Abstract
Previous studies have shown that spinal cord stimulation (SCS) of upper lumbar segments decreases visceromotor responses to mechanical stimuli in a sensitized rat colon and reduces symptoms of irritable bowel syndrome in patients. SCS applied to the upper cervical spinal dorsal column reduces pain of chronic refractory angina. Further, chemical stimulation of C1-C2 propriospinal neurons in rats modulates the responses of lumbosacral spinal neurons to colorectal distension. The present study was designed to compare the effects of upper cervical and lumbar SCS on activity of lumbosacral neurons receiving noxious colorectal input. Extracellular potentials of L6-S2 spinal neurons were recorded in pentobarbital anesthetized, paralyzed and ventilated male rats. SCS (50 Hz, 0.2 ms) at low intensity (90% of motor threshold) was applied to the dorsal column of upper cervical (C1-C2) or upper lumbar (L2-L3) ipsilateral spinal segments. Colorectal distension (CRD, 20, 40, 60 mmHg, 20 s) was produced by air inflation of a latex balloon. Results showed that SCS applied to L2-L3 and C1-C2 segments significantly reduced the excitatory responses to noxious CRD from 417.6±68.0 imp to 296.3±53.6 imp (P<0.05, n=24) and from 336.2±64.5 imp to 225.0±73.3 imp (P<0.05, n= 18), respectively. Effects of L2-L3 and C1-C2 SCS lasted 10.2±1.9 min and 8.0±0.9 min after offset of CRD. Effects of SCS were observed on spinal neurons with either high or low threshold excitatory responses to CRD. However, L2-L3 or C1-C2 SCS did not significantly affect inhibitory neuronal responses to CRD. C1-C2 SCS-induced effects were abolished by cutting the C7-C8 dorsal column but not by spinal transection at cervicomedullary junction. These data demonstrated that upper cervical or lumbar SCS modulated responses of lumbosacral spinal neurons to noxious mechanical stimulation of the colon, thereby, proved two loci for a potential therapeutic effect of SCS in patients with irritable bowel syndrome and other colonic disorders.
Keywords: Visceral hypersensitivity, irritable bowel syndrome, colorectal distension, spinal cord
INTRODUCTION
During the last three decades, spinal cord stimulation (SCS) has become a therapy used for treating certain chronic pains, such as neuropathic pain and ischemic pain (Cameron 2004; Meyerson and Linderoth 2000a). Various neurophysiological and neurochemical mechanisms underlying the beneficial effects of SCS have also been proposed (Linderoth and Foreman 1999; 2006). In general, electric stimulation to the dorsal column, which contains large diameter afferent fibers, inhibits transmission of nociceptive information at the spinal segmental level. This finding implicates elements of the gate control theory (Melzack and Wall 1965), although activation of supraspinal circuits may also be involved (El-Khoury et al., 2002). Several experimental studies have been performed to explore effects of SCS on spinal neuronal processing of noxious somatic inputs. For example, SCS mainly suppresses excitatory responses of spinothalamic tract neurons (STT) and spinal neurons to noxious somatic stimuli in monkeys (Foreman et al. 1976) and cats (Lindblom et al. 1977), attenuates dorsal horn neuronal hyperexcitability in rats with mononeuropathy (Yakhnisa et al. 1999), and inhibits long-term potentiation of spinal dynamic range neurons in rats (Wallin et al. 2003).
The mechanisms evoked by SCS have primarily addressed relief of somatic pain, particularly neuropathic pain. However, few studies have examined effects of SCS on visceroreceptive transmission in the spinal cord. Indeed, SCS is used in patients to treat chronic refractory angina (Eliasson et al., 1996, Hautvast et al., 1998). Persistent esophageal pain also has been treated with SCS (Jackson and Simpson, 2004). Chandler et al. (1993) report that SCS in monkeys reduces excitatory responses of thoracic STT neurons to electrical stimulation of cardiopulmonary sympathetic afferent fibers and to intracardiac injection of bradykinin. Recently, experimental studies have shown that SCS suppresses or attenuates the nociceptive visceromotor reflex produced by colorectal distension in rats with acute or chronic colonic hypersensitivity produced with acetic acid or trinitrobenzenesulfonic acid (Greenwood-Van Meerveld et al. 2003; 2005). Based on these animal studies, Krames and Mousad (2004) demonstrated in a case study that SCS might be a potential therapy for the treatment of patients with irritable bowel syndrome. However, the effects of SCS on spinal neuronal responses to colorectal distension have not been examined.
Commonly SCS is applied to the segments that elicit paresthesias in areas where patients experience the pain (Linderoth and Foreman 1999; 2006; Meyerson & Linderoth, 2000a). However, in one human study SCS applied distant to the site of origin of refractory angina in upper cervical spinal segments also reduced the pain symptoms (Gonzalez-Darder et al., 1991). Animal studies have also shown that chemical activation of cell bodies in the C1-C2 spinal segments of spinal cord significantly suppresses excitatory responses of thoracic spinal neurons receiving noxious inputs from heart and esophagus (Qin et al. 2004), and lumbosacral spinal neurons with noxious colorectal input (Qin et al., 1999). These observations suggest that SCS applied to upper cervical segments might also affect lumbosacral spinal neuronal responses to noxious colorectal stimulus. The present study in rats was designed to examine and compare the effects of SCS applied to upper cervical and lumbar segments on responses of lumbosacral spinal neurons to noxious colorectal stimulation (CRD). The results showed that SCS at both locations using clinical stimulation parameters significantly reduced excitatory responses to noxious CRD in L6-S2 spinal neurons. A preliminary report has been published in abstract form (Foreman et al. 2005).
METHODS
Experiments were performed on 26 male Sprague-Dawley rats (Charles River Inc.) weighing between 320-480 g. Protocols were approved by the Institutional Animal Care and Use committee of the University of Oklahoma Health Sciences Center and followed guidelines of the American Physiological Society and the International Association for the Study of Pain. Animals initially were anesthetized with sodium pentobarbital (50 mg/kg ip). The right carotid artery and left jugular vein were cannulated to monitor blood pressure and to infuse pentobarbital (15-25 mg/kg/h) during the experiment, respectively. After tracheal cannulation, a constant volume pump was used to provide artificial ventilation (55-60 strokes/min, 3.0-5.0 ml stroke volume). Paralysis of animals was established with pancuronium bromide (0.2 mg/kg/h, i.v.). Body temperature was kept between 37 and 38°C using a thermostatically controlled heating blanket and overhead infrared lamps.
Laminectomies were performed to expose L6-S2 spinal segments for recording spinal neurons. L2-L3 and C1-C2 spinal segments also were exposed for placing electrodes for spinal cord stimulation (SCS). Animals were mounted in a stereotaxic headholder and spinal clamps attached to a metal frame were fixed at caudal thoracic and sacral vertebrae. The dura mater of exposed spinal segments was carefully removed. A small well was made on the L6-S2 segments with dental impression material and filled with agar (3-4% in saline) to improve recording stability. Carbon-filament glass microelectrodes were used to record extracellular action potentials of single spinal neurons in a region from midline to 2 mm lateral and 0-1.2 mm deep from the dorsal surface of L6-S1 segments. A spring-loaded platinum-ball electrode (0.5-1.0 mm in diameter) was applied to the dorsal column ipsilateral to neuronal recording sites at either upper lumbar (L2-L3) or upper cervical (C1-C2) segments for SCS. The electrical current at the onset of small contractions in paraspinal muscles was defined as the motor threshold (Tanaka et al. 2001). Average motor thresholds of SCS (50 Hz, 0.2 ms) at C1-C2 and L2-L3 were 0.35±0.8 mA and 0.40±0.09 mA, respectively. Spinal cord stimulation was performed for 3-5 min at an intensity of 90% motor threshold before animals were paralyzed. In some cases, the short-term SCS (10 s) was used to compare the effects on spontaneous activity and responses of spinal neurons to CRD before and after spinal transection at rostral C1 segment (cervicomedullary) and cutting C7-C8 dorsal column. Spinal transections were gently performed by using a sharp surgical blade. In addition, in a few cases, ibotenic acid (1 mg/ml) was absorbed onto filter paper pledgets (2mm × 2mm) and placed on the dorsal surface of the C1-C2 to inactivate cell bodies. Effects of C1-C2 SCS on spontaneous activities and nociceptive responses to CRD were assessed 20 min after ibotenic acid was applied to the dorsal surface of C1-C2. Ibotenic acid is an excitatory neurotoxin and a glutamate analog that destroys neuronal perikarya, but spares axons and non-neuronal cells (Ren et al., 1990; Marini et al., 2000).
Innocuous and noxious CRD (20, 40, 60 mmHg, 20s) were produced by air-inflation of a 4-5 cm long latex balloon that was inserted into the descending colon and connected to a sphygmomanometer (Qin et al. 1999). Intracolonic pressure of 60 mmHg for 20 s was used as a search stimulus. To induce CRD, the intracolonic pressure rapidly reached the required level at a rate of 20-40 mmHg per second and then the pressure was consistently kept at this level by monitoring the pressure gauge and adjusting it with an air pump to make sure the pressure remained constant throughout the stimulation period. Neurons responding to CRD at 60 mmHg for 20 s were tested with this stimulus 2-3 times to make sure responses were consistent and repeatable. Raw traces of neuronal activity were stored in a computer with Spike-2 software (CED, Cambridge, UK) and evaluated using rate histograms (bin width 1 s). Spontaneous activity of neurons was counted for 10 s before the onset of CRD to obtain impulses per second (imp/s). Neuronal responses to CRD were calculated as total impulses (imp) of a change in activity from the onset of increased or decreased activity until the evoked activity returned to control. Latency and duration of responses to CRD also were measured. Based on the intracolonic pressure that produced a neuronal response, L6-S2 neurons excited by CRD were divided into the following two subgroups: low-threshold (LT) neurons responded to intracolorectal pressure 20 ≤mmHg; high-threshold (HT) neurons responded to ≥40 mmHg pressure of CRD (Qin et al. 2003). For testing SCS effects, two consistent responses to noxious CRD (60 mmHg, 20 s) were first obtained as pre-control responses and then a noxious CRD was performed during SCS (3-5 min). After SCS offset, noxious CRD at 3-8 min intervals were administered until the CRD-response recovered (>80% of pre-control responses). Recovery time of the effects of SCS was identified as the period from offset of SCS to the return of the CRD responses to control levels. Descriptive data are reported as means ± SE. Statistical comparisons were made using Student's paired t-test and Chisquare analysis. Comparisons of data were considered statistically different if P < 0.05.
Somatic receptive fields of spinal neurons also were characterized. For innocuous stimulation of cutaneous receptive fields of spinal neurons, a camel-hair brush or light pressure from a blunt probe was used, whereas for noxious stimulation pinching the skin and muscles with blunt forceps was used. Neurons were classified as follows: wide dynamic range (WDR) neurons responded to innocuous stimulation of skin and had greater responses to noxious pinching of the somatic field; high-threshold (HT) neurons responded only to noxious pinching of the somatic field; and low-threshold (LT) neurons responded primarily to innocuous stimuli. If a cutaneous receptive field was not found, movement of tail (MT) was tested.
To mark spinal recording sites of neurons that responded to CRD, an anodal electrolytic lesion (50 μA DC, 20 s) was made after a neuron was studied. At the end of the experiment, the animal was euthanized with an overdose of pentobarbital sodium (200 mg/kg). The lumbosacral spinal cord was removed and placed in 10% buffered formalin solution. Frozen sections (55-60 μm) of the spinal cord were viewed to identify lesion sites using the cytoarchitectonic scheme of Molander et al. (1984).
RESULTS
A total of 28 lumbosacral spinal neurons with excitatory (n=24) or inhibitory (n=4) responses to noxious CRD (60 mmHg, 20 s) were examined for effects of SCS at upper lumbar (L2-L3) and/or upper cervical (C1-C2) spinal segments. These neurons were recorded from the left (n = 18) or the right side (n= 10) of L6-S2 segments. Examples of LT and HT neurons are shown in Fig.1A and B. Twenty of 28 neurons responsive to CRD received convergent inputs from cutaneous receptive fields or tail rotation. Of viscerosomatic convergent neurons, 7 neurons were classified as WDR, 10 neurons were HT, 3 neurons were MT, and no LT neuron was found. Cutaneous receptive fields were generally on the ipsilateral scrotum, perianal region, areas around tail root, and lower back. Electrolytic lesions made at the recording sites were identified (Fig. 1C). Spinal neurons with colorectal inputs were located in laminae I-III, VI, VII, and X (Fig.1C). Regional distribution of the recording sites of the spinal neurons responding to L2-L3 SCS was not different from the neurons responding to C1-C2 SCS (Fig.1C).
Fig. 1.
Response patterns and recording sites of lumbosacral spinal neurons to graded colorectal distensions (CRD). A: low-threshold excitatory response to CRD. B: high-threshold excitatory response to CRD. C: Black circles (●) represent neurons excited by CRD and inhibited by L2-L3 SCS. Open circles (○) represent neurons excited by CRD and not responding to L2-L3 SCS. C': Black squares (■) represent neurons excited by CRD and inhibited by C1-C2 SCS. Open squares (□) represent neurons excited by CRD and not responding to C1-C2 SCS. C": spinal laminae of gray matter of L6 segment drawing from Molander et al. (1989). I-X, laminae; Liss, Liss's tract; LSN, lateral spinal nucleus; Pyr, pyramidal tract; IM, intermedial nucleus.
Effects of L2-L3 SCS
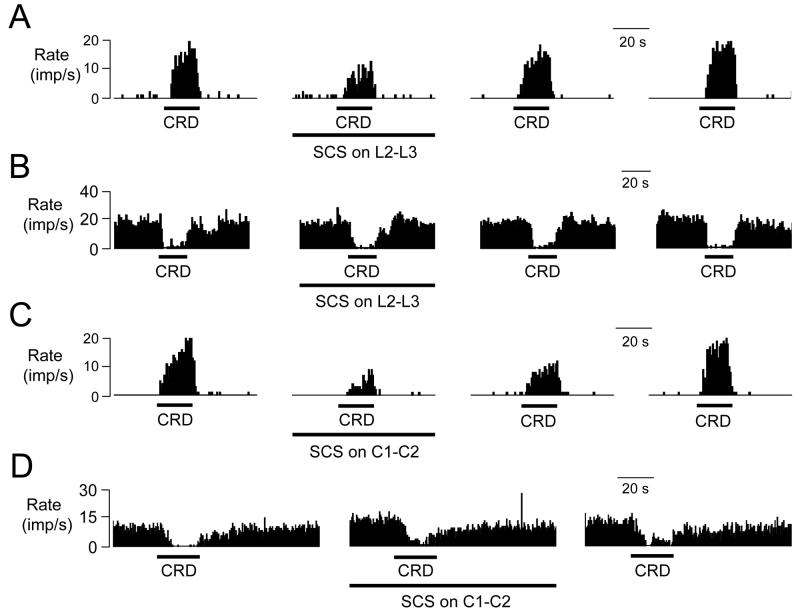
Low intensity SCS at L2-L3 spinal segments suppressed excitatory responses of 16/24 (67%) L6-S2 neurons (10 LT, 6 HT) to noxious CRD (60 mmHg, 20s); enhanced excitatory responses of 4 neurons (3 LT, 1 HT) to noxious CRD and did not affect the excitatory responses of 4 neurons (3 LT, 1 HT). However, taking the 24 tested neurons together, SCS on L2-L3 significantly reduced the total excitatory responses to CRD from 417.6±68.0 imp to 296.3±53.6 imp (P<0.05) and also shortened the duration of CRD-responses from 37.5±4.4 s to 31.0±4.2 s (P<0.05). An example of the effect of L2-L3 SCS on an excitatory response to CRD is shown in Fig. 2A. A summary of the effects of L2-L3 SCS is shown in Table 1 (n=24). Effects of L2-L3 SCS on excitatory neuronal responses to CRD lasted 10.2±1.9 min after offset of CRD (range: 3.5-25.3 min). For 4 lumbosacral spinal neurons inhibited by CRD, L2-L3 SCS did not significantly affect mean inhibitory responses to noxious CRD (409.1±112.3 imp vs 333.7±133.6 imp). Fig. 2B shows an example of a spinal neuron inhibited by CRD but unaffected by L2-L3 SCS. In addition, characteristics of somatic receptive fields for spinal neurons with colorectal input were not correlated with the responses to L2-L3 SCS (Table 2).
Fig. 2.
Effects of SCS on responses of lumbosacral spinal neurons to noxious CRD (60 mmHg, 20s). A: L2-L3 SCS suppressed the excitatory response of a spinal neuron to CRD. B: L2-L3 SCS did not affect the inhibitory response of a spinal neuron to CRD. C: C1-C2 SCS suppressed the excitatory response of a spinal neuron to CRD. D: C1-C2 SCS did not significantly affect the inhibitory response of a spinal neuron to CRD.
Table 1.
Effects of L2-L3 SCS on excitatory responses of lumbosacral spinal neurons to noxious colorectal distension (CRD, 60 mmHg, 20 s, n=24).
| L2-L3 SCS | Spontaneous activity (imp/s) |
Latency (s) | Total responses (imp) |
Duration (s) |
|---|---|---|---|---|
| Before | 4.9±1.5 | 1.9±0.3 | 417.6±68.0 | 37.5±4.4 |
| During | 5.1±1.4 | 2.6±0.5 | 296.3±53.6* | 31.0±4.2* |
| After | 6.0±1.6 | 1.6±0.1 | 521.6±91.8 | 40.3±5.8 |
P<0.05 compared with corresponding activity of before and after SCS.
Table 2.
Effects of SCS on spinal neurons excited by CRD and characteristics of somatic receptive fields.
| SCS effects | Characteristics of somatic receptive fields | ||||
|---|---|---|---|---|---|
| WDR | HT | MT | NF | ||
| L2-L3 SCS | I | 5 | 5 | 0 | 6 |
| E | 1 | 0 | 3 | 0 | |
| NR | 0 | 2 | 0 | 2 | |
| C1-C2 SCS | I | 3 | 4 | 1 | 3 |
| E | 2 | 1 | 0 | 0 | |
| NR | 1 | 0 | 1 | 2 | |
E, excitatory response to SCS. I, inhibitory response to SCS. NR, no response to SCS. WDR, wide dynamic range. HT, high threshold. MT, movement of tail. NF, not found for somatic field.
Effects of C1-C2 SCS
Application of SCS on C1-C2 segments reduced excitatory responses of 11/18 (61%) lumbosacral neurons (6 LT, 5 HT) to noxious CRD (60 mmHg, 20s); enhanced responses of 3 LT neurons to CRD and did not affect responses of 4 neurons (3 LT, 1 HT) to CRD. Taking the 18 tested neurons together, C1-C2 SCS significantly reduced total excitatory responses to CRD from 336.2±64.5 imp to 225.0±73.3 imp (P<0.05). Effects of C1-C2 SCS on excitatory neuronal responses to CRD lasted 8.0±0.9 min (range: 3.2-15.7 min) after offset of CRD. An example of inhibitory effects of C1-C2 SCS on an excitatory response to noxious CRD is shown in Fig. 2C. Characteristics of excitatory responses to CRD before, during and after C1-C2 SCS are shown in Table 3. For 4 neurons with inhibitory responses to CRD, C1-C2 SCS did not significantly alter mean inhibitory responses to noxious CRD (337.8±123.2 imp vs 326.9±166.0 imp). Fig. 2D shows a spinal neuron that was inhibited by noxious CRD but not significantly affected by C1-C2 SCS. Additionally, characteristics of somatic receptive fields for spinal neurons with colorectal input were not correlated with the responses to C1-C2 SCS (Table 2).
Table 3.
Effects of C1-C2 SCS on excitatory responses of lumbosacral spinal neurons to noxious colorectal distension (CRD, 60 mmHg, 20 s, n=18).
| C1-C2 SCS | Spontaneous activity (imp/s) |
Latency (s) | Total responses (imp) |
Duration (s) |
|---|---|---|---|---|
| Before | 5.6±1.3 | 2.0±0.4 | 336.2±64.5 | 32.2±4.9 |
| During | 3.9±1.1 | 2.3±0.6 | 225.0±73.3* | 25.3±6.6 |
| After | 4.4±1.2 | 2.4±0.4 | 293.0±92.7 | 28.7±5.7 |
P<0.05 compared with corresponding activity of before SCS.
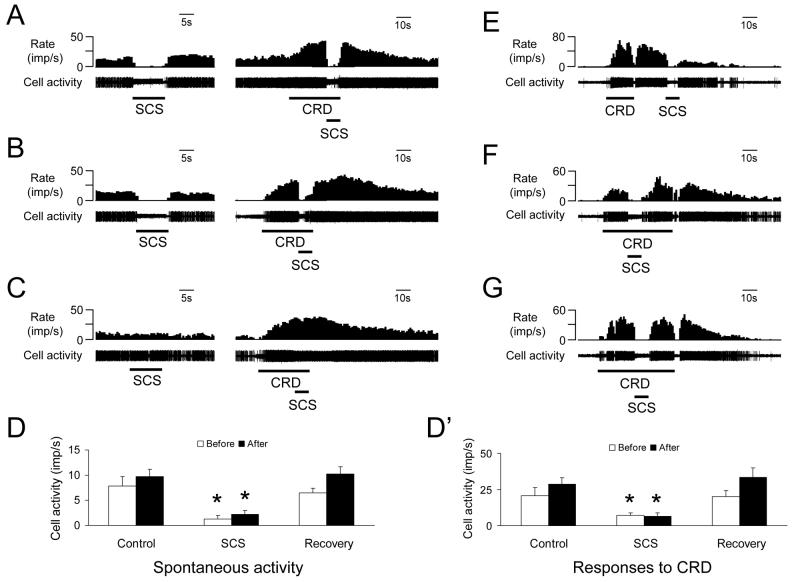
Identification of the pathways
To identify the neural pathway(s) for effects of SCS on the lumbosacral neurons with colorectal input, transections of spinal cord at the cervicomedullary junction were performed in 6 rats. The cervicomedullary transections did not affect the inhibitory effects of C1-C2 SCS on spontaneous activity and excitatory responses of the lumbosacral neuron to noxious CRD (13.7±4.8 vs 22.3±3.2 imp/s, n=6). An example of the responses of these neurons before an after transaction is shown in Fig. 3A-B and a summary for effects of C1-C2 SCS on spontaneous activity and excitatory responses to CRD before and after spinalization is shown in Fig. 3D and D'. For excitatory CRD responses of two neurons were still inhibited by SCS after cervicomedullary transaction; the pledgets with ibotenic acid did not significantly affect the inhibitory effects of C1-C2 SCS on spinal neuronal responses to CRD (Fig. 3E-G). However, transections of C7-C8 dorsal column abolished the inhibitory effects of C1-C2 SCS on excitatory response of 3 spinal neurons to noxious CRD. An example is shown in Fig. 3A-C.
Fig. 3.
Identification of the pathway for effects of SCS on activity of the lumbosacral spinal neurons responding to CRD. A-C: Inhibitory effects of C1-C2 SCS on spontaneous activity and excitatory responses of spinal neurons to noxious CRD (60 mmHg) in an animal with intact spinal cord (A), cervicomedullary transection (B) and C7 dorsal column transection (C). D, D': Summary for inhibitory effects of C1-C2 SCS on the spontaneous activity and excitatory responses of spinal neurons to noxious CRD (n=6) before and after cervicomedullary transection. * P<0.05 compared to control and recovery responses to CRD. E: C1-C2 SCS suppressed excitatory responses of a spinal neurons to CRD (60 mmHg). F-G: Cervicomedullary transection (F) and ibotenic acid (G) on C1-C2 did not affect inhibitory effect of C1-C2 SCS on excitatory responses to noxious CRD in spinal neuron E.
DISCUSSION
To our knowledge, this study is the first to describe effects of SCS on spinal neuronal neurons receiving inputs from noxious stimulation of pelvic visceral organs. Results showed that SCS, applied at clinically relevant stimulus parameters, significantly reduced excitatory responses of rat lumbosacral spinal neurons to noxious CRD. On the other hand SCS did not affect inhibitory responses to CRD. Generally, observations were similar to previous studies in which SCS effects were examined on noxious somatic inputs in STT and spinal neurons of monkeys and rats (Foreman et al. 1976; Lindblom et al. 1977; Saade et al. 1985; Yakhnisa et al. 1999; Wallin et al. 2003) and on cardiac inputs in STT neurons of monkeys (Chandler et al. 1993). Therefore, SCS does not only affect spinal neuronal processing for somatic afferent inputs but also modulates spinal neuronal responses to noxious visceral stimulation such as colorectal distension. The present study supports the idea that SCS might be useful therapy for the potential management of patients with hypersensitivity of irritable bowel syndrome and other colonic disorders.
Effects of L2-L3 SCS
Clinically, low intensity SCS often is performed at or near spinal segments that receive afferent inputs from the origin of somatic or visceral pain (Cameron 2004; Meyerson and Linderoth 2000a). To mimic the clinical SCS setting in this study, L2-L3 segments were selected for SCS because noxious colorectal input enters the spinal cord at L6-S2 segments in rats. Previously, the majority of experimental studies in animals applied SCS as single or short trains of pulses at relatively high amplitude. Such stimulation usually results in very short-lasting inhibition of nociceptive activity in the spinal dorsal horn or STT neurons with peripheral noxious inputs (Foreman et al. 1976; Chandler et al. 1993). An important characteristic of SCS in patients is that the effects often exceed the stimulus period. The present study used low-intensity (90% MT) and relatively long duration (3-5 min) and produced sustained effects after L2-L3 SCS (3.5-25.3 min) was turned off. These parameters are used in other studies that also demonstrate longer periods of inhibition of intraspinal nociceptive transmission (Lindblom et al. 1977; Rees and Roberts 1989; Yakhnitsa et al. 1999). The long lasting effects of SCS also occurred when recordings were made from neurons of the intrinsic cardiac nervous system (Armour et al., 2002). The important point of this study was these long lasting effects were observed in spinal neurons that responded to a noxious visceral stimulus.
In the present study, mean spontaneous activity for the entire group of tested neurons was not different before and after L2-L3 SCS. This finding is similar to previous reports of SCS effects on STT and spinal neurons in monkeys and rats (Chandler et al. 1993; Yakhnitsa et al. 1999), although both inhibitory and excitatory effects of SCS on spontaneous discharges were observed. Furthermore, L2-L3 SCS suppressed responses of 67% of spinal neurons excited by CRD. Based on neuronal responses to CRD, spinal neurons examined in this study were classified as low- and high-threshold responsive neurons; SCS exerted effects on both LT and HT CRD responsive neurons. Even when neurons excited or unaffected by SCS also were included, SCS significantly reduced evoked excitatory activity to noxious CRD. Chandler et al. (1993) reports that C3-C5 SCS reduces excitatory responses of all upper thoracic STT neurons to electrical stimulation of cardiopulmonary sympathetic afferent fibers and 86% of STT neurons to intracardiac injection of bradykinin in monkeys. In the present study in rats, spinal neurons but not specific projecting neurons (i.e. STT neurons) excited by noxious CRD were selected to examine the effects of SCS. The differences in species, neuronal classifications and visceral stimuli examined might explain the differences between these studies for effects of SCS on nociceptive visceral spinal inputs. However, the inhibitory effects of SCS on intraspinal visceral transmission are generally similar to other studies showing that SCS reduced activity of lumbosacral STT and spinal neurons activated by noxious thermal and mechanical stimulation of somatic fields or electrical stimulation of nerve fibers (Foreman et al. 1976; Lindblom et al. 1977).
In this study, the majority of spinal neurons responding to CRD also received convergent input from somatic fields, which were classified as WDR and HT; no LT neurons were found. The effects of SCS on activity of WDR neurons were not different from effects on HT neurons. However, for thoracic STT viscerosomatic convergent neurons receiving noxious cardiac and somatic inputs in monkeys, SCS was more likely to inhibit activity of HT neurons than activity of WDR and LT neurons (Chandler et al. 1993). Again, the difference between these results might be due to different groups of neurons studied and animal species.
Effects of C1-C2 SCS
The rostral cervical spinal cord (C1-C2) may be a source of important propriospinal regulation of visceral sensory processing in the more caudal spinal segments (Foreman 2000). Neuroanatomical and electrophysiological studies show that cell bodies of upper cervical propriospinal neurons have projections to the caudal spinal cord of monkeys (Burton and Loewy 1976), cats (Matsushita et al. 1979; Yezierski et al. 1980), and rats (Menetrey et al. 1985; Miller et al. 1998). Chemical and electrical activation of cell bodies in C1-C2 segments generally suppress responses of thoracic spinal neurons to noxious cardiac, pulmonary, and esophageal stimuli and to splanchnic nerve stimulation in rats (Poree and Schramm, 1992; Qin et al. 2004; 2006). Responses of lumbosacral STT and spinal neurons to noxious colorectal and urinary bladder distension in rats and monkeys also are reduced by activation of C1-C2 cell bodies (Qin et al. 1999; Chandler et al. 2002). These modulatory effects originating in C1-C2 spinal neurons likely descend in propriospinal pathways to reach caudal spinal segments, because supraspinal structures are not required (Poree and Schramm, 1992; Qin et al. 1999; 2004). Clinically, SCS electrode placement at a high cervical level (C2) is effective for relief of angina pectoris (Gonzalez-Darder et al. 1991); however, T1-T2 levels are often selected for inducing paraesthesias by SCS to cover the precordial chest because angina pectoris is usually referred to this region (De Jongste et al., 1994). Based on these data, C1-C2 spinal segments in the present study were selected to explore the possibility that upper cervical activation via SCS can affect colorectal neuronal transmission in the lumbosacral spinal cord for colorectal input. Results showed that effects of C1-C2 SCS suppressed excitatory responses to noxious CRD in 61% of the lumbosacral spinal neurons, which was not significantly different from effects of SCS on L2-L3 (67%). Effects of C1-C2 SCS were observed on both LT and HT responses to CRD and were not different from L2-L3 SCS. Thus, the same spinal pathway might modulate visceral transmission in lumbosacral spinal cord whether SCS is located at near (L2-L3) or distant (C1-C2) spinal segments.
Modulatory pathways and mechanism underlying SCS
In the present study, 90% MT SCS (50 Hz, 0.2 ms) at either C1-C2 or L2-L3 were performed and induced modulatory effects on activity of the lumbosacral spinal neurons with colorectal input. The effects of SCS might result from antidromic activation of primary afferent fibers in the dorsal column or from activation of the C1-C2 propriospinal pathway. Such low SCS intensities used in this study might more likely excite low-threshold large fibers (Linderoth and Foreman 1999; 2006) in the dorsal column at the C1-C2 level and might not be intense enough to excite cells bodies of the C1-C2 propriospinal pathway. The C1-C2 propriospinal pathway is proposed because chemical activation of the cell bodies with glutamate in these segments most commonly suppresses the responses of lumbosacral spinal neurons to noxious CRD (Qin et al., 1999). The results of this study showed that the effects were being transmitted by the afferent fibers in the dorsal column because transection of C7-C8 dorsal column rather than ibotenic acid at C1-C2 abolished the inhibitory effect of C1-C2 SCS on excitatory response of lumbosacral spinal neurons to noxious CRD in the present study. If the C1-C2 propriospinal pathway had contributed to the inhibitory effects, then the effects would have been attenuated or abolished because ibotenic acid is an excitotoxin that produces depolarization block of the cell bodies (Ren et al., 1990; Marini et al., 2000). Thus, it is suggested that SCS antidromically activates primary afferent axons in the dorsal column which, in turn, activate inhibitory mechanisms that modulate the processing of nociceptive information in the lumbosacral spinal neurons. A similar mechanism could be used to explain the effects of L2-L3 SCS on lumbosacral spinal neurons with noxious colorectal input, although the modulatory pathway of L2-L3 SCS to lumbosacral spinal segments was not examined by spinal dorsal column transection in the present study. It should be noted that supraspinal sites are not required because electrical excitation of dorsal column in the present study and previous studies (Yakhnitsa et al., 1999; Foreman et al., 1976; Chandler et al., 1993; Myerson and Linderoth, 2003) and chemical activation C1-C2 neurons in other studies (Qin et al. 1999; 2004) still exert effects on activity of the spinal neurons with visceral inputs after cervicomedullary spinal transection. The results of SCS do not agree with studies showing that supraspinal pathways are required to activate the inhibitory (El-Khoury et al. 2002; Rees and Roberts 1989; Saade et al. 1985). Presently, this controversy has not been resolved.
The inhibitory mechanisms of SCS on intraspinal sensory transmission are likely to be complex (Linderoth and Foreman 1999; 2006). The spinal gate-control theory (Melzack and Wall 1965) has been used to explain how low intensity stimulation of spinal dorsal column, which primarily transfers information via large afferent fibers, reduces spinal segmental transmission of colonic afferent impulses traveling in small diameter visceral fibers. While this mechanism is an attractive possibility, the inability of SCS to reduce nociceptive pain clinically limits its application (Meyerson and Linderoth, 2006). Several possibilities might explain spinal segmental mechanisms underlying suppressive effects of SCS on excitatory responses to noxious CRD observed in this study. First, dorsal column antidromic volleys evoked by SCS may collide or interfere with colorectal ascending input originating from postsynaptic dorsal column tract (PSDC) neurons X in spinal gray matter (Al-Chaer et al. 1996). However, this mechanism is unlikely, because therapeutic SCS in not perceived as being painful. If the PSDC axons are excited by SCS, then one would expect to evoke painful responses (Meyerson and Linderoth, 2003; Krames and Mousad, 2004). Second, antidromic dorsal column volleys induced by SCS have been shown to evoke inhibitory postsynaptic potentials in some STT neurons (Foreman et al. 1976). In the present study, lumbosacral spinal neurons excited by noxious CRD should include some STT and PDCT neurons. Third, antidromic impulses in dorsal columns also produce primary afferent depolarization via excitatory interneurons to elicit presynaptic inhibition for blocking noxious afferent barrages (Foreman et al. 1976). In the present study, it should be noted that SCS at either L2-L3 or C1-C2 did not significantly affect activity of lumbosacral spinal neurons inhibited by CRD. In contrast, chemical (glutamate) activation of C1-C2 cell bodies that are the origin of a descending propriospinal modulatory pathway results in an increased activity of lumbosacral spinal neurons inhibited by CRD (Qin et al. 1999). This difference supports the suggestion that the lumbosacral segmental inhibitory circuit activated by SCS is different from that elicited by chemical activation of C1-C2 propriospinal neurons. Finally, application of SCS was performed for 3-5 min but its effects on spinal neuronal activity lasted up to 25 min after cessation of SCS. The prolonged post-stimulus effect of SCS might be explained by the release and the sustained action of segmental neurotransmitters and neuromodulators. It has been demonstrated that SCS causes a decrease in the dorsal horn release of excitatory amino acids and an increase in the release of GABA in rats (Cui et al. 1997; Stiller et al. 1996).
Limitations
It is possible that colorectal distention might change the compliance of the colon (via a change in tone of the musculature) and thereby altered the distention threshold to activate spinal neurons. In a previous study we showed that the colonic pressure-volume relationship measured after SCS almost perfectly matched the responses produced before SCS (Greenwood-Van Meerveld et al. 2003). The same method for producing distention was used in the present study. This observation supports our statement that the inhibitory responses were the result of SCS modulating spinal neuronal activity and did not result from a change in colonic compliance. It has been shown that directly stimulating pelvic nerve afferent nerves from the colon with a high intensity and low frequency (12 V with trains of stimuli at 1.5 c/s, 4 shocks at 100 c/s and 0.05 msec duration) produce strong propulsive contractions of the colon (De Groat and Krier 1978). In the present studies, the stimulus intensity was much lower. In fact, the intensities were below motor threshold for activating somatic contractions. It should also be noted that single shocks or trains of stimuli applied at a higher stimulus frequency (7-15 c/s) did not generate colonic reflexes (De Groat and Krier, 1978). In the present study an even high stimulation frequency of 50 Hz was used. Additionally, SCS at the same parameters as used in this present study does not change blood pressure, heart rate and cardiac pressure-volume loops (Armour et al. 2002; Foreman et al. 2000; Kingma et al. 2001).
Potential clinical significance
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder. Abdominal pain and discomfort resulting from visceral hypersensitivity is the major complaint in patients with IBS (Posserud et al. 2006). Recent studies have demonstrated that low intensity SCS at L1 spinal segment induces a significant depression of the visceromotor behavioral response produced by CRD in rats with normal or sensitized colons. The suppressive effect of SCS on colonic hypersensitivity suggests that SCS may have therapeutic potential for the treatment of abdominal pain observed in patients with IBS (Greenwood et al. 2003; 2005). Furthermore, it has been demonstrated that SCS in a case study is effective in relieving symptoms of patients with irritable bowel syndrome (Krames and Mousad 2004). Results of the present study showed that low intensity SCS at both L2-L3 and C1-C2 segments reduced excitatory responses to noxious CRD in lumbosacral spinal neurons and, therefore, might provide a spinal mechanism for SCS suppression of abdominal pain.
ACKNOWLEDGEMENTS
The authors thank Drs. J. P. Farber and M. J. Chandler for helpful comments and D. Holston for excellent technical assistance. This study was supported by NIH grants (NS-35471, HL-075524).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Al-Chaer ED, Lawand NB, Westlund KN, Willis WD. Visceral nociceptive input into the ventral posterolateral nucleus of the thalamus: a new function for the dorsal column pathway. J Neurophysiol. 1996;76:2661–74. doi: 10.1152/jn.1996.76.4.2661. [DOI] [PubMed] [Google Scholar]
- Armour JA, Linderoth B, Arora RC, DeJongste MJ, Ardell JL, Kingma JG, Jr, Hill M, Foreman RD. Long-term modulation of the intrinsic cardiac nervous system by spinal cord neurons in normal and ischaemic hearts. Auton Neurosci. 2002;95:71–79. doi: 10.1016/s1566-0702(01)00377-0. [DOI] [PubMed] [Google Scholar]
- Burton H, Loewy AD. Descending projections from the marginal cell layer and other regions of the monkey spinal cord. Brain Res. 1976;116:485–491. doi: 10.1016/0006-8993(76)90495-9. [DOI] [PubMed] [Google Scholar]
- Cameron T. Safety and efficacy of spinal cord stimulation for the treatment of chronic pain: a 20-year literature review. J Neurosurg. 2004;100:254–267. doi: 10.3171/spi.2004.100.3.0254. [DOI] [PubMed] [Google Scholar]
- Chandler MJ, Brennan TJ, Garrison DW, Kim KS, Schwartz PJ, Foreman RD. A mechanism of cardiac pain suppression by spinal cord stimulation: implications for patients with angina pectoris. Eur Heart J. 1993;14:96–105. doi: 10.1093/eurheartj/14.1.96. [DOI] [PubMed] [Google Scholar]
- Chandler MJ, Zhang J, Qin C, Foreman RD. Spinal inhibitory effects of cardiopulmonary afferent inputs in monkeys: neuronal processing in high cervical segments. J Neurophysiol. 2002;87:1290–302. doi: 10.1152/jn.00079.2001. [DOI] [PubMed] [Google Scholar]
- Cui JG, O'Connor WT, Ungerstedt U, Linderoth B, Meyerson BA. Spinal cord stimulation attenuates augmented dorsal horn release of excitatory amino acids in mononeuropathy via a GABAergic mechanism. Pain. 1997;73:87–95. doi: 10.1016/s0304-3959(97)00077-8. [DOI] [PubMed] [Google Scholar]
- De Groat WC, Krier J. The sacral parasympathetic reflex pathway regulating colonic motility and defaecation in the cat. J Physiol. 1978;276:481–500. doi: 10.1113/jphysiol.1978.sp012248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Jongste MJ, Nagelkerke D, Hooyschuur CM, Journee HL, Meyler PW, Staal MJ, de Jonge P, Lie KI. Stimulation characteristics, complications, and efficacy of spinal cord stimulation systems in patients with refractory angina: a prospective feasibility study. Pacing Clin Electrophysiol. 1994;17:1751–60. doi: 10.1111/j.1540-8159.1994.tb03742.x. [DOI] [PubMed] [Google Scholar]
- Eliasson T, Augustinsson LE, Mannheimer C. Spinal cord stimulation in severe angina pectoris--presentation of current studies, indications and clinical experience. Pain. 1996;65:169–79. doi: 10.1016/0304-3959(95)00238-3. [DOI] [PubMed] [Google Scholar]
- El-Khoury C, Hawwa N, Baliki M, Atweh SF, Jabbur SJ, Saade NE. Attenuation of neuropathic pain by segmental and supraspinal activation of the dorsal column system in awake rats. Neuroscience. 2002;112:541–53. doi: 10.1016/s0306-4522(02)00111-2. [DOI] [PubMed] [Google Scholar]
- Foreman RD, Beall JE, Coulter JD, Willis WD. Effects of dorsal column stimulation on primate spinothalamic tract neurons. J Neurophysiol. 1976;39:534–46. doi: 10.1152/jn.1976.39.3.534. [DOI] [PubMed] [Google Scholar]
- Foreman RD, Lehew RT, Khan KA, Wienecke GM, Fitch JCK, Qin C. Abstract Viewer/Itinerary Planner. Society for Neuroscience; Washington, DC: 2005. Spinal cord stimulation modulates intraspinal visceroreceptive transmission for noxious colorectal afferent input in rats. Program No. 294.1. Online. [Google Scholar]
- Foreman RD. Integration of viscerosomatic sensory input at the spinal level. Prog Brain Res. 2000;122:209–21. doi: 10.1016/s0079-6123(08)62140-8. [DOI] [PubMed] [Google Scholar]
- Foreman RD, Linderoth B, Ardell JL, Barron KW, Chandler MJ, Hull SS, Jr, TerHorst GJ, DeJongste MJ, Armour JA. Modulation of intrinsic cardiac neurons by spinal cord stimulation: implications for its therapeutic use in angina pectoris. Cardiovasc Res. 2000;47:367–75. doi: 10.1016/s0008-6363(00)00095-x. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Darder JM, Canela P, Gonzalez-Martinez V. High cervical spinal cord stimulation for unstable angina pectoris. Stereotact Funct Neurosurg. 1991;56:20–7. doi: 10.1159/000099389. [DOI] [PubMed] [Google Scholar]
- Greenwood-Van Meerveld B, Johnson AC, Foreman RD, Linderoth B. Attenuation by spinal cord stimulation of a nociceptive reflex generated by colorectal distention in a rat model. Auton Neurosci. 2003;104:17–24. doi: 10.1016/s1566-0702(02)00262-x. [DOI] [PubMed] [Google Scholar]
- Greenwood-Van Meerveld B, Johnson AC, Foreman RD, Linderoth B. Spinal cord stimulation attenuates visceromotor reflexes in a rat model of post-inflammatory colonic hypersensitivity. Auton Neurosci. 2005;122:69–76. doi: 10.1016/j.autneu.2005.08.002. [DOI] [PubMed] [Google Scholar]
- Hautvast RW, Brouwer J, DeJongste MJ, Lie KI. Effect of spinal cord stimulation on heart rate variability and myocardial ischemia in patients with chronic intractable angina pectoris--a prospective ambulatory electrocardiographic study. Clin Cardiol. 1998;21:33–8. doi: 10.1002/clc.4960210107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson M, Simpson KH. Spinal cord stimulation in a patient with persistent oesophageal pain. Pain. 2004;112:406–8. doi: 10.1016/j.pain.2004.09.009. [DOI] [PubMed] [Google Scholar]
- Krames E, Mousad DG. Spinal Cord Stimulation Reverses Pain and Diarrheal Episodes of Irritable Bowel Syndrome: A Case Report. Neuromodulation. 2004;7:82. doi: 10.1111/j.1094-7159.2004.04011.x. [DOI] [PubMed] [Google Scholar]
- Kingma JG, Jr, Linderoth B, Ardell JL, Armour JA, DeJongste MJ, Foreman RD. Neuromodulation therapy does not influence blood flow distribution or left-ventricular dynamics during acute myocardial ischemia. Auton Neurosci. 2001;91:47–54. doi: 10.1016/S1566-0702(01)00285-5. [DOI] [PubMed] [Google Scholar]
- Lindblom U, Tapper DN, Wiesenfeld Z. The effect of dorsal column stimulation on the nociceptive response of dorsal horn cells and its relevance for pain suppression. Pain. 1977;4:133–44. doi: 10.1016/0304-3959(77)90127-0. [DOI] [PubMed] [Google Scholar]
- Linderoth B, Foreman RD. Physiology of spinal cord stimulation: review and update. Neuromodulation. 1999;2:150–164. doi: 10.1046/j.1525-1403.1999.00150.x. [DOI] [PubMed] [Google Scholar]
- Linderoth B, Foreman RD. Mechanisms of spinal cord stimulation in painful syndromes: role of animal models. Pain Med. 2006;7(Suppl 1):S14–26. [Google Scholar]
- Marini G, Ceccarelli P, Mancia M. Effects of bilateral microinjections of ibotenic acid in the thalamic reticular nucleus on delta oscillations and sleep in freely-moving rats. J Sleep Res. 2000;9:359–66. doi: 10.1046/j.1365-2869.2000.00224.x. [DOI] [PubMed] [Google Scholar]
- Matsushita M, Ikeda M, Hosoya Y. The location of spinal neurons with long descending axons (long descending propriospinal tract neurons) in the cat: a study with horseradish peroxidase technique. J. Comp. Neurol. 1979;184:63–80. doi: 10.1002/cne.901840105. [DOI] [PubMed] [Google Scholar]
- Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150:971–9. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- Menetrey D, de Pommery J, Roudier F. Propriospinal fibers reaching the lumbar enlargement in the rat. Neurosci. Lett. 1985;58:257–261. doi: 10.1016/0304-3940(85)90174-0. [DOI] [PubMed] [Google Scholar]
- Meyerson BA, Linderoth B. Spinal Cord Stimulation. In: Loeser JD, editor. Bonica's Management of Pain. 3rd ed. Lippincott Williams & Wilkins; Philadelphia: 2000a. pp. 1857–1876. Chapter 100. [Google Scholar]
- Meyerson BA, Linderoth B. Mechanisms of spinal cord stimulation in neuropathic pain. Neurol Res. 2000b;22:285–92. doi: 10.1080/01616412.2000.11740672. [DOI] [PubMed] [Google Scholar]
- Meyerson BA, Linderoth B. Spinal cord stimulation—mechanism of action in neuropathic and ischaemic pain. In: Simpson BA, editor. Electrical Stimulation and Relief of Pain, Pain Research and Clinical Management. Vol. 15. Elsevier Science B.V.; 2003. pp. 161–182. [Google Scholar]
- Meyerson BA, Linderoth B. Mode of action of spinal cord stimulation in neuropathic pain. J Pain Symptom Manage. 2006;31(4 Suppl):S6–12. doi: 10.1016/j.jpainsymman.2005.12.009. [DOI] [PubMed] [Google Scholar]
- Miller KE, Douglas VD, Richards AB, Chandler MJ, Foreman RD. Propriospinal neurons in the C1-C2 spinal segments project to the L5-S1 segments of the rat spinal cord. Brain Res. Bull. 1998;47:43–47. doi: 10.1016/s0361-9230(98)00065-3. [DOI] [PubMed] [Google Scholar]
- Molander C, Xu Q, Grant G. Cytoarchitectonic organization of the spinal cord in the rat. I. The lower thoracic and lumbosacral cord. J Comp Neurol. 1984;230:133–141. doi: 10.1002/cne.902300112. [DOI] [PubMed] [Google Scholar]
- Poree LR, Schramm LP. Role of cervical neurons in propriospinal inhibition of thoracic dorsal horn neurons. Brain Res. 1992;599:302–8. doi: 10.1016/0006-8993(92)90405-x. [DOI] [PubMed] [Google Scholar]
- Posserud I, Ersryd A, Simren M. Functional findings in irritable bowel syndrome. World J Gastroenterol. 2006;12:2830–8. doi: 10.3748/wjg.v12.i18.2830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin C, Chandler MJ, Miller KE, Foreman RD. Chemical activation of cervical cell bodies: effects on responses to colorectal distension in lumbosacral spinal cord of rats. J Neurophysiol. 1999;82:3423–33. doi: 10.1152/jn.1999.82.6.3423. [DOI] [PubMed] [Google Scholar]
- Qin C, Greenwood-Van Meerveld B, Myers DA, Foreman RD. Corticosterone acts directly at the amygdala to alter spinal neuronal activity in response to colorectal distension. J Neurophysiol. 2003;89:1343–52. doi: 10.1152/jn.00834.2002. [DOI] [PubMed] [Google Scholar]
- Qin C, Kranenburg A, Foreman RD. Descending modulation of thoracic visceroreceptive transmission by C1-C2 spinal neurons. Auton Neurosci. 2004;114:11–6. doi: 10.1016/j.autneu.2004.05.009. [DOI] [PubMed] [Google Scholar]
- Qin C, Foreman RD, Farber JP. Afferent pathway and neuromodulation of superficial and deeper thoracic spinal neurons receiving noxious pulmonary inputs in rats. Auton Neurosci. 2006 Aug 25; doi: 10.1016/j.autneu.2006.07.007. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Rees H, Roberts MH. Antinociceptive effects of dorsal column stimulation in the rat: involvement of the anterior pretectal nucleus. J Physiol. 1989;417:375–88. doi: 10.1113/jphysiol.1989.sp017807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren K, Randich A, Gebhart GF. Electrical stimulation of cervical vagal afferents. I. Central relays for modulation of spinal nociceptive transmission. J Neurophysiol. 1990;64:1098–114. doi: 10.1152/jn.1990.64.4.1098. [DOI] [PubMed] [Google Scholar]
- Saade NE, Tabet MS, Banna NR, Atweh SF, Jabbur SJ. Inhibition of nociceptive evoked activity in spinal neurons through a dorsal column-brainstem-spinal loop. Brain Res. 1985;339:115–8. doi: 10.1016/0006-8993(85)90627-4. [DOI] [PubMed] [Google Scholar]
- Stiller CO, Cui JG, O'Connor WT, Brodin E, Meyerson BA, Linderoth B. Release of gamma-aminobutyric acid in the dorsal horn and suppression of tactile allodynia by spinal cord stimulation in mononeuropathic rats. Neurosurgery. 1996;39:367–75. doi: 10.1097/00006123-199608000-00026. [DOI] [PubMed] [Google Scholar]
- Tanaka S, Barron KW, Chandler MJ, Linderoth B, Foreman RD. Low intensity spinal cord stimulation may induce cutaneous vasodilation via CGRP release. Brain Res. 2001;896:183–7. doi: 10.1016/s0006-8993(01)02144-8. [DOI] [PubMed] [Google Scholar]
- Wallin J, Fiska A, Tjolsen A, Linderoth B, Hole K. Spinal cord stimulation inhibits long-term potentiation of spinal wide dynamic range neurons. Brain Res. 2003;973:39–43. doi: 10.1016/s0006-8993(03)02530-7. [DOI] [PubMed] [Google Scholar]
- Yakhnitsa V, Linderoth B, Meyerson BA. Spinal cord stimulation attenuates dorsal horn neuronal hyperexcitability in a rat model of mononeuropathy. Pain. 1999;79:223–33. doi: 10.1016/s0304-3959(98)00169-9. [DOI] [PubMed] [Google Scholar]
- Yezierski RP, Culberson JL, Brown PB. Cells of origin of propriospinal connections to cat lumbosacral gray as determined with horseradish peroxidase. Exp. Neurol. 1980;69:493–512. doi: 10.1016/0014-4886(80)90047-3. [DOI] [PubMed] [Google Scholar]