Abstract
Context: Although dozens of individual mechanical and functional insufficiencies have been reported in those with chronic ankle instability (CAI), no authors to date have examined the relationship of the insufficiencies to each other. Therefore, studying both the functional and mechanical insufficiencies in the same experimental design will provide valuable information.
Objective: To determine the relationships among the numerous functional and mechanical insufficiencies purported to cause CAI.
Design: Descriptive study with a correlational design.
Setting: Medical center and research laboratory.
Patients or Other Participants: Thirty subjects with unilateral CAI (15 males and 15 females: age = 20.3 ± 1.3 years; height = 172.5 ± 10.7 cm; mass = 72.9 ± 15.8 kg).
Main Outcome Measure(s): Twenty-six measures of mechanical insufficiencies (ankle laxity and hypomobility) and functional insufficiencies (subjective level of function, static and dynamic balance, ankle and hip strength) were taken on both limbs of all subjects. Bivariate correlations using Pearson product moment coefficients were calculated between all dependent variables measured in the unstable ankles. The level of significance was set a priori at P ≤ .05 for all analyses.
Results: A number (35) of significant bivariate correlations were identified. Most (32) of these significant relationships were found between functional instability measures ( r = .38 to .96). Three significant relationships were noted between measures of functional (balance, strength) and mechanical (laxity, hypomobility) instability ( r = .47 to .52). No significant relationships were found between the different mechanical instability measures.
Conclusions: Certain measures of functional instability were significantly correlated and may be redundant. Additionally, the significant correlations between measures of functional (balance, strength) and mechanical instability (laxity, hypomobility) demonstrate that the 2 factors are not completely dichotomous and need to be examined together.
Keywords: ankle sprains, correlation analysis, rehabilitation
Key Points
Functional and mechanical ankle instability are not completely dichotomous and need to be assessed together.
When testing subjects with functional ankle instability, it may not be necessary to test all elements of balance and strength.
All elements of mechanical ankle instability should be examined, as few relationships exist among them.
Chronic ankle instability (CAI) has been reported to occur in approximately 31% to 40% of people with a previous history of a lateral ankle sprain 1, 2 and describes the occurrence of repetitive bouts of lateral ankle instability. 3 Numerous ankle sprains and a subjective feeling of the ankle “giving way” result. These chronic symptoms limit the patient in both activities of daily living and athletic activity. Two primary causes of CAI have been deemed responsible: mechanical ankle instability (MAI) and functional ankle instability (FAI). 3–5 A variety of insufficiencies that lead to each type of instability have been identified in those with CAI. Mechanical insufficiencies include pathologic laxity, impaired arthrokinematics, and synovial and degenerative changes. 3, 6 Functional insufficiencies include impaired proprioception, altered neuromuscular control, strength deficits, and diminished postural control. 3 Despite the fact that dozens of individual mechanical and functional insufficiencies have been reported in those with CAI, no authors have examined the relationship of multiple measures of these insufficiencies to each other. Therefore, examining both the functional and mechanical insufficiencies of CAI together in the same experimental design will provide important information.
Previous researchers 4, 5, 7–13 examining ankle instability have focused on identifying differences between individuals with and without CAI. Mechanical and functional instability are often seen as 2 dichotomous causes of CAI. Although a relationship between MAI and FAI has been suggested, 3, 5, 7 we do not currently know what this exact relationship is. The aforementioned groups 3, 5, 7 did not compare the different measures of FAI and MAI statistically. Additionally, we do not know what the relationship is within the measures of FAI and MAI. For example, if a patient has a deficit in one FAI measure, can we assume he or she also has deficits in other FAI measures as well? Also, are MAI and FAI truly dichotomous? By understanding these relationships, we can make more informed clinical decisions regarding which exercises would best help a particular patient without having to test or examine for all possible insufficiencies. Scientifically, by better understanding these relationships, we improve our knowledge of the relationships among the different measures related to CAI and make better decisions as to which variables should be examined in future research projects.
Therefore, our purpose was to examine the bivariate correlations of self-reported ankle function, ankle mobility, static and dynamic balance, ankle and hip strength, and selected lower extremity alignment and flexibility measures in subjects with unilateral CAI. We selected these variables because previous authors have reported deficits in subjects with CAI. Three primary comparisons were examined: (1) FAI to FAI variables, (2) MAI to MAI variables, and (3) MAI to FAI variables.
METHODS
Subjects
This study is part of a larger study in which we examined differences between subjects with and without CAI. 8 Thirty subjects with unilateral CAI (15 males and 15 females: age = 20.3 ± 1.3 years; height = 172.5 ± 10.7 cm; mass = 72.9 ± 15.8 kg) participated in the current arm of the study. Subjects had a mean of 5.8 ± 2.7 previous ankle sprains, with a mean time since the first ankle sprain of 37.5 ± 23.8 months. Subjects filled out an ankle instability questionnaire 9 that contained the criteria for CAI classification. Inclusion criteria included a previous history of unilateral ankle sprain, frequent giving way of the ankle (at least once a month), pain, feelings of instability, and decreased function. Subjects were excluded if they had experienced an acute ankle sprain within 6 weeks of participation in the study, if they had a history of surgery or fracture to either lower extremity, or if they had experienced any previous sprain of the limb contralateral to the chronically unstable ankle. All subjects signed an informed consent agreement approved by the university's institutional review board (which also approved the study) before initiation of testing.
Protocol
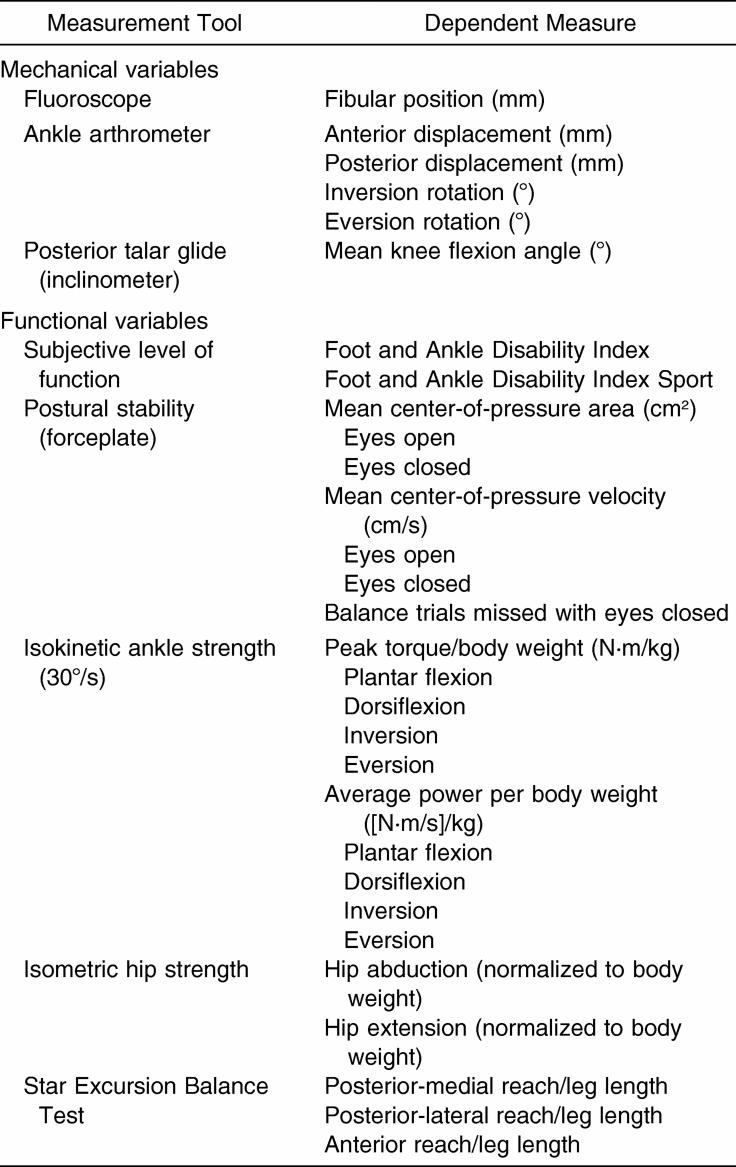
Data collection took place in 2 sessions that were separated by 2 to 4 weeks. Table 1 lists all measurement tools and dependent variables. At session 1, all subjects completed the Foot and Ankle Disability Index (FADI) to gauge the amount of self-reported disability. 10 The FADI is a subjective self-report of function with 2 components. The main FADI assesses activities of daily living, while the Sport Scale assesses more difficult tasks that are essential to sport. Reliability and sensitivity of both components have been previously reported in subjects with and without CAI. 10 Session 1 also comprised completion of fluoroscopic images, which were recorded at an orthopaedic clinic, whereas all other measures were collected at a sports medicine research laboratory during session 2. The measures obtained in session 2 were counterbalanced with a Latin square to avoid any order effects. All measures were taken on both limbs of each subject, but for this part of the study, we report only those from the limbs with CAI.
Table 1. Measurement Tools and Dependent Measures.
Mechanical Variables
Fibular position was determined by taking a lateral image of each ankle. A Mini 6600 fluoroscope with a digital mobile C-arm (OEC Medical Systems Inc, Salt Lake City, UT) recorded the images. Subject positioning and set-up replicated previously reported methods. 11, 12 Reliability has been reported for test-retest reliability (intraclass correlation [ICC] coefficient = .98, SEM = 0.64 mm) and for intratester reliability (ICC = .98, SEM = 0.64 mm). 11 A radiographic marker was placed on all ankles to correct for variances in magnification. Measurements to determine the position of the fibula were made on the printed images. The distance between the anterior margin of the fibula and the anterior margin of the tibia was recorded in millimeters. 11, 12 A smaller value indicates a more anteriorly positioned fibula in relation to the tibia.
Instrumented measurement of ankle-subtalar joint stability was performed using a portable ankle arthrometer (Blue Bay Research Inc, Navarre, FL). The arthrometer has been reported to be a highly reliable and valid tool for ankle ligamentous stability assessment. 13, 14 Testing and subject positioning replicated previously reported methods. 13–15 To measure anterior-posterior laxity, the ankles were loaded with 125 N in each direction. Starting at the neutral position, an anterior load was applied initially, followed by a posterior load. For inversion-eversion laxity, the ankles were loaded to 4000 N·m of inversion and eversion torque. Starting at the neutral position, inversion loading was applied first, followed by eversion loading. One trial was carried out for each direction. Dependent measures were the amount of anterior and posterior laxity (in millimeters) and the inversion and eversion laxity (in degrees).
To assess talar hypomobility, a posterior talar glide test was performed. 16 Subjects were seated with their legs at 90° off the end of an examining table, and an inclinometer was positioned just above the talocrural joint to measure the amount of knee flexion range of motion. With the subject relaxed, the foot was placed into subtalar neutral while the examiner gently glided the talus posteriorly until a firm capsular end-feel was encountered. 16 Once this restriction was felt, the angle of knee flexion represented an indirect measure of talar mobility. A lower angle of knee flexion represented less posterior talar mobility. 16 The mean of 3 trials served as the dependent variable.
Functional Variables
Postural control was measured using an AMTI Accusway forceplate (AMTI Inc, Watertown, MA) interfaced with a laptop computer using Swaywin software (AMTI). Subject positioning and set-up replicated previously reported methods. 17 Three-dimensional forces and moments were recorded at 50 Hz, and the software program calculated center-of-pressure (COP) excursions. Subjects performed 6 trials (3 with eyes open, 3 with eyes closed) of quiet standing in single-leg stance on both the right and left limbs. Each trial lasted 10 seconds. Trials were disregarded if a touchdown (foot contacted forceplate or ground) occurred during the trial. Subjects who could not complete all 3 balance trials were assigned a zero and were not included in the analysis. The number of missed trials (foot touchdowns) for each condition was also counted. Subjects' touchdown scores ranged from 0 (no missed trials) to 3 (missed all 3 trials). Dependent variables included COP velocity, COP area, and the number of missed balance trials. Missing values for COP velocity and COP area were assigned to the subjects who touched down during all 3 trials in a given condition.
Dynamic balance was assessed with the Star Excursion Balance Test (SEBT). The SEBT is a reliable and valid tool for balance assessment in those with ankle instability. 18, 19 Dependent variables were the posterior-medial, posterior-lateral, and anterior reach directions. A verbal and visual demonstration was given to each subject. The subject performed 6 practice trials in each direction and on each leg. To perform the SEBT, the subject maintained a single-leg stance while reaching with the contralateral leg (reach leg) as far as possible along the specified direction. 18, 19 The subject touched the furthest point possible on the line with the most distal part of the reach foot. The distance from the center of the grid to the touch point was manually measured (in centimeters) with a tape measure. Three reach distances in each direction were recorded and normalized to subject leg length. 20 The average of the 3 reach trials in each direction was calculated.
Strength was measured on a Biodex 2 isokinetic dynamometer (Biodex Medical Systems Inc, Shirley, NY). Subject positioning and set-up replicated previously reported methods. 21 Peak torque/body weight and average power/body weight for concentric muscle contractions at 30°/s in plantar flexion, dorsiflexion, inversion, and eversion were recorded. Subjects performed 3 submaximal warm-ups before each test. Five maximal repetitions were performed in each direction. The mean peak torque/body weight and average power/body weight for each direction were recorded.
For hip strength testing, a handheld dynamometer was attached to a fixed platform, similar to the one developed by Nadler et al. 22 Good intertester reliability (hip extension ICC = .56 to 80, hip abduction ICC = .69 to .88) and intratester reliability (ICC = .72 to .89) have been previously reported with these procedures. 23 Mean hip abduction and hip extension isometric strength (in kilograms of force normalized to body weight) were measured. A Nicholas Manual Muscle Tester (Lafayette Instruments Co, Lafayette, IN) was mounted to a platform and attached to a standard treatment table. The platform could be lowered or elevated based on the size of the subject. For hip extension, subjects were positioned prone. The dynamometer was placed one third of the distance from the gluteal crest to the popliteal fossa. With the subject's knee flexed, a maximal voluntary isometric contraction for hip extension was held for 5 seconds. The mean of 3 trials was recorded.
For hip abduction, the dynamometer was placed one third of the distance from the greater trochanter to the lateral joint line of the knee. A pillow was placed between the subject's legs to keep them in a neutral position. A maximal voluntary isometric contraction for hip abduction was held for 5 seconds. The mean of 3 trials was recorded.
Statistical Analysis
We calculated bivariate correlations using Pearson product moment correlations between all dependent measures taken on the involved limbs of the subjects with unilateral CAI. Three primary comparisons were examined: (1) FAI to FAI variables, (2) MAI to MAI variables, and (3) MAI to FAI variables. A correlation coefficient r of 0 to .4 was considered to represent a weak relationship, a coefficient of .4 to .7 was considered to represent a moderate relationship, and a coefficient of .7 to 1.0 was considered to represent a strong relationship. 24 The level of significance was set a priori at P < .05.
RESULTS
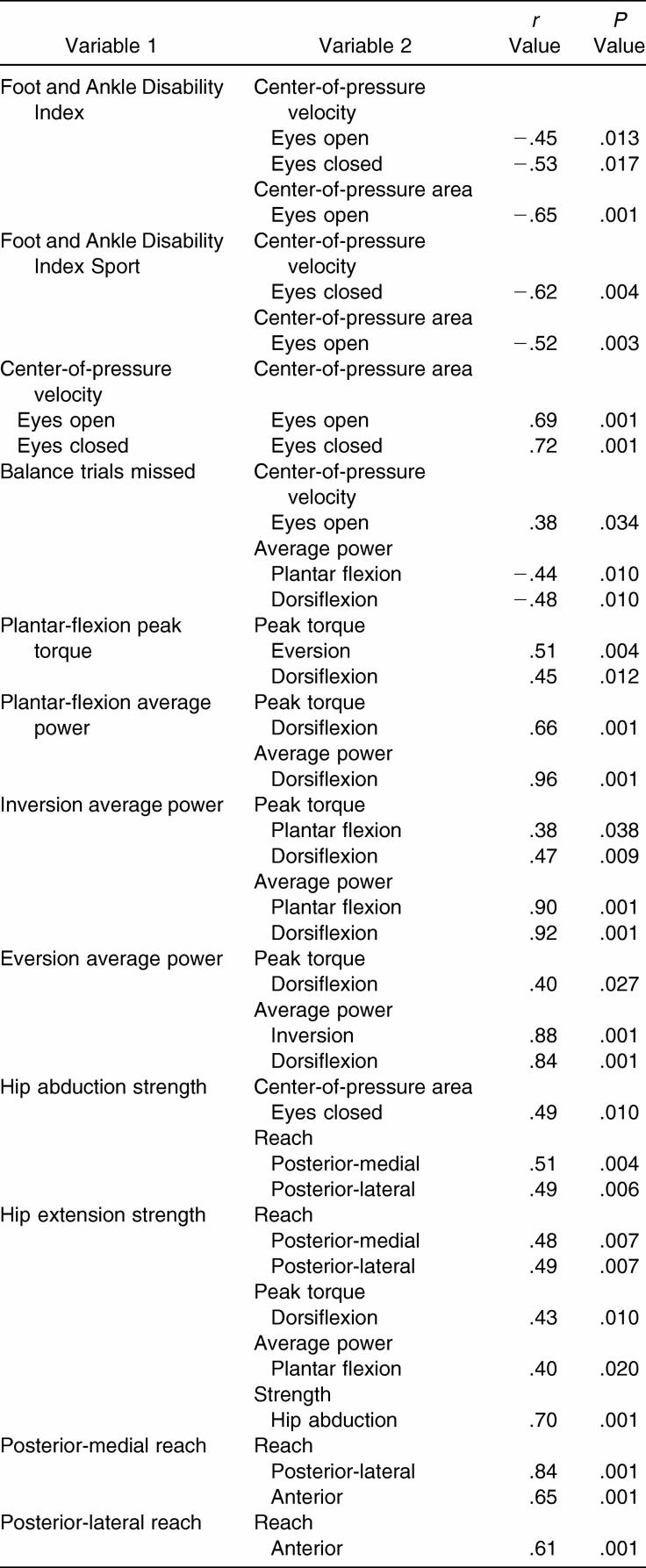
A number (35) of significant bivariate correlations were identified. Most (32) of these significant relationships were found between the functional instability measures. The strength of the relationships ranged from r = .38 to r = .96. The range of the nonsignificant relationships was r = .01 to r = .34. The strongest relationship was between plantar-flexion average power (AP) and dorsiflexion AP ( r = .96, P < .0001). Table 2 lists all significant relationships between FAI measures.
Table 2. Bivariate Correlations Between Functional Instability Measures Identified as Statistically Significant ( P ≤ .05) for the Ankles With Chronic Instability .
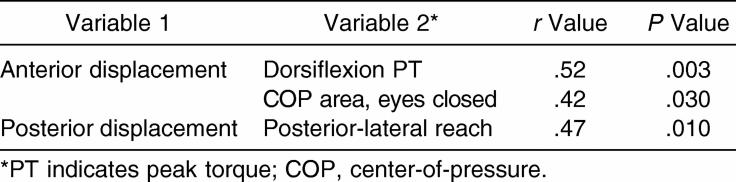
Three significant relationships were noted between measures of FAI and MAI. The strengths of the relationships ranged from r = .38 to r = .52. The range of the nonsignificant relationships was r = .01 to r = .36. The strongest relationship was between anterior laxity and dorsiflexion peak torque (PT) ( r = .52, P = .003). Table 3 lists all significant relationships between FAI and MAI measures. No significant relationships were noted between the MAI measures. The strengths of these relationships ranged from r = .02 to r = .25.
Table 3. Bivariate Correlations Between Measures of Functional and Mechanical Instability Identified as Being Statistically Significant ( P < .05) for the Ankles With Chronic Instability .
DISCUSSION
Numerous significant relationships were seen between the FAI measures. The direct relationships between similar variables, such as individual measures of strength and balance, were strong. A few significant relationships were demonstrated between the FAI and MAI variables. Although the relationships were significant, they were relatively moderate relationships, as demonstrated by the Pearson product moment correlation values, with the strongest direct relationship being between anterior laxity and dorsiflexion PT ( r = .52). No significant correlations occurred between the mechanical variables.
Relationships Between Functional Instability Measures
The strongest relationships were found between the ankle strength measures. Numerous significant relationships were revealed between PT and AP for all 4 planes of ankle motion. As strength decreased in one plane, it decreased in the other planes as well. The strongest direct relationship between plantar-flexion AP and dorsiflexion AP was r = .96, and the weakest direct relationship was between inversion AP and plantar-flexion PT ( r = .38). It may not be necessary to test all 4 planes of ankle motion or both AP and PT. Additionally, the relationship among all 4 planes of ankle motion demonstrates that central changes may be the cause of strength deficits, instead of peripheral changes. Clinically, if strength is reduced in one direction, strengthening exercises should still be performed in all directions. The results of our strength values compare favorably with those from previous research. 7, 21, 25
The main FADI scores correlated moderately with COP velocity with eyes open ( r = −.45), COP area with eyes open ( r = −.65), and COP velocity with eyes closed ( r = −.53). The FADI Sport scores also correlated moderately with COP area with eyes open ( r = −.52) and COP velocity with eyes closed ( r = −.62). As the scores on the main FADI and FADI Sport decreased (indicating worse subjective functioning), COP velocity and area increased (indicating poorer static balance). Of all the FAI variables we measured, static postural control measures were most closely related to self-reported functional deficits. Interestingly, a limitation of static balance is that it is not as “functional” a measure as dynamic balance; however, we found it to significantly correlate with self-reported function, whereas our measures of dynamic balance with the SEBT did not. Based on these results, subjects who report decreased function also have deficits in static balance.
The number of missed balance trials with eyes closed correlated moderately with plantar flexion ( r = −.44) and dorsiflexion ( r = −.48) AP. As the number of missed balance trials increased (foot touchdowns), strength decreased. During balance performance, only 20 of 30 subjects were able to complete at least 1 of the 3 trials for the eyes-closed condition. Balance trials missed were counted, so we did not lose data from the subjects who could not balance with their eyes closed. The ability to maintain a single-leg stance without falling or touching the ground requires activation of all dynamic stabilizers surrounding the ankle. Although the significant relationship was between the ankle plantar flexors and dorsiflexors, based on the correlations between the strength variables, in the larger portion of this study, 8 we reported an overall weakness of all 4 muscle groups that may cause an increase in balance trials missed. We only saw this relationship with strength and balance trials missed, not with COP velocity and area. However, missed balance trials correlated moderately with COP velocity with eyes open ( r = .38). As for our other static balance measures, COP velocity with eyes open significantly correlated ( r = .69) with COP area with eyes open, and COP velocity with eyes closed significantly correlated ( r = .72) with COP area with eyes closed. With these relationships between the static balance measures, it may not be necessary to test more than 1 variable. We may be able to understand static balance by simply looking at 1 variable (COP velocity with eyes open).
A significantly strong relationship was noted between hip abduction and extension strength ( r = .70). Additionally, hip abduction ( r = .51, r = .49) and extension strength ( r = .48, r = .49) correlated with the posterior-medial and posterior-lateral reach directions of the SEBT, respectively. In addition to requiring balance on the affected limb, the posterior directions may require considerable hip strength. The stronger the hip abductors and extensors, the further subjects were able to reach in both directions. This indicates that the dynamic balance deficits seen in the ankles with CAI may also be related to weakness in the hip abductors and extensors. We did not observe any significant relationships between the SEBT and ankle strength measures. One reason we may not have seen these relationships at the ankle is that subjects with a history of ankle instability perhaps used a “top-down” or hip strategy to control their balance. Tropp et al 5 first noted that when postural control could no longer be corrected by the ankle, the body seemed to react as a multisegmental chain, with large corrections occurring in the hip. Changes in hip strength may then result in deficits in balance. Hip abduction also correlated with COP area with eyes closed ( r = .49). In addition to relating to dynamic balance, weaker hip abductors may relate to poor static balance. Previous researchers have noted proximal neuromuscular changes in those with CAI. 26 Bullock-Saxton et al 26 reported bilateral deficits in hip muscle activation in subjects with severe ankle sprains. These proximal changes may influence the subject's ability to maintain upright posture. Further evidence of these proximal changes may be noted in the significant relationships among hip extension strength and plantar-flexion AP ( r = .40) and dorsiflexion PT ( r = .43).
A significant and strong relationship was seen between our dynamic balance task variables. Posterior-medial reach correlated with posterior-lateral reach ( r = .85) and anterior reach ( r = .66). Additionally, posterior-lateral reach correlated with anterior reach ( r = .61). Recently a study group 19 examined all 8 components of the SEBT and found that the posterior-medial component was most representative of the performance of all 8 components of the test in subjects with and without CAI. Considerable redundancy between performance scores in all 8 directions was also found. 19 The r values we report compare favorably with those reported by Hertel et al. 19 From the results of these 2 studies, it is apparent that not all components of the SEBT need to be tested as a result of the redundancy in the tasks.
No significant relationships were demonstrated between the static and dynamic postural control variables, likely because they test different aspects of neuromuscular control. Thus, we need to test both static and dynamic balance activities in those with CAI.
The strongest relationships were reported within the functional variables. Given these relationships, it may not be necessary to test the different static and dynamic balance variables in all planes of ankle strength and hip strength. Examining 1 element of each may give us an idea of the functional status of the subject, minimizing the time required of subjects but still giving researchers the information needed. Additionally, clinicians can determine which elements need emphasis during rehabilitation. If an athlete has poor dynamic balance, hip strength should also be addressed during rehabilitation.
Relationships Between Mechanical Instability Measures
No significant correlations were found between any of the mechanical instability measures we examined. To our knowledge, no authors have reported a relationship between anterior and inversion laxity. Damage to the lateral ligament structures of the ankle leads to an increase in anterior-medial rotation of the talus. 27 Stress tests may be able to demonstrate the increase in anterior laxity but not inversion laxity, which may explain the lack of a relationship. The lack of a significant relationship with posterior talar glide may be because a decreased posterior glide has only been reported after an acute lateral ankle sprain. 16 It may not be present in those with CAI. As a result of these findings, it is important to examine both hypermobility and hypomobility in subjects with CAI, as little relationship appears to exist between the variables. Clinically, all planes should be evaluated for mechanical laxity, and hypomobility should be examined as well in patients with CAI.
Relationships Between Functional and Mechanical Instability Measures
We observed few relationships between our FAI and MAI measures. Increased anterior laxity correlated moderately with increased dorsiflexion PT ( r = .52) and an increased COP area with eyes closed ( r = .42). Increased dorsiflexion strength may compensate for the decreased static stability, thereby helping to prevent or slow the plantar-flexion injury mechanism. The relationship between laxity and increased COP area is not unexpected. Although speculative, damage to the ligamentous mechanoreceptors is one of the purported causes of postural control deficits. 4, 5, 28
Posterior laxity correlated moderately with posterior-lateral reach ( r = .47). As posterior laxity decreased, posterior-lateral reach decreased. The mobility of the talus influences the physiologic motions of plantar flexion and dorsiflexion. Posterior laxity may be due to altered talar mobility, which could affect ankle planar flexion, resulting in decreased posterior-lateral reach.
One limitation of this study is that a large number of comparisons were conducted without adjusting the α level. However, we feel that interpretation of a correlation analysis relies more on the r value than the P value. Additionally, based on the exploratory nature of this study, more important information is conveyed by leaving the α level at .05 and reporting the r values of the significant correlations than is conveyed by adjusting the α level.
No previous investigators have directly examined the relationships between FAI and MAI in the same study design. Typically, MAI and FAI have been thought of as dichotomous variables. However, based on our results, a relationship between the two is apparent. Although this relationship may appear to be limited based on the number of significant variables, those variables are important (laxity, strength, balance) in both static and dynamic control of the ankle and have important implications in the care and rehabilitation of ankle injuries. Therefore, FAI and MAI should be examined together. A patient with MAI may still benefit from rehabilitation, and treating the mechanical instability may improve the FAI. Yet not all functional variables may need to be examined or treated. In the acute case, MAI can be addressed by focusing on ligament healing (immobilization, crutches). 29 Both bracing and surgery have been demonstrated to improve FAI in those with CAI. 30, 31
CONCLUSIONS
When investigating FAI, we need not examine all measures because of the moderate to strong relationships between some of them. Specifically, it may not be necessary to examine multiple elements of balance and strength. However, when examining MAI, it is important to look at the numerous insufficiencies, as few relationships exist between the measures. Additionally, the relationships between FAI and MAI demonstrate that the two are not completely dichotomous and need to be examined together. Clinically, some functional variables need to be treated even in the absence of obvious limitations, because they relate strongly to other variables with deficits.
Acknowledgments
We would like to thank the NATA Research & Education Foundation for support of this project.
REFERENCES
- Bosien WR, Staples OS, Russell SW. Residual disability following acute ankle sprains. J Bone Joint Surg Am. 1955;37:1237–1243. [PubMed] [Google Scholar]
- Staples OS. Result study of ruptures of lateral ligaments of the ankle. Clin Orthop Rel Res. 1972;85:50–58. doi: 10.1097/00003086-197206000-00011. [DOI] [PubMed] [Google Scholar]
- Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37:364–375. [PMC free article] [PubMed] [Google Scholar]
- Freeman MAR, Dean MRE, Hanham IWF. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47:678–685. [PubMed] [Google Scholar]
- Tropp HP, Odenrick P, Gillquist J. Stabilometry recordings in functional and mechanical instability of the ankle joint. Int J Sports Med. 1985;6:180–182. doi: 10.1055/s-2008-1025836. [DOI] [PubMed] [Google Scholar]
- Hubbard TJ, Hertel J. Mechanical contributions to chronic ankle instability. Sports Med. 2006;36:263–277. doi: 10.2165/00007256-200636030-00006. [DOI] [PubMed] [Google Scholar]
- Wilkerson GB, Pinerola JJ, Caturano RW. Invertor vs. evertor peak torque and power deficiencies associated with lateral ankle ligament injury. J Orthop Sports Phys Ther. 1997;26:78–86. doi: 10.2519/jospt.1997.26.2.78. [DOI] [PubMed] [Google Scholar]
- Hubbard TJ, Kramer LC, Denegar CR, Hertel J. Contributing factors to chronic ankle instability. Foot Ankle Int. 2007;28:343–354. doi: 10.3113/FAI.2007.0343. [DOI] [PubMed] [Google Scholar]
- Hubbard TJ, Kaminski TW. Kinesthesia is not affected by functional ankle instability status. J Athl Train. 2002;37:481–486. [PMC free article] [PubMed] [Google Scholar]
- Hale SA, Hertel J. Reliability and sensitivity of the Foot and Ankle Disability Index in subjects with chronic ankle instability. J Athl Train. 2005;40:35–40. [PMC free article] [PubMed] [Google Scholar]
- Hubbard TJ, Hertel J, Sherbondy P. Fibular position in individuals with self-reported chronic ankle instability. J Orthop Sports Phys Ther. 2006;36:3–9. doi: 10.2519/jospt.2006.36.1.3. [DOI] [PubMed] [Google Scholar]
- Mavi A, Yildirim H, Gunes H, Pestamalci T, Gumusburun E. The fibular incisura of the tibia with recurrent sprained ankle on magnetic resonance imaging. Saudi Med J. 2002;23:845–849. [PubMed] [Google Scholar]
- Hubbard TJ, Kovaleski JE, Kaminski TW. Reliability of intratester and intertester measurements derived from an instrumented ankle arthrometer. J Sport Rehabil. 2003;12:208–220. [Google Scholar]
- Kovaleski JE, Gurchiek LR, Heitman RJ, Hollis JM, Pearsall AW., IV. Instrumented measurement of anteroposterior and inversion-eversion laxity of the normal ankle joint complex. Foot Ankle Int. 1999;20:808–814. doi: 10.1177/107110079902001210. [DOI] [PubMed] [Google Scholar]
- Hubbard TJ, Kaminski TW, Vander Griend RA, Kovaleski JE. Quantitative assessment of mechanical laxity in the functionally unstable ankle. Med Sci Sports Exerc. 2004;36:760–766. doi: 10.1249/01.mss.0000126604.85429.29. [DOI] [PubMed] [Google Scholar]
- Denegar CR, Hertel J, Fonseca J. The effect of lateral ankle sprain on dorsiflexion range of motion, posterior talar glide, and joint laxity. J Orthop Sports Phys Ther. 2002;32:166–173. doi: 10.2519/jospt.2002.32.4.166. [DOI] [PubMed] [Google Scholar]
- Hertel J, Guskiewicz KM, Kahler DM, Perrin DH. Effect of lateral joint anesthesia on center of balance, postural sway, and joint position sense. J Sport Rehabil. 1996;5:111–119. [Google Scholar]
- Olmsted LC, Carcia CR, Hertel J, Shultz SJ. Efficacy of the Star Excursion Balance Tests in detecting reach deficits in subjects with chronic ankle instability. J Athl Train. 2002;37:501–506. [PMC free article] [PubMed] [Google Scholar]
- Hertel J, Braham RA, Hale SA, Olmsted-Kramer LC. Simplifying the Star Excursion Balance Test: analyses of subjects with and without chronic ankle instability. J Orthop Sports Phys Ther. 2006;36:131–137. doi: 10.2519/jospt.2006.36.3.131. [DOI] [PubMed] [Google Scholar]
- Gribble PA, Hertel J. Predictors for performance of dynamic postural control using the Star Excursion Balance Task. Measure Phys Ed Exerc Sci. 2003;7:89–100. [Google Scholar]
- Kaminski TW, Perrin DH, Gansneder BM. Eversion strength analysis of uninjured and functionally unstable ankles. J Athl Train. 1999;34:239–245. [PMC free article] [PubMed] [Google Scholar]
- Nadler SF, DePrince ML, Hauesien N, Malanga GA, Stitik TP, Price E. Portable dynamometer anchoring station for measuring strength of the hip extensors and abductors. Arch Phys Med Rehabil. 2000;10:1072–1076. doi: 10.1053/apmr.2000.7165. [DOI] [PubMed] [Google Scholar]
- Scott DA, Bond EQ, Sisto SA, Nadler SF. The intra- and interrater reliability of hip muscle strength assessments using a handheld versus a portable dynamometer anchoring station. Arch Phys Med Rehabil. 2004;85:598–603. doi: 10.1016/j.apmr.2003.07.013. [DOI] [PubMed] [Google Scholar]
- Lomax RG. Statistical Concepts: A Second Course for Education and Behavioral Sciences. 2nd ed. Mahwah, NJ: Lawrence Erlbaum Assoc Inc; 1998:179–188.
- McKnight CM, Armstrong CW. The role of ankle strength in functional ankle instability. J Sport Rehabil. 1997;6:21–29. [Google Scholar]
- Bullock-Saxton JE, Janda V, Bullock MI. The influence of ankle sprain injury on muscle activation during hip extension. Int J Sports Med. 1994;15:330–334. doi: 10.1055/s-2007-1021069. [DOI] [PubMed] [Google Scholar]
- Kjaersgaard-Andersen P, Wethelund JO, Helmig P, Nielsen S. Effect of the calcaneofibular ligament on hindfoot rotation in amputation specimens. Acta Orthop Scand. 1987;58:135–138. doi: 10.3109/17453678709146459. [DOI] [PubMed] [Google Scholar]
- Riemann BL. Is there a link between chronic ankle instability and postural instability? J Athl Train. 2002;37:386–393. [PMC free article] [PubMed] [Google Scholar]
- Cordova ML, Ingersoll CD, Palmieri RM. Efficacy of prophylactic ankle support: an experimental perspective. J Athl Train. 2002;37:446–457. [PMC free article] [PubMed] [Google Scholar]
- Baumhauer JF, O'Brien T. Surgical considerations in the treatment of ankle instability. J Athl Train. 2002;37:458–462. [PMC free article] [PubMed] [Google Scholar]
- Karlsson J, Bergsten T, Lansinger O, Peterson L. Reconstruction of the lateral ligaments of the ankle for chronic ankle instability. J Bone Joint Surg Am. 1988;70:581–588. [PubMed] [Google Scholar]