Abstract
Sexual assault and rape routinely produce extreme distress and negative psychological reactions in victims. Further, past research suggests that victims are at increased risk of developing substance use or abuse post-rape in efforts to ameliorate post assault distress. The post-rape forensic medical exam may itself exacerbate peritraumatic distress because it includes cues that may serve as reminders of the assault, thereby potentiating post-assault negative sequelae. To address this problem, a two-part video intervention was developed to take advantage of the existing sexual assault forensic exam infrastructure, and to specifically (a) minimize anxiety/discomfort during forensic examinations, thereby reducing risk of future emotional problems, and (b) prevent increased substance use and abuse following sexual assault. Updated findings with a sample of 268 sexual assault victims participating in the forensic medical exam and completing one or more follow-up assessments at: (1) < 3 months post-assault; (2) 3 to 6 months post-assault; or (3) 6 months or longer post-assault indicated that the video was associated with significantly lower frequency of marijuana use at each time point, among women who reported use prior to the assault.
Keywords: Sexual Assault, Rape, Intervention, Marijuana, Drug
1. Introduction
Rape and sexual assault affects over 15 million women (12.6%) in the US (Kilpatrick et al., 1992; Resnick et al., 1993; Tjaden & Thoennes, 1998), and increases risk of drug, alcohol, and nicotine use and abuse in its victims (Steketee & Foa, 1987; Resick, 1993; Kilpatrick et al., 2000; 2003). Consequently, early interventions that could accelerate recovery or otherwise reduce risk of substance abuse and other negative outcomes following sexual assault would be of considerable value to individuals and society. Since sexual assault victims who report the crime to police or other authorities receive routine post-rape medical care (Ledray & Kraft, 2001), the medical setting could provide the infrastructure in which secondary prevention services targeting substance use and potential mental health difficulties could be addressed.
Drug Use and Abuse Following Sexual Assault
Several studies demonstrate that raped or sexually assaulted women and adolescents display substantial increases in drug, alcohol, and nicotine use and abuse (Burnam et al., 1988; Kilpatrick et al., 2000; 2003; Miller, Downs, Gondali, & Keil, 1987; Miranda et al., 2002; Polusny & Follette, 1995; Rheingold et al., 2004; Simpson & Miller, 2002). Prospective data from the National Women's Study (Kilpatrick, et al., 1997) demonstrate that rape and physical assault increase risk of alcohol and drug abuse in previously non-abusing women. In addition, drug use appears to then increase subsequent risk of further assault (Kilpatrick et al., 1997). Thus the relationship between substance use and assault may be bidirectional, such that use may increase vulnerability to assault and substance use may also be employed to reduce post-assault distress (for a review see Testa & Parks, 1996).
Prospective longitudinal studies of those experiencing a recent traumatic event such as sexual assault need to control for prior rape or other assault history and pre-assault use patterns when examining use or abuse following a new assault incident. It may also be important to evaluate potential associations between race and use of specific substances when conducting longitudinal research. Different patterns of use have been previously reported among White and Black populations with Black participants in epidemiological studies reporting lower prevalence of alcohol and drug use (Kilpatrick et al., 1987). In our previous report with a subset of the sample described here, we found that minority participants were less likely to report post-rape use or abuse of alcohol but not drug use or abuse (Acierno et al., 2003).
Given the link between history of sexual assault and risk for drug and alcohol use and abuse, empirically supported early interventions aimed at decreasing such outcomes would be beneficial. Mixed findings have been obtained from studies of early interventions targeting mental health problems including posttraumatic stress disorder (PTSD) following assault or other traumatic events. There is more support for multiple-session interventions anchored in cognitive and behavioral principles. Some studies demonstrate that such interventions lead to greater improvement in functioning and decreased levels of PTSD and depression as compared to supportive counseling, with differences persisting through six month follow-up (Bryant et al., 1998; 1999). Other studies with samples of sexual and physical assault victims have found that such multi-session early interventions based in cognitive behavioral principles show efficacy relative to supportive counseling in the short term but have not shown clear long term benefits (Foa et al., 1995; Foa et al., 2006).
Brief Interventions That Target Substance Abuse
There is empirical support for using brief intervention strategies for substance abuse (e.g., Moyer et al., 2002; Stephens et al., 2000). Such approaches appear efficacious when delivered in an emergency department setting with older adolescents (Monti et al., 1999) and adult victims of accident or assault (Zatzick et al., 2004). For example, Zatzick et al. implemented a Motivational Interviewing treatment (MI) targeting alcohol abuse at the hospital trauma ward among those who screened positive for alcohol use and who were randomly assigned to treatment. Booster sessions and case management were conducted over the course of follow-up, while additional treatment targeting PTSD was offered to patients who demonstrated PTSD at three months post-injury. Results indicated that patients assigned to treatment vs. standard care were less symptomatic in terms of PTSD and were significantly less likely to meet criteria for alcohol abuse during a one year follow-up. Thus, brief intervention for substance use/abuse prevention in the aftermath of a traumatic event appears to be a promising strategy.
Video-Based Interventions
The use of educational videos has a precedent in health care settings (Gagliano, 1988) but has not been evaluated in the medical setting as an intervention to promote coping by recent assault or other trauma victims. In a recent review of studies implementing video instruction, Krouse (2001) found three main uses of videos in health care settings: to provide education about treatment options; to reduce anxiety and increase coping skills; and to teach self-care procedures. Krouse's review generally concluded that whereas videos have been effective at increasing knowledge about treatment options and at decreasing acute anxiety, the effects of videos on long-term behavior change were not as consistent. However, some studies found supporting evidence of knowledge and behavior change following a video intervention (e.g., Avis et al., 2004). Therefore, this modality of intervention has potential usages for sexual assault survivors who receive acute care in the medical setting post-assault, particularly if aimed at decreasing anxiety and increasing knowledge about medical procedures, such as the forensic medical exam.
This paper describes results of an intervention for sexual assault victims designed to be offered in the aftermath of the assault, within the health care setting immediately preceding the forensic medical exam. The intervention is delivered in video format, and considers findings reviewed above regarding the potential benefits of cognitive behavioral strategies including instruction in (1) in vivo exposure, (2) reducing behavioral avoidance, and (3) methods to limit substance use and abuse. In 2003, pilot data were reported in this Journal from an initial efficacy study of 124 sexual assault victims seen for a post-assault forensic medical exam who were randomly assigned to the video intervention or standard care. As previously reported, those receiving the treatment were significantly less likely to meet criteria for marijuana abuse than those receiving standard care at 6 weeks post-assault (Acierno et al., 2003). Other descriptive findings, consistent with literature cited above, indicated that alcohol use and abuse were less prevalent among minority participants, marijuana use was more prevalent among those reporting prior history of assault, and use of each substance including hard drugs was more prevalent among those reporting use within the 6 weeks prior to sexual assault. Finally, nested analyses indicated that the intervention was not significantly associated with substance use outcomes after controlling for other predictors.
The current report describes updated findings with the completed study sample of 268 participants. This paper extends previous findings using a larger sample as well as longer term follow-up periods through six months post-assault. The current report examines frequency of recent use of alcohol, marijuana, and hard drugs as well as abuse using multi-variable analyses to evaluate the potential impact of the intervention controlling for other factors. A final difference between this and the previous report is that the current report includes participants from a second dismantling phase of the study who were exposed to either the first half of the video intervention, entitled Medical Exam Preparation (ME), or to the second half entitled Psychoeducation (PE), as well as those exposed to the Full Video (FV) or Nonvideo (NV) (Standard Care) Conditions (as in the previous report). The goal of this dismantling phase was to examine whether there were unique and/or interactive effects of specific content designed to prepare women for the medical exam and reduce potential exam related anxiety versus content presenting strategies to cope directly with symptoms including drug and alcohol use that might occur post-sexual assault. Unfortunately, due to limited sample sizes in the two dismantling conditions the analyses reported here focused on comparison of those who were in Any Video (AV) condition vs. Nonvideo (NV) over the course of the full study period.
We hypothesized that participants exposed to AV would report lower post-rape frequency of alcohol, marijuana, and hard drug use and would be less likely to meet criteria for current drug and alcohol abuse at each assessment than participants in the NV condition. As in our previous report we also evaluated potential associations between race, prior assault history, and recent pre-rape use with post-rape use and abuse patterns and assessed whether such factors might moderate effects of the intervention.
2. Method
2.1. Participants
Eligible participants were adolescent girls and women age 141 years or older who were victims of sexual assault within the previous 72 hours and who participated in a post-sexual assault forensic medical exam designed to treat medical concerns and to gather evidence related to nonconsensual sexual assault. All participants were recruited when they presented for forensic examinations at a Southeastern academic medical center. Individuals who could not provide informed consent to participate in the study (e.g., those with mental retardation, extreme intoxication) were considered ineligible. Of 592 eligible victims, 442 (74.7%) agreed to participate. Of those who agreed to participate, 159 (36%) were in the NV condition and 283 were assigned to one of the 3 video conditions (AV). Of those assigned to AV, 247 (87%) watched more than half of the content which was the criterion for having received treatment. There was no difference across video conditions in terms of percentage watching the video. Thus, the final participating sample size was 406. Of this group of 406 participants at the time of the forensic examination, 268 (66%) completed at least one follow-up assessment. The majority of sexual assault victims completing follow-up assessment (92.5%) reported vaginal, anal, or oral penetration as part of the assault. The remaining 7.5% consisted of incidents of molestation, attempted rape, or suspected rape (e.g., drug facilitated rape).
There were no differences among follow-up completers and noncompleters in terms of treatment condition, race, age or marital status assessed at the time of the medical exam. Demographic characteristics are displayed in Table 1. For the analyses in this paper, participants who reported that they were Hispanic, Black, Asian, or Native American were classified as minority race/ethnicity.
Table 1.
Demographics of the Standard Care and Video Groups
| Demographic | NonVideo (N =107) | Any Video (N = 161) |
|---|---|---|
| Mean Age (and SD) | 26.49 (10.40) | 25.93 (10.24) |
|
| ||
| Race | ||
| White | 59.8% | 57.1% |
| Black | 36.4% | 38.5% |
| Asian | .9% | 1.9% |
| Hispanic | .9% | 1.9% |
| Native American | 1.9% | .6% |
|
| ||
| Marital Status | ||
| Single | 83.8% | 80.1% |
| Divorced or Separated | 9.5% | 7.7% |
| Widowed | 1.9% | 1.9% |
| Married/Cohabiting | 4.8 | 10.3% |
In terms of specific follow-up time frames: 216 participants completed Time 1, which occurred within 3 months post-sexual assault (M = 48.94, SD = 11.14); 1332 participants completed Time 2 assessment between 3 and 6 months post-sexual assault (M = 104.83, SD = 19.55); and 219 participants completed Time 3 assessment at 6 months or more post-sexual assault (M = 196.37, SD = 79.27). The breakdown by condition at Time 1 was as follows: 83 participants were in the NV group (38.4%); 133 (61.6%) were in the AV group. At Time 2: 47 (35.3%) were in the NV group and 86 (64.7%) were in the AV group. At Time 3: 93 (42.5%) were in the NV group and 126 (57.5%) were in the AV group.
2.2. Intervention conditions
2.2.1. Nonvideo condition (NV)
Standard services, referred to as NV, involved accompaniment at the examination by a rape crisis counselor and completion of a forensic sexual assault examination performed by a nurse or physician.
2.2.2. Full Video intervention (FV)
This condition was identical to the standard services condition in all aspects save the presentation of a 17-min video immediately preceding the exam. The video comprised two components. The first was specifically designed to reduce distress during forensic medical examinations by describing key aspects of the examination, while the second contained information that could be used by victims to prevent future emotional problems and substance abuse, such as instructions for proper implementation of self directed exposure exercises, methods to recognize and terminate inappropriate avoidance, and strategies to engage in activities that specifically do not involve alcohol or drug use and to avoid situations or cues that have been triggers for use.
2.2.3. Medical Exam Preparation (ME)
This condition was identical to the standard services condition in all aspects except for the 7 minute 40 second component of the video that contained information relevant to the medical exam only, as described above.
2.2.4. Psyhoeducation and Instruction (PE)
This condition was identical to the standard services condition in all aspects except for the approximately ten minute component of the video that contained information relevant to education about potential reactions following sexual assault and constructive strategies for reducing anxiety and substance use and abuse as described above.
2.3. Measures
A structured clinical interview entitled the Sexual Assault Interview was developed for this study. The substance abuse section was based on DSM-IV criteria for alcohol and drug abuse. The substance abuse and assault history and characteristics sections were developed and evaluated in prior epidemiological studies (Kilpatrick et al., 1997; 2000). The interview was used to collect data regarding lifetime victimization, lifetime and recent substance use, and lifetime and recent substance abuse. Interviewers were blind to intervention condition. The following variables were collected: Lifetime sexual or physical assault included incidents of previous vaginal, anal, or digital rape or physical attacks by someone who intended to seriously injure or kill the participant. Minority status was defined as being non-White versus White.
Potentially problematic substance use was operationalized differently for each substance so as to consider legal and normative realities. Lifetime Potentially Problematic Alcohol Use was defined as consuming four or more 1-oz drinks in a day. Pre-assault Potentially problematic Alcohol Use was defined as consuming four or more 1-oz drinks in a day in the 6 weeks before the index sexual assault. Lifetime Potentially Problematic Marijuana Use was defined as self-report of using marijuana on at least four occasions. Similarly, Lifetime Potentially Problematic Hard Drug Use was defined as self-reported use of cocaine, LSD, PCP, heroin, angel dust, ecstasy, nonprescription tranquilizers, etc., on at least four occasions. Both Pre-Assault Potentially Problematic Marijuana Use and Hard Drug Use were defined as any use of marijuana or hard drugs, respectively in the 6 weeks before the index sexual assault. Frequency of current alcohol, marijuana, and hard drug use was defined as number of days in which the specific substance was consumed based on self-report of use during the previous 2 weeks via the Time-Line Follow-back (TLFB) method (Sobell & Sobell, 1978). The TLFB uses a calendar method to gather retrospective information on substance use for a specified time interval, and has good reliability and validity for substance use frequency (Fals-Stewart, O'Farrell, Freitas, McFarlin, & Rutigliano, 2000). Alcohol, Marijuana, and Hard Drug Abuse were defined according to DSM-IV criteria for substance abuse and diagnosed via structured clinical interview. The time frame for assessment of post-assault abuse was based on the period since the assault at initial assessment and since the previous interview at subsequent assessments.
2.4. Procedures
Women presenting at the hospital for a post-sexual assault forensic examination were assessed in terms of their ability to give informed consent to participate in the project by medical students trained specifically for that purpose. Individuals who were not psychotic, clearly intoxicated, mentally retarded, unconscious, or highly agitated were considered capable of giving informed consent. Women who agreed to participate were randomly assigned to the video intervention or standard services (NV) condition. Women in the video condition watched the video before receiving the forensic sexual assault examination. Following the examination, participants were scheduled for 6-week follow-up interviews during which time-dependent measures were collected. In May 2000, after 231/442 participants had been recruited, we added two additional study conditions (ME and PE) as described above.
3. Results
3.1. Analytic method
Statistical Analyses
Regression analyses were used for models predicting continuous measures of alcohol, marijuana, and hard drug use at the 3 follow-up time points. A log(x+1) transformation method was used to better approximate normality. The main effects of Minority status, prior assault history, prior alcohol or drug use, and video condition and all possible higher order interactions between the intervention condition and other predictor variables with substance use were tested. To reduce risk of Type 1 error within multivariable analyses, alpha for those analyses was set at .005. Due to low prevalence of abuse variables, univariate and nested chi-square analyses were used to evaluate associations between predictor and outcome variables as in the previous report.
Table 2 presents the proportion of participants in each intervention condition reporting lifetime assault, lifetime substance use and abuse, and recent pre-sexual assault substance use in the total sample. Levels of experienced violence and substance use and abuse were high but did not differ significantly between groups with the exception that a higher percentage of those in the video condition reported hard drug use in the 6 weeks prior to index sexual assault. As noted in Table 2 only 34 participants in the sample reported recent pre-assault hard drug use. Table 3 includes frequency of substance use and prevalence of abuse outcomes at each time point.
Table 2.
Frequencies for Study Variables
| Total with Risk Factor | Participants in the Non-Video Condition | Participants in the Video Condition | |||||
|---|---|---|---|---|---|---|---|
| Risk Factor | % | n | % | n | % | n | Total N |
| Lifetime Sexual or Physical Assault | 59.3 | 159 | 61.7 | 66 | 57.8 | 93 | 268 |
| Minority | 41.8 | 112 | 40.2 | 43 | 42.9 | 69 | 268 |
| Lifetime Use Alcohol1 | 72.3 | 193 | 76.6 | 82 | 69.4 | 111 | 267 |
| Lifetime Use Marijuana | 54.5 | 146 | 52.3 | 56 | 55.9 | 90 | 268 |
| Lifetime use Hard Drugs | 29.2 | 78 | 27.1 | 29 | 30.6 | 49 | 267 |
| Lifetime Abuse Alcohol | 39.5 | 105 | 43.0 | 46 | 37.5 | 59 | 266 |
| Lifetime Abuse Marijuana | 16.9 | 45 | 20.6 | 22 | 14.5 | 23 | 266 |
| Lifetime Abuse Hard Drugs | 14.3 | 38 | 10.3 | 11 | 17.0 | 27 | 266 |
| Use Alcohol 6-week Pre-assault1 | 52.1 | 136 | 54.2 | 58 | 50.6 | 81 | 267 |
| Use Marijuana 6-week Pre-assault | 29.1 | 77 | 26.9 | 28 | 30.4 | 49 | 265 |
| Use Hard Drugs 6-week Pre-assault | 12.7 | 34 | 7.5 | 8 | 16.3 | 26* | 267 |
p < .05.
Alcohol use defined as 4 or more drinks in a one-day period.
Table 3.
Frequencies of Outcomes by Timepoint
| Time One | Time Two | Time Three | ||||
|---|---|---|---|---|---|---|
| Outcome | M | (S.D.) | M | (S.D.) | M | (S.D.) |
| Alcohol Use Frequency | 2.47 | 3.71 | 2.31 | 2.94 | 2.47 | 3.37 |
| Marijuana Use Frequency | .84 | 2.66 | 1.02 | 3.00 | .98 | 2.85 |
| Hard Drug Use Frequency | .20 | .78 | .21 | .69 | .20 | .96 |
|
|
||||||
| % | n | % | n | % | n | |
|
|
||||||
| Alcohol Abuse | 15.4 | 33 | 15.0 | 20 | 19.2 | 42 |
| Marijuana Abuse | 7 | 15 | 6.8 | 9 | 7.8 | 17 |
| Hard Drug Abuse | 3.3 | 7 | 3.0 | 4 | 4.6 | 10 |
Note: For frequency of use data the total sample size at Time One was 216, at Time Two was 130 (with the exception of marijuana use, n =131), and at Time Three was 217. For abuse variables the sample size at Time One was 214, at Time Two was 133, and at Time Three was 219.
3.1.1. Alcohol
Point biserial correlations between individual predictors and alcohol use frequency indicated that minority status was inversely related to prior alcohol use and frequency of use at Time 1 and Time 2 (p < .01). Prior history of assault was positively associated with frequency of use at Time 3 (p < .05), while prior alcohol use was positively correlated with use at each time point (all p < .001). Table 4 presents the results of the analysis for frequency of alcohol use within the previous 2 weeks at each assessment. Prior alcohol use was a significant predictor of post-sexual assault frequency of use at Time 1 and Time 2. The overall models were significant at each time point with full model R2 ranging from .20 to .41.
Table 4.
Linear Regression Analyses of Predictors of Alcohol Use at Time One, Two and Three
| Predictor | B (s.e.) | Beta | t | p | ||
|---|---|---|---|---|---|---|
| Time One | Prior Use of Alcohol | .49 (.17) | .63 | 2.85 | .005 | R2 =.29 |
| Minority Status | −.06 (.18) | −.07 | −.32 | .75 | ||
| Prior Assault History | −.13 (.17) | −.17 | −.81 | .42 | ||
| Video Intervention | −.14 (.31) | −.17 | −.44 | .66 | ||
| Video Intervention x Prior Assault History | .12 (.10) | .33 | 1.22 | .23 | ||
| Video Invervention x Minority Status | .04 (.10) | .11 | .39 | .70 | ||
| Video Intervention x Prior Use of Alcohol | −.05 (.10) | −.15 | −.52 | .60 | F(7,207)=12.14, p <.001 | |
|
| ||||||
| Time Two | Prior Use of Alcohol | .77 (.20) | 1.06 | 3.91 | <.001 | R2 =.41 |
| Minority Status | .12 (.20) | .16 | .61 | .54 | ||
| Prior Assault History | −.11 (.19) | −.15 | −.57 | .57 | ||
| Video Intervention | .38 (.32) | .51 | 1.18 | .24 | ||
| Video Intervention x Prior Assault History | .07 (.11) | .23 | .66 | .51 | ||
| Video Invervention x Minority Status | −.12 (.11) | −.35 | −1.04 | .30 | ||
| Video Intervention x Prior Use of Alcohol | −.21 (.11) | −.65 | −1.88 | .06 | F(7,122)=11.86, p <.001 | |
|
| ||||||
| Time Three | Prior Use of Alcohol | .21 (.17) | .29 | 1.28 | .20 | R2 =.20 |
| Minority Status | −.003 (.17) | −.004 | −.02 | .98 | ||
| Prior Assault History | .17 (.16) | .22 | 1.05 | .29 | ||
| Video Intervention | .02 (.29) | .03 | .08 | .94 | ||
| Video Intervention x Prior Assault History | −.06 (.10) | −.17 | −.60 | .55 | ||
| Video Invervention x Minority Status | −.01 (.10) | .04 | .13 | .90 | ||
| Video Intervention x Prior Use of Alcohol | .06 (.10) | .18 | .62 | .53 | F(7,208)=6.91, p <.001 | |
Alcohol abuse at Time 1 was significantly higher among those who were non-minority compared to minority (21.8% vs. 6.7%, X2 (1, 214) = 9.13, p < .01) or who were using alcohol in the 6 weeks before being sexually assaulted (27.5% vs. 2.9%, X2 (1, 214) = 24.95, p < .001). Similarly, non-minority status was a predictor of alcohol abuse at Time 3, and prior alcohol use predicted abuse at Time 2 and Time 3 (all p < .01). Time 3 alcohol abuse was higher among those with reported prior history of assault (24.0% vs. 12.2%, X2 (1, 218) = 4.77, p < .05). The video was not significantly associated with alcohol abuse. There were no significant differences in alcohol abuse in association with AV vs. NV conditions after controlling for other predictor variables.
3.1.2. Marijuana
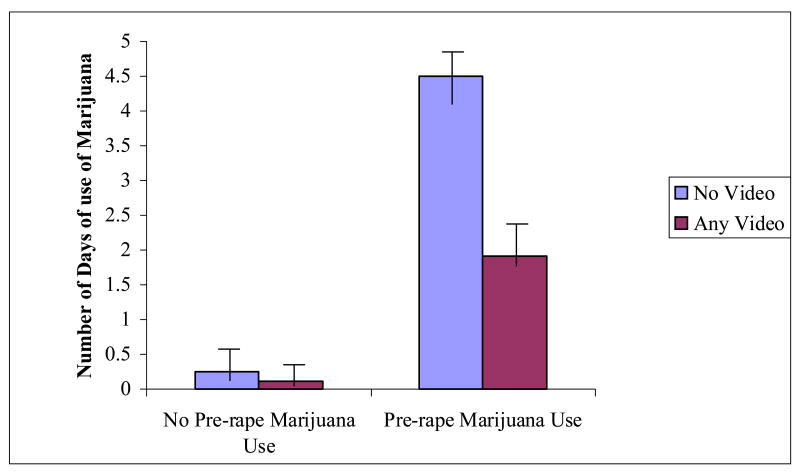
Point biserial correlations between individual predictors and marijuana use frequency indicated that pre-assault marijuana use was inversely related to minority status and positively related to prior assault history (p < .05). Frequency of marijuana use at Time 1 and Time 3 was inversely related to minority status and positively related to prior history of assault (all p < .05). Frequency of use at all time points was positively related to prior marijuana use (all p < .001). Table 5 presents results of the analysis for frequency of marijuana use within the previous 2 weeks at each assessment. The two-way interaction for intervention condition by prior use was significant at each time point. Being in the AV condition was significantly associated with reduced frequency of use, but only among those who were using marijuana prior to the recent sexual assault. The pattern of findings is depicted in Figure 1 using nontransformed scores. The overall models predicting marijuana use were significant at each time point with full model R2 ranging from .33 to .41.
Table 5.
Linear Regression Analyses of Predictors of Marijuana Use at Time One, Two and Three
| Predictor | B (s.e.) | Beta | t | p | ||
|---|---|---|---|---|---|---|
| Time One | Prior Use of Marijuana | .72 (.12) | 1.20 | 5.95 | <.001 | R2 =.40 |
| Minority Status | .10 (.11) | .19 | .95 | .34 | ||
| Prior Assault History | .17 (.11) | .31 | 1.59 | .11 | ||
| Video Intervention | .42 (.17) | .75 | 2.43 | .02 | ||
| Video Intervention x Prior Assault History | −.07 (.06) | −.29 | −1.11 | .27 | ||
| Video Invervention x Minority Status | −.05 (.06) | −.21 | −.81 | .42 | ||
| Video Intervention x Prior Use of Marijuana | −.23 (.07) | −.85 | −3.18 | .002 | F (7,206)=19.39, p <.001 | |
|
| ||||||
| Time Two | Prior Use of Marijuana | .95 (.18) | 1.38 | 5.37 | <.001 | R2 =.41 |
| Minority Status | −.10 (.16) | −.16 | −.61 | .54 | ||
| Prior Assault History | .23 (.17) | .37 | 1.39 | .17 | ||
| Video Intervention | .50 (.23) | .78 | 2.15 | .03 | ||
| Video Intervention x Prior Assault History | −.12 (.10) | −.44 | −1.26 | .21 | ||
| Video Invervention x Minority Status | .03 (.09) | .10 | .31 | .76 | ||
| Video Intervention x Prior Use of Marijuana | −.36 (.10) | −1.13 | −3.42 | .001 | F (7,122)=12.28, p <.001 | |
|
| ||||||
| Time Three | Prior Use of Marijuana | .69 (.13) | 1.07 | 5.42 | <.001 | R2 =.33 |
| Minority Status | .04 (.12) | .07 | 0.35 | .73 | ||
| Prior Assault History | .11 (.12) | .19 | 0.96 | .34 | ||
| Video Intervention | .34 (.19) | .60 | 1.89 | .06 | ||
| Video Intervention x Prior Assault History | −.06 (.07) | −.21 | −0.79 | .43 | ||
| Video Invervention x Minority Status | −.04 (.07) | −.14 | −0.53 | .60 | ||
| Video Intervention x Prior Use of Marijuana | −.23 (.08) | −.76 | −2.92 | .004 | F (7,206)=14.48, p <.001 | |
Figure 1.
Number of days of marijuana use in the previous two weeks as a function of pre-assault use and treatment group.
Note: The data presented in this figure are from Time 1. The same pattern of results was found at Times 2 and 3.
Pre-sexual assault marijuana use compared to non-use was the only variable associated with increased marijuana abuse at each time point. Those using marijuana in the 6 weeks prior to assault were more likely to meet criteria for marijuana abuse at Time 1 (22% vs. 0%), Time 2 (20.6% vs. 2%), and Time 3(21% vs. 2.6%); all p < .001. There were no significant differences in association with AV vs. NV conditions after controlling for other predictor variables at any time point.
3.1.3. Hard drugs
Point biserial correlations between individual predictors and hard drug use frequency indicated that prior hard drug use was positively related prior history of assault and to being in the AV condition as well as to frequency of hard drug use at each time point (all p < .001). There were no independent predictors of post assault hard drug use at any time point after controlling for other variables. However, the overall models were significant at each time point with full model R2 ranging from .18 to .23.
Time 1 hard drug abuse was higher among those reporting pre-assault use (12.5% vs. 2.1%, X2 (1, 214) = 7.28, p < .05) and was higher in the AV condition (5.3% vs. 0%, X2 (1, 214) = 4.59, p < .05). As noted above, AV condition was also associated with pre-assault use. There were no significant predictors of hard drug abuse at Time 2. Time 3 hard drug abuse was also predicted by pre-sexual assault hard drug use (p < .0005). There were no significant associations between treatment condition and hard drug abuse after controlling for pre-assault use or other predictor variables at any time point.
4. Discussion
The primary objective of the current study was to examine the efficacy of a two-part video intervention in reducing post-sexual assault substance use and abuse. We previously reported findings based on a smaller sample (Acierno et al., 2003) in which data indicated that the video intervention was associated with significantly lower prevalence of marijuana abuse at a 6 week post-assault assessment. The purpose of the current report was to update and extend these important findings within a larger sample of 268 participants who provided data throughout the end of the study period.
Descriptive analyses indicated that similar to previous findings (Acierno et al., 2003; Kilpatrick et al., 1987) minority participants were less likely to report recent use of alcohol or marijuana prior to the sexual assault; were less likely to meet criteria for alcohol abuse at follow-up; and were less frequent users of alcohol and marijuana at follow-up assessment. Consistent with hypothesized bidirectional associations between sexual assault and substance misuse (Testa & Parks, 1996) prior history of assault was positively associated with pre-assault marijuana and hard drug use which may potentially have increased risk of index assault. In addition, prior assault history was positively associated with frequency of alcohol use and abuse at 6 months post-assault and with frequency of marijuana use at assessments within 3 months and at 6 months. Thus, history of assault may increase risk of substance use which in turn may increase risk of victimization and substance use and abuse. Minority status and prior history of assault were not predictors of post-assault use after controlling for the more proximal predictor of pre-assault substance use.
Results of the current study indicate that women viewing the video reported lower frequency of marijuana use at each assessment point, after controlling for pre-assault use. Thus, among recent (e.g., pre-assault) marijuana users this brief intervention appeared to have a positive impact that persisted over time. Although our initial study indicated a difference between video and nonvideo groups in terms of marijuana abuse rather than use, the current findings are consistent in the sense that marijuana use is a precursor of abuse, and is itself an illicit activity. It is possible that this type of brief intervention may be most helpful in impacting behaviors prior to development of a longer standing or more problematic pattern of abuse.
We did not observe any other associations between the video and use or abuse of alcohol or hard drugs controlling for prior use. In each case, pre-assault use was a strong predictor of post-assault use. It is possible that this brief intervention is insufficient to effect change in use or abuse of alcohol or hard drugs. In addition or alternatively, prevalence of pre-assault alcohol use was high (approximately half the sample) and the criterion may have been too broad to identify a subgroup with pre-assault problem drinking. Similarly, we were restricted in our alcohol use outcome measures to looking at number of days used as opposed to information about amount of use which may have limited our ability to identify more problematic behavior at follow-up time points. Prevalence of pre- and post-assault hard drug use was relatively low which limited power to evaluate potential associations with the intervention. In addition, hard drug use may be less likely to be affected by a brief intervention.
A major limitation of the current study was our inability to examine separate components of the video intervention that might have been differentially associated with outcomes assessed. Theoretically, the video content addressing preparation for the medical exam and that addressing psychological reactions could both reduce acute and/or longer term anxiety or other distress and might be expected to reduce risk of substance use or abuse via the tension reduction or self-medication hypothesis. The conceptualization of post-victimization substance use as a negatively reinforced coping response (Stewart, 1997) is consistent with findings across multiple studies (Coffey et al., 2002; Miranda et al., 2002; Saladin et al., 2003; Sharkansky et al., 1999; and Stewart et al., 2000) finding increased drinking and drug use behavior associated with exposure to anxiety-provoking situations or cues. Alternatively, those exposed to the psychoeducation content received specific information and modeling of behaviors that more directly addressed substance use and abuse behaviors. Specifically, content related to drug and alcohol abuse was consistent with that provided in existing brief interventions and included messages focused on identification of potential triggers for use, identification of and recommendations to engage in situations that are incompatible with use, and modeling of activities that did not involve drug or alcohol use.
Participants in the AV condition included those who watched the Full Video as well as those who watched only the Medical Exam Preparation or Psychoeducation components. Thus, we are limited in terms of inferences that can be made about whether content related to preparing for the stressor of the medical exam or content directly addressing drug and alcohol related behaviors was associated with reduced frequency of use of marijuana. Therefore we are unable to elucidate possible mechanisms that might mediate observed changes in behavior. Similarly, because we did not include a time and attention control condition we are unable to rule out the possibility that the video may have served as a distraction rather than the possibility that specific content was relevant in terms of association with marijuana use.
Conclusions and Limitations
Despite the larger number of participants in the full study sample, we had limited power to detect potential differences between the major video components. Future research should control for nonspecific effects of time and attention by including an attention control video of comparable length to further evaluate the impact of this brief easily delivered hospital based intervention. Measures to assess motivation for use of drugs or alcohol would be helpful to address potential mechanisms of change that might be associated with the intervention as would evaluation of activity schedules and psychological functioning. Additionally, the effects of this intervention were small. Nonetheless, we were encouraged by the positive impact of the treatment in light of its brevity, low cost, and ease of exportation to forensic exam settings across the country. Even low intensity interventions, when they have the potential for reaching large numbers of people in the population can have high public health impact. Results of this study need to be replicated. It would be particularly useful to conduct a replication study at an independent site and with samples that may differ from the current sample population in terms of demographics to evaluate validity and generalizeability of findings.
Acknowledgments
This research was supported by:
1. National Institute on Drug Abuse grant no. R01 DA11158 entitled “Prevention of Post Rape Psychopathology and Drug Abuse”;
2. Medical University of South Carolina Healthy South Carolina Grant-in-Aid Initiative entitled “Multidisciplinary Treatment of Acute and Long Term Health Effects of Rape Victimization: Development of A Model Program”;
3. NIH sponsored Medical University of South Carolina General Clinical Research Center Supported Study, 5M01 RR01070;
4. NIMH R01MH068626, entitled “New Longitudinal Methods for Trauma Research” (Daniel King, PI).
We wish to acknowledge thoughtful critical feedback and suggestions from Kenneth Ruggiero and Dean Kilpatrick in development of this manuscript.
Footnotes
Only 4 participants recruited at the time of the forensic exam were 14. All others were 15 or older. All participants completing at least one follow-up assessment were 15 or older.
A smaller number of participants completed the Time 2 assessment because that assessment was added into the study, after the dismantling phase began in 2000. The Time 1 and Time 2 assessments were conducted throughout the entire course of the study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Acierno R, Resnick HS, Flood A, Holmes M. An acute post-rape intervention to prevent substance use and abuse. Addictive Behaviors. 2003;28:1701–1715. doi: 10.1016/j.addbeh.2003.08.043. [DOI] [PubMed] [Google Scholar]
- Avis NE, Smith KW, Link CL, Goldman MB. Increasing mammography screening among women over age 50 with a videotape intervention. Preventive Medicine. 2004;39:498–506. doi: 10.1016/j.ypmed.2004.05.024. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Harvey AG, Basten C, Dang ST, Sackville T. Treatment of acute stress disorder: A comparison of cognitive behavioral therapy and supportive counseling. Journal of Consulting and Clinical Psychology. 1998;66:862–866. doi: 10.1037//0022-006x.66.5.862. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Sackville T, Dang ST, Moulds M, Guthrie R. Treating acute stress disorder: An evaluation of cognitive behavior therapy and supportive counseling techniques. American Journal of Psychiatry. 1999;156:1780–1786. doi: 10.1176/ajp.156.11.1780. [DOI] [PubMed] [Google Scholar]
- Burnam MA, Stein JA, Golding JM, Siegel JM, Sorenson SB, Forsythe AB, Telles CA. Sexual assault and mental disorders in a community population. Journal of Consulting and Clinical Psychology. 1988;56:843–850. doi: 10.1037//0022-006x.56.6.843. [DOI] [PubMed] [Google Scholar]
- Coffey SF, Saladin ME, Drobes DJ, Brady KT, Dansky BS, Kilpatrick DG. Trauma and substance cue reactivity in individuals with comorbid posttraumatic stress disorder and cocaine or alcohol dependence. Drug and Alcohol Dependence. 2002;65:115–127. doi: 10.1016/s0376-8716(01)00157-0. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hearst-Ikeda D, Perry KK. Evaluation of a brief cognitive–behavioral program for the prevention of chronic PTSD in recent assault victims. Journal of Consulting and Clinical Psychology. 1995;63:948–955. doi: 10.1037//0022-006x.63.6.948. [DOI] [PubMed] [Google Scholar]
- Foa EB, Zoellner LA, Feeny NC. An evaluation of three brief programs for facilitating recovery after assault. Journal of Traumatic Stress. 2006;19:29–43. doi: 10.1002/jts.20096. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, O'Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The timeline followback reports of psychoactive substance use by drug-abusing patients: Psychometric properties. Journal of Consulting and Clinical Psychology. 2000;68:134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- Gagliano ME. A literature review on the efficacy of video in patient education. Journal of Medical Education. 1988;63:785–792. doi: 10.1097/00001888-198810000-00006. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Resnick HS, Saunders B, Best CL. The relationship between assault and alcohol, marijuana, and hard drug use in women. Journal of Consulting and Clinical Psychology. 1997;65:834–847. doi: 10.1037//0022-006x.65.5.834. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Schnurr PP, Saunders B, Resnick HS, Best CL. Risk factors for adolescent substance abuse and dependence: Data from a national sample. Journal of Consulting and Clinical Psychology. 2000;68:19–30. doi: 10.1037//0022-006x.68.1.19. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Edmunds CN, Seymour AK. Rape in America: A report to the nation. Arlington, VA: National Victim Center & Medical University of South Carolina; 1992. [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the national survey of adolescents. Journal of Consulting and Clinical Psychology. 2003;71:692–700. doi: 10.1037/0022-006x.71.4.692. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Saunders BE, Veronen LJ, Best CL, Von JM. Criminal victimization: Lifetime prevalence, reporting to police, and psychological impact. Crime and Delinquency. 1987;33:479–189. [Google Scholar]
- Krouse HJ. Video modeling to education patients. Journal of Advanced Nursing. 2001;33:748–757. doi: 10.1046/j.1365-2648.2001.01716.x. [DOI] [PubMed] [Google Scholar]
- Ledray LE, Kraft J. Evidentiary examination without a police report: Should it be done? Are delayed reporters and nonreporters unique? Journal of Emergency Nursing. 2001;27:396–400. doi: 10.1067/men.2001.117421. [DOI] [PubMed] [Google Scholar]
- Miller BA, Downs WR, Gondoli DM, Keil A. The role of childhood sexual abuse in the development of alcoholism in women. Violence and Victims. 1987;2:157–172. [PubMed] [Google Scholar]
- Miranda R, Meyerson LA, Long PJ, Marx BP, Simpson SM. Sexual assault and alcohol use: Exploring the self-medication hypothesis. Violence and Victims. 2002;17:205–217. doi: 10.1891/vivi.17.2.205.33650. [DOI] [PubMed] [Google Scholar]
- Monti PM, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers M, Woolard R, Lewander W. Brief intervention for harm reduction with alcohol positive older adolescents in a hospital emergency department. Journal of Consulting and Clinical Psychology. 1999;67:989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97:279–292. doi: 10.1046/j.1360-0443.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- Polusny MA, Follette VM. Long term correlates of child sexual abuse: Theory and review of the empirical literature. Applied and Preventive Psychology. 1995;4:143–166. [Google Scholar]
- Resick PA. The psychological impact of rape. Journal of Interpersonal Violence. 1993;8:223–255. [Google Scholar]
- Resnick H, Acierno R, Holmes M, Kilpatrick D, Jager N. Prevention of post rape psychopathology: Preliminary evaluation of an acute rape treatment. Journal of Anxiety Disorders. 1999;13:359–370. doi: 10.1016/s0887-6185(99)00010-9. [DOI] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and PTSD in a representative sample of women. Journal of Consulting and Clinical Psychology. 1993;61:985–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- Rheingold AA, Acierno R, Resnick HS. Trauma, posttraumatic stress disorder, and health risk behaviors. In: Schnurr PP, Green BL, editors. Trauma and health. Washington, DC: American Psychological Association; 2004. pp. 217–243. [Google Scholar]
- Saladin ME, Drobes DJ, Coffey SF, Dansky BS, Brady KT, Kilpatrick DG. PTSD symptom severity as a predictor of cue-elicited drug craving in victims of violent crime. Addictive Behaviors. 2003;28:1611–1629. doi: 10.1016/j.addbeh.2003.08.037. [DOI] [PubMed] [Google Scholar]
- Sharkansky E, Brief D, Meehan J, Mannix L. Substance abuse patients with post-traumatic stress disorder (PTSD): Identifying specific triggers of substance abuse and their association with PSTD symptoms. Psychology of Addictive Behaviors. 1999;13:89–97. [Google Scholar]
- Simpson TL, Miller WR. Concomitance between childhood sexual and physical abuse and substance use problems. A review. Clinical Psychology Review. 2002;22:27–77. doi: 10.1016/s0272-7358(00)00088-x. [DOI] [PubMed] [Google Scholar]
- Sobell MB, Sobell LC. Behavioral treatment of alcohol problems. New York: Plenum; 1978. [Google Scholar]
- Steketee G, Foa EB. Rape victims: Post-traumatic stress responses and their treatment: A review of the literature. Journal of Anxiety Disorders. 1987;1:69–86. [Google Scholar]
- Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. Journal of Consulting and Clinical Psychology. 2000;68:898–908. [PubMed] [Google Scholar]
- Stewart S. Trauma memory and alcohol abuse: Drinking to forget? In: Read JD, Lindsay DS, editors. Recollections of trauma: Scientific evidence and clinical practice. Plenum; NY: 1997. pp. 461–467. [Google Scholar]
- Stewart S, Conrod P, Samoluk S, Pihl R, Dongier M. Post-traumatic stress disorder symptoms and situation-specific drinking in women substance abusers. Alcoholism Treatment Quarterly. 2000;18:31–47. [Google Scholar]
- Testa M, Parks KA. The role of women's alcohol consumption in sexual victimization. Aggression and Violent Behavior. 1996;1:217–234. [Google Scholar]
- Tjaden P, Thoennes N. Research in Brief. Washington, DC: U.S. Department of Justice, National Institute of Justice; 1998. Prevalence, incidence, and consequences of violence against women. (NCJ172837) [Google Scholar]
- Zatzick D, Roy-Byrne P, Russo J, Rivara F, Droesch R, Wagner A, et al. A randomized effectiveness trial of stepped collaborative care for acutely injured trauma survivors. Archives of General Psychiatry. 2004;61:498–506. doi: 10.1001/archpsyc.61.5.498. [DOI] [PubMed] [Google Scholar]