Abstract
Problematic substance use is associated with depression. Clarifying the relationship between substance use and depression remains an important research goal, with implications for prevention and treatment. Individual differences in the ability to tolerate negative physical and emotional sensations were hypothesized to play a role in substance use behaviors among depressed individuals. The present study investigated the roles of discomfort and distress tolerance in the relationship between alcohol and cannabis problems and depression among undergraduates (N = 265). Consistent with other reports, depression was correlated with alcohol and cannabis problems. As predicated, distress tolerance mediated the relationships between depression and alcohol and cannabis problems. Interestingly, discomfort intolerance moderated the relationship between depression and cannabis problems such that depressed individuals with high discomfort tolerance were most vulnerable to cannabis problems. These data suggest that distress intolerance may at least partially account for alcohol and cannabis problems among depressed young adults whereas discomfort intolerance may actually serve a protective role in the development of cannabis problems.
Keywords: Marijuana, Cannabis, Alcohol, Depression, Distress Intolerance, Discomfort Intolerance
Alcohol use disorders (AUD) and illicit substance use disorders (SUD) are associated with high rates of depression (Grant et al., 2003). Depression is associated with a two-fold increase in the rate of AUD (Grant et al., 2004; Grant et al., 2003) and a six-fold increase in the rate of cannabis use disorder (Grant, 1995). Despite the high rates of AUD and SUD among depressed individuals, the mechanisms underlying these relations remain unclear. Individual differences in the ability to tolerate negative emotional and physical sensations could help explain these linkages. Distress intolerance is a decreased capacity to withstand negative emotional states and has been linked to substance misuse (Simons & Gaher, 2005). There is good reason to believe distress intolerance may at least partially account for substance problems in depressed individuals. To illustrate, using alcohol to cope with psychological distress mediates the link between negative affect regulation expectancies and alcohol use (Galen, Henderson, & Coovert, 2001). Comparable relations have been found for cannabis use (Simons, Gaher, Correia, Hansen, & Christopher, 2005).
Discomfort intolerance is similar to distress tolerance but refers to an individual difference in the capacity to tolerate unpleasant bodily sensations (Schmidt, Richey, Cromer, & Buckner, in press). Although we know of no direct tests of the moderational effects of discomfort intolerance on substance use, past work suggests discomfort intolerance may increase the risk of substance-related impairment. For instance, using alcohol in response to physical discomfort is related to alcohol use problems (Turner, Annis, & Sklar, 1997). The relation between physical discomfort and cannabis has received less attention; yet data suggest that cannabis use may also be linked to discomfort intolerance. For instance, cannabis users are more likely to endorse the expectation that using cannabis will attenuate physical discomfort (Schafer & Brown, 1991) and some patients report using cannabis to relieve discomfort associated with physical illness (Woolridge et al., 2005).
In sum, the link between problematic substance use and depression is well established, yet much work remains to identify the mechanisms underlying this association. Conceptual models and some empirical data suggest that distress and discomfort intolerance may act as vulnerabilities for substance use problems. The present study is the first to directly examine distress and discomfort intolerance in relation to substance use problems and depression. Specifically, we examined both moderation and mediation models. It was hypothesized that discomfort intolerance would moderate the link between depression and substance use problems such that depressed individuals with high discomfort intolerance would demonstrate the greatest risk of alcohol and cannabis problems. In line with past work on affect regulation and substance use (e.g., Simons et al., 2005), it was hypothesized that distress intolerance would mediate the relation between depression and alcohol and cannabis use problems.
1. Methods
1.1. Participants
The present sample consisted of 265 psychology undergraduates. The sample was predominantly Caucasian (78.1%) and female (62.3%) with a mean age of 18.7 (SD = 1.2). Nearly 74% reported consuming alcohol more than once in the past month and 48.4% reported five or more drinks per session. About 60% reported ever using cannabis, 31.3% reported past-month cannabis use and 8.2% reported daily cannabis use.
1.2. Measures
Participants provided written informed consent and completed self-report measures in a group setting. The Substance Use Form assessed whether they had ever used alcohol/cannabis, usual frequency of alcohol/cannabis use in the past month, and usual quantity of alcohol consumed (on a 0-9 rating scale). The Rutgers Alcohol Problems Index (RAPI; White & Labouvie, 1989) assessed frequency of alcohol use problems. The RAPI demonstrated excellent internal consistency (α = .89) and scores ranged from 17 to 74 (M = 50.04, SD = 14.01). The Marijuana Problems Scale (MPS; Stephens, Roffman, & Curtin, 2000) evaluated negative social, occupational, physical, and personal consequences associated with cannabis use in the past 90 days. The MPS demonstrated excellent internal consistency (α = .86) and scores ranged from 0 to 17 (M = 1.83, SD = 3.38). The Discomfort Intolerance Scale (DIS; Schmidt, Richey, & Fitzpatrick, 2006) assessed ability to tolerate physical discomfort. The DIS demonstrated good internal consistency (α = .72) and scores ranged from 0 to 30 (M = 13.00, SD = 5.71). The Distress Tolerance Scale (DTS; Simons & Gaher, 2005) assessed ability to tolerate psychological distress. The DTS demonstrated excellent internal consistency (α = .93) and scores ranged from 17 to 74 (M = 8.63, SD = 8.14). The Beck Depression Inventory-II (BDI; Beck & Steer, 1987) assessed depressive symptoms. The BDI-II demonstrated excellent internal consistency (α = .92) and scores ranged from 0 to 48 (M = 8.63, SD = 8.14).
2. Results
Using a probability factor of .025 to control for Type I error, we found that depression was related to alcohol problems (r = .27, p < .01), cannabis problems (r = .26, p < .01), and distress intolerance (r = -.53, p < .01) but was unrelated to alcohol quantity, alcohol and cannabis frequency, and discomfort intolerance (r’s < .10, p’s > .025). Discomfort intolerance was related to decreased distress tolerance (r = -.16, p < .025) and decreased cannabis frequency (r = -.23, p < .01). Distress tolerance was related to decreased alcohol quantity (r = -.17, p < .025) and fewer alcohol (r = -.31, p < .01) and cannabis (r = -.18, p < .01) problems.
To test the moderational roles of distress and discomfort intolerance on the link between depression and alcohol use behaviors, hierarchical regressions were computed. Alcohol quantity, alcohol frequency, and alcohol problems were dependent variables and gender was entered as a covariate. Predictive variables were the main effects of distress intolerance or discomfort intolerance and BDI score and the interaction of distress/discomfort intolerance × BDI score. Variables were centered to reduce the multicollinearity. None of the moderation analyses were significant. To test moderation on the link between depression and cannabis use, additional hierarchical regressions were computed with cannabis use frequency and problems as dependent variables. Only discomfort intolerance moderated this relation (Table 1). The form of the interaction was examined (Cohen & Cohen, 1983). Unexpectedly, those with low discomfort intolerance and depression showed the greatest risk cannabis problems (see Figure 1). The mediational role of distress tolerance on the relationship between depression and cannabis and alcohol problems was tested (Kenny, Kashy, & Bolger, 1998). Distress tolerance mediated the relation between depression and both alcohol and cannabis problems (Table 2).
Table 1.
Individual Variable Contributions Predicting Cannabis Use Behaviors
| ΔR2 | t | β | f2 | p | |
|---|---|---|---|---|---|
| Dependent Variable: Cannabis Frequency | |||||
| Step 1: Covariates | .049 | <.05 | |||
| Gender | -3.19 | - .22 | .05 | ns | |
| Step 2: Main Effects | .012 | ns | |||
| Distress tolerance | -1.58 | - .13 | .00 | ns | |
| Depression | - .77 | - .06 | .00 | ns | |
| Step 3: Interaction Effect | .001 | ns | |||
| Distress tolerance X depression | - .50 | - .05 | .00 | ns | |
| Dependent Variable: Cannabis Frequency | |||||
| Step 1: Covariates | .050 | <.01 | |||
| Gender | -3.36 | - .22 | .05 | ns | |
| Step 2: Main Effects | .017 | ns | |||
| Discomfort tolerance | -1.90 | - .13 | .02 | ns | |
| Depression | .58 | .04 | .00 | ns | |
| Step 3: Interaction Effect | .004 | ns | |||
| Discomfort tolerance X | - .91 | - .06 | .00 | ns | |
| Dependent Variable: Cannabis-Related Problems | |||||
| Step 1: Covariates | .023 | <.05 | |||
| Gender | -2.17 | -.15 | .02 | <.05 | |
| Step 2: Main Effects | .057 | <.01 | |||
| Distress tolerance | -1.57 | -.13 | .01 | ns | |
| Depression | 1.82 | .15 | .01 | ns | |
| Step 3: Interaction Effect | .000 | ns | |||
| Distress tolerance X depression | .05 | .01 | .00 | ns | |
| Dependent Variable: Cannabis -Related Problems | |||||
| Step 1: Covariates | .024 | <.05 | |||
| Gender | -2.28 | - .15 | .02 | <.05 | |
| Step 2: Main Effects | .096 | <.001 | |||
| Discomfort tolerance | -1.54 | - .11 | .01 | ns | |
| Depression | 4.61 | .30 | .09 | <.001 | |
| Step 3: Interaction Effect | .022 | <.05 | |||
| Discomfort tolerance X | -2.34 | - .15 | .02 | <.05 | |
Note. Depression was measured using the Beck Depression Inventory (BDI), cannabis-related problems were measured with the Marijuana Problems Scale (MPS), discomfort intolerance was measured using the Discomfort Intolerance Scale (DIS) and distress tolerance was measured using the Distress Tolerance Scale (DTS). β = standardized beta weight provided for multiple regression.
*p < .05, ** p < .01.
Figure 1.
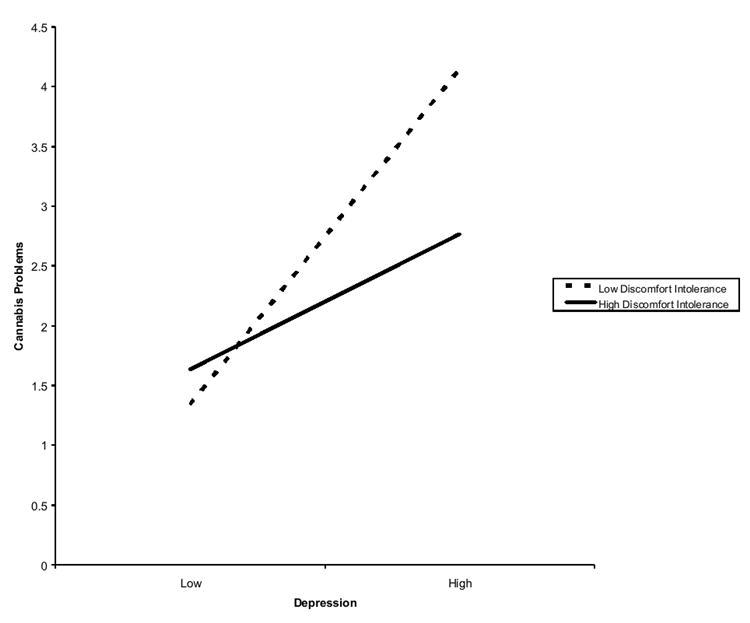
Moderation Effect of Discomfort Intolerance on the Relationship between Depression and Cannabis-Related Problems.
Table 2.
Regression Analyses Testing for Mediation: (1) Effect of Social Anxiety on Alcohol and Cannabis Problems, (2) Effect of Social Anxiety on Distress Tolerance, (3) Effect of Distress Intolerance on Alcohol and Cannabis Problems, (4) Effect of Social Anxiety on Alcohol and Cannabis Problems after Controlling for Distress Tolerance
| Dependent Variable | Independent Variable(s) | β | F |
|---|---|---|---|
| Alcohol Model | |||
| Alcohol-Related Problems | 1. Depression | .27 | 19.80** |
| Distress Tolerance | 2. Depression | -.54 | 79.23** |
| Alcohol-Related Problems | 3. Distress Tolerance | -.31 | 20.99** |
| Alcohol-Related Problems | 4. Depression
Distress Tolerance |
.06
-.32 |
.54
21.55** |
| Cannabis Model | |||
| Cannabis -Related Problems | 1. Depression | .26 | 18.42** |
| Distress Tolerance | 2. Depression | -.54 | 79.23** |
| Cannabis -Related Problems | 3. Distress Intolerance | -.18 | 6.87** |
| Cannabis -Related Problems | 4. Depression
Distress Tolerance |
.12
-.19 |
2.05
6.99** |
Note. Depression was measured using the Beck Depression Inventory-II (BDI-II), alcohol-related problems were measured using the Rutgers Alcohol Problems Index (RAPI), cannabis-related problems were measured with the Marijuana Problems Scale (MPS), and distress tolerance was measure using the Distress Tolerance Scale (DTS). β = standardized beta weight provided for multiple regression. Depression was separately regressed on each dependent variable in steps (1) and (2). Depression and distress were simultaneously regressed for each dependent variable in step (4).
*p < .05
p < .01
3. Discussion
The first goal of the present study was to investigate whether discomfort intolerance and distress intolerance were linked to problematic alcohol and cannabis use. Consistent with past work (e.g., Simons & Gaher, 2005), distress intolerance was related to alcohol and cannabis problems, increased alcohol quantity, and increased cannabis use frequency. Together, these data suggest that individuals with low distress tolerance use substances to regulate emotions which is cause for concern given that substance use to cope with negative emotions is related to high-risk substance behaviors (Carey, 1993; Turner et al., 1997). Importantly, distress tolerance mediated the links between depression and alcohol and cannabis use problems.
Discomfort intolerance moderated the link between depression and cannabis-related problems such that only those individuals with high capacity to tolerate physical discomfort were vulnerable to cannabis-related problems. Although unexpected, this novel result suggests that discomfort intolerance may serve a protective role in problematic cannabis use behaviors (yet less protective among depressed individuals). These data indicate that individuals less able to tolerate bodily sensations (such as those produced by cannabis) are less likely to use cannabis.
It is noteworthy that although distress and discomfort intolerance were related, the modest size of the association and the different correlates between them suggests these are two distinct constructs. Also the present study was the first known investigation of the relationships between depression and discomfort and distress intolerance. Depression was associated with distress intolerance, supporting the notion that individuals with depression experience impairment tolerating psychological (but not physical) distress. This study has some limitations that suggest future work. First, due to the cross-sectional nature of these analyses, causal inferences cannot be made. Second, self-report measures are subject to memory bias. Despite these limitations, the present study serves as an important step toward understanding the roles of discomfort and distress tolerance in problematic substance use behaviors.
Acknowledgments
This research was supported in part by a National Research Service Award from the National Institute of Drug Abuse (F31 DA12457-01) awarded to Julia D. Buckner.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Beck AT, Steer RA. Manual for the revised Beck Depression Inventory. San Antonio, TX: Psychological Corporation; 1987. [Google Scholar]
- Carey KB. Situational determinants of heavy drinking among college students. Journal of Counseling Psychology. 1993;40:217–220. [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum; 1983. [Google Scholar]
- Galen LW, Henderson MJ, Coovert MD. Alcohol expectancies and motives in a substance abusing male treatment sample. Drug and Alcohol Dependence. 2001;62:205–214. doi: 10.1016/s0376-8716(00)00168-x. [DOI] [PubMed] [Google Scholar]
- Grant BF. Comorbidity between DSM-IV drug use disorders and major depression: Results of a national survey of adults. Journal of Substance Abuse. 1995;7:481–497. doi: 10.1016/0899-3289(95)90017-9. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991-1992 and 2001-2002. Drug and Alcohol Dependence. 2004;11:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2003;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, Bolger N. Data analysis in social psychology. In: Gilbert DT, Fiske ST, Lindzey G, editors. The handbook of social psychology. 4. Vol. 1. New York: McGraw-Hill; 1998. pp. 233–265. [Google Scholar]
- Schafer J, Brown SA. Marijuana and cocaine effect expectancies and drug use patterns. Journal of Consulting and Clinical Psychology. 1991;59:558–565. doi: 10.1037//0022-006x.59.4.558. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Richey JA, Cromer KR, Buckner JD. Discomfort Intolerance: Evaluation of a Potential Risk Factor for Anxiety Pathology. Behavior Therapy. doi: 10.1016/j.beth.2006.08.004. in press. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Richey JA, Fitzpatrick KK. Discomfort intolerance: Development of a construct and measure relevant to panic disorder. Journal of Anxiety Disorders. 2006;20:263–280. doi: 10.1016/j.janxdis.2005.02.002. [DOI] [PubMed] [Google Scholar]
- Simons J, Gaher RM, Correia CJ, Hansen CL, Christopher MS. An affective-motivational model of marijuana and alcohol problems among college students. Psychology of Addictive Behaviors. 2005;19:326–334. doi: 10.1037/0893-164X.19.3.326. [DOI] [PubMed] [Google Scholar]
- Simons JS, Gaher RM. The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion. 2005;29:83–102. [Google Scholar]
- Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. Journal of Consulting and Clinical Psychology. 2000;68:898–908. [PubMed] [Google Scholar]
- Turner NE, Annis HM, Sklar SM. Measurement of antecedents to drug and alcohol use: Psychometric properties of the Inventory of Drug-Taking Situations (IDTS) Behaviour Research and Therapy. 1997;35:465–483. doi: 10.1016/s0005-7967(96)00119-2. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- Woolridge E, Barton S, Samuel J, Osorio J, Dougherty A, Hodcroft A. Cannabis use in HIV for pain and other medical symptoms. Journal of Pain and Symptom Management. 2005;29:358–367. doi: 10.1016/j.jpainsymman.2004.07.011. [DOI] [PubMed] [Google Scholar]


