Abstract
This study evaluated the effects of sectioning the scapholunate interosseous ligament, radioscaphocapitate ligament, and scaphotrapezial ligament on the kinematics of the scaphoid and lunate. Eight cadaver upper extremities were placed in a wrist joint simulator and moved in continuous cycles of flexion-extension and radial-ulnar deviation. Positional data of the scaphoid and lunate were obtained in the intact state, after the scapholunate ligament was cut; after the scapholunate and scaphotrapezial ligaments were cut; after the scapholunate, scaphotrapezial, and radioscaphocapitate ligaments were cut; and after all 3 ligaments were cut and the specimen was placed through an additional 1,000 cycles of flexion-extension. Cutting the scapholunate ligament caused changes in scaphoid and lunate motion during flexion-extension, but not radial-ulnar deviation. Additional sectioning of the scaphotrapezial ligament followed by the radioscaphocapitate ligament caused further kinematic changes in these carpal bones. One thousand cycles of motion after all 3 ligaments were sectioned caused additional kinematic changes in the scaphoid and lunate. The scapholunate ligament appears to be the primary stabilizer between the scaphoid and lunate. The radioscaphocapitate and scaphotrapezial ligaments are secondary restraints. Repetitive cyclic motion after ligament sectioning appears to have additional deleterious effects on carpal kinematics.
Keywords: Carpal instability, scaphoid, lunate, kinematics
Ligament injuries of the wrist are a common cause of wrist pain. A frequent site of injury is in the region of the scaphoid and lunate. Diagnosis and treatment of this condition are confusing and controversial. The anatomy in this area of the wrist is complex.
The region of the scaphoid and lunate is a confluence of several ligamentous structures. Meticulous anatomic dissections have defined their configuration. The scapholunate interosseous ligament (SLIL) connects the scaphoid and lunate.1 The radioscapho-capitate ligament (RSC) originates at the palmar radial cortex of the radius, inserts in the palmar cortex of the scaphoid, and continues on to terminate in the palmar cortex of the capitate.2,3 The scapho-trapezium ligament (ST) connects the distal pole of the scaphoid with the trapezium and trapezoid.4,5 Dorsally the dorsal intercarpal ligament and the dorsal radiocarpal ligament help to stabilize the wrist.6−9
Although the ligamentous anatomy has been described, the functional role of these structures in stabilizing the carpal bones remains incompletely understood. This results in confusion as to what structures should be repaired at the time of surgery. Because the etiology of scapholunate instability is unclear, treatment recommendations vary and the clinical outcome can be disappointing for many patients.10−16 An additional problem is that changes in 3-dimensional carpal bone positions may be too subtle to be seen on standard 2-dimensional x-rays. There may also be no positional changes of these carpal bones after ligament injury until forces are applied to the wrist, or the wrist is moving. This creates a problem in diagnosis because radiographs are the most commonly used noninvasive imaging technique to evaluate this condition.
The purpose of this study was to evaluate the stabilizing function of the SLIL, RSC, and ST ligaments on the scaphoid and lunate in a biomechanical cadaver experiment. Because changes in the motion of the scaphoid and lunate may be dependent on the order in which these ligaments are sectioned, one specific ligament sequence was examined in this study. These ligaments were chosen because of their attachment to either the scaphoid, lunate, or both. The primary aim was to study the effect of sequential sectioning of these ligaments on scaphoid and lunate motion during cyclic wrist flexion-extension and wrist radial-ulnar deviation. The additional effect of repetitive cyclic motion after sequential ligament sectioning was also evaluated. This was done to mimic the effect of continued use after ligament injury. The hypothesis of this study is that sectioning the SLIL alters scaphoid and lunate motion. It is theorized that further sectioning of the RSC and ST would not result in further carpal bone changes during wrist motion. Our third hypothesis was that cyclic motion after ligament sectioning results in additional changes to the motion of the scaphoid and lunate.
Methods
The methodology used in this experiment is a modification of the protocol used in studies published previously.9,17,18 Eight fresh-frozen cadaver right upper extremities were determined by fluoroscopy and arthroscopic examination to be free of traumatic and systemic defects that could potentially result in altered wrist biomechanics. Four specimens had degenerative tears of the triangular fibrocartilage complex and one specimen had a membranous tear of the lunotriquetral ligament. The age range of the specimens was 48 to 93 years with an average of 71 years; 5 specimens were from men and 3 from women. All specimens were amputated at midhumerus level. The skin, subcutaneous tissue, and muscle were excised. The tendons of the extensor carpi radialis longus, extensor carpi radialis brevis, extensor carpi ulnaris, flexor carpi radialis, flexor carpi ulnaris, and the abductor pollicus longus were left intact whereas the remaining tendons were removed. All capsular and retinacular structures were spared.
Polhemus Fastrak sensors (Polhemus, Colchester, VT) were indirectly attached to the scaphoid, lunate, and distal radius, and directly to the third metacarpal to measure each bone’s motion or position relative to an electromagnetic source. The sensor for the third metacarpal was screwed onto an acrylic platform attached to the distal aspect of the third metacarpal by nylon screws. The motion of the third metacarpal sensor relative to the fixed radius was defined as global wrist motion. The sensors for the scaphoid and lunate were mounted onto acrylic platforms that were glued onto pultruded carbon fiber rods that were inserted into 2.7-mm unicortical drill holes made in the dorsal nonarticular portion of the scaphoid and lunate. The holes were positioned so that there was no interference with dorsal capsular structures and so that the rods did not impinge with each other or bony or tendinous structures. The rods were grouted into the drill holes with polymethylmethacrylate.
After these 3 Fastrak sensors were attached, the specimen was placed in the wrist joint simulator,17 an apparatus that allows repetitive, reproducible cycles of motion in both flexion-extension and radialulnar deviation as well as complex motions such as circumduction by applying physiologic forces on both the wrist flexor and extensor tendons. To permit a smooth reversal of motion, each desired and actual cycle of wrist motion was sinusoidal.
The elbow was fixed in the simulator at 90° of flexion by multiple Steimann pins and the forearm was positioned in neutral pronation-supination. To prevent forearm rotation an acrylic fork was placed around the radius and ulna and a Delrin rod (Dupont, Wilmington, DE), inserted into the proximal radius, was tethered to the simulator. A rectangular acrylic platform was then passed between the radius and ulna at the level of the interosseous membrane and fastened to the proximal ulna so that it was perpendicular to the long axis of the ulna and parallel to the floor. The long axis of this platform determined the plane of flexion-extension of the wrist while the plane perpendicular to the platform defined the plane of radial-ulnar deviation. Two Fastrak electromagnetic sources were then attached to this platform. One source, mounted dorsally, was used with the sensor on the third metacarpal that monitored global wrist motion. The other source was mounted palmarly and was used with the scaphoid, lunate, and radial sensors.
The fourth Fastrak sensor was attached to a universal clamp and platform that was screwed into the volar cortex of the radius. This sensor was adjusted by using the Fastrak data so that this sensor was aligned with neutral wrist flexion-extension, neutral wrist radial-ulnar deviation, and neutral forearm pronation-supination. This sensor’s coordinate system was defined as the origin for the scaphoid, lunate, and third metacarpal sensors (Fig. 1).
Figure 1.
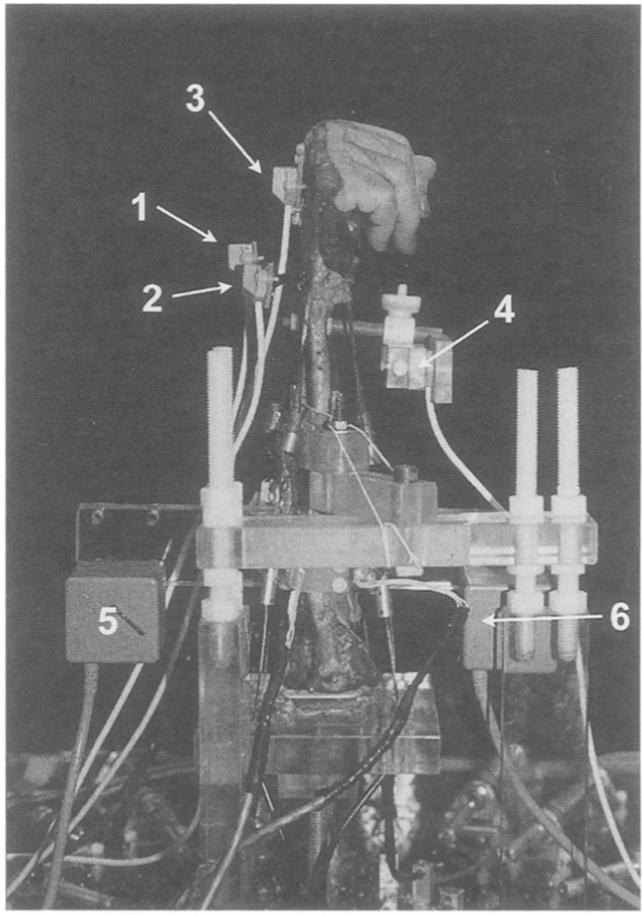
Experimental setup. Wrist joint motion simulator with Fastrak sensors mounted on scaphoid (1), lunate (2), third metacarpal (3), and distal radius (4). The Fastrak electromagnetic sources are mounted on the ulna dorsally (5) for use with the third metacarpal sensor and volarly (6) for use with the scaphoid, lunate, and radial sensors.
Static position data were collected for the scaphoid, lunate, distal radius, and third metacarpal in neutral wrist position in the simulator with load applied to the tendons. The wrist was then cyclically moved under computer control by the wrist simulator from 30° wrist extension to 30° wrist flexion for 6 consecutive cycles while force data from the simulator and positional data from the Fastrak sensors were collected. The specimen was then moved in a planar cyclic motion of 30° extension to 50° wrist flexion. Force and positional data were again collected. Data were also collected during a third cyclic motion from 10° radial deviation to 20° ulnar deviation. These motions were chosen because some cadaver wrists were occasionally incapable of further extremes of motion. Further wrist extension was sometimes limited by impingement of the rods on the dorsal rim of the radius.
After the data were recorded with the carpus intact, the SLIL, including the dorsal, palmar, and membranous portions of the ligament,1 were sectioned by placing a no. 11 blade through the radial midcarpal arthroscopy portal and sectioning the entire SLIL by palpation. Insertion of a hemostat through the portal and palpating the scapholunate joint helped to verify the completeness of the sectioning. At the conclusion of the experiment the specimen was dissected to verify completeness of ligament sectioning. This arthroscopy portal did perforate the margin of the dorsal radiocarpal ligament and was believed not to violate the integrity of the structure. Kinematic data were then collected for the scaphoid, lunate, distal radius, and third metacarpal in static neutral, and the 3 cyclic motions tested previously. The ST was then sectioned and kinematic data again recorded for the earlier-described motions. This ligament was identified during the anatomic dissection of the specimen and was the same ligament described by Drewniany et al.5 It was then marked with a surgical skin marker and at the appropriate time in the experiment cut with a scalpel under direct vision. The RSC was then sectioned and the same data were again recorded. The RSC was identified before the experiment by radiocarpal joint arthroscopy. The RSC ligament as described by Berger and Landsmeer2 was located. A suture was then placed around the ligament arthroscopically from within the joint and the 2 ends of the suture exited the volar capsule. At the time of RSC sectioning, cutting the tissue between the 2 limbs of the suture under direct vision from the volar aspect of the wrist severed the RSC between the radius and scaphoid without damaging adjacent ligaments. At the time of the anatomic dissection at the end of the experiment it appeared that the RSC ligament had an attachment to the scaphoid. After these 3 ligaments had been sectioned and data were recorded, the arm was moved through 1,000 cycles of a 30° flexion to 30° extension. The purpose of which was to mimic the condition of continued use after ligament injury. On conclusion of 1,000 cycles, the static and cyclic motion data were again recorded. During the entire experiment the specimen was kept moist by spraying normal saline onto the tissues at regular intervals.
At the end of the experiment the entire forearm was placed and secured in a foam box. Expandable polyurethane foam was injected into plastic bags surrounding the forearm to hold the wrist, forearm, and the 4 sensors and 2 sources in place while the forearm was scanned by computed tomography (CT) at 1-mm intervals with 1-mm slices. Fastrak data were recorded before and after the CT scans. This was done to determine the Fastrak sensor locations relative to the respective carpal bone into which each sensor platform was inserted, as well as the position of the sensors relative to the sources. In addition pre- and post-CT scan sensor data were compared to ensure that there was no movement during the CT scan. These data were combined to produce animations of the kinematic data.
The angular and positional data were analyzed in several different ways. The angular motion of the scaphoid and lunate were examined for each phase of the study by plotting their individual flexion-extension, radial-ulnar deviation, and supination-pronation against the primary wrist motion such as wrist flexion-extension or wrist radial-ulnar deviation. Additionally the motion of the wrist (3rd metacarpal) was plotted against time for each dynamic motion to ensure that the primary motion was repeatable between the intact and sectioned phases of the experiment, and to verify that there was minimal out-of-plane motion.
Three-dimensional surface-rendered models of the scaphoid, lunate, radius, and ulna were individually created by using Sliceomatic software (Tomovision, Montreal, Canada) based on the CT scan data. These models were then imported into 3D Studio Max (Discreet, Montreal, Canada) for rendering and animation. By using the kinematic data recorded in the wrist simulator during a motion, the models of the scaphoid and lunate were similarly moved in the animation software. These animations allowed us to view the 3-dimensional motion of the bones from any perspective.
Specific frames of motions were exported to Geomagic (Raindrop Geomagic, Research Park Triangle, NC), which converted the surface-rendered scaphoid and lunate into solid objects that could be viewed in computer-aided design software such as Solid Works (Solid Works, Concord, MA). In-house software, written in C++ and integrated into Solid Works, permitted us to determine the minimum distance between the scaphoid and lunate at any particular flexion-extension or radial-ulnar deviation position during a motion when the wrist was intact, or after sectioning of the various ligaments.
Finally, the specimen was dissected and the appropriate positioning of the posts and documentation of the intra-articular abnormalities seen at arthroscopy were verified. The completeness of ligament sectioning was also confirmed.
Changes in carpal bone motion owing to ligament sectioning were analyzed by using a 1-way repeated measures analysis of variance (Duncan’s method) at each degree of wrist flexion-extension or radial-ulnar deviation at p < .05. The power of this experiment was 90%.
Results
In the intact specimen during wrist flexion-extension the scaphoid followed the wrist’s flexion-extension movement, although to a lesser magnitude (Fig. 2). Thus, when the wrist flexed 40° the scaphoid flexed 31.5°. When the wrist extended 20° the scaphoid extended 16.2°. There was little out-of-plane movement of the scaphoid during wrist flexion-extension (Fig. 3). As the wrist flexed 40° the scaphoid ulnarly deviated 2.5°. There was minimal scaphoid pronation-supination during wrist flexion-extension.
Figure 2.
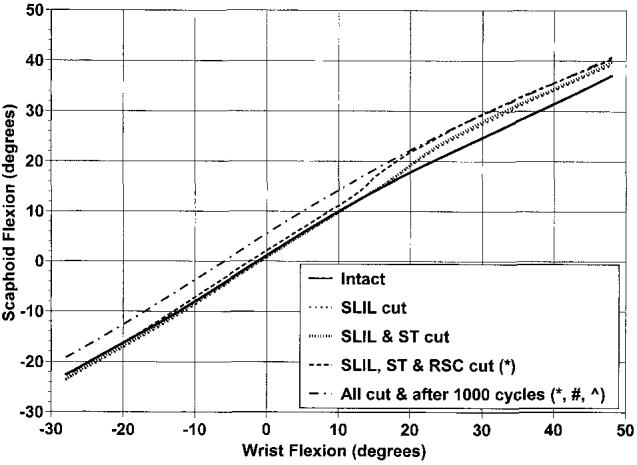
Average scaphoid flexion and extension as a function of wrist flexion and extension in the intact wrist and after sequential ligamentous sectioning. The graph represents the motion as the wrist moves from wrist extension to flexion. Flexion is positive. *Scaphoid position is statistically different from intact specimen as the specimen is moving from maximum flexion to neutral. #Scaphoid position is statistically different from the intact specimen as the wrist was going into and coming out of flexion. ^Scaphoid position is statistically different when compared with SLIL cut specimen when the wrist was going into and out of extension.
Figure 3.
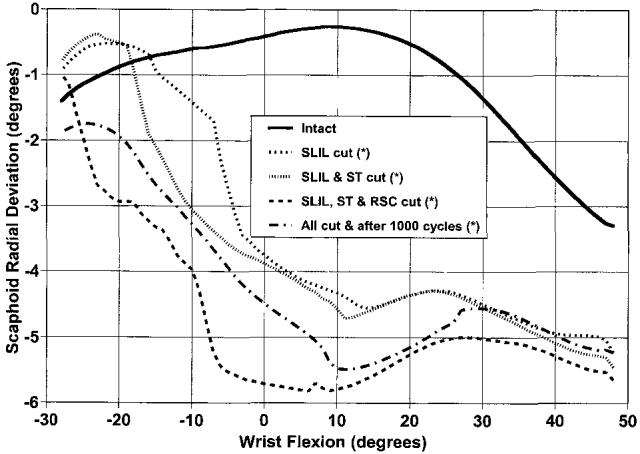
Average scaphoid radial and ulnar deviation as a function of wrist flexion and extension in the intact wrist and after sequential ligamentous sectioning. The graph represents the motion as the wrist moves from wrist flexion to extension. Flexion is positive, radial deviation is positive. *Scaphoid position is statistically different from intact specimen when the wrist is moving from flexion to extension.
In the intact specimen during wrist flexion-extension the lunate also flexed and extended in a linear fashion but to a lesser degree (Fig. 4). At 40° of wrist flexion the lunate flexed 20.4° and at 20° wrist extension the lunate had extended 9.6°. During wrist flexion-extension there was little motion of the lunate in the plane of radial-ulnar deviation (Fig. 5). Pronation-supination of the lunate during wrist flexion-extension was also minimal.
Figure 4.
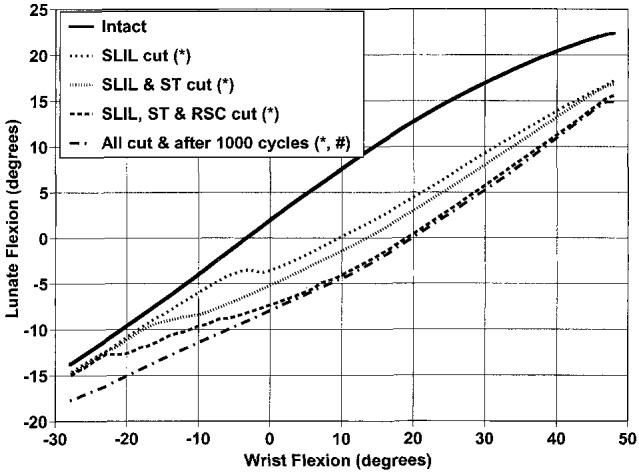
Average lunate flexion and extension as a function of wrist flexion and extension in the intact wrist and after sequential ligamentous sectioning. The graph represents the motion as the wrist moves from wrist flexion to extension. Flexion is positive. *Lunate position is statistically different from intact specimen during wrist flexion. #Lunate position is statistically different from intact specimen when the wrist is extended.
Figure 5.
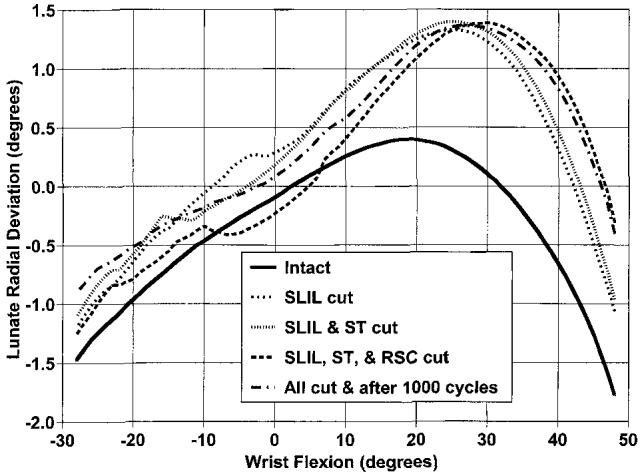
Average lunate radial and ulnar deviation as a function of wrist flexion and extension in the intact wrist and after sequential ligamentous sectioning. The graph represents the motion as the wrist moves from wrist flexion to extension. Flexion is positive, radial deviation is positive.
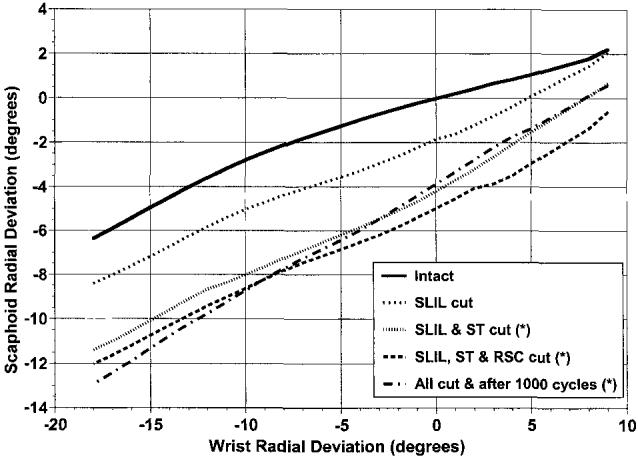
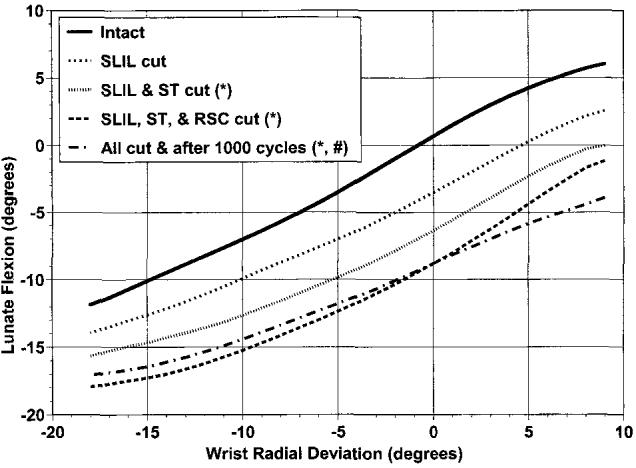
In the intact specimen during wrist radial-ulnar deviation the scaphoid flexed 5.5° during radial deviation of 9°, and extended 14.5° during ulnar deviation of 18° (Fig. 6). The scaphoid radially deviated 2.2° during wrist radial deviation and the scaphoid ulnarly deviated 6.4° during wrist ulnar deviation (Fig. 7). The lunate flexed and extended in a linear fashion as the wrist radially and ulnarly deviated (Fig. 8). When the wrist radially deviated 5° the lunate flexed 4.1° and when the wrist ulnarly deviated 15° the lunate extended 10.1°. During a wrist radial-ulnar deviation of 27° there was a total of 9.3° of lunate radial-ulnar deviation (Fig. 9).
Figure 6.
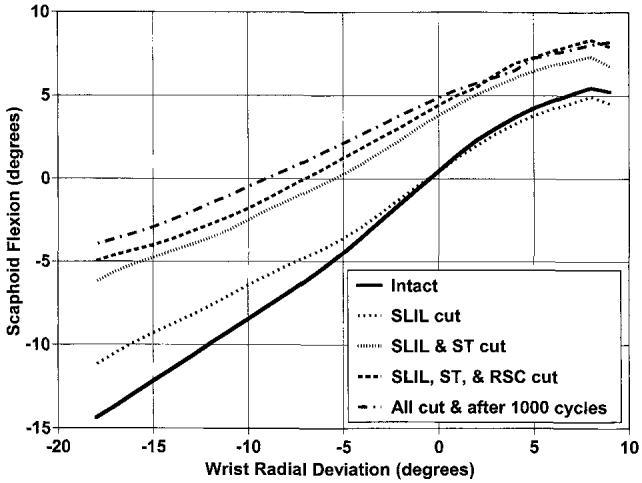
Average scaphoid flexion and extension as a function of wrist radial and ulnar deviation in the intact wrist and after sequential ligamentous sectioning. The graph represents the motion as the wrist moves from radial to ulnar deviation. Flexion is positive, radial deviation is positive.
Figure 7.
Average scaphoid radial and ulnar deviation as a function of wrist radial and ulnar deviation in the intact wrist and after sequential ligamentous sectioning. The graph represents the motion as the wrist moves from radial to ulnar deviation. Radial deviation is positive. *Scaphoid position is statistically different when compared with intact or SLIL-sectioned specimen as the wrist is going into ulnar deviation.
Figure 8.
Average lunate flexion and extension as a function of wrist radial and ulnar deviation in the intact wrist and after sequential ligamentous sectioning. The graph represents the motion as the wrist moves from radial to ulnar deviation. Flexion is positive, radial deviation is positive. *Lunate position is statistically different when compared with intact or SLIL-sectioned specimen throughout the entire radial-ulnar motion. #Further statistical difference when compared with the SLIL-sectioned specimen during nearly all of wrist radial and ulnar deviation.
Figure 9.
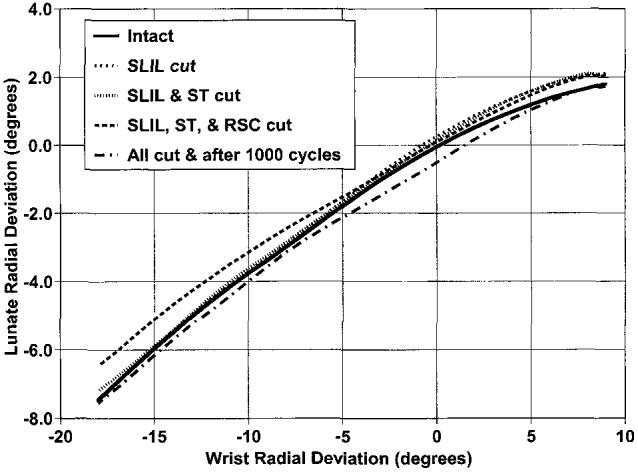
Average lunate radial and ulnar deviation as a function of wrist radial and ulnar deviation. The graph represents the motion as the wrist moves from radial to ulnar deviation. Radial deviation is positive.
A hysteresis effect of the carpal bones was identified in all times of wrist motion (Fig. 10). For example, the amount of scaphoid flexion at 5° of wrist radial deviation going into further radial deviation is different from the amount of the scaphoid flexion at 5° of wrist radial deviation going toward ulnar deviation. This hysteresis effect has been described in previous studies.9,18
Figure 10.
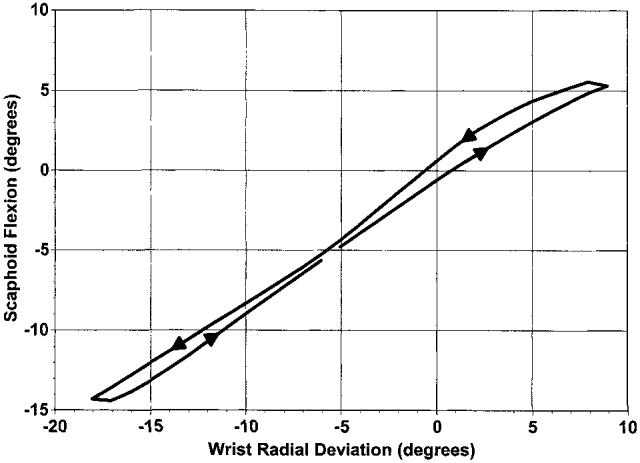
Average scaphoid flexion and extension as a function of wrist radial and ulnar deviation in the intact wrist. The direction of wrist motion is shown with the arrowhead.
During flexion and extension motion and radial and ulnar deviation motion, a number of statistically significant changes in carpal bone motion occurred after incremental sectioning of those ligaments attached to the scaphoid. Some of these changes were statistically significant even though the change was only on the order of 1°. Stated later are changes that were statistically significant and greater than 2° .
In the wrist flexion-extension motion, with sectioning of the SLIL, there was a statistically significant increase in scaphoid ulnar deviation, especially as the wrist was moving from wrist flexion to wrist extension (Fig. 3). Also after sectioning only the SLIL, there was a significant increase in lunate extension through nearly all of wrist flexion (Fig. 4). There were no further statistically significant increases in either scaphoid ulnar deviation or lunate extension as the ST and RSC were sectioned or after 1,000 cycles of motion were performed, except for an increase in lunate extension with the wrist in extension after all structures were sectioned and 1,000 cycles of motion.
During the wrist flexion-extension motion there was a significant increase in scaphoid flexion after all 3 ligaments were sectioned as compared with the intact wrist, as the wrist moved from maximum flexion to neutral. During wrist flexion-extension after all 3 ligaments were sectioned and 1,000 cycles of motion there was an increase in scaphoid flexion as the wrist was going into flexion (Fig. 2) and coming out of flexion compared with intact wrist. As the wrist was going into extension and coming out of extension there was an increase in scaphoid flexion after the SLIL, RSC, and ST ligaments were sectioned and 1,000 cycles of motion as compared with just the SLIL sectioned.
During wrist radial and ulnar deviation motion there were no statistically significant changes with scaphoid or lunate motion after only the SLIL was sectioned. After the SLIL and ST were sectioned there was an increase in scaphoid ulnar deviation (Fig. 7) as the wrist was going into ulnar deviation.
After the SLIL and ST were sectioned there was an increase in lunate extension (Fig. 8) through all of the radial-ulnar motion. After all 3 ligaments were sectioned, with or without 1,000 cycles of motion, there were no additional significant increases in scaphoid ulnar deviation. With all the structures sectioned and 1,000 cycles of motion there was a further increase in lunate extension during nearly all of wrist radial and ulnar deviation, as compared to that with only the SLIL sectioned (Fig. 8).
The minimum distance between the scaphoid and lunate was determined from the 3-dimensional models created from the kinematic data (Table 1). As the number of ligaments cut were increased there was a trend for an increase in the distance between the scaphoid and lunate. There was a statistical increase in this distance when the intact specimen (Fig. 11) was compared with the specimen in which all 3 ligaments were cut (Fig. 12) or when all the ligaments were cut and the specimen was cycled through 1,000 cycles of motion.
Table 1.
Minimum Distance Between Scaphoid and Lunate in Millimeters (SD)
| Wrist Position | Intact Wrist | SLIL Cut | SLIL and ST Cut | SLIL, ST, and RSC Cut | All Cut and 1,000 Cycles of Motion |
|---|---|---|---|---|---|
| Maximum flexion (50°) | 1.6 (0.8) | 2.2 (0.8) | 2.9 (1.8) | 3.0 (1.7) | 4.4 (3.8) |
| Maximum ulnar deviation (20°) | 1.2 (0.6) | 2.2 (2.6) | 4.3 (4.4) | 6.1 (4.5) | 4.8 (4.3) |
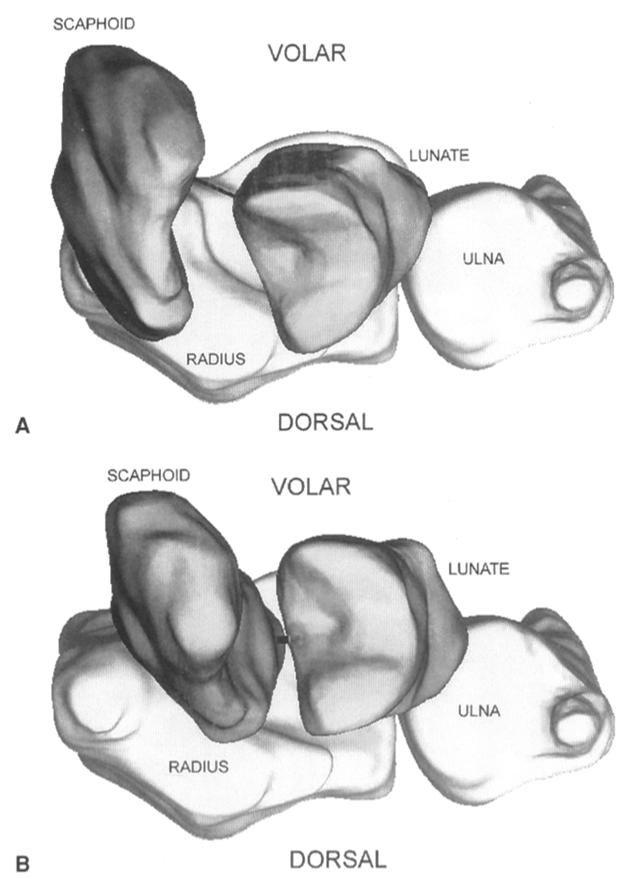
Figure 11.
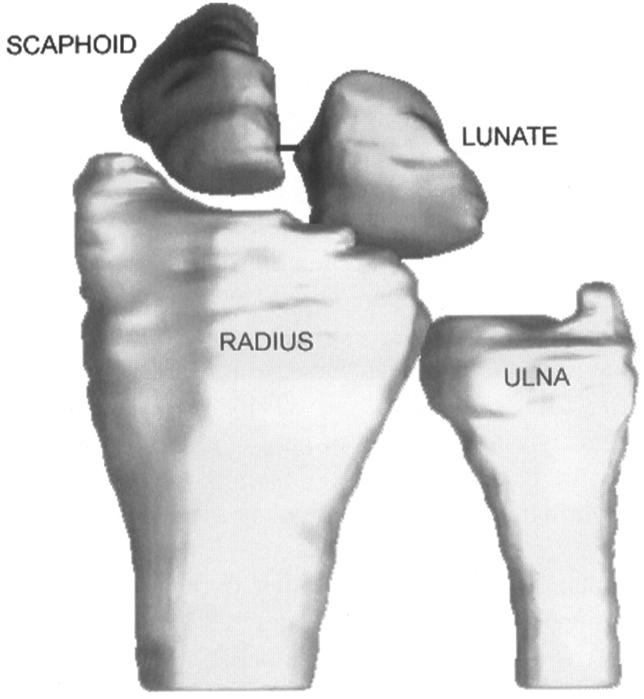
Dorsal view of the distal radius, ulna, scaphoid, and lunate for one intact wrist in 50° of flexion. The line connecting the scaphoid and lunate connects the points on the bones where the minimum distance (1.7 mm) of bones occurs. In some views part of the minimum distance line may be hidden by the scaphoid or lunate.
Figure 12.
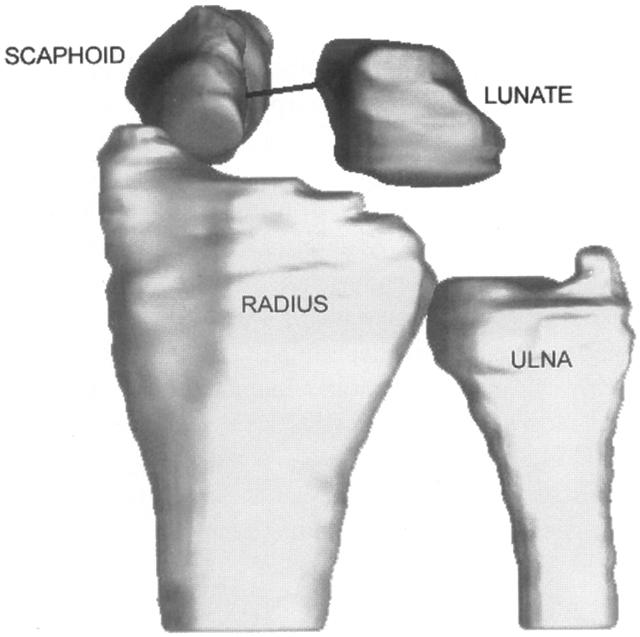
Dorsal view of the distal radius, ulna, scaphoid, and lunate after the SLIL, ST, and RSC ligaments have been sectioned. This is the same wrist as in Fig. 11 and is also in 50° of flexion. The line connecting the scaphoid and lunate indicates the minimum distance (6.0 mm) between the bones. In some views part of the minimum distance line may be hidden by the scaphoid or lunate.
The animations of the data were scrutinized. It was difficult to develop a method to analytically or statistically compare the movies. It was therefore decided to qualitatively analyze the images and determine if changes could be visualized. Changing the perspective and comparing motions of the scaphoid and lunate in the intact and sectioned specimens were enlightening and confirmed the changes in angular position of the carpal bones. Visualization of the scaphoid clunk after all 3 ligaments have been sectioned can be seen in 3-dimensional views of the carpus (Fig. 13). In neutral wrist flexion-extension, as the wrist is going from flexion into extension, the scaphoid had risen up onto the dorsal rim of the radius (Fig. 13A). As the wrist starts from maximum extension going toward neutral the scaphoid jumps back into the radioscaphoid fossa (Fig. 13B). A representative animation can be viewed at the Journal’s Web site, www.jhandsurg.org.
Figure 13.
Visualization of the scaphoid clunk after all 3 ligaments have been sectioned (A) Three-dimensional transverse view of one wrist in neutral wrist flexion-extension as the wrist is going from flexion into extension. The scaphoid has risen up onto the dorsal rim of the radius. The minimum distance between the bones is 3.8 mm as shown by the line connecting the bones. In some views part of the minimum distance line may be hidden by the scaphoid or lunate. (B) Three-dimensional transverse view of the same wrist but with the wrist in 20° of wrist extension as the wrist is moving from maximum extension toward neutral. Here the scaphoid has jumped back into the radioscaphoid fossa. The minimum distance between the bones is 1.0 mm as shown by the line connecting the bones.
Discussion
The purpose of this study was to determine the stabilizing functions of the SLIL, ST, and RSC ligaments on the scaphoid and lunate. These ligaments were chosen because of their proximity and attachments to the scaphoid and lunate, as well as the observation (made during surgery for treatment of carpal instability) that these ligaments have frequently been damaged. It is also necessary to more fully understand the contributions of these ligaments to wrist stability to better design and test suggested surgical repairs of scapholunate instability.
During the planar motion of wrist flexion-extension the scaphoid and lunate move predominantly in the plane of flexion-extension. During wrist flexion the scaphoid ulnarly deviates slightly. There was minimal scaphoid pronation-supination or lunate radial-ulnar deviation and pronation-supination during wrist flexion-extension. The scaphoid flexed and extended more than the lunate, but less than the wrist, during wrist flexion-extension. When the wrist was moved in the plane of radial-ulnar deviation the scaphoid and lunate both flexed and extended as well as radially and ulnarly deviated. Comparison of these results with those of our previous studies9,18 by using an identical methodology revealed similar results in the intact wrist. The only variances were that there was slightly less lunate ulnar deviation during wrist flexion and the scaphoid extended less during wrist extension in this present study.
Analysis of the ligament-sectioning data confirms the importance of the SLIL in stabilizing the scaphoid and lunate. Initial sectioning of this ligament caused scaphoid ulnar deviation and lunate extension during wrist flexion-extension. The results of the present study can also be compared with our previous biomechanical study that evaluated the SLIL with similar methodology. In the first study,18 SLIL sectioning resulted in increased scaphoid flexion, pronation, and lunate extension during wrist flexion-extension. The difference between the results of these 2 studies may be explained by the fact that a dorsal capsulotomy was performed and a pressure sensor was inserted in the first study. Subsequent studies by this research laboratory9 have shown that either sectioning the dorsal radial carpal ligament or inserting a pressure sensor into the joint alone affects carpal kinematics. Sectioning the ST ligament after the SLIL causes no further changes in scaphoid and lunate kinematics during wrist flexion-extension. This implies that the ST ligament is a relatively less important stabilizer than the SLIL ligament during wrist flexion-extension. Sectioning the SLIL ligament followed by the ST ligament and then the RSC ligament resulted in increased scaphoid flexion. This would suggest that either the RSC or the combination of the ST and RSC ligaments did contribute to scaphold stability after the SLIL ligament was damaged. Based on the order of sectioning it was not possible to determine if stability of the scaphoid was maintained if the SLIL ligament was intact and the ST and RSC ligaments were cut. The addition of 1,000 cycles of flexion-extension after ligament sectioning caused further destabilization of the scaphoid and lunate, but the reason was unclear. Dissection of the specimens at the end of the experiment revealed no further visible changes in any of the other (intact) ligaments. It is our hypothesis that after ligament sectioning forces across the wrist were transferred to the other intact ligaments. These increased forces may not have generated enough energy to cause rupture of the intact structures, but may instead have caused plastic deformation or weakening of their tensile properties, which may explain why these intact ligaments appeared normal but may have had decreased structural properties. Based on the anatomy of the remaining ligaments and the fact that the lunate’s position was altered we surmised that cyclic motion after ligament sectioning caused either a decrease in stiffness or a partial elongation of the dorsal radiocarpal, the short radial lunate, the long radial lunate, or some combination of these ligaments that produced further instability.
Scaphoid and lunate motion was unchanged during wrist radial-ulnar deviation after the SLIL ligament was sectioned. The SLIL ligament, therefore, seemed to have a different role in controlling scaphoid and lunate motions during wrist flexion-extension compared with wrist radial-ulnar deviation. After SLIL and ST sectioning there was an increase in scaphoid ulnar deviation and lunate extension during wrist radial-ulnar deviation, which would suggest that either the ST or the combination of ST and SLIL ligaments helped to support the scaphoid and lunate during this wrist motion. After all 3 ligaments were cut and the wrist was moved through 1,000 cycles there were further changes in lunate position. We are unsure of the cause but, again, believe that plastic deformation of remaining intact ligaments under repetitive loads contributes to further changes in carpal bone position.
It is difficult to analyze translational changes that occurred in a comparative and quantitative way. The gap between the scaphoid and lunate was thought to be a measure of carpal instability. In an attempt to quantify the translational data and make this information clinically useful, the minimum distances between the scaphoid and lunate were measured as the wrist was moving. There was a trend for this distance to increase as more ligaments were sectioned. There was a statistical difference between the minimum distance for the intact specimen compared with the specimen in which 3 ligaments were sectioned and 1,000 cycles of motion had occurred. We observed that this minimum distance was constantly changing with wrist motion, as were the locations on the scaphoid and lunate where the distance was determined. When the motion of these bones is viewed 3-dimensionally, it is frequently noticed that there may be a wide gap between the scaphoid and lunate when measured between 2 arbitrary dorsal points. In a simulated typical radiographic measurement (Fig. 14A) of the gap between the scaphoid and lunate in neutral flexion-extension, with the SLIL, ST, and RSC ligaments sectioned, a gap of 3.8 mm might be measured. When the motion of these bones is viewed 3-dimensionally from a transverse view (Fig. 14B), however, the gap between the scaphoid and lunate can be seen to be opening up and to be much larger. Another compounding problem in measuring this gap is whether the space measured by the clinician is the true minimum distance between the bones. The x-ray is a 2-dimensional portrayal of 3-dimensional objects. Because of the 2-dimensional projection of the bones and the perspective in which they are viewed, this gap measurement may be erroneous. It is certainly feasible, for example, for the clinician to believe to measure the minimum distance between the scaphoid and lunate on a plain x-ray and actually measure the distance between 2 nonarticular points on these bones (Fig. 15). The true distance between the scaphoid and lunate can only be measured from a 3-dimensional image; measuring the “scapholunate gap” on plain x-rays is not completely accurate.
Figure 14.
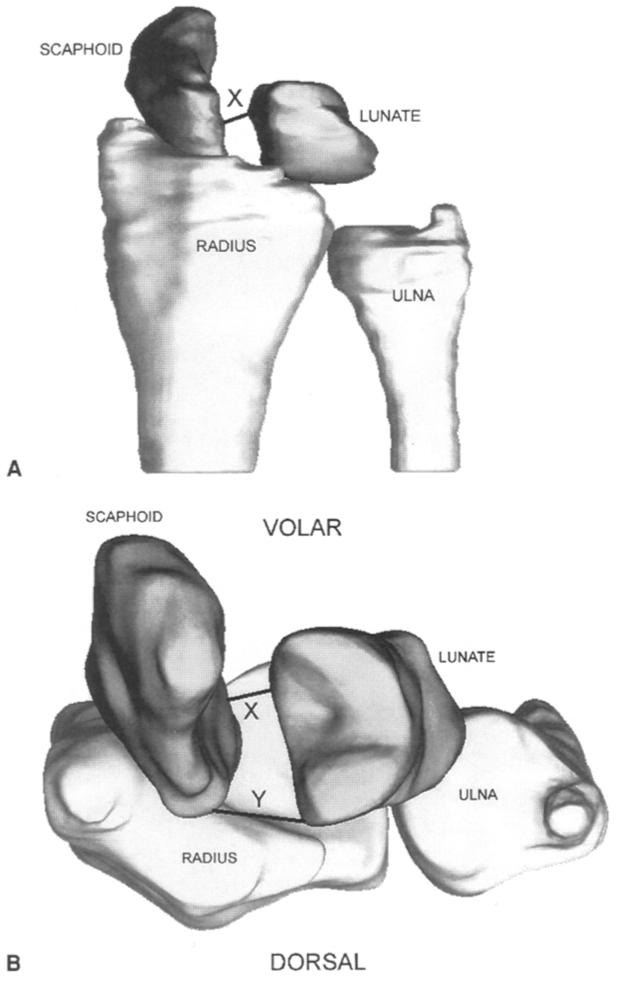
Variation in gap measurement between the scaphoid and lunate depends on where it is measured. (A) In a simulated typical radiographic measurement of the gap between the scaphoid and lunate in a wrist, in neutral flexion-extension, with the SLIL, ST, and RSC ligaments sectioned, a gap of 3.8 mm and labeled as “X,” would be measured. (B) When the motion of these bones is viewed 3-dimensionally from a transverse view, the gap between the scaphoid and lunate can be seen to be opening up, and is labeled as “Y.” In some views part of the minimum distance line may be hidden by the scaphoid or lunate. Therefore the calculated minimum distance between the bones may not completely represent changes in the scaphoid and lunate positions. Furthermore the gap measurement is dependent on which points are chosen on the scaphoid and lunate.
Figure 15.
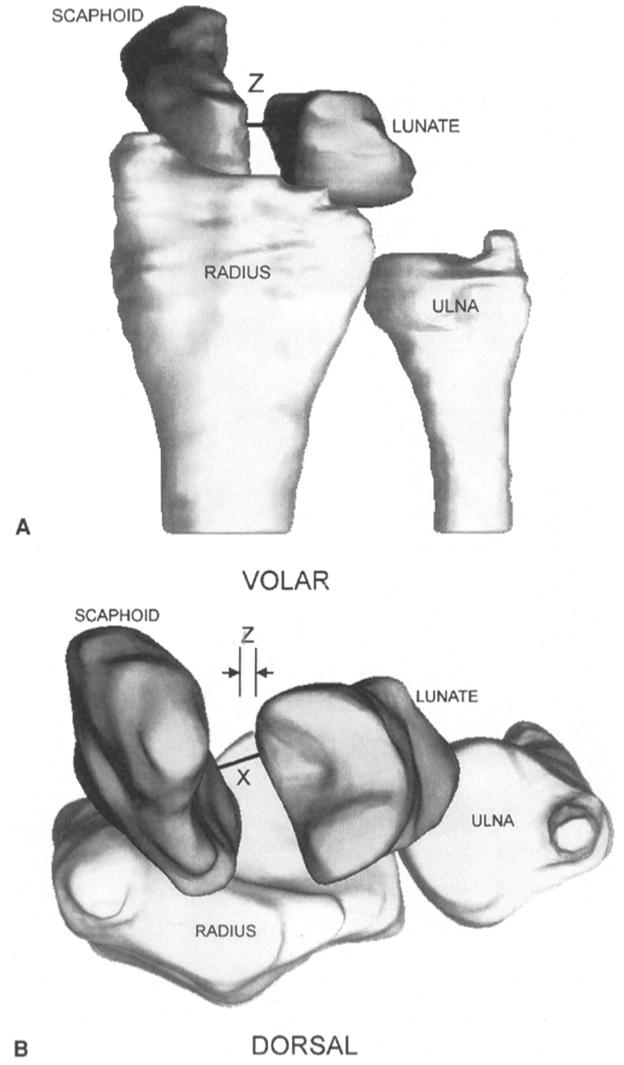
Effect of radiographic arm position on gap measurement between scaphoid and lunate. (A) An apparently small gap could be measured from a radiograph with the forearm slightly rotated so that the radiograph is not a true posteroanterior x-ray. (A and B) Here a simulated whole arm rotation of 10° would suggest a gap of 2.4 mm, labeled as “Z” on the figure, whereas the true minimum distance is 3.8 mm as seen in B as “X” and in Fig. 14A as “X.” In some views part of the minimum distance line may be hidden by the scaphoid or lunate.
It is difficult to analyze in a quantitative fashion the 3-dimensional animations created from the data in this study. Visualization of the scaphoid and lunate moving and the ability to view this from any perspective is an exceptional educational tool. This methodology has the ability to create movies that are stereoscopic and can be viewed with virtual reality or liquid crystal display shutter glasses (a video can be viewed at the Journal’s Web site, www.jhandsurg. org). The translation of the scaphoid during radialulnar wrist motion is well shown in these animations. During radial deviation the scaphoid and lunate flexion translates 3- to 4-mm ulnarward on the radius. During ulnar deviation the opposite occurs.
After SLIL, ST, and RSC ligament sectioning a snapping or subluxation of the scaphoid as the wrist moved in flexion-extension was noted in several specimens. Analysis of the angular and translational data was less helpful in explaining this phenomenon. Repetitive viewing of the animation from several perspectives allowed us to reach an explanation. As the wrist flexed the scaphoid also flexed and translated dorsally over the dorsal rim of the radius, which resulted in subluxation of the scaphoid. As the wrist then extended the proximal pole of the scaphoid became impinged against the dorsal rim of the scaphoid and could not extend further. With additional wrist extension, the scaphoid suddenly translated volarly and reduced into its proper position in the scaphoid fossa of the radius with a snap. The scaphoid then continued to extend with the wrist and lunate. In our judgment this represents an example of dynamic scapholunate instability as described by Watson et al19 (this video can be seen on the Journal’s Web site, www.jhandsurg.org). In the laboratory, 3-dimensional animations of the carpal bones can be viewed from any perspective.
The disadvantages of this biomechanical study are similar to all such cadaver studies. We have tried to eliminate specimens that have pre-existing ligament injuries. Data collection on each specimen was completed within a day to prevent deterioration of the soft tissues. The wrist joint simulator applies loads in a physiologic range. Unfortunately the specific loads in the living subject are not completely known and probably vary from one patient to the next. Loads applied by the simulator are an estimation of the in vivo situation and within physiologic range and capabilities. We believe that the simulator is the best available device that allows data collection on carpal bone motion while the wrist is moving in a repeatable cyclic fashion. Different orders of ligament sectioning will be studied to assess any sequence-dependent effects of ligament sectioning on carpal bone motion. We believe that there is very valuable information that can be obtained from the portrayal of the data as animations or movies, which has not yet been fully evaluated.
This biomechanical investigation supports the hypothesis that the SLIL ligament is a major stabilizer of the scaphoid and lunate, and that the RSC and ST ligaments are secondary restraints. We are unable to determine from these data whether there would be different results if their sectioning sequence were different, but the function of these ligaments seems to change depending on how the wrist is moving. Cyclic motion after ligament sectioning has a further detrimental effect on carpal stability.
Acknowledgments
The authors would like to express their appreciation to David Barnwell and Ann Scaramuzzino, Department of Radiology, for their assistance in performing the computed tomography scans of each forearm.
Supported by Extramural Research from the National Center for Injury Prevention and Control grant number R49/CCR216814-03 from the Centers for Disease Control and Prevention. Contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention.
Footnotes
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1.Berger RA. The gross and histologic anatomy of the scapholunate interosseous ligament. J Hand Surg. 1996;21A:170–178. doi: 10.1016/S0363-5023(96)80096-7. [DOI] [PubMed] [Google Scholar]
- 2.Berger RA, Landsmeer JMF. The palmar radiocarpal ligaments: a study of adult and fetal human wrist joints. J Hand Surg. 1990;15A:847–854. doi: 10.1016/0363-5023(90)90002-9. [DOI] [PubMed] [Google Scholar]
- 3.Berger RA. The ligaments of the wrist. A current overview of anatomy with considerations of their potential functions. Hand Clin. 1997;13:63–82. [PubMed] [Google Scholar]
- 4.Moritomo H, Viegas SF, Nakamura K, DaSilva MF, Patterson RM. The scaphotrapezio-trapezoidal joint. Part 1: an anatomic and radiographic study. J Hand Surg. 2000;25A:899–910. doi: 10.1053/jhsu.2000.4582. [DOI] [PubMed] [Google Scholar]
- 5.Drewniany JJ, Palmer AK, Flatt AE. The scaphotrapezial ligament complex: an anatomic and biomechanical study. J Hand Surg. 1985;10A:492–498. doi: 10.1016/s0363-5023(85)80070-8. [DOI] [PubMed] [Google Scholar]
- 6.Viegas SF. The dorsal ligaments of the wrist. Hand Clin. 2001;17:65–75. [PubMed] [Google Scholar]
- 7.Viegas SF, Yamaguchi S, Boyd NL, Patterson RM. The dorsal ligaments of the wrist: anatomy, mechanical properties, and function. J Hand Surg. 1999;24A:456–468. doi: 10.1053/jhsu.1999.0456. [DOI] [PubMed] [Google Scholar]
- 8.Viegas SF, Patterson RM, Ward K. Extrinsic wrist ligaments in the pathomechanics of ulnar translation instability. J Hand Surg. 1995;20A:312–318. doi: 10.1016/S0363-5023(05)80032-2. [DOI] [PubMed] [Google Scholar]
- 9.Short WH, Werner FW, Green JK, Weiner MM, Masaoka S. The effect of sectioning the dorsal radiocarpal ligament and insertion of a pressure sensor into the radiocarpal joint on scaphoid and lunate kinematics. J Hand Surg. 2002;27A:68–76. doi: 10.1053/jhsu.2002.30074. [DOI] [PubMed] [Google Scholar]
- 10.Lavernia CJ, Cohen MS, Taleisnik J. Treatment of scapholunate dissociation by ligamentous repair and capsulodesis. J Hand Surg. 1992;17A:354–359. doi: 10.1016/0363-5023(92)90419-p. [DOI] [PubMed] [Google Scholar]
- 11.Blatt G. Capsulodesis in reconstructive hand surgery. Dorsal capsulodesis for the unstable scaphoid and volar capsulodesis following excision of the distal ulna. Hand Clin. 1987;3:81–102. [PubMed] [Google Scholar]
- 12.Weiss A-PC. Scapholunate ligament reconstruction using a bone-retinaculum-bone autograft. J Hand Surg. 1998;23A:205–215. doi: 10.1016/S0363-5023(98)80115-9. [DOI] [PubMed] [Google Scholar]
- 13.Watson HK, Weinzweig J, Guidera PM, Zeppieri J, Ashmead D. One thousand intercarpal arthrodeses. J Hand Surg. 1999;24B:307–315. doi: 10.1054/jhsb.1999.0066. [DOI] [PubMed] [Google Scholar]
- 14.Kleinman WB, Carroll C., IV Scapho-trapezio-trapezoid arthrodesis for treatment of chronic static and dynamic scapho-lunate instability: a 10-year perspective on pitfalls and complications. J Hand Surg. 1990;15A:408–414. doi: 10.1016/0363-5023(90)90051-r. [DOI] [PubMed] [Google Scholar]
- 15.Wyrick JD, Youse BD, Kiefhaber TR. Scapholunate ligament repair and capsulodesis for the treatment of static scapholunate dissociation. J Hand Surg. 1998;23B:776–780. doi: 10.1016/s0266-7681(98)80095-8. [DOI] [PubMed] [Google Scholar]
- 16.Wyrick JD, Stern PJ, Kiefhaber TR. Motion-preserving procedures in the treatment of scapholunate advanced collapse wrist: proximal row carpectomy versus four-corner arthrodesis. J Hand Surg. 1995;20A:965–970. doi: 10.1016/S0363-5023(05)80144-3. [DOI] [PubMed] [Google Scholar]
- 17.Werner FW, Palmer AK, Somerset JH, Tong JJ, Gillison DB, Fortino MD, et al. Wrist joint motion simulator. J Orthop Res. 1996;14:639–646. doi: 10.1002/jor.1100140420. [DOI] [PubMed] [Google Scholar]
- 18.Short WH, Werner FW, Fortino MD, Palmer AK, Mann KA. A dynamic biomechanical study of scapholunate ligament sectioning. J Hand Surg. 1995;20A:986–999. doi: 10.1016/S0363-5023(05)80147-9. [DOI] [PubMed] [Google Scholar]
- 19.Watson HK, Weinzweig J, Zeppieri J. The natural progression of scaphoid instability. Hand Clin. 1997;13:39–49. [PubMed] [Google Scholar]


