Abstract
Objective
Previous studies have found that breastfeeding may protect infants against future overweight. One proposed mechanism is that breastfeeding, compared with bottle-feeding, may promote maternal feeding styles that are less controlling and more responsive to infant cues of hunger and satiety, thereby allowing infants greater self-regulation of energy intake. The objective of this study was to examine whether preponderance of breastfeeding in the first 6 months of life and breastfeeding duration are associated with less maternal restrictive behavior and less pressure to eat.
Methods
We studied 1160 mother–infant pairs in Project Viva, an ongoing prospective cohort study of pregnant mothers and their children. The main outcome measures were mothers’ reports of restricting their children’s food intake and of pressuring their children to eat more food, as measured by a modified Child Feeding Questionnaire (CFQ) at 1 year postpartum. Restriction was defined by strongly agreeing or agreeing with the following question from the modified CFQ: “I have to be careful not to feed my child too much.” We derived a continuous pressure to eat score from 5 questions of the modified CFQ. We used multiple logistic regression to examine the association between preponderance of breastfeeding in the first 6 months of life, breastfeeding duration, and mothers’ restriction of children’s access to food. We used multiple linear regression, both before and after adjusting for several groups of confounders, to predict the effects of breastfeeding on the mothers’ scores for pressuring their children to eat.
Results
The mean (SD) age of the women was 32.4 (4.8) years; 24% of the women were nonwhite, and 32% were primigravidas. At 6 months postpartum, 24% of the mothers were exclusively breastfeeding, 25% were mixed feeding, 41% had weaned, and 10% had fed their infants formula only. The mean (SD) duration of breastfeeding was 6.3 (4.5) months. Thirteen percent of the mothers strongly agreed or agreed with the restriction question. The mean (SD) score on the pressure to eat scale was 5.3 (3.7), and the range was 0 to 20. After adjusting for mothers’ preexisting concerns about their children’s future eating and weight status, as well as sociodemographic, economic, and anthropometric predictors of breastfeeding duration, we found that the longer the mothers breastfed, the less likely they were to restrict their children’s food intake at age 1 year. The adjusted odds ratio was 0.89 (95% confidence interval [CI]: 0.84–0.95) for each 1-month increment in breastfeeding duration. In addition, we found that compared with mothers who were exclusively formula feeding, mothers who were exclusively breastfeeding at 6 months of age had much lower odds of restricting their children’s food intake at 1 year (odds ratio: 0.27; 95% CI: 0.10–0.72). Preponderance of breastfeeding in the first 6 months of life and breastfeeding duration (β = −0.01 points on the 0–20 scale for each additional 1 month of breastfeeding [95% CI: −0.07 to 0.05]) were not related to mothers’ pressuring their children to eat more.
Conclusion
Mothers who fed their infants breast milk in early infancy and who breastfed for longer periods reported less restrictive behavior regarding child feeding at 1 year. Additional longitudinal studies should examine the extent to which any protective effect of breastfeeding on overweight is explained by decreased maternal feeding restriction.
Several recent studies suggest a protective effect of breastfeeding versus bottle-feeding of infants on future overweight.1–7 Despite differences in methods, the studies are consistent in demonstrating a reduced risk of overweight among children and adolescents who were breastfed as infants. Findings from 3 of the studies also indicate that increased duration of breastfeeding predicts lower rates of child and adolescent overweight.1,5,7
One proposed mechanism by which breastfeeding may protect against overweight is behavioral. Infants naturally regulate their energy intake, but their parents’ behavior can override cues for hunger and satiety. During infancy, it is possible that mothers who breastfeed, compared with parents who bottle-feed, may be more responsive to their infants’ signals in terms of frequency and volume of feedings.8 In this way, the mothers of breastfeeding infants may develop feeding styles that are less controlling, thereby allowing their infants to learn to self-regulate their energy intake and respond to internal appetite cues.
Several studies have examined the role of parental control over children’s eating habits in the development of childhood overweight. Using findings from cross-sectional studies, Birch et al9,10 reported that highly controlling feeding practices by parents were directly associated with poorer self-regulation of energy intake among children 3 to 5 years of age. Increased adiposity was also noted among the girls but not the boys. Increased parental feeding restriction has also been found to be associated with increased child eating and weight status.11–14 Experimental studies have shown that restricting children’s access to preferred foods increases the probability that children will consume those foods when given free access.11,12 In addition, parental feeding restrictions on girls can promote overeating,14 snack food consumption,13 and negative feelings about eating.13 In some studies, mothers’ pressure on their children to eat in the absence of hunger has been associated with disinhibited eating,15 increased child energy intake, and body weight.16,17 Three other studies, however, have failed to find an association between parental feeding behaviors and child weight status.18–20 Additional studies with larger sample sizes and broad categories of covariates are needed to examine the role of parental control over children’s eating habits.
Limited epidemiologic evidence exists regarding the relationship between breastfeeding and maternal control of infant feeding. Fisher et al21 proposed that breastfeeding may promote parenting feeding styles that are more responsive to infant cues of hunger and satiety. In a longitudinal study of 55 infants and their mothers, Fisher et al21 found that mothers who breastfed their infants for at least 12 months used lower levels of control when feeding their infants at 18 months of age. That study was limited, however, by a small sample size.21
The purpose of the present study was to examine whether type of infant feeding in the first 6 months of life and breastfeeding duration were associated with maternal control of infant feeding. We hypothesized that mothers who fed their infants breast milk in early infancy or who breastfed for longer periods would be less likely to report restricting their children’s food intake and to pressure their children to eat more.
METHODS
Subjects/Study Design
The subjects for this study were participants in Project Viva, a prospective observational cohort study of gestational diet, pregnancy outcomes, and offspring health.22 We recruited women who were attending their initial prenatal visit at 8 urban and suburban obstetric offices of a multispecialty group practice in eastern Massachusetts. Eligibility criteria included fluency in English, gestational age <22 weeks at the initial prenatal clinical appointment, and singleton pregnancy. Details of recruitment and retention procedures are available elsewhere.22 Of the 2128 women who delivered a live infant, 268 mothers disenrolled from the study, and we excluded 45 infants whose gestational age at birth was <34 weeks. At the time of analysis, 1399 subjects had reached the 1-year time point. We excluded mothers who did not return their 1-year survey within the required time period (N = 155) as well as mothers who completed a shortened telephone version of the 1-year survey, which did not include questions measuring our outcomes of interest (N = 46). Of the remaining 1198 mothers with available 1-year survey data, we excluded 31 mothers who were missing data on the main outcome measure (restriction and pressure to eat) and 7 mothers who were missing data on either breastfeeding duration or race/ethnicity. Thus, our sample size for analysis was 1160 mother–infant pairs with complete 1-year survey information.
After obtaining informed consent, we collected demographic and health history information via interviews and self-administered questionnaires. The mothers completed their interviews and self-administered questionnaires during their first trimester of pregnancy, during midpregnancy (26–28 weeks’ gestation), and 6 months postpartum; the mothers also followed up with a self-administered questionnaire at 1 year postpartum. Institutional review boards of participating institutions approved the study. All procedures were in accordance with the ethical standards for human experimentation established by the Declaration of Helsinki.
Measurements
Main Exposure
Our 2 exposures of interest were (1) type of infant feeding in the first 6 months of life and (2) duration of breastfeeding. At 6 months postpartum, we grouped women into 4 categories on the basis of their extent of breastfeeding or formula feeding. We defined exclusive breastfeeders as feeding only breast milk since birth. Mixed breastfeeding included mothers who fed their infants formula in addition to breast milk. Weaned was defined as having initiated breastfeeding but having discontinued it completely before 6 months of age. Formula feeders were mothers who had fed their infants formula only since birth. To address breastfeeding duration at 1 year postpartum, we asked women whether they had ever breastfed. Of those who reported that they had breastfed their infants for any length of time, we asked the following: “How old was your child when you stopped breastfeeding?” Response options included months, weeks, and days. We converted all responses to days for statistical analyses and reported the results in months.
Outcome Measures
The main outcome measures were the mothers’ reports of (1) restricting their children’s food intake and (2) pressuring their children to eat more food. We measured both items by a modified Child Feeding Questionnaire (CFQ) at 1 year postpartum. The CFQ is a self-report measure to assess parental beliefs, attitudes, and practices regarding child feeding and has been validated among parents of children ages 2 to 11 years.23 We made appropriate modifications to the CFQ for parents of children 1 year of age. We used confirmatory factor analysis to test a 2-factor hypothetical structure of parental control attitudes and practices in child feeding, including the use of restriction and pressuring children to eat more. Factor analysis confirmed 2 factors: restriction (1 item) and pressure to eat (5 items; Table 1).
TABLE 1.
Main Study Outcome Measures—Mothers’ Reports of Restricting Their Children’s Food Intake and Pressuring Their Children To Eat More Food—as Measured by a Modified CFQ at 1 Year Postpartum
| Domain | Questions* |
|---|---|
| Restriction | I have to be careful not to feed my child too much |
| Pressure to eat† | I often have to encourage my infant to eat more |
| I have to be sure that my infant finishes the bottle | |
| I have to be sure that my child finishes everything in the cup | |
| I have to be sure that my infant finishes all of the baby food in the jar | |
| I have to be sure that my child finishes all of the food on the plate |
All items were measured using 4-point Likert-type scales ranging from strongly agree to strongly disagree.
Items were composed using confirmatory factor analysis and expressed as a score ranging from 0 to 20, with high scores indicating a higher level of maternal pressure on the child to eat more food. Internal reliability of the 5 items, measured by standardized Cronbach α, was acceptable (α = .90). Item-to-total correlations ranged from .5 to .8.
Restriction was measured by 1 question: “I have to be careful not to feed my child too much.” Response categories were dichotomized to strongly agree/agree versus strongly disagree/disagree for statistical analyses. We derived a continuous pressure to eat score from 5 questions of the modified CFQ. All items were measured using 4-point Likert-type scales ranging from strongly agree to strongly disagree. Items were composited using confirmatory factor analysis and expressed as a score ranging from 0 to 20, with high scores indicating a higher level of maternal pressure on her child to eat. Internal reliability of the 5 items, measured by standardized Cronbach α, was acceptable (α = .90). Item-to-total correlations ranged from .5 to .8.
Mothers’ Preexisting Concerns With Infant Eating and Weight
In the midpregnancy questionnaire, at a mean age of 27 weeks’ gestation, we asked 4 questions related to the mothers’ concerns about their children’s future eating and weight status. Because maternal control of infant feeding at 12 months of age could be merely a reflection of preexisting maternal attitudes, we wanted to measure and control for these factors. Consequently, we asked the mothers the following: “Thinking ahead to when your infant is 6 months old, how concerned will you be that your infant is (1) not eating enough and (2) eating too much.” We then measured the responses using 4-point Likert-type scales ranging from “very concerned” to “no need to be concerned.” We also asked mothers, “Are you worried that your infant will become overweight as he/she is growing up?” and, “Are you worried that your infant will become underweight as he/she is growing up?” Each item was measured as a dichotomous response (ie, yes or no).
Other Measures
During the first trimester of pregnancy, the women reported their age, racial/ethnic background, education, household income, gravidity, height, and prepregnancy weight. The women’s prepregnancy body mass index (BMI) was computed using the following formula: BMI = weight/height2 (kg/m2). We obtained the infants’ birth weights from medical records. When the infants were 6 months of age, we measured their length and weight during their primary care visits. We calculated weight-for-length percentiles at 6 months on the basis of growth charts developed by the Centers for Disease Control and Prevention.24 The weight-for-length percentile at 6 months was available for 891 (77%) infants.
Statistical Analysis
We first examined the bivariate relationships of type of infant feeding, breastfeeding duration, and other covariates with the 2 main outcomes: (1) the mothers’ reports of restricting their children’s food intake and (2) the mothers’ reports of pressuring their children to eat more food. We then used multiple logistic regression models to assess the independent effects of infant feeding type and breastfeeding duration on mothers’ restricting their children’s food intake, adjusted for potential confounders. We initially performed all analyses separately by gender; however, because the results were similar, we combined the regression analyses and adjusted for gender. Multivariate model 1 was adjusted only for gender (N = 1160). Multivariate model 2 added demographic, social, economic, and anthropometric predictors of breastfeeding (maternal education, age, race/ethnicity, gravidity, prepregnancy BMI, household income, and enrollment center), as well as mothers’ preexisting concerns with their children’s future eating and weight status (N = 1031). In a subset for which we had data (N = 805), we examined the confounding effects of infants’ birth weight and 6-month weight-for-length percentiles (model 3). We reported odds ratios (ORs) and 95% confidence intervals (CIs) for the main predictor.
Using the same model-building strategy as for the restriction outcome, we used multiple linear regression to examine the effects of infant feeding type and breastfeeding duration on the mothers’ pressure to eat scores. We reported regression estimates (β) and 95% CIs for the main predictor.
Finally, using interaction terms in the multivariate models, we examined whether mothers’ gravidity and preexisting concerns with their children’s future eating and weight status modified the effects of breastfeeding on the main outcomes. We conducted all analyses using SAS, version 8.0 (Cary, NC).
RESULTS
Study Population
The study group was 76% white, 11% black, 6% Hispanic, 4% Asian, and 3% multiracial or other, with a mean (SD) age of 32.4 (4.8) years at enrollment. Thirty-two percent of the mothers had no previous pregnancies. Reflecting a generally employed and insured population, 73% of the mothers had a college degree, and ~64% had a total household income >$70 000. The mothers’ mean (SD) prepregnancy BMI was 24.5 (5.0) kg/m2; the mean reported duration of breastfeeding was 6.3 (4.5) months. At 6 months postpartum, 24% of the mothers were exclusively breastfeeding, 25% were mixed feeding, 41% had weaned, and 10% were formula feeding.
The mean birth weights (SD) for male and female infants were 3623 (536) grams and 3451 (470) g, respectively, corresponding to the 62nd and 52nd percentiles of birth weight-for-gestational age, respectively.24 At 6 months, weight-for-length percentiles were 73rd for male infants and 68th for female infants.
Mothers’ Preexisting Concerns and Breastfeeding Duration
We did not find that mothers’ preexisting concerns with their children’s becoming underweight or overweight were associated with breastfeeding duration (data not shown). Preexisting concerns about under-and overeating among infants were associated with breastfeeding duration but both in the same direction—that is, more concern with shorter breastfeeding duration.
Restriction
In bivariate analyses, mothers who had fed their infants breast milk in the first 6 months of life or who had breastfed their infants for any length of time were more likely than formula-feeding mothers to disagree with the following statement at 1 year of age: “I have to be careful not to feed my child too much” (Table 2). In addition, mean breastfeeding duration was shorter among mothers who agreed with the restriction statement. Women who were younger or who were multigravida were more likely to report restricting their children’s food intake at 1 year of age (Table 2). Likewise, women who had a higher prepregnancy BMI, lower household income, or lower educational attainment were more likely to restrict their children’s food intake at 1 year of age (Table 2). White mothers (9%) were less likely to restrict their children’s food intake at 1 year of age than were black (29%), Hispanic (23%), and Asian (24%) mothers.
TABLE 2.
Maternal and Infant Characteristics Associated With Mothers’ Restricting Their Children’s Food Intake at 1 Year Postpartum, Among 1160 Mother–Infant Pairs Who Participated in Project Viva
| Variable | “I Have to Be Careful Not to Feed My Child too Much”
|
||
|---|---|---|---|
| Agree (N = 149) | Disagree (N = 1011) | P | |
| Duration of breastfeeding in each category, mo, mean (SD) | 4.3 (4.1) | 6.6 (4.5) | <.0001 |
| Maternal age, y, mean (SD) | 31.0 (5.7) | 32.6 (4.7) | .001 |
| Prepregnancy BMI, kg/m2, mean (SD) | 25.9 (6.1) | 24.3 (4.7) | .002 |
| Infant’s birth weight, g, mean (SD) | 3555 (535) | 3535 (508) | .66 |
| Weight-for-length percentile at 6 mo, percentile, mean (SD) | 73.3 (25.7) | 70.0 (25.2) | .21 |
| Infant feeding type at 6 mo, n (%) | < .0001 | ||
| Fed only formula since birth | 19 (17) | 92 (83) | |
| Weaned | 74 (16) | 374 (84) | |
| Mixed feeding | 30 (11) | 248 (89) | |
| Fed only breast milk since birth | 13 (5) | 250 (95) | |
| Household income, n (%) | < .0001 | ||
| Don’t know | 8 (35) | 15 (65) | |
| <$20 000 | 10 (45) | 12 (55) | |
| $20 001–$40 000 | 24 (25) | 72 (75) | |
| $40 001–$70 000 | 35 (15) | 199 (85) | |
| >$70 000 | 63 (9) | 676 (91) | |
| Education, n (%) | < .0001 | ||
| High school diploma or less | 23 (29) | 57 (71) | |
| Some college | 46 (20) | 187 (80) | |
| College graduate | 48 (11) | 386 (89) | |
| Graduate degree | 32 (8) | 381 (92) | |
| Gravidity, n (%) | .04 | ||
| Primigravida | 37 (10) | 337 (90) | |
| Multigravida | 112 (14) | 674 (86) | |
| Race/ethnicity, n (%) | < .0001 | ||
| White | 79 (9) | 798 (91) | |
| Black | 37 (29) | 90 (71) | |
| Hispanic | 15 (23) | 50 (77) | |
| Asian or Pacific Islander | 12 (24) | 38 (76) | |
| Other | 6 (15) | 35 (85) | |
As shown in Fig 1, the odds of mothers’ restricting their children’s food intake decreased monotonically with increasing category of breastfeeding duration. In logistic regression analyses, the longer that the mothers breastfed their infants, the less likely the mothers were to restrict their children’s food intake at age 1 year (Table 3). For each 1-month increment in breastfeeding duration, the reduction in odds was ~10%. Adjusting for infant gender; mothers’ sociodemographic, economic, and anthropometric predictors of breastfeeding continuation; and mothers’ preexisting concerns about their children’s future eating and weight status did not materially change the association between breastfeeding duration and mothers’ restricting their children’s food intake. Similarly, adjusting for an infant’s birth weight and his or her 6-month weight-for-length percentile in the subgroup analysis did not materially change the estimate. We found that a significant interaction existed only between mothers’ gravidity and maternal restriction of their children’s food intake. The association between breastfeeding and maternal feeding restriction was slightly stronger among mothers with no previous pregnancies (OR: 0.85; 95% CI: 0.73–1.01) than among multigravidas (OR: 0.89; 95% CI: 0.83–0.96).
Fig 1.
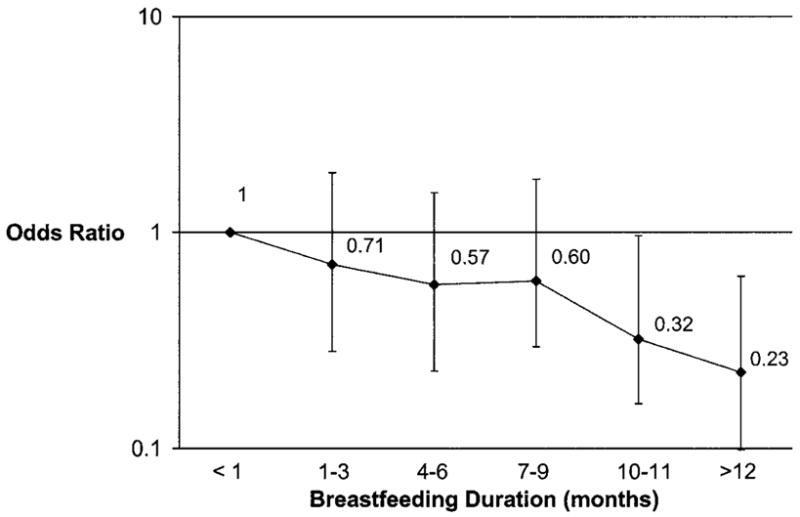
Relationship of breastfeeding duration with maternal restriction of child’s intake at age 1 year. ORs and 95% CIs for each category compared with the reference group of never breastfed or breastfed <1 month. Estimates are adjusted for gender only. P < .0001 for trend. Data from 1160 mother–infant pairs who participated in Project Viva.
TABLE 3.
Odds of Mothers’ Restricting Their Children’s Food Intake and Increment in Pressure on Child to Eat Score (0–20 Scale) at 1 Year Postpartum for Each 1-Month Increment in Breastfeeding Duration
| Model Covariates | Odds of Mothers’ Restricting Their Children’s Food Intake at Age 1 Year
|
Increment in Pressure on Child to Eat Score at Age 1 Year
|
||
|---|---|---|---|---|
| OR | 95% CI | β | 95% CI | |
| Model 1. Adjusted for gender only | 0.89 | 0.85–0.93 | −0.04 | −0.09 to 0.01 |
| Model 2. Model 1 + mother’s sociodemographic, economic, and anthropometric predictors of breastfeeding continuation* + mothers’ preexisting concerns with their children’s future eating and weight status† | 0.90 | 0.86–0.95 | −0.02 | −0.07 to 0.04 |
| Model 3. Model 2 + infants’ birth weight and 6-mo weight-for- length percentile | 0.89 | 0.84–0.95 | −0.01 | −0.07 to 0.05 |
Data from multivariate analyses of 1160 mother–infant pairs who participated in Project Viva.
Predictors include maternal education, age, race/ethnicity, gravidity, prepregnancy BMI, household income, and enrollment center.
Preexisting concerns include mother concerned that child will become overweight/underweight and mother concerned that at 6 months the child will not eat enough/will eat too much.
In multivariate models, we also found that compared with formula-feeding mothers, mothers who fed their infants breast milk only in the first 6 months of life had lower odds of restricting their children’s food intake at 1 year, even after adjusting for all potential confounders (Table 4).
TABLE 4.
Adjusted Odds of Mothers’ Restricting Their Children’s Food Intake and Increment in Pressure on Child to Eat Score (0–20 Scale) at 1 Year Postpartum Among Infant Feeding Types at 6 Months of Age
| Infant Feeding Type at 6 Months | Odds of Mothers’ Restricting Their Children’s Food Intake at Age 1 Year
|
Increment in Pressure on Child to Eat Score at Age 1 Year
|
||
|---|---|---|---|---|
| OR* | 95% CI | β* | 95% CI | |
| Fed only formula since birth | 1 | (Reference) | 0 | (Reference) |
| Weaned | 0.72 | 0.34–1.55 | 0.21 | −0.70 to 1.12 |
| Mixed feeding | 0.42 | 0.17–1.04 | 0.41 | −0.57 to 1.40 |
| Fed only breast milk since birth | 0.27 | 0.10–0.72 | 0.20 | −0.78 to 1.18 |
Data from multivariate analyses of 1160 mother–infant pairs who participated in Project Viva.
Estimates adjusted for maternal education, age, race/ethnicity, gravidity, prepregnancy BMI, household income, and enrollment center; mother’s preexisting concerns that child would become overweight/underweight; mother’s preexisting concerns that at 6 mo the child will not eat enough/will eat too much; and infant’s gender, birth weight, and 6-mo weight-for-length percentile.
Pressure to Eat
The mean (SD) pressure to eat score was 5.3 (3.7), and the range was 0 to 20. In bivariate analyses, neither type of infant feeding or breastfeeding duration was associated with maternal pressure on a child to eat more food (data not shown). Likewise, in the multivariate models, after adjusting for all groups of confounders, mothers’ pressuring their children to eat more was not associated with either breastfeeding duration (Table 3) or infant feeding type in the first 6 months of life (Table 4).
DISCUSSION
In this study, we found that mothers who fed their infants breast milk in the first 6 months of life or who breastfed them for longer periods had decreased odds of restricting their children’s food intake at 1 year. After adjusting for mothers’ preexisting concerns about their children’s future eating and weight status as well as mothers’ and infants’ sociodemographic, economic, and anthropometric predictors of breastfeeding duration, the estimated reduction in maternal feeding restriction was ~10% for each 1-month increment in breastfeeding duration. We found no association between breastfeeding and maternal pressure on a child’s food intake.
Previous studies have found that having been breastfed may protect against child and adolescent overweight.1–7 Several mechanisms have been proposed for this protective effect, including that breast-feeding may promote a balance of control in feeding across mother–infant pairs.9,25 Experimental9,10 and observational16 studies suggest a role for maternal child feeding practices in shaping how much children eat and the extent to which children are responsive to internal appetite cues to control their food intake. In a cross-sectional study of 3- to 5-year-old children, Johnson et al10 found that parents who reported using a high degree of control over what and how much their children ate had children who showed relatively little evidence of energy regulation. Similarly, among children who varied in age from 12 to 30 months, Klesges et al16 found positive correlations between the children’s relative weight and parental encouragement to eat.
In a recent systematic review of parental feeding styles and later child eating/weight status, Faith et al26 found that increased parental feeding restriction but not other feeding domains was associated with later increased eating and weight status among children. In our study, we found that breastfeeding duration was associated with less maternal restriction but not with pressure to eat. Thus, 1 underlying pathway by which breastfeeding may be related to child and adolescent overweight is through its influence on maternal feeding restriction.
Only a few studies have addressed how breast-feeding may affect maternal control of infant feeding. Evidence suggests that infants are able to adjust the volume of milk consumed to maintain a constant energy intake.8 Fomon et al8 suggested that because breastfeeding mothers are less able than bottle-feeding mothers to monitor how much milk their infants consume, the quantity of milk consumed is primarily under the infants’ control. Thus, breastfeeding may promote maternal feeding styles that are less controlling.8 It is also likely that feeding duration and intake in bottle-fed infants may be influenced by visual cues. Parents who bottle-feed their infants may be more responsive to visible milk remaining in the bottle and, consequently, more likely to have their infants finish the bottle even when satiated. This hypothesis is supported by 1 study that found that breastfed infants at 6 to 9 months consumed less nonmilk food offered to them than did bottle-fed infants.27
In the only longitudinal study that has examined the relationship between breastfeeding and maternal feeding control, Fisher et al21 found that mothers who breastfed their infants for at least 12 months used lower levels of control in feeding, including less restriction and pressure to eat, than mothers who did not breastfeed their infants for at least 12 months. That study, conducted among 55 white infants and their mothers who were followed longitudinally between the ages of 12 or 13 months to 18 months, suggested that breastfeeding may promote parenting feeding styles that are more responsive to infant cues of hunger and satiety and, thus, promote shared mother–infant regulation of food intake.21 Although they studied maternal control in feeding, Fisher et al did not separate out the association of breastfeeding with restriction versus pressure to eat, as in the current study.
Our study has several strengths, including a larger sample size and a population with more racial/ethnic diversity than the one previous study that examined the relationship between breastfeeding and maternal control of infant feeding.21 We were also able to examine multiple confounders, including a wide range of preexisting maternal concerns with infants’ future eating and weight status. Because the information on preexisting concerns regarding child future eating and weight status was collected before the infants were born, our data were not influenced by the mothers’ experiences with feeding their infants or by the sizes of the mothers’ infants.
In our analyses, we found that mothers’ preexisting concerns regarding their children’s future eating and weight status did not confound the relationship between breastfeeding and maternal feeding restriction. Thus, it is more likely that mothers learn their infant-feeding control behaviors from their infants’ cues rather than have predetermined attitudes and behaviors.
When interpreting our study, several limitations should be considered. First, although mothers in the study had diverse racial/ethnic backgrounds, their educational and income levels were relatively high. Our results may not be generalizable to more socioeconomically disadvantaged populations. In any observational study, it is possible that unmeasured characteristics might explain the observed associations between exposure and outcome. Finally, we asked only mothers who had returned to work or school whether they were using a breast pump. Therefore, we were unable to examine the differences in maternal control of infant feeding between mothers who were exclusively breastfeeding and those who were bottle-feeding expressed breast milk.
Implications
The results of our study suggest that 1 way in which breastfeeding may be protective of child and adolescent overweight is through its association with maternal feeding restriction. Additional longitudinal studies should examine the extent to which any protective effect of breastfeeding on overweight is explained by decreased maternal feeding restriction. If other studies confirm this association, then these findings may lead to new approaches for counseling both breastfeeding and bottle-feeding mothers. Encouraging mothers to initiate and continue breast-feeding, as well as teaching bottle-feeding parents strategies to promote infant self-regulation of energy intake, may decrease children’s risk of later overweight.
Acknowledgments
This study was supported in part by grants from the Centers for Disease Control and Prevention (Task Order 0957-007) and the National Institutes of Health (HD 34568, HL 64925, and HL 68041). Dr Taveras is supported in part by the Minority Medical Faculty Development Program of the Robert Wood Johnson Foundation.
The abstract of this manuscript was published as part of the proceedings of the 44th Annual Conference on Cardiovascular Disease Epidemiology and Prevention featuring the “L.J. Filer Symposium on Prevention of Overweight and Its Consequences Beginning in Youth”; San Francisco, CA; March 5, 2004.
We thank the participants and staff of Project Viva.
ABBREVIATIONS
- CFQ
Child Feeding Questionnaire
- BMI
body mass index
- OR
odds ratio
- CI
confidence interval
References
- 1.Gillman MW, Rifas-Shiman SL, Camargo CAJ, et al. Risk of overweight among adolescents who were breastfed as infants. JAMA. 2001;285:2461–2467. doi: 10.1001/jama.285.19.2461. [DOI] [PubMed] [Google Scholar]
- 2.Hediger ML, Overpeck MD, Kuczmarski RJ, Ruan WJ. Association between infant breastfeeding and overweight in young children. JAMA. 2001;285:2453–2460. doi: 10.1001/jama.285.19.2453. [DOI] [PubMed] [Google Scholar]
- 3.Bergmann KE, Bergmann RL, Von Kries R, et al. Early determinants of childhood overweight and adiposity in a birth cohort study: role of breast-feeding. Int J Obes Relat Metab Disord. 2003;27:162–172. doi: 10.1038/sj.ijo.802200. [DOI] [PubMed] [Google Scholar]
- 4.Toschke AM, Vignerova J, Lhotska L, Osancova K, Koletzko B, Von Kries R. Overweight and obesity in 6- to 14-year-old Czech children in 1991: protective effect of breast-feeding. J Pediatr. 2002;141:764–769. doi: 10.1067/mpd.2002.128890. [DOI] [PubMed] [Google Scholar]
- 5.von Kries R, Koletzko B, Sauerwald T, et al. Breast feeding and obesity: cross sectional study. BMJ. 1999;319:147–150. doi: 10.1136/bmj.319.7203.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dewey KG. Is breastfeeding protective against child obesity? J Hum Lact. 2003;19:9–18. doi: 10.1177/0890334402239730. [DOI] [PubMed] [Google Scholar]
- 7.Grummer-Strawn LM, Mei Z Centers for Disease Control and Prevention, Pediatric Nutrition Surveillance System. Does breastfeeding protect against pediatric overweight? Analysis of longitudinal data from the Centers for Disease Control and Prevention Pediatric Nutrition Surveillance System. Pediatrics. 2004;113(2) doi: 10.1542/peds.113.2.e81. Available at: www.pediatrics.org/cgi/content/full/113/2/e81. [DOI] [PubMed]
- 8.Fomon SJ, Filmer LJ, Jr, Thomas LN, Anderson TA, Nelson SE. Influence of formula concentration on caloric intake and growth of normal infants. Acta Paediatr Scand. 1975;64:172–181. doi: 10.1111/j.1651-2227.1975.tb03818.x. [DOI] [PubMed] [Google Scholar]
- 9.Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101:539–549. [PubMed] [Google Scholar]
- 10.Johnson SL, Birch LL. Parents’ and children’s adiposity and eating style. Pediatrics. 1994;94:653–661. [PubMed] [Google Scholar]
- 11.Fisher JO, Birch LL. Restricting access to foods and children’s eating. Appetite. 1999;32:405–419. doi: 10.1006/appe.1999.0231. [DOI] [PubMed] [Google Scholar]
- 12.Fisher JO, Birch LL. Restricting access to palatable foods affects children’s behavioral response, food selection, and intake. Am J Clin Nutr. 1999;69:1264–1272. doi: 10.1093/ajcn/69.6.1264. [DOI] [PubMed] [Google Scholar]
- 13.Fisher JO, Birch LL. Parents’ restrictive feeding practices are associated with young girls’ negative self-evaluation of eating. J Am Diet Assoc. 2000;100:1341–1346. doi: 10.1016/S0002-8223(00)00378-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Birch LL, Fisher JO, Davison KK. Learning to overeat: maternal use of restrictive feeding practices promotes girls’ eating in the absence of hunger. Am J Clin Nutr. 2003;78:215–220. doi: 10.1093/ajcn/78.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carper JL, Orlet Fisher J, Birch LL. Young girls’ emerging dietary restraint and disinhibition are related to parental control in child feeding. Appetite. 2000;35:121–129. doi: 10.1006/appe.2000.0343. [DOI] [PubMed] [Google Scholar]
- 16.Klesges RC, Coates TJ, Brown G, et al. Parental influences on children’s eating behavior and relative weight. J Appl Behav Anal. 1983;16:371–378. doi: 10.1901/jaba.1983.16-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klesges RC, Malott JM, Boschee PF, Weber JM. The effects of parental influences on children’s food intake, physical activity, and relative weight. Int J Eat Disord. 1986;5:335–346. [Google Scholar]
- 18.Saelens BE, Ernst MM, Epstein LH. Maternal child feeding practices and obesity: a discordant sibling analysis. Int J Eat Disord. 2000;27:459–463. doi: 10.1002/(sici)1098-108x(200005)27:4<459::aid-eat11>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 19.Robinson TN, Kiernan M, Matheson DM, Haydel KF. Is parental control over children’s eating associated with childhood obesity? Results from a population-based sample of third graders. Obes Res. 2001;9:306–312. doi: 10.1038/oby.2000.38. [DOI] [PubMed] [Google Scholar]
- 20.Baughcum AE, Powers SW, Johnson SB, et al. Maternal feeding practices and beliefs and their relationships to overweight in early childhood. J Dev Behav Pediatr. 2001;22:391–408. doi: 10.1097/00004703-200112000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Fisher JO, Birch LL, Smiciklas-Wright H, Picciano MF. Breast-feeding through the first year predicts maternal control in feeding and subsequent toddler energy intakes. J Am Diet Assoc. 2000;100:641–646. doi: 10.1016/S0002-8223(00)00190-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gillman MW, Rich-Edwards JW, Rifas-Shiman SL, Lieberman ES, Kleinman KP, Lipshultz SE. Maternal age and other predictors of newborn blood pressure. J Pediatr. 2004;144:240–245. doi: 10.1016/j.jpeds.2003.10.064. [DOI] [PubMed] [Google Scholar]
- 23.Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the Child Feeding Questionnaire: a measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite. 2001;36:201–210. doi: 10.1006/appe.2001.0398. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Growth charts. [Accessed on April 12, 2004]; Available at: www.cdc.gov/nchs/about/major/nhanes/growthcharts/datafiles.html.
- 25.Fomon SJ. Nutrition of Normal Infants. St. Louis, MO: Mosby-Yearbook; 1993. [Google Scholar]
- 26.Faith MS, Francis L, Sherry B, Scanlon K, Birch LL. Relationship between maternal feeding style and child energy intake and body composition: findings from a quantitative and qualitative literature review [abstract] Obes Res. 2001;9:123S. [Google Scholar]
- 27.Dewey KG, Heinig MJ, Nommsen LA, Lonnerdal B. Adequacy of energy intake among breast-fed infants in the DARLING study: relationships to growth velocity, morbidity, and activity levels. Davis Area Research on Lactation, Infant Nutrition and Growth. J Pediatr. 1991;119:538–547. doi: 10.1016/s0022-3476(05)82401-1. [DOI] [PubMed] [Google Scholar]


