Abstract
Smoking cessation often results in weight gain. Although smoking cessation frequently is recommended to patients presenting for weight loss surgery (WLS), the relationship between smoking cessation and weight gain among WLS candidates is poorly understood. Thus, we sought to document the history and prevalence of smoking and smoking-related weight gain among WLS candidates. Subjects (N = 67) presenting for bariatric surgery provided demographic information, were interviewed about smoking, and weighed and measured prior to operation. Sixty-seven percent of patients reported a lifetime history of smoking, and 26.9% were current smokers. Among lifetime smokers who had attempted to quit, the average maximum amount of weight gained following smoking cessation was 28.1 pounds, but there was wide variability in postcessation weight gain. These data suggest that smoking among candidates for bariatric surgery is prevalent, and that previous cessation attempts were associated with considerable weight gain. Because patients often receive recommendations to quit smoking and lose weight prior to surgery, additional information on the impact of presurgical smoking cessation on long-tem weight control in this population is needed.
Keywords: tobacco smoking, smoking cessation, body weight, obesity, surgery
1. Introduction
Bariatric surgery, the recommended treatment for obese individuals with Class 3 [body mass index (BMI) greater than 40] or Class 2 (BMI of 35 to 40) obesity with medical comorbitities (NIH Consensus Development Panel, 1992), has become increasingly common (Santry, Gillen, & Lauderdale, 2005). Bariatric, or weight loss, surgery (WLS) typically results in loss of 61% of excess weight (Buchwald et al., 2004), and resolution or improvement in obesity-related comorbidities (Buchwald et al., 2004; Maggard et al., 2005). However, it also carries the risks of a major abdominal operation, with adverse events in about 20% of cases (Maggard et al., 2005).
Cigarette smoking is one documented risk factor for surgical complications in general and for complications after WLS in particular. Among patients undergoing pulmonary surgery, smokers had more post-operative complications than those who had never smoked (Nakagawa, Tanaka, Tsukama, & Kishi, 2001), and smokers tend to have longer hospital stays than do non smokers (Barrera et al., 2005). Smoking also has been related to thomboembolic and pulmonary complications (Gonzalez, Haines, Nelson, Gallagher, & Murr, 2006) and poor long-term survival for WLS patients (Zhang, Mason, Renquist, & Zimmerman, 2005). Although smoking cessation is associated with improvements in health and decreases in surgical complications, it also is associated with weight gain. On average, smokers gain 8–10 pounds upon quitting smoking (e.g., Hudmon, Gritz, Clayton, & Nisenbaum, 1999; Klesges et al., 1997), and some subgroups of smokers, most notably those concerned about postcessation weight, have reported maximum previous weight gains of 13.7 pounds (Levine, Perkins, & Marcus, 2001). The high rates of psychiatric comorbidity in WLS candidates (Sarwer, Wadden & Fabricatore, 2005; Kalarchian et al., in press) and the well-established link between psychiatric disorders and tobacco use (Breslau, Novak & Kessler, 2004; John, Meyer, Rumpf & Hapke, 2004) further complicate the potential impact of smoking cessation on weight for WLS candidates. Thus, the relationship between smoking cessation and weight change may be important in WLS.
Estimates of the prevalence of smoking prior to surgery among WLS patients range from 16% to 38% (Grace, Pederson, Speechley, & McAlpine, 1990; Nguyen, Rivers, & Wolfe, 2003; Zhang et al., 2005). However, data on the effects of smoking on WLS outcome are limited. Some investigations have shown that smoking pre- (Dixon, Dixon & O’Brien, 2001), or postoperatively (Grace et al., 1990) modestly increased weight loss after operation, but others have found preoperative smoking to be associated with decreased weight loss (Latner, Wetzler, Goodman, & Glinski, 2004). Nonetheless, the current recommendation is that patients quit smoking prior to WLS (Saltzman et al., 2005). Patients are also encouraged to lose weight prior to WLS (Saltzman et al., 2005). Given these recommendations, it is important to understand smoking and cessation-related weight gain among individuals presenting for WLS. Thus, we documented rates of lifetime and current smoking and the relationship between smoking and smoking-related weight gain in candidates for weight loss surgery.
2. Method
2.1. Participants
Participants were 67 individuals presenting for WLS at a large medical center. On average, participants were 40.1 (±6.2) years old, with a BMI of 52.4 (±9.8). Most were female (85.1 %) and white (82.1%).
2.2. Procedure
Participants provided demographic information, and were weighed, measured and interviewed about smoking behaviors prior to operation. Participants were divided into lifetime smokers and never smokers according to self-reported smoking status. Lifetime smokers were participants who indicated having ever been a smoker, while never smokers reported neither current nor lifetime smoking. Lifetime smokers were further divided according to smoking status at the preoperation interview into current smokers and former smokers, with former smokers representing participants who had smoked in their lifetime, but were not smoking at the time of the preoperation evaluation. Among lifetime smokers, we further separated those reporting having ever made a quit attempt (attempted quitters).
Data analyses included descriptive statistics to document rates of lifetime and current smoking, the number of cessation attempts, amount of cessation-related weight gain. Current smokers were compared to never and former smokers, using t-tests and chi-squares for continuous and categorical responses, respectively. To examine the association of postcessation weight gain to other presurgery characteristics (demographic and weight factors), we divided attempted quitters according to those who did (n =25) and did not (n = 9) report weight gain in previous smoking cessation attempts and compared these groups using t-tests and chi-squares for continuous and categorical responses, respectively. In addition, the association between previous postcessation weight gain and preoperation weight and BMI was examined using bivariate Pearson correlations.
2.3. Assessments
2.3.1. Weight and demographic information
Preoperation weight and height were obtained from the surgeon’s records, and BMI was calculated as weight in kilograms divided by height in meters squared. Prior to surgery, patients completed a brief questionnaire on which they indicated their marital status, race and ethnicity, highest completed level of education and gender.
2.3.2. Smoking behavior
Patients were asked if they had ever been a smoker, and those answering yes were considered lifetime smokers. Lifetime smokers were asked about current smoking, efforts to quit and weight gain associated with smoking cessation. Patients who indicated having ever made a quit attempt, (attempted quitters) were asked to report the maximum amount of weight gained after quit attempts, the time frame in which the weight gain occurred and whether weight gain related to a resumption of smoking.
3. Results
Sixty-seven percent (n = 45) reported a lifetime history of cigarette smoking, and 26.9% (n = 18) were smoking at the time of the preoperation evaluation. As shown in Table 1, current smokers were younger (36.3 ± 9.1 vs. 43.5 ± 8.5 years, p = .01) and less well educated (33% vs. 85% with some college education, p<.001) than were former smokers. However, there was no difference in preoperation BMI between current and former smokers (49.7 ± 12.0 vs. 53.3 ± 8.5 k/m2 for current vs. former smokers, respectively). Most lifetime smokers (82.2%; n = 37) reported having tried to quit (i.e., attempted quitters), with an average of 3.3 ± 4.2 cessation attempts. Additional details on the smoking histories of attempted quitters are provided in Table 2.
Table 1.
Characteristics of WLS candidates by smoking status (N = 67).
| Never Smokers (n = 18) | Former Smokers (n = 27) | Current Smokers (n = 18) | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Current age | 39.1a | 10.2 | 43.5ab | 8.6 | 36.3a | 9.1 |
| BMI | 53.4a | 9.1 | 53.3a | 8.5 | 49.7a | 12.0 |
| % female | 95.5a | 74.1b | 88.9a,b | |||
| % white | 90.9a | 81.5a | 72.2a | |||
| % married | 45.5a | 55.6a | 50.0a | |||
| % partial college or more | 77.3a | 85.2a | 33.3b | |||
Note. Cells with different superscripts are significantly different in post-hoc, two way comparisons.
Table 2.
Smoking history of WLS patients who have attempted to quit smoking (n = 37).
| Mean | SD | |
|---|---|---|
| Current age | 41.0 | 9.0 |
| Age started smoking | 16.2 | 5.1 |
| Age of regular smoking | 19.1 | 6.6 |
| Number of cessation attempts | 3.3 | 4.2 |
| % female | 81.1 | |
| % white | 81.1 | |
| % married | 54.1 | |
| % partial college or more | 62.2 | |
Among attempted quitters, 45.9% reported worrying about gaining weight with smoking cessation, and 67.6% reported having gained weight after quitting smoking. On average, surgery candidates reported having gained 28.1 (± 20.6) pounds over an 8.7 (± 12.8) month period after smoking cessation. As shown in Figure 1, there was wide variability in maximum postcessation weight gains. Close to half (45.9 %) of WLS candidates indicated that weight gain led to a resumption of smoking. However, maximum postcessation weight gain was not correlated with preoperation BMI, r = .10, p = .67. In addition, patients who did and did not gain weight upon quitting were similar in preoperation weight, BMI, age, sex, marital status or education level.
Figure 1.
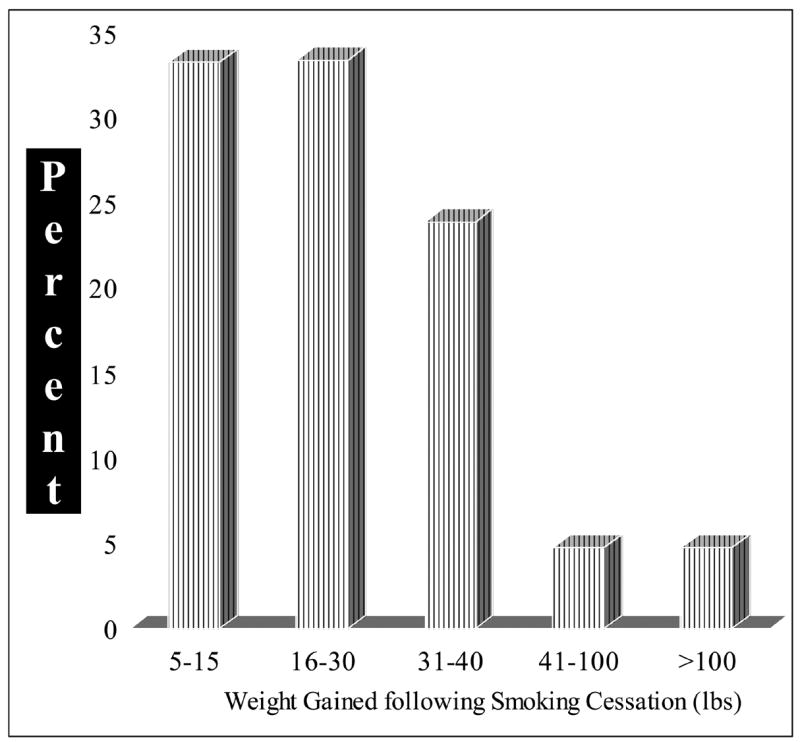
Maximum postcessation weight gains among candidates presenting for WLS.
4. Discussion
A considerable proportion of individuals presenting for bariatric surgery report a history of smoking. In this study, 67% of WLS candidates had a lifetime history of smoking, and 27% were currently smoking. By comparison, estimates of the population prevalence of lifetime (ever smoking 100 cigarettes or more) and current smoking (smoking on at least some days) are 42.4% and 21%, respectively (CDC, 2005). Thus, the rate of current smoking among WLS candidates appears to be similar to, and the rate of lifetime smoking appears to be higher than, that observed in the general population.
Additionally, previous attempts at smoking cessation in WLS candidates were associated with considerable weight gain. Average maximum postcessation weight gain in this sample (28 pounds) is approximately double that found among smokers with specific concerns about postcessation weight gain (Levine et al., 2001), and larger than the average amount gained by smokers within six months of cessation (Hudmon et al., 1999; Perkins et al., 2001). Although the presurgical BMIs of former and never smokers did not differ, the large weight gains experienced by WLS candidates in previous cessation attempts suggest that the recommendations to WLS patients to lose weight and quit smoking prior to operation (Saltzman et al., 2005) may conflict. Patients who are asked to quit smoking in anticipation of WLS may gain weight. However, patients are also encouraged to lose weight prior to surgery, and the weight gain associated with smoking cessation could negatively affect efforts to lose weight before WLS. It is also possible that a smoking cessation attempt made in preparation for surgery may be followed by relapse to smoking after operation. Pre-operative smoking cessation programs have been shown to increase abstinence rates before (Ratner et al., 2004; Wolfenden et al., 2005) and immediately post surgery (McHugh et al., 2001; Wolfenden et al, 2005), but the longer-term cessation outcome of these interventions is poor (Ratner et al., 2004). Moreover, WLS has not been shown to affect smoking behavior reliably (Karason, Lindroos, Stenlof, & Sjostrom, 2000; Latner et al., 2004). Thus, efforts to quit smoking in preparation for surgery may not increase rates of long-term smoking cessation and may negatively affect weight loss outcomes among WLS candidates. Nonetheless, any negative impact of smoking cessation on weight loss may be offset by the health benefits of quitting.
Although these data provide preliminary evidence of a smoking-related weight gain in bariatric surgery candidates, there are several important limitations to this study. First, these data are from a small sample of patients presenting for surgery, and both smoking and weight gain were assessed through retrospective, self-report. Thus, there is limited power for tests of differences among current, former and never smokers, and the data are subject to recall and reporting biases. Second, the majority of participants in this study were female, and the relationship between smoking and weight differs between men and women (e.g., Borrelli, Spring, Niaura, Hitsman, & Papandonatos, 2001; John, Meyer, Rumpf, & Hapke, 2005).
Nonetheless, these data suggest future work on smoking and smoking cessation among bariatric surgery patients is needed. For example, because many WLS patients may be worried about gaining additional weight, addressing smoking cessation in this population may require a specific focus on weight. A smoking cessation program treatment designed to ameliorate cessation-related weight concerns has been found to improve rates of cessation and to attenuate cessation-related weight gain relative to efforts to prevent weight gain after smoking cessation (Perkins et al., 2001), and may be useful with WLS candidates. Finally, medications, such as bupropion, that promote cessation and may mitigate weight gain (Hays et al., 2001; Jorenby et al., 1999) may be useful for WLS candidates.
Acknowledgments
This research was supported by grant K01 DA04174 from the National Institute on Drug Abuse (PI: Levine) and grant K23 DK62291 from the National Institute of Diabetes and Digestive and Kidney Diseases (PI: Kalarchian). The authors are grateful to Rebecca Ringham, Ph.D. for assistance with interviews and data collection.
Portions of this paper were presented at the 23rd Annual Meeting of the American Society for Bariatric Surgery, San Francisco, CA, June, 2006.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Barrera R, Weiji S, Amar D, Thaler HT, Gabovich N, Bains MS, White DA. Smoking and timing of cessation: Impact on pulmonary complications after thoracotomy. CHEST. 2005;127(6):1977–1983. doi: 10.1378/chest.127.6.1977. [DOI] [PubMed] [Google Scholar]
- Borrelli B, Spring B, Niaura R, Hitsman B, Papandonatos G. Influences of gender and weight gain on short-term relapse to smoking in a cessation trial. Journal of Consulting and Clinical Psychology. 2001;69(3):511–515. doi: 10.1037//0022-006x.69.3.511. [DOI] [PubMed] [Google Scholar]
- Breslau N, Novak SP, Kessler RC. Psychiatric disorders and stages of smoking. Biological Psychiatry. 2004;55(1):69–76. doi: 10.1016/s0006-3223(03)00317-2. [DOI] [PubMed] [Google Scholar]
- Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K. Bariatric surgery: A systematic review and meta-analysis. Journal of the American Medical Association. 2004;292:1724–37. doi: 10.1001/jama.292.14.1724. [DOI] [PubMed] [Google Scholar]
- CDC. Cigarette smoking among adults--United States, 2004. MMWR. 2005;54(44):1121–1124. [PubMed] [Google Scholar]
- Dixon JB, Dixon ME, O’Brien PE. Pre-operative predictors of weight loss at 1-year after lap-band surgery. Obesity Surgery. 2001;11:200–207. doi: 10.1381/096089201321577884. [DOI] [PubMed] [Google Scholar]
- Gonzalez R, Haines K, Nelson KG, Gallagher SF, Murr MM. Predictive factors of thromboembolic events in patients undergoing Roux-en-Y gastric bypass. Surgery for Obesity & Related Diseases. 2006;2(1):30–35. doi: 10.1016/j.soard.2005.10.003. [DOI] [PubMed] [Google Scholar]
- Grace DM, Pederson L, Speechley KN, McAlpine D. A longitudinal study of smoking status and weight loss following gastroplasty in a group of morbidly obese patients. International Journal of Obesity. 1990;14:311–317. [PubMed] [Google Scholar]
- Hays JT, Hurt RD, Rigotti NA, Niaura R, Gonzales D, Durcan MJ, Sachs DP, Wolter TD, Buist AS, Johnston JA, White JD. Sustained-release bupropion for pharmacologic relapse prevention after smoking cessation. A randomized, controlled trial. Annals of Internal Medicine. 2001;135(6):423–433. doi: 10.7326/0003-4819-135-6-200109180-00011. [DOI] [PubMed] [Google Scholar]
- Hudmon KS, Gritz ER, Clayton S, Nisenbaum R. Eating orientation, postcessation weight gain, and continued abstinence among female smokers receiving an unsolicited smoking cessation intervention. Health Psychology. 1999;18(1):29–36. doi: 10.1037//0278-6133.18.1.29. [DOI] [PubMed] [Google Scholar]
- John U, Meyer C, Rumpf H, Hapke U. Smoking, nicotine dependence and psychiatric comorbidity—A population-based study including smoking cessation after three years. Drug and Alcohol Dependence. 2004;76(3):287–295. doi: 10.1016/j.drugalcdep.2004.06.004. [DOI] [PubMed] [Google Scholar]
- John U, Meyer C, Rumpf H, Hapke U. Relationships of psychiatric disorders with overweight and obesity in an adult general population. Obesity Research. 2005;13(1):101–109. doi: 10.1038/oby.2005.13. [DOI] [PubMed] [Google Scholar]
- Jorenby DE, Leischow SJ, Nides MA, Rennard SI, Johnston JA, Hughes AR, Smith SS, Muramoto ML, Daughton DM, Doan K, Fiore MC, Baker TB. A controlled trial of sustained-release bupropion, a nicotine patch, or both for smoking cessation. The New England Journal of Medicine. 1999;340(9):685–691. doi: 10.1056/NEJM199903043400903. [DOI] [PubMed] [Google Scholar]
- Kalarchian MA, Marcus MD, Levine MD, Courcoulas AP, Pilkonis PA, Ringham RM, Soulakova JN, Weissfeld LA, Rofey DL. Psychiatric disorders among bariatric surgery candidates: Relationship to obesity and functional health status. American Journal of Psychiatry. doi: 10.1176/ajp.2007.164.2.328. in press. [DOI] [PubMed] [Google Scholar]
- Karason K, Lindroos AK, Stenlof K, Sjostrom L. Relief of cardiorespiratory symptoms and increased physical activity after surgically induced weight loss: results from the Swedish Obese Subjects Study. Archives of Internal Medicine. 2000;160(12):1797–802. doi: 10.1001/archinte.160.12.1797. [DOI] [PubMed] [Google Scholar]
- Klesges RC, Winders SE, Meyers AW, Eck LH, Ward KD, Hultquist CM, Ray JW, Shadish WR. How much weight gain occurs following smoking cessation? A comparison of weight gain using both continuous and point prevalence abstinence. Journal of Consulting and Clinical Psychology. 1997;65(2):286–291. doi: 10.1037//0022-006x.65.2.286. [DOI] [PubMed] [Google Scholar]
- Latner JD, Wetzler S, Goodman ER, Glinski J. Gastric bypass in a low-income, inner-city population: Eating disturbances and weight loss. Obesity Research. 2004;12(6):956–961. doi: 10.1038/oby.2004.117. [DOI] [PubMed] [Google Scholar]
- Levine MD, Perkins KA, Marcus MD. The characteristics of women smokers concerned about postcessation weight gain. Addictive Behaviors. 2001;26:749–756. doi: 10.1016/s0306-4603(00)00156-8. [DOI] [PubMed] [Google Scholar]
- Maggard MA, Shugarman LR, Suttorp M, Maglione M, Sugarmen HJ, Livingston EH, Nguyen NT, Li Z, Mojica WA, Hilton L, Rhodes S, Morton SC, Shekelle PG. Meta-analysis: Surgical treatment of obesity. Annals of Internal Medicine. 2005;142:547–59. doi: 10.7326/0003-4819-142-7-200504050-00013. [DOI] [PubMed] [Google Scholar]
- McHugh F, Lindsay GM, Hanlon P, Hutton I, Brown MR, Morrison C, Wheatley DJ. Nurse led shared care for patients on the waiting list for coronary artery bypass surgery: A randomised controlled trial. Heart. 2001;86:317–323. doi: 10.1136/heart.86.3.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakagawa M, Tanaka H, Tsukuma H, Kishi Y. Relationship between the duration of the preoperative smoke-free period and the incidence of postoperative pulmonary complications after pulmonary surgery. CHEST. 2001;120(3):705–710. doi: 10.1378/chest.120.3.705. [DOI] [PubMed] [Google Scholar]
- National Institutes of Health Consensus Development Panel. Gastrointestinal surgery for severe obesity: National Institutes of Health Consensus Development Conference Statement. American Journal of Clinical Nutrition. 1992;(55):615S–619S. doi: 10.1093/ajcn/55.2.615s. [DOI] [PubMed] [Google Scholar]
- Nguyen NT, Rivers R, Wolfe BM. Factors associated with operative outcomes in laparoscopic gastric bypass. Journal of the American College of Surgeons. 2003;197(4):548–555. doi: 10.1016/S1072-7515(03)00648-3. [DOI] [PubMed] [Google Scholar]
- Perkins KA, Marcus MD, Levine MD, D’Amico D, Miller A, Broge M, Ashcom J, Shiffman S. Cognitive-behavioral therapy to reduce weight concerns improves smoking cessation outcome in weight-concerned women. Journal of Consulting and Clinical Psychology. 2001;69:604–613. [PubMed] [Google Scholar]
- Ratner PA, Johnson JL, Richardson CG, Bottorff JL, Moffat B, Mackay M, Fofonoff D, Kingsbury K, Miller C, Budz B. Efficacy of a smoking-cessation intervention for elective-surgical patients. Research in Nursing & Health. 2004;27:148–161. doi: 10.1002/nur.20017. [DOI] [PubMed] [Google Scholar]
- Saltzman E, Anderson W, Apovian CM, Boulton H, Chamberlain A, Cullum-Dugan D, Cummings S, Hatchigian E, Hodges B, Keroack CR, Pettus M, Thomason P, Veglia L, Young LS. Criteria for patient selection and multidisciplinary evaluation and treatment of the weight loss surgery patient. Obesity Research. 2005;13(2):234–243. doi: 10.1038/oby.2005.32. [DOI] [PubMed] [Google Scholar]
- Santry HP, Gillen DL, Lauderdale DS. Trends in bariatric surgery procedures. Journal of the American Medical Association. 2005;294(15):1909–1917. doi: 10.1001/jama.294.15.1909. [DOI] [PubMed] [Google Scholar]
- Sarwer DB, Wadden TA, Fabricatore AN. Psychosocial and behavioral aspects of bariatric surgery. Obesity Research. 2005;13(4):639–648. doi: 10.1038/oby.2005.71. [DOI] [PubMed] [Google Scholar]
- Wolfenden L, Wiggers J, Knight J, Campbell E, Rissel C, Kerridge R, Spigelman AD, Moore K. A programme for reducing smoking in pre-operative surgical patients: Randomised controlled trial. Anaesthesia. 2005;60:172–179. doi: 10.1111/j.1365-2044.2004.04070.x. [DOI] [PubMed] [Google Scholar]
- Zhang W, Mason EE, Renquist KE, Zimmerman MB. Factors influencing survival following surgical treatment of obesity. Obesity Surgery. 2005;15:43–50. doi: 10.1381/0960892052993422. [DOI] [PubMed] [Google Scholar]


