Abstract
Endotracheal intubation has been proposed as a risk factor for temporomandibular joint dysfunction (TMD) in a limited number of published case reports and systematic studies. Symptoms may result from forces applied with the laryngoscope, or manually in an attempt to complete the intubation, and may be related to the duration in which temporomandibular joint (TMJ) structures are stressed. The objective of this study was to examine risk factors for TMD complaints associated with endotracheal intubation. One hundred twenty-two patients who underwent endotracheal intubation for surgery at the University of Washington Medical Center participated. Exclusions included surgery of the head or neck, cognitive deficit, or emergency surgery. Subjects were assessed presurgically, and at 7 and 14 days postoperatively. Gender, interincisal distance, and age were found to be significantly associated with TMD symptoms lasting as long as 14 days following intubation. For both TMD pain and TMD nonpain symptoms, the most reliable predictor of a complaint following intubation was a history of TMD complaints within a year preoperatively. Any association between endotracheal intubation and the development of short-term TMD symptoms is likely to be found in patients with prior report of such conditions, and we therefore recommend a review of TMD complaint history when planning general anesthesia.
Keywords: Intubation, TMJ, Headache, Facial pain, Mallampati
The performance of endotracheal intubation for general anesthesia has long been considered a risk factor for the development or exacerbation of temporomandibular joint dysfunction (TMD) including facial pain. A recent update of guidelines for the management of the difficult airway by the American Society of Anesthesiologists specifically recommends measures to evaluate temporomandibular joint (TMJ) function preoperatively.1,2 However, the literature in this area is limited, with only a small number of published case reports,3–9 and even fewer systematic studies.10–13 During endotracheal intubation the anesthesiologist typically attempts both rotation and translation of the TMJ to allow for the maximum opening of the patient's mouth. This maneuver allows for a successful visualization of the epiglottis and vocal cords, and consequently the atraumatic passage of an endotracheal tube. During this procedure, damage may occur to the TMJ apparatus due to excessive forces being applied either with the laryngoscope, or manually in an attempt to complete the intubation. Additionally, it is possible that damage may occur due to the length of time that the structures are in a “stressed” position, or to the positioning of the patient during the procedure for which the intubation was performed. If the patient is prone, for example, there may be force applied to the mandible during the entire procedure. Sequelae that have been reported in the cited case reports and studies include: transient or permanent jaw locking, disc dislocation, muscle pain, ear pain, and facial pain.
A 1987 report of a study of 50 patients having inhalation anesthesia via endotracheal intubation versus 50 having spinal anesthesia found significant differences between groups on the first postoperative day for several TMD-related findings including both a reduced maximum mandibular range of motion (ROM), and an increase in joint sounds postoperatively among intubated patients.9 A 1988 published report included results of 2 studies.10 In one, 140 patients requiring general anesthesia were assigned to 1 of 3 groups: orotracheal intubation, nasotracheal intubation, or face mask. There were no significant differences in demographics or preoperative TMD findings between groups. The ROM was assessed preoperatively and on each day following for 3 days. The authors found that the ROM was significantly reduced postoperatively for the group undergoing orotracheal intubation compared to the other 2 groups, although by day 3 the differences had largely disappeared. In the second study, 400 patients undergoing orotracheal intubation were interviewed postoperatively regarding TMD symptoms. While the preoperative incidence was unknown, the authors found that nearly 5% reported having TMD problems following the procedure.
A study published in 2003 reported on a sample of 68 patients who underwent endotracheal intubation and were evaluated both pre- and postoperatively.11 Their criteria for a TMJ disturbance included having at least 2 of the following signs: a reduced ROM without pain; preauricular pain and earache; or clicking or grating sounds on mandibular movement. Patients were evaluated preoperatively, and 1 day postoperatively. Nine of the 68 patients were considered to have a TMJ disturbance preoperatively. Of those with a TMJ disturbance prior to the intubation procedure, 44% (4/9) showed worsening, and 5% of those without a prior TMJ disturbance (3/59) developed TMJ disorders for the first time postoperatively. A 1999 report of closed insurance claim analyses on a large database examining airway injury during anesthesia showed that injuries to the TMJ accounted for 10% of airway trauma claims (27/266), were submitted more frequently by women (85%), and interestingly were more frequently associated with non-difficult intubations.12 Preexisting TMJ disease was documented in 30% of the 27 claims, and 16 of the 27 claims were for TMJ pain versus 11 for TMJ dislocation.
Although little studied, the potential effect of endotracheal intubation on TMJ dysfunction (TMJD) and/or facial pain is generally accepted. TMJD is a topic of discussion in most texts on general anesthesia, and an assessment for TMJ status is generally considered to be standard of care prior to administration of endotracheal intubation for general anesthesia.1,2 The purpose of this study was to assess risk factors of endotracheal intubation for short-term exacerbation or initiation of TMD.
METHODS
Subjects were recruited from among those patients who were to undergo endotracheal intubation for surgical anesthesia at the University of Washington Medical Center and who met the eligibility requirements. The inclusion criteria included being 18 years of age or older, ability to understand and speak English, and being suitable for endotracheal intubation as determined by the anesthesiologist. Exclusion criteria included planned surgery of the head or neck, existing neurological disease or cognitive impairment (as determined by the anesthesiologist), and patients receiving urgent or emergency surgery because this would not allow for informed consent and the taking of preanesthesia measurements. This study was approved by the human subjects review board of the University of Washington. Subjects were recruited as a convenience sample during a 6-week period, and 122 subjects met all eligibility requirements and consented for participation.
The primary sources of data for this study included a questionnaire administered on enrollment, preoperative measurement of interincisal distance (a measure of ROM), the anesthesia record produced by the anesthesiologist for the general anesthesia procedure, and a follow-up questionnaire used at 2 points in time after surgery (7 and 14 days). The follow-up questionnaires were administered by telephone.
The study coordinator met with subjects the morning of surgery, prior to the administration of any medications that might alter cognition, and performed the initial data collection. The preoperative questionnaire was administered orally. In addition, the study coordinator assessed prior history of, and current TMD symptoms, status, age, and gender. Interincisal distance was measured as to how wide the subject could open (using the distance between the biting edge of the upper and lower central incisors) without pain or discomfort. Following surgery, the study coordinator contacted each subject on days 7 and 14 to administer the postoperative questionnaire. Primary outcome measures for each of the 3 assessment points (baseline, 7, and 14 days) included a report of TMD pain (jaw, jaw joint, or face pain), both with and without headache, a report of TMD nonpain symptoms (clicking, grinding, locking, or pressure), limitation of range of motion, and use of pain medication on the day of assessment. Following the surgical procedure, the study coordinator obtained a copy of the anesthesia record for extraction of the Mallampati score (potential difficulty of intubation) and the duration of procedure (duration in minutes of time intubated).
The intubations of subjects included in this study were performed by a number of anesthesiologists; however, all were of a very high skill level, and all utilized the same standardized performance checklist. There were never more than 2 attempts at intubation, each lasting no more than 30 seconds. Although there was some minor variation in the equipment utilized for intubation in this study, less than 5% were with other than a Macintosh #3 blade and a 7.5-mm ID endotracheal tube. No subjects were intubated with a Sellick's maneuver, but an undetermined number had gentle tracheal pressure during intubation.
One criteria of presurgical evaluation for anesthesia involving an endotracheal intubation is the Mallampati score, which is widely used as a measure of potential difficulty of intubation and airway management (and therefore a potential risk for TMJ damage). The score is graded with the patient seated, neck extended, mouth opened as widely as possible, and tongue protruded without phonation. The scale (0–4) describes the degree of visualization of the tongue base, tonsillar pillars, uvula, and posterior pharynx.14 The criteria for scoring of the Mallampati scale are seen in Table 1.
Table 1.
Mallampati Score
All analyses were performed using SPSS-PC. Standard t-tests were used to compare group means for age, interincisal distance, and duration of intubation. Chi-square analyses were used to examine group differences in Mallampati score distributions. Multiple regression analyses were performed to examine associations between TMD pain (complaint of jaw, jaw joint, or face pain) and nonpain (complaint of clicking, grinding, pressure, or locking) measures and variables of interest. Because headache is frequently considered to be a symptom of TMD, but is also a separate entity, analyses have been performed separately for TMD pain with and without headache. TMD pain and nonpain scores are adjusted for use of pain medication on the day of assessment for all analyses since the use of pain medication may affect the pain report. Significance is considered as P < .05.
RESULTS
Baseline
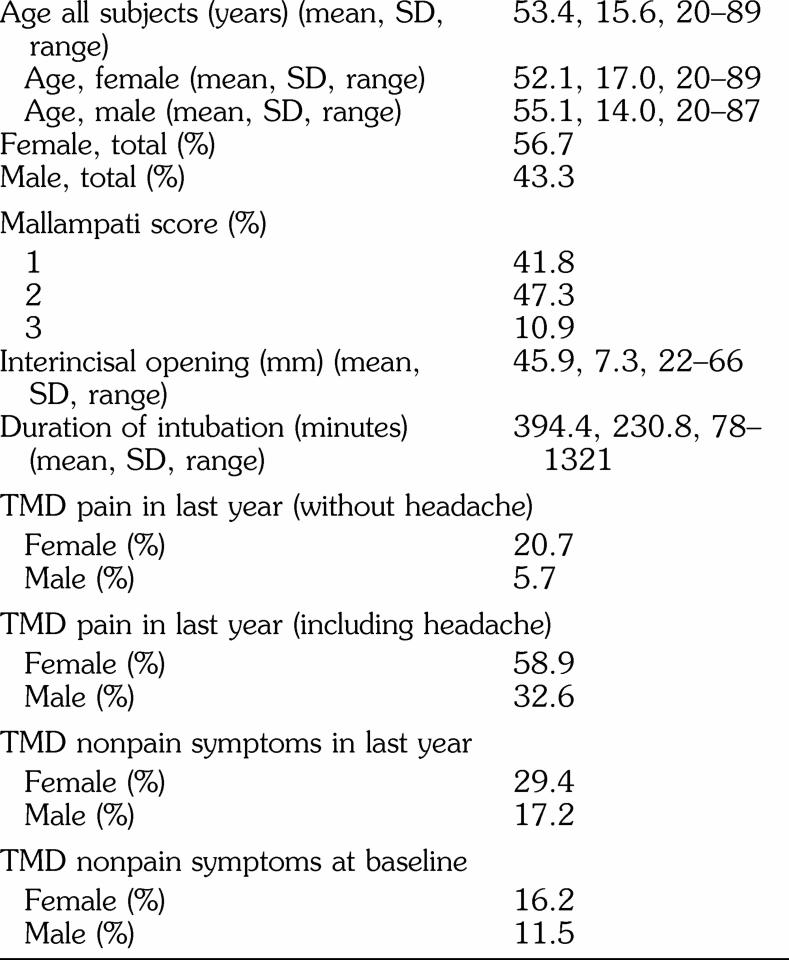
One hundred thirty-one subjects met all eligibility requirements and provided consent. Of those, 9 are not included in the analyses either because their surgery was cancelled following consent, or because the interviewer did not have time to complete the baseline interview prior to surgery. The demographics and selected characteristics of the study population at baseline (n = 122) are seen in Table 2. Male subjects were slightly, but not significantly, older than female subjects (mean male age 55.1 years [SD ± 14.0]; mean female age 52.1 years [SD ± 17.0]). Not surprisingly, male subjects demonstrated greater interincisal distance (male 49.0 mm, SD ± 6.6; female 43.6 mm, SD ± 7.1; P < .01). As expected, the Mallampati score was associated with interincisal distance (P < .01). There were no significant differences between male and female subjects for Mallampati scores or duration of intubation.
Table 2.
Characteristics of Study Population (n = 122)
From the original n of 122, there was a small loss of follow-up data at the day 7 (n = 118) and day 14 (n = 113) interviews. In all cases this was because the subject was not reached by telephone on the day of assessment. There were no significant differences for any of the demographic or study characteristics between the groups of subjects included at any of the 3 time points. Eighteen subjects reported TMD pain in the last year without headache, and 58 reported with headache.
There were significant gender differences (Table 2) for reports of TMD pain in the last year (both with and without headache included), TMD pain at baseline, and TMD nonpain symptoms (both in the last year and at baseline), with women consistently more frequently endorsing these complaints.
TMD Pain Symptoms
When looking at the total population of subjects (Table 3), neither the duration of the intubation, nor the Mallampati score are associated with a complaint of TMD pain at either the day 7 or day 14 assessments. Both gender (female) and age (increasing age) were associated with a report of TMD pain at 7 days, although the association is less strong without headache. Neither of these was associated with TMD pain at 14 days. Interincisal distance was inversely correlated with TMD pain at 7 days (adjusted for gender), but this association had disappeared by 14 days. A complaint of TMD pain both with or without headache in the last year was significantly associated with TMD pain (both with and without headache) at both the day 7 and day 14 assessments. Report of TMD nonpain symptoms are associated with report of TMD pain complaints both with and without headache at both 7 and 14 days (P < .01).
Table 3.
P Values for Associations With Complaint of “TMD Pain During Last Week,” All Subjects (TMD Pain With and Without Headache) *
When examining only those subjects who reported TMD pain in the last year, both with (n = 58) and without (n = 18) headache, again neither the duration of intubation nor the Mallampati score was associated with pain reports. Gender (female) is associated with TMD pain with headache at day 7 (P = .02), but not at day 14, and age was not associated at any time point. For those who reported TMD pain with headache in the last year, interincisal distance was inversely associated with TMD pain both with and without headache at 7 days (both P < .01), but not at 14 days. For those with TMD pain in the last year without headache, this same relationship was present for pain report without headache (P = .05), but not for those with headache.
TMD Nonpain Symptoms
When considering those TMD symptoms which were not necessarily pain-related (clicking, grinding, pressure, and locking), age, duration of intubation, and Mallampati score were not significantly associated with TMD pain with or without headache at either time point (Table 4). This was true when considering only those subjects with TMD pain with (n = 58) or without (n = 18) headache during the prior 12 months as well.
Table 4.
P Values for Associations With “TMD Nonpain Symptoms During Last Week,” All Subjects (Clicking, Grinding, Pressure, Locking) *
For all subjects, reports of TMD pain in the last year both with and without headache were significantly associated with reports of TMD nonpain symptoms at both 7 and 14 days (both P < .001, Table 4). When examining only those subjects who reported TMD pain in the last year without headache, TMD nonpain symptoms are associated with a day 14 report of TMD pain (with headache, P = .06; without headache, P = .02), but not day 7. For those with TMD pain in the last year with headache, TMD nonpain symptoms are associated with TMD pain both with and without headache at both 7 and 14 days (all P < .05).
Interincisal distance (inversely) and gender (female) are significantly associated with reports of TMD non-pain symptoms at both 7 and 14 days, although the association with gender at 7 days is marginal (P = .08, Table 4).
DISCUSSION
The ability to open the mouth in the preoperative period correlated well with the Mallampati score; however, the Mallampati score itself was not a good predictor of postoperative TMD pain or nonpain symptoms. This may be due to the fact that the Mallampati score, although a crude measure of ROM, is primarily an assessment of the relative size of the tongue to the oropharynx, and thus the ability to visualize oropharyngeal structures.
Preoperative interincisal distance, a measure of ROM was associated with pain at 7 days, but the association at 14 days was nonsignificant. This observation is consistent with clinical experience, in that the individual performing the intubation must attempt to obtain the most favorable access to the airway, and this would include a wide ROM. The operator may of necessity strain the “normal” ROM of the individual, resulting in a transitory injury to the TMJ apparatus, including the muscles of mastication. This would be most likely exhibited as a transient experience of TMD pain, as seen in this study.
Female gender was significantly associated with pre-operative TMD pain, and pain at 7 days, but this effect disappears by 14 days. Female gender was also associated with a report of TMD nonpain symptoms both at baseline and at 7 and 14 days. These findings are consistent with prior investigations of the epidemiology of TMD complaints.
Increasing age was significantly associated with TMD pain at 7 days, but as with gender, this association disappeared by 14 days. The lack of association at 14 days for gender and age may be attributed to the relatively mild and transient nature of the injury to the TMJ apparatus during intubation. The duration of intubation was not associated with TMD pain or TMD nonpain symptoms at either 7 or 14 days, suggesting that once the endotracheal tube is in place, the “strain” put on the TMJ apparatus is minimal or of little consequence.
The best predictor of both TMD pain and nonpain symptoms at either 7 or 14 days was a report of TMD pain within the last year (Tables 3 and 4). Associations were strong at both time points for both of these, regardless of a history that included headache or not.
In this study, we performed separate analyses for all subjects and those with a history of TMD pain both with and without headache. The number of subjects in the group of those with a history of TMD pain without headache was small (n = 18). This small “n” gave us limited statistical power, and in some cases, led to slightly different findings for the same risk factor. For example, for female gender at the 7-day time point, Table 3 shows P < .01 for a complaint of TMD pain with headache, but only P = .07 for a complaint of TMD pain without headache. Overall, we found no important differences between TMD pain with or without headache. This finding may serve to reinforce the common role of headache in TMD pain symptom complexes.
Interestingly, the reports of TMD nonpain symptoms generally mirror those for TMD pain. Gender and interincisal distance as well as prior history show positive associations, while Mallampati score, age, and duration of intubation do not.
All subjects included in this study were in the supine position during anesthesia, eliminating positioning as a potential source of variance. Additional potential bias may have been introduced due to both stretching of the TMJ apparatus beyond normal because of neuromuscular blockade during intubation, and to the fasciculations that succinylcholine may cause. None of the cases included in this study required more than 2 attempts at intubation, and none were noted as difficult, indicating that severe stretching of the TMJ apparatus was not an important factor. Although succinylcholine is known to introduce muscle fasciculations which can produce postoperative muscle pain, there are no reports in the literature of this pain in the muscles of mastication. Additionally, in this study population, less than 5% of subjects were treated with nondepolarizing agents, minimizing the potential for bias from this source.
CONCLUSIONS
Lesser interincisal distance, female gender, and increasing age are risk factors for a transient TMD pain experience following endotracheal intubation; however, it is clear from our data that the best predictor of postoperative TMD symptoms which may be associated with an endotracheal intubation procedure is a report of prior symptoms. In individuals with a report of prior symptoms, there is an increased reporting of symptoms which continues for as long as 2 weeks postoperatively. Therefore, it appears that it is important to continue to assess all patients preoperatively for prior TMJ symptoms, and take this into account when planning an endotracheal intubation procedure. We suggest that the addition of a brief TMD history be added to the Mallampati assessment, as well as a thorough discussion of the risk of TMD complaints following surgery for those patients at risk.
Acknowledgments
Supported by NIH Grant DE07132.
REFERENCES
- American Society of Anesthesiologists Task Force on Management. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003;98:1269–1277. doi: 10.1097/00000542-200305000-00032. [DOI] [PubMed] [Google Scholar]
- Benumof JL, Agrò FE. TMJ assessment before anaesthesia. Br J Anaesth. 2003;91:757. doi: 10.1093/bja/aeg634. [DOI] [PubMed] [Google Scholar]
- Tey HK. Difficult tracheal intubation as a result of unsuspected abnormality of the temporomandibular joint. Anaesthesia. 1986;41:436–437. doi: 10.1111/j.1365-2044.1986.tb13246.x. [DOI] [PubMed] [Google Scholar]
- Redick LF. The temporomandibular joint and tracheal intubation. Anesth Analg. 1987;66:675–676. [PubMed] [Google Scholar]
- Knibbe MA, Carter JB, Frokjer GM. Postanesthetic temporomandibular joint dysfunction. Anesth Prog. 1989;36:21–25. [PMC free article] [PubMed] [Google Scholar]
- Gould DB, Banes CH. Iatrogenic disruptions of right temporomandibular joints during orotracheal intubation causing permanent closed lock of the jaw. Anesth Analg. 1995;81:191–194. doi: 10.1097/00000539-199507000-00041. [DOI] [PubMed] [Google Scholar]
- Liu YH, Wang JJ, Chang CF, Jin CH. Difficult tracheal intubation as a result of unsuspected abnormality of the temporomandibular joint. Anesth Analg. 2001;93:783–784. doi: 10.1097/00000539-200103000-00043. [DOI] [PubMed] [Google Scholar]
- Lim BS, Andrews R. Unexpected difficult intubation in a patient with normal airway assessment. Anaesth Intensive Care. 2001;29:642–643. doi: 10.1177/0310057X0102900617. [DOI] [PubMed] [Google Scholar]
- Oofuvong M. Bilateral temporomandibular joint dislocations during induction of anesthesia and orotracheal intubation. J Med Assoc Thai. 2005;88:695–697. [PubMed] [Google Scholar]
- Lipp M, von Domarus H, Daublander M, Leyser KH, Dick W. Temporomandibular joint dysfunction after endotracheal intubation. Anaesthesist. 1987;36:442–445. [PubMed] [Google Scholar]
- Lipp M, Daublander M, Ellmauer ST, von Domarus H, Stauber A, Dick W. Changes in temporomandibular joint function following different general anesthesia techniques. Anaesthesist. 1988;37:366–373. [PubMed] [Google Scholar]
- Agrò FE, Salvinelli F, Casale M, Antonelli S. Temporomandibular joint assessment in anaesthetic practice. Br J Anaesth. 2003;50:707–708. doi: 10.1093/bja/aeg561. [DOI] [PubMed] [Google Scholar]
- Domino KB, Posner KL, Caplan RA, Cheney FW. Airway injury during anesthesia: a closed claims analysis. Anesthesiology. 1999;91:1703–1711. doi: 10.1097/00000542-199912000-00023. [DOI] [PubMed] [Google Scholar]
- Walls RM. Manual of Emergency Airway Management. Philadelphia, Pa: Lippincott Williams and Wilkins; 2001. pp. 33–34. ed. [Google Scholar]