controlled, unspecified velocity during the exercise 24, 25, 27–31; 3 involved a slow, constant velocity 26, 33, 34; and 2 progressively increased the velocity of exercise throughout the session. 32, 34 Two eccentric exercise protocols disallowed pain during rehabilitation, 28, 34 but in 8 exercise protocols, moderate pain was allowed or encouraged during exercise. 24–27, 29–31, 33, 34 The basis for progressive overload was determined by lack of pain, 24–29, 33, 34 ease of the exercise, 31 or time since initiation of the rehabilitation program. 30, 32 Progressive overload occurred by increasing the velocity of the exercise, 32 load, 24–29, 31, 33, 34 a combination of velocity and load, 34 or the cumulative addition of repetitions to the exercise protocol. 30
Another important consideration during eccentric exercise is how the load returns to the starting position after a repetition. Seven exercise protocols passively returned the load to the original position, 24–27, 29, 33, 34 whereas 4 used some degree of concentric muscle action to return the load to the starting position. 28, 30, 31, 34
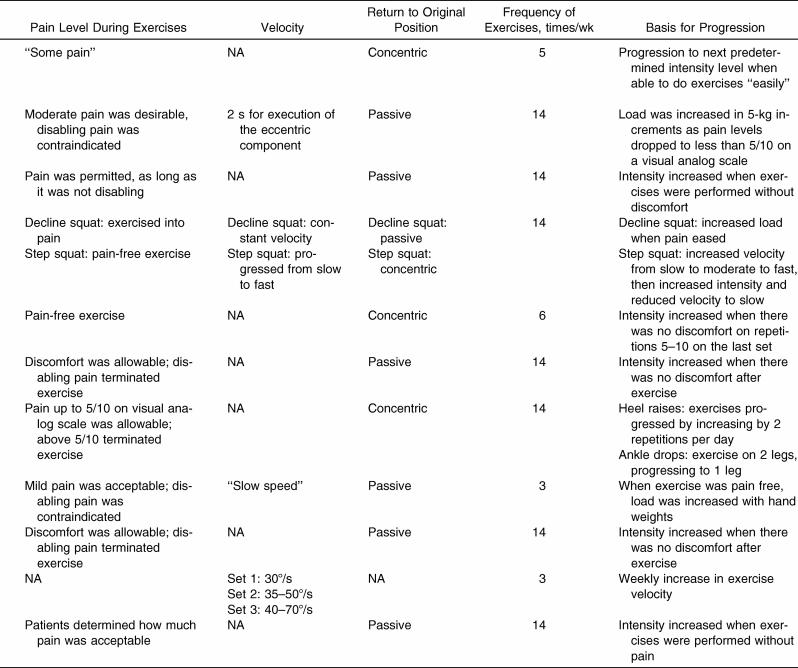
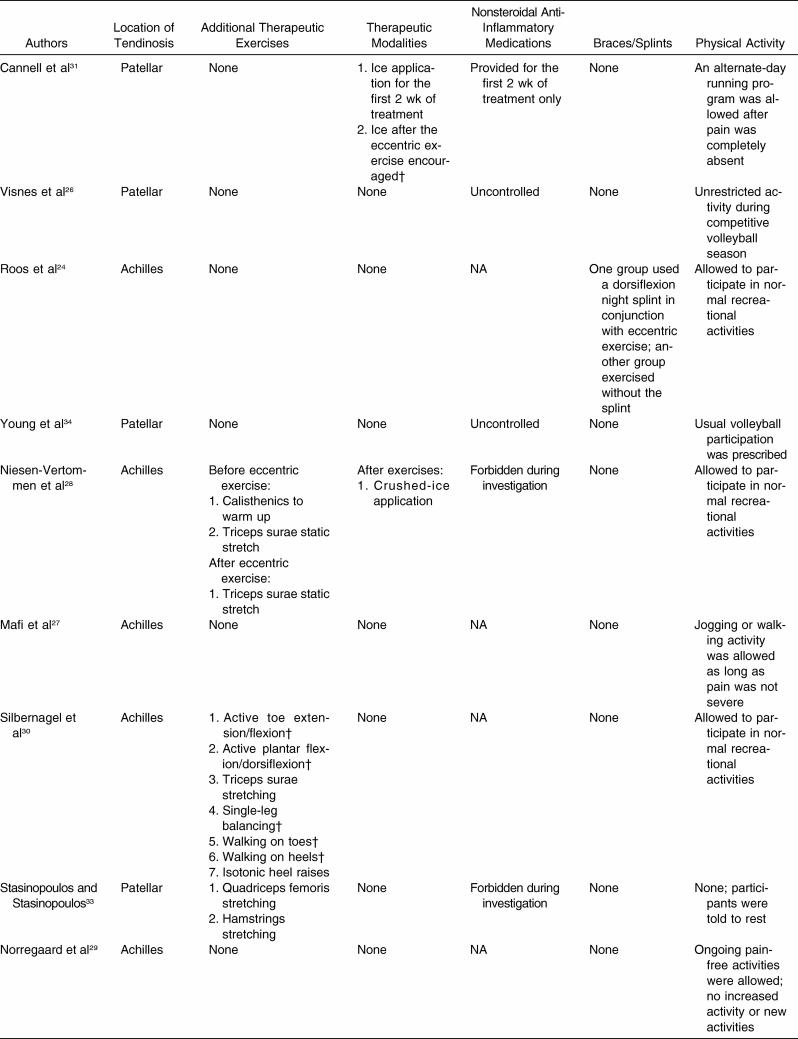
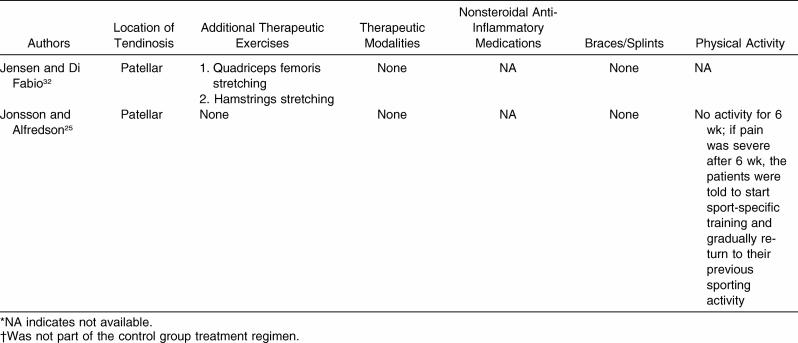
Concomitant Treatments and Physical Activity
Treatments supplemental to eccentric exercise ( Table 3) may or may not contribute to improved outcomes. Authors of 7 of the 11 selected studies used eccentric exercise exclusively as a form of therapeutic exercise to treat tendinosis. 24–27, 29, 31, 34 The remaining trials used other therapeutic exercises in conjunction with eccentric exercise, including active warm-up, 28 stretching, 28, 30, 32, 33 active motion, 30 isotonic concentric/eccentric exercises, 30 and balancing exercises. 30 Two groups 28, 31 requested that participants ice the symptomatic tendon after eccentric exercise. Additionally, 1 group 24 used night splints during the treatment period. The role of anti-inflammatory medication in these studies is unclear, because only 5 of the 11 groups accounted for medication or “other” forms of treatment. 26, 28, 31, 33, 34 Only 2 groups prohibited the use of nonsteroidal anti-inflammatory medication during the investigation. 28, 33
Table 3. Adjunctive Treatments Concurrent With Eccentric Exercise in Randomized Clinical Trials for Tendinosis*.
Table 3. Continued.
Maintaining high activity levels while symptomatic may affect the outcome of tendinosis. Authors of 7 of the 11 studies 24, 26–28, 30, 31, 34 allowed the participants to engage in normal physical activity, 1 group 29 allowed ongoing pain-free activities without starting new activities or increasing the quantity of training, 1 group 33 mandated rest, 1 group 25 allowed a progressive return to activity if no pain occurred after 6 weeks of rest, and another group 32 did not report the activity status.
Adjunctive treatments and the amount of physical activity allowed in each trial were consistent between the treatment and control groups, with few exceptions. One exception was found in the RCT by Cannell et al, 31 in which ice was applied to only the knees in the eccentric exercise group. Another exception was identified in the study by Silbernagel et al, 30 in which several noneccentric therapeutic exercises were performed only by the eccentric exercise group. These treatments may have confounded each of the trials by making it unclear if any treatment effect was due to eccentric exercise or the adjunctive treatment.
Effectiveness of Eccentric Exercise
Eccentric Exercise Versus No Treatment
Currently, no authors have compared eccentric exercise with either a no-treatment or placebo-controlled group for Achilles tendinosis. Visnes et al, 26 however, examined the effect of eccentric exercise on patellar tendinosis against an untreated control group. Both groups consisted of elite volleyball players assessed during the competitive season. The treatment group performed eccentric exercise for a total of 12 weeks, without any apparent benefit over the untreated group for pain (Victorian Institute of Sport Assessment [VISA] scores and global knee function score) or strength (standing jump height and countermovement jump height). The methodologic quality of this study was 6/10, which was above the average of the selected studies.
Eccentric Exercise Versus Concentric Exercise
Authors of 3 RCTs compared eccentric and concentric exercise for the treatment of Achilles tendinosis, whereas another 2 groups investigated these interventions on patellar tendinosis. Niesen-Vertommen et al 28 compared concentric and eccentric exercise for the treatment of Achilles tendinosis symptoms. Eccentric ankle drop and standard isometric plantar-flexion exercises were used for each of the treatment groups. Pain and ankle torque were assessed before, during, and after the 12-week intervention program. Pain and ankle torque were not different between the experimental conditions during any of the follow-up periods. However, when the authors analyzed pain levels in the eccentric and concentric groups averaged across all 4 evaluation times, the eccentric exercise group exhibited significantly less pain. Nonetheless, the authors suggested that the trends for decreasing pain were similar between the eccentric and concentric exercise groups because no interaction effects existed between the groups over time. The methodologic score of this study was 5/10, or approximately the average of the selected studies.
Silbernagel et al 30 also compared concentric and eccentric exercise in patients with Achilles tendinosis. Comparisons between groups yielded no significant effects for pain or strength (vertical jump test), with 1 exception. During a 6-week follow-up of a 12-week rehabilitation protocol, the concentric exercise group had significantly higher vertical jump scores. This trial was of average quality, based on a 5/10 PEDro score, and had a relatively large sample size of 44 tendons in the 2 groups.
Mafi et al 27 studied eccentric and concentric exercise for the treatment of Achilles tendinosis. The outcome measures evaluated were pain during physical activity and patient satisfaction. No measure of strength was recorded. Despite no apparent differences in pain levels between the treatment groups, the authors stated that eccentric exercise was superior to concentric training based on a greater percentage of participants in the eccentric exercise group indicating that they were satisfied. Because it was unclear how patient satisfaction was measured in the study and this variable was not a primary outcome of interest for this review, we did not include this measure as a positive outcome. The PEDro score for this study was 5/10, which is near the average methodologic score.
Cannell et al 31 compared eccentric drop squats and concentric knee flexion and extension exercises for the treatment of patellar tendinosis. The outcome measures assessed included pain and average knee extensor and flexor torque. Ten participants were analyzed in the eccentric exercise group and 9 in the concentric exercise group. No significant differences were noted between groups for the outcome measures. The methodology of this study was better than for any of the other included studies, scoring 7/10 on the PEDro scale.
In contrast, Jonsson and Alfredson 25 demonstrated a large treatment effect for eccentric exercise relative to concentric exercise for patellar tendinosis. Strength was not assessed as an outcome measure in this study. In spite of the positive outcome, the trial could be considered a relatively weak source of evidence, considering that the PEDro score was 4/10 and the concentric exercise group consisted of only 5 tendons. 25 Three patients (4 tendons) in the concentric exercise group dropped out before completing the exercise program because of poor progress. This prompted the authors to terminate the study because of “ethical reasons.” 25 In all, data from 8 participants in the eccentric exercise group and 4 participants in the concentric exercise group were analyzed.
Eccentric Exercise Versus Alternative Eccentric Exercise Protocol
To date, no authors have published studies comparing various eccentric exercise protocols for changes in pain or strength in participants with Achilles tendinosis.
One group 34 investigated 2 eccentric exercise protocols to determine if one protocol is advantageous for patellar tendinosis. The protocols differed by exercise (unilateral decline squats versus unilateral step squats), loading (eccentric only versus concentric and eccentric), pain (exercising short of pain versus into pain), and progression (load only versus load and velocity). No statistical differences were seen in the VISA or a visual analog scale for pain between treatment protocols. Despite the lack of effect between the treatment groups, both protocols significantly reduced pain and improved outcome at 12-week and 12-month follow-up relative to baseline. Knee strength was not tested in this trial. The PEDro score of this study was 6/10.
Eccentric Exercise Versus Stretching
Norregaard et al 29 assessed the effectiveness of 12 weeks of eccentric exercise or stretching in those with Achilles tendinosis. Outcomes measured included a manually assessed tenderness score, a modified version of the Knee Injury and Osteoarthritis Outcome Score (KOOS) questionnaire, and a global assessment of the condition. Both the eccentric exercise group and the stretching group demonstrated modest but significant decreases in pain during time. However, no significant differences in pain were noted between the eccentric exercise group and the stretching group at any of the follow-up times. Muscular strength was not assessed in this study. The methodologic quality of this RCT was 4/10 based on the PEDro criteria.
Jensen and Di Fabio 32 investigated the effectiveness of eccentric exercise with an adjunctive stretching protocol for patellar tendinosis versus a control group that only performed the stretching protocol. Both pain and strength outcome measures were assessed; however, the pain scale data were presented in a way that precluded between-groups comparisons. No significant differences in strength existed between the groups at follow-up. This trial had a PEDro score of 4/10, which is below the average of the selected studies.
Eccentric Exercise Versus Night Splint
Roos et al 24 compared the effectiveness of eccentric exercise, night splints, and a combination of eccentric exercise and night splints for 12 weeks on Achilles tendinosis. The primary outcome variable measured was the Foot and Ankle Outcome Score (FOOS). No strength-related outcome measures were assessed in this study. All groups demonstrated substantial improvement in the FOOS Pain subscale across all follow-up times. Differences in the FOOS Pain subscale existed between the eccentric exercise-only and night splint-only groups at the 12-week follow-up, as the eccentric exercise group perceived less pain at that time. No significant differences were apparent among the 3 treatment groups during follow-up at 6, 26, and 52 weeks. 24 This study yielded a higher-than-average PEDro score of 6/10.
Splinting and eccentric exercise for patellar tendinosis have not been examined with respect to pain or strength outcomes.
Eccentric Exercise Versus Nonthermal Ultrasound Versus Friction Massage
Therapeutic modalities have not yet been compared with eccentric exercise for the treatment of Achilles tendinosis.
Stasinopoulos and Stasinopoulos 33 compared 3 treatment groups receiving interventions of eccentric exercise, nonthermal ultrasound, or transverse friction massage for patellar tendinosis during the course of 8 weeks. Significant improvements in pain were noted at the end of the treatment period and at 1-month and 3-month follow-up in the eccentric exercise group relative to the ultrasound and massage groups. The PEDro score of this study was 5/10.
DISCUSSION
Does eccentric exercise reduce pain and improve strength in physically active adults with symptomatic tendinosis? Unfortunately, the current body of evidence is insufficient to provide a simple yes or no response at this time. The best evidence to date demonstrates that eccentric exercise is likely a useful treatment for tendinosis 28–32; however, evidence is currently insufficient to suggest it is superior or inferior to other forms of therapeutic exercise. 25, 27–32 Eccentric exercise may be more effective in treating tendinosis than splinting 24 or some physical agents, 33 yet eccentric exercise was no more effective than no treatment during a competitive sports season. 26
The methodologic quality of the 11 selected studies was moderately good based on the average PEDro score (5.3/10), but power was insufficient to control type II error. Hence, additional significant differences may exist between eccentric exercise and alternative forms of treatment for tendinosis, but the selected trials lacked sufficient sample sizes for this to be determined.
Evaluation of Positive Outcomes
A minority of studies (3/11) provided evidence that eccentric exercise is superior to alternative rehabilitation for the treatment of tendinosis. 24, 25, 33 Benefits of eccentric exercise were observed when compared with control treatments consisting of concentric exercise, 25 night splinting, 24 nonthermal ultrasound, 33 and friction massage. 33 Of these studies, the 2 groups that demonstrated large reductions in pain investigated patellar tendinosis, 25, 33 whereas the others demonstrated smaller reductions in pain. 24 The positive outcomes do not appear to be related to any particular tendon, as 20% and 33% of the selected studies on Achilles and patellar tendinosis, respectively, demonstrated statistically significant improvements in the eccentric treatment over the control treatment.
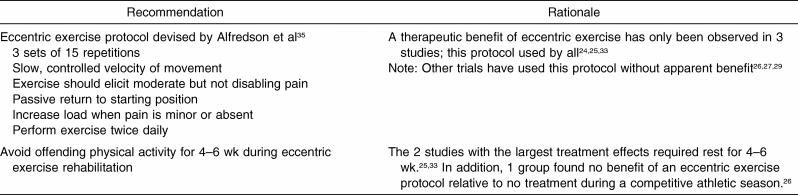
The 3 groups 24, 25, 33 that demonstrated eccentric exercise was superior to a control treatment for tendinosis used a similar exercise protocol. The protocol consisted of 3 sets of 15 repetitions, with a passive return to the starting position and a loading progression based on the amount of pain during the eccentric exercises, but it varied exercise frequencies of either 3 33 or 14 24, 25 times per week. These factors, although effective in 3 studies, 24, 25, 33 did not elicit the same benefits in 3 other studies. 26, 27, 29 This protocol is recommended despite inconsistent outcomes because it was the only protocol to demonstrate effectiveness relative to a control treatment ( Table 4).
Table 4. Recommendations for the Use of Eccentric Exercise in Symptomatic Tendinosis*.
Stress to the musculotendinous unit, regardless of whether it is concentric exercise or a passive stretch, may decrease symptoms associated with tendinosis as effectively as eccentric exercise. Eight of the selected groups used either passive stretching 29, 32 or concentric exercise 25, 27, 28, 30, 31, 34 as a treatment for the control group. Only 1 group 25 demonstrated that eccentric exercise reduced pain levels relative to an alternative therapeutic exercise, and the methodologic quality of the trial equaled the lowest PEDro score of the selected RCTs. In contrast to these studies, 3 groups compared eccentric exercise with interventions that did not stress the musculotendinous unit. 24, 26, 33 Eccentric exercise was more effective than splinting, 24 friction massage, 33 and nonthermal ultrasound 33 but no more effective than no treatment during a competitive athletic season. 26 These trends may suggest that any exercises that stress the musculotendinous unit are more effective treatment for tendinosis than treatments that do not stress the tissue.
The amount of physical activity allowed during rehabilitation had a tendency to be less in trials that demonstrated a benefit of eccentric exercise. In fact, the only 2 groups that mandated a period of rest from physical activity showed eccentric exercise to be far superior for pain control relative to the control treatment. 25, 33 Conversely, when full athletic participation was continued during the competitive season, eccentric exercise was no more effective than no treatment. 26 Thus, physical activity during rehabilitation appears to be a significant confounding factor that needs to be addressed in future research trials. In the interim, it is rational to combine eccentric exercise with a prolonged break (4–6 weeks), when feasible, from physical activities that stress the affected tendon ( Table 4).
The methodologic quality of the 3 studies with positive outcomes was mixed. The 2 studies that demonstrated large treatment effects with eccentric exercise had PEDro scores that were less than the average of the selected studies (4/10 25 and 5/10 33) and the sample sizes in these studies were limited to 10 or fewer per group. In a higher-quality trial (PEDro score of 6) 24 with only 10 to 13 participants per group, marginal treatment effects were noted for eccentric exercise. These limitations, although not extreme, may have biased the results and may confine generalizations to very specific clinical populations.
Mechanisms for the Efficacy of Eccentric Exercise
The mechanism of action for eccentric exercise on tendinosis remains speculative, but some interesting possibilities do exist. In their pioneering work, Curwin and Stanish 14 proposed that poor neuromuscular control during muscle action, especially during eccentric muscle action, may overload the tendon with high impulses. Hence, retraining the neuromuscular system to accommodate to eccentric loads may reduce excessive forces on the tendon. Although data demonstrate differences in movement patterns between patients with tendinosis and uninjured controls, 36, 37 whether eccentric training normalizes movement and loading patterns of patients with symptomatic tendinosis is unknown.
Eccentric exercise may enhance the mechanical properties of the degenerative tendon. Weight-bearing exercise has long been known to enhance the mechanical properties of tendons 38 by increasing blood flow, oxygen uptake, metabolic rate, collagen degradation, and collagen synthesis in healthy tendons. 39 Unfortunately, little information is available about how exercise affects tendinosis and how eccentric exercise differs from other types of exercise with respect to the structural basis of the tendon. Recently, Langberg et al 40 found that 12 weeks of eccentric exercise reduced tendinosis-related pain and stimulated collagen synthesis but did not change the rate of collagen degradation. This finding suggests that eccentric exercise may increase the mass of the tendon because of the enhanced deposition of type I collagen. The stimulation of type I collagen production may be of particular benefit because fibroblasts from areas of tendinosis normally synthesize a greater proportion of mechanically inferior type III collagen than their healthy counterparts. 41 Thus, eccentric exercise may serve to strengthen the tendon and protect it from subsequent overuse.
It has been theorized that eccentric exercise may inhibit the production of agents responsible for producing pain in tendinosis. 42 Chemical agents associated with symptomatic tendinosis include substance P, glutamate, and calcitonin gene-related peptide but exclude prostaglandin E 2. 43 Although these neuropeptides may be responsible for tendinosis pain, patients treated with eccentric exercise demonstrated no change in tendinous glutamate levels despite reduced pain. 42
Tendinosis pain is also associated with neovascularization, 44–46 but the pain may stem from the mechanical stimulation of pressure-sensitive autonomic nerves in the muscular walls of the arteries. 47 Interventions such as sclerosing injections 48 and eccentric exercise 49 may halt the growth of blood vessels in tendinosis and subsequently relieve some of the associated pain. Ohberg and Alfredson 49 speculated that mechanical forces from eccentric exercise disrupt or damage the neovessels, impairing their growth. However, recent evidence refutes this contention. 50 Alternately, Pufe et al 47 demonstrated that intermittent hydrostatic pressure elevation may increase the production of antiangiogenic factors and, thus, limit the growth of new vessels. However, limiting the growth of new vessels may eliminate the increased blood flow that could reduce tendon degeneration and ultimately strengthen the structure. Intermittent fluctuations in hydrostatic pressure may occur between sets during exercise, as blood flow is minimized during tension on the tendon. 51 Both eccentric and concentric exercise immediately increase water content and/or hyperemia in normal tendons and in those with tendinosis, 52 which may also activate the expression of antiangiogenic factors. 47
Although it is encouraging that clinicians may be able to reduce symptoms of tendinosis through eccentric exercise, it is questionable if the treatment actually reduces degeneration within the tendon. We must consider the long-term consequences of treating the symptoms only. In the absence of inflammation, healing of the damaged extracellular matrix remains unlikely, and the tendon will progressively weaken and may rupture.
Another important consideration with eccentric exercise is the potentially disparate effects that tensile force may have on tendinous adaptation. Participation in physical activity and sports may cause and aggravate tendinosis, yet large eccentric forces in a controlled rehabilitation setting may have a therapeutic effect. The location of the threshold between safe and unsafe eccentric loading is unclear. Clinicians must be aware of the continuum of factors that affect tendinous adaptation and ensure that the adopted protocol optimizes healing without producing harmful stresses.
Recommendations for Future Research
Several recommendations can be made to those who wish to study the effects of eccentric exercise on tendinosis. First, researchers should work to validate or refute the trends observed in this review. In general, studies comparing eccentric exercise with other therapeutic exercises, such as stretching or concentric exercise, yielded little or no differences in outcome. However, when eccentric exercise was compared with therapies that did not involve any form of therapeutic exercise, large differences in outcomes were generally noted. Also, eccentric exercise was more effective for tendinosis when the offending activity was avoided for an extended period.
Researchers must be vigilant against methodologic bias. Concealed allocation, intention-to-treat analyses, and assessor blinding were lacking in many of the included RCTs. Concealed allocation ensures that the person responsible for recruiting participants is unaware of the group to which the participant will be allocated. The bias produced by failing to conceal allocation may overestimate the effect of treatment by 30% to 40%. 53 Intention to treat is a strategy involving analysis of subject data in the groups to which the participants were originally assigned, regardless of whether any treatment was actually rendered. Intention to treat is important because persons with better outcomes are more likely to adhere to a treatment protocol than those with poorer outcomes. 54 Excluding noncompliant participants from the analysis leaves those participants who were bound to have a better outcome, biasing the original randomized comparison. 55 Lastly, by not blinding the outcome assessors to group membership, bias may occur because of treatment expectations. Adhering to the CONSORT guidelines 56 when conducting and reporting RCTs may eliminate many of these pitfalls.
Investigators in future trials should recruit sufficient numbers of subjects. Obtaining a large sample size is a difficult undertaking, as was noted by Roos et al, 24 who stated that it took 3 years to recruit 44 patients from a group of 20 primary care physicians. To facilitate this process, future researchers should consider undertaking multicenter trials to obtain adequate subject pools.
Lastly, another recommendation for future research is to use valid and reliable outcome measures that are patient oriented, such as pain, satisfaction, return to participation, and quality of life. Pain may be quantified with multidimensional general instruments, such as the McGill Pain Questionnaire, Brief Pain Inventory, or Descriptor Differential Scale, 57 or specifically, with the VISA outcome measures designed for Achilles 58 and patellar tendinoses. 59 Strength testing may be reliably performed at the ankle 60 and knee 61 with an isokinetic dynamometer. These suggestions are not the only viable outcome measures; however, it is imperative that the outcome measures used be psychometrically sound and appropriate for an active population.
CONCLUSIONS
Current research indicates that eccentric exercise is an effective form of treatment for lower extremity tendinoses, but little evidence suggests that it is superior to other forms of therapeutic exercise, such as concentric exercise or stretching. Eccentric exercise may produce better outcomes than some treatments, such as splinting, nonthermal ultrasound, and friction massage, and be most effective during a respite from activity-related loading.
We also recommend that clinicians follow the eccentric exercise protocol devised by Alfredson et al 35 and have patients rest for 4 to 6 weeks for optimal reduction of tendinosis symptoms. These recommendations are based on the best current evidence and are likely to be refined as more evidence arises.
REFERENCES
- Jarvinen M, Jozsa L, Kannus P, Jarvinen TL, Kvist M, Leadbetter W. Histopathological findings in chronic tendon disorders. Scand J Med Sci Sports. 1997;7:86–95. doi: 10.1111/j.1600-0838.1997.tb00124.x. [DOI] [PubMed] [Google Scholar]
- Case and Demographic Characteristics for Work-Related Injuries and Illnesses Involving Days Away From Work. Washington, DC: US Department of Labor, Bureau of Labor Statistics; 2003.
- James SL, Bates BT, Osternig LR. Injuries to runners. Am J Sports Med. 1978;6:40–50. doi: 10.1177/036354657800600202. [DOI] [PubMed] [Google Scholar]
- Kvist M. Achilles tendon injuries in athletes. Ann Chir Gynaecol. 1991;80:188–201. [PubMed] [Google Scholar]
- Lian OB, Engebretsen L, Bahr R. Prevalence of jumper's knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med. 2005;33:561–567. doi: 10.1177/0363546504270454. [DOI] [PubMed] [Google Scholar]
- Cook JL, Khan KM, Harcourt PR, Grant M, Young DA, Bonar SF. A cross sectional study of 100 athletes with jumper's knee managed conservatively and surgically: the Victorian Institute of Sport Tendon Study Group. Br J Sports Med. 1997;31:332–336. doi: 10.1136/bjsm.31.4.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kettunen JA, Kvist M, Alanen E, Kujala UM. Long-term prognosis for jumper's knee in male athletes: a prospective follow-up study. Am J Sports Med. 2002;30:689–692. doi: 10.1177/03635465020300051001. [DOI] [PubMed] [Google Scholar]
- Kannus P, Natri A. Etiology and pathophysiology of tendon ruptures in sports. Scand J Med Sci Sports. 1997;7:107–112. doi: 10.1111/j.1600-0838.1997.tb00126.x. [DOI] [PubMed] [Google Scholar]
- Kvist M. Achilles tendon injuries in athletes. Sports Med. 1994;18:173–201. doi: 10.2165/00007256-199418030-00004. [DOI] [PubMed] [Google Scholar]
- Chiara Vulpiani M, Guzzini M, Ferretti A. Operative treatment of chronic Achilles tendinopathy. Int Orthop. 2003;27:307–310. doi: 10.1007/s00264-003-0472-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman BD, Khan KM, Kiss ZS, Bartlett J, Young DA, Wark JD. Open and arthroscopic patellar tenotomy for chronic patellar tendinopathy: a retrospective outcome study. Victorian Institute of Sport Tendon Study Group. Am J Sports Med. 2000;28:183–190. doi: 10.1177/03635465000280020801. [DOI] [PubMed] [Google Scholar]
- Alfredson H, Lorentzon R. Chronic Achilles tendinosis: recommendations for treatment and prevention. Sports Med. 2000;29:135–146. doi: 10.2165/00007256-200029020-00005. [DOI] [PubMed] [Google Scholar]
- Puddu G, Ippolito E, Postacchini F. A classification of Achilles tendon disease. Am J Sports Med. 1976;4:145–150. doi: 10.1177/036354657600400404. [DOI] [PubMed] [Google Scholar]
- Curwin S, Stanish W. Tendinitis: Its Etiology and Treatment. Lexington, MA: Collamore Press; 1984.
- Fyfe I, Stanish WD. The use of eccentric training and stretching in the treatment and prevention of tendon injuries. Clin Sports Med. 1992;11:601–624. [PubMed] [Google Scholar]
- Stanish WD, Rubinovich RM, Curwin S. Eccentric exercise in chronic tendinitis. Clin Orthop Relat Res. 1986:208;65–68 . [PubMed]
- Verhagen AP, de Vet HC, de Bie RA. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol. 1998;51:1235–1241. doi: 10.1016/s0895-4356(98)00131-0. et al. [DOI] [PubMed] [Google Scholar]
- Sherrington C, Herbert RD, Maher CG, Moseley AM. PEDro. A database of randomized trials and systematic reviews in physiotherapy. Man Ther. 2000;5:223–226. doi: 10.1054/math.2000.0372. [DOI] [PubMed] [Google Scholar]
- Foley NC, Bhogal SK, Teasell RW, Bureau Y, Speechley MR. Estimates of quality and reliability with the physiotherapy evidence-based database scale to assess the methodology of randomized controlled trials of pharmacological and nonpharmacological interventions. Phys Ther. 2006;86:817–824. [PubMed] [Google Scholar]
- Hedges LV. Distribution theory for Glass's estimator of effect size and related estimators. J Educ Res. 1981;6:107–128. [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Assoc; 1988.
- Altman DG, Gardner MJ. Statistics with Confidence: Confidence Intervals and Statistical Guidelines. 2nd ed. Oxford, UK: BMJ Books; 2000:45– 56.
- Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of reporting of meta-analyses. Lancet. 1999;354:1896–1900. doi: 10.1016/s0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- Roos EM, Engstrom M, Lagerquist A, Soderberg B. Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy: a randomized trial with 1-year follow-up. Scand J Med Sci Sports. 2004;14:286–295. doi: 10.1111/j.1600-0838.2004.378.x. [DOI] [PubMed] [Google Scholar]
- Jonsson P, Alfredson H. Superior results with eccentric compared to concentric quadriceps training in patients with jumper's knee: a prospective randomised study. Br J Sports Med. 2005;39:847–850. doi: 10.1136/bjsm.2005.018630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visnes H, Hoksrud A, Cook J, Bahr R. No effect of eccentric training on jumper's knee in volleyball players during the competitive season: a randomized clinical trial. Clin J Sport Med. 2005;15:227–234. doi: 10.1097/01.jsm.0000168073.82121.20. [DOI] [PubMed] [Google Scholar]
- Mafi N, Lorentzon R, Alfredson H. Superior short-term results with eccentric calf muscle training compared to concentric training in a randomized prospective multicenter study on patients with chronic Achilles tendinosis. Knee Surg Sports Traumatol Arthrosc. 2001;9:42–47. doi: 10.1007/s001670000148. [DOI] [PubMed] [Google Scholar]
- Niesen-Vertommen SL, Taunton JE, Clement DB, Mosher RE. The effect of eccentric versus concentric exercise in the management of Achilles tendonitis. Clin J Sport Med. 1992;2:109–113. [Google Scholar]
- Norregaard J, Larsen CC, Bieler T, Langberg H. Eccentric exercise in treatment of Achilles tendinopathy. Scand J Med Sci Sports. 2007;17:133–138. doi: 10.1111/j.1600-0838.2006.00545.x. [DOI] [PubMed] [Google Scholar]
- Silbernagel KG, Thomee R, Thomee P, Karlsson J. Eccentric overload training for patients with chronic Achilles tendon pain: a randomised controlled study with reliability testing of the evaluation methods. Scand J Med Sci Sports. 2001;11:197–206. doi: 10.1034/j.1600-0838.2001.110402.x. [DOI] [PubMed] [Google Scholar]
- Cannell LJ, Taunton JE, Clement DB, Smith C, Khan KM. A randomised clinical trial of the efficacy of drop squats or leg extension/leg curl exercises to treat clinically diagnosed jumper's knee in athletes: pilot study. Br J Sports Med. 2001;35:60–64. doi: 10.1136/bjsm.35.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen K, Di Fabio RP. Evaluation of eccentric exercise in treatment of patellar tendinitis. Phys Ther. 1989;69:211–216. doi: 10.1093/ptj/69.3.211. [DOI] [PubMed] [Google Scholar]
- Stasinopoulos D, Stasinopoulos I. Comparison of effects of exercise programme, pulsed ultrasound and transverse friction in the treatment of chronic patellar tendinopathy. Clin Rehabil. 2004;18:347–352. doi: 10.1191/0269215504cr757oa. [DOI] [PubMed] [Google Scholar]
- Young MA, Cook JL, Purdam CR, Kiss ZS, Alfredson H. Eccentric decline squat protocol offers superior results at 12 months compared with traditional eccentric protocol for patellar tendinopathy in volleyball players. Br J Sports Med. 2005;39:102–105. doi: 10.1136/bjsm.2003.010587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfredson H, Pietila T, Jonsson P, Lorentzon R. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med. 1998;26:360–366. doi: 10.1177/03635465980260030301. [DOI] [PubMed] [Google Scholar]
- Baur H, Divert C, Hirschmuller A, Muller S, Belli A, Mayer F. Analysis of gait differences in healthy runners and runners with chronic Achilles tendon complaints. Isokinet Exerc Sci. 2004;12:111–116. [Google Scholar]
- Richards DP, Ajemian SV, Wiley JP, Zernicke RF. Knee joint dynamics predict patellar tendinitis in elite volleyball players. Am J Sports Med. 1996;24:676–683. doi: 10.1177/036354659602400520. [DOI] [PubMed] [Google Scholar]
- Tipton CM, Matthes RD, Maynard JA, Carey RA. The influence of physical activity on ligaments and tendons. Med Sci Sports. 1975;7:165–175. [PubMed] [Google Scholar]
- Kjaer M, Magnusson P, Krogsgaard M. Extracellular matrix adaptation of tendon and skeletal muscle to exercise. J Anat. 2006;208:445–450. doi: 10.1111/j.1469-7580.2006.00549.x. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langberg H, Ellingsgaard H, Madsen T. Eccentric rehabilitation exercise increases peritendinous type I collagen synthesis in humans with Achilles tendinosis. Scand J Med Sci Sports. 2007;17:61–66. doi: 10.1111/j.1600-0838.2006.00522.x. et al. [DOI] [PubMed] [Google Scholar]
- Maffulli N, Ewen SW, Waterston SW, Reaper J, Barrass V. Tenocytes from ruptured and tendinopathic Achilles tendons produce greater quantities of type III collagen than tenocytes from normal Achilles tendons: an in vitro model of human tendon healing. Am J Sports Med. 2000;28:499–505. doi: 10.1177/03635465000280040901. [DOI] [PubMed] [Google Scholar]
- Alfredson H, Lorentzon R. Intratendinous glutamate levels and eccentric training in chronic Achilles tendinosis: a prospective study using microdialysis technique. Knee Surg Sports Traumatol Arthrosc. 2003;11:196–199. doi: 10.1007/s00167-003-0360-0. [DOI] [PubMed] [Google Scholar]
- Alfredson H. The chronic painful Achilles and patellar tendon: research on basic biology and treatment. Scand J Med Sci Sports. 2005;15:252–259. doi: 10.1111/j.1600-0838.2005.00466.x. [DOI] [PubMed] [Google Scholar]
- Cook JL, Malliaras P, De Luca J, Ptasznik R, Morris M. Vascularity and pain in the patellar tendon of adult jumping athletes: a 5 month longitudinal study. Br J Sports Med. 2005;39:458–461. doi: 10.1136/bjsm.2004.014530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gisslen K, Alfredson H. Neovascularisation and pain in jumper's knee: a prospective clinical and sonographic study in elite junior volleyball players. Br J Sports Med. 2005;39:423–428. doi: 10.1136/bjsm.2004.013342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchis-Alfonso V, Rosello-Sastre E, Subias-Lopez A. Neuroanatomic basis for pain in patellar tendinosis (“jumper's knee”): a neuroimmunohistochemical study. Am J Knee Surg. 2001;14:174–177. [PubMed] [Google Scholar]
- Pufe T, Petersen W, Kurz B, Tsokos M, Tillmann B, Mentlein R. Mechanical factors influence the expression of endostatin—an inhibitor of angiogenesis—in tendons. J Orthop Res. 2003;21:610–616. doi: 10.1016/S0736-0266(02)00262-0. [DOI] [PubMed] [Google Scholar]
- Alfredson H, Ohberg L. Neovascularisation in chronic painful patellar tendinosis—promising results after sclerosing neovessels outside the tendon challenge the need for surgery. Knee Surg Sports Traumatol Arthrosc. 2005;13:74–80. doi: 10.1007/s00167-004-0549-x. [DOI] [PubMed] [Google Scholar]
- Ohberg L, Alfredson H. Effects on neovascularisation behind the good results with eccentric training in chronic mid-portion Achilles tendinosis? Knee Surg Sports Traumatol Arthrosc. 2004;12:465–470. doi: 10.1007/s00167-004-0494-8. [DOI] [PubMed] [Google Scholar]
- Boesen M, Koenig MJ, Torp-Pedersen S, Bliddal H, Langberg H. Tendinopathy and Doppler activity: the vascular response of the Achilles tendon to exercise. Scand J Med Sci Sports. 2006;16:463–469. doi: 10.1111/j.1600-0838.2005.00512.x. [DOI] [PubMed] [Google Scholar]
- Ohberg L, Lorentzon R, Alfredson H. Neovascularisation in Achilles tendons with painful tendinosis but not in normal tendons: an ultrasonographic investigation. Knee Surg Sports Traumatol Arthrosc. 2001;9:233–238. doi: 10.1007/s001670000189. [DOI] [PubMed] [Google Scholar]
- Shalabi A, Kristoffersen-Wiberg M, Aspelin P, Movin T. Immediate Achilles tendon response after strength training evaluated by MRI. Med Sci Sports Exerc. 2004;36:1841–1846. doi: 10.1249/01.mss.0000145450.75035.61. [DOI] [PubMed] [Google Scholar]
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273:408–412. doi: 10.1001/jama.273.5.408. [DOI] [PubMed] [Google Scholar]
- Horwitz RI, Viscoli CM, Berkman L. Treatment adherence and risk of death after a myocardial infarction. Lancet. 1990;336:542–545. doi: 10.1016/0140-6736(90)92095-y. et al. [DOI] [PubMed] [Google Scholar]
- Montori VM, Guyatt GH. Intention-to-treat principle. CMAJ. 2001;165:1339–1341. [PMC free article] [PubMed] [Google Scholar]
- Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet. 2001;357:1191–1194. [PubMed] [Google Scholar]
- O'Connor P J, Murphy RM, Courson RW, Ferrara MS. Pain assessment in Journal of Athletic Training articles 1992-1998: implications for improving research and practice . J Athl Train. 2000;35:151–154. [PMC free article] [PubMed] [Google Scholar]
- Robinson JM, Cook JL, Purdam C. The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. Br J Sports Med. 2001;35:335–341. doi: 10.1136/bjsm.35.5.335. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visentini PJ, Khan KM, Cook JL, Kiss ZS, Harcourt PR, Wark JD. The VISA score: an index of severity of symptoms in patients with jumper's knee (patellar tendinosis). Victorian Institute of Sport Tendon Study Group. J Sci Med Sport. 1998;1:22–28. doi: 10.1016/s1440-2440(98)80005-4. [DOI] [PubMed] [Google Scholar]
- Chester R, Costa ML, Shepstone L, Donell ST. Reliability of isokinetic dynamometry in assessing plantarflexion torque following Achilles tendon rupture. Foot Ankle Int. 2003;24:909–915. doi: 10.1177/107110070302401207. [DOI] [PubMed] [Google Scholar]
- Li RC, Wu Y, Maffulli N, Chan KM, Chan JL. Eccentric and concentric isokinetic knee flexion and extension: a reliability study using the Cybex 6000 dynamometer. Br J Sports Med. 1996;30:156–160. doi: 10.1136/bjsm.30.2.156. [DOI] [PMC free article] [PubMed] [Google Scholar]