Abstract
Background
Despite numerous clinical and regulatory efforts, problems of poor quality of care in nursing homes continue, suggesting a need for effective management practices.
Objective
To test complexity science derived hypotheses about the relationship between management practices (communication openness, participation in decision making, relationship-oriented leadership, and formalization) and resident outcomes (prevalence of aggressive behavior, restraint use, complications of immobility, and fractures), while controlling for casemix, size, ownership, and director of nursing tenure and experience.
Method
A cross-sectional, correlational, field study design was used. Primary data were obtained from directors of nursing and registered nurses employed in 164 Texas nursing homes. Investigators administered self-report surveys onsite. Secondary data were obtained from 1995 Medicaid Cost Reports and the Texas nursing home Minimum Data Set (MDS) and were linked to primary data using a unique identifier.
Results
Hypotheses were supported in that each management practice explained one or more of the resident outcomes. Larger size and longer director of nursing tenure and experience also explained better resident outcomes. Predictors explained 11% to 21% of the variance.
Discussion
We use complexity science to explain the results. The findings open the door to rethinking nursing home management practice. Practices that increase connections and interaction among people are needed for better resident outcomes.
Keywords: nursing management, complexity science, resident outcomes, nursing homes
Despite widespread concern about poor quality of care in US nursing homes and numerous efforts to improve, serious problems persist (U.S. General Accounting Office, (1999). Interestingly, we have knowledge needed to improve, such as best practice guidelines, quality improvement, models such as Wellspring (Reinhard & Stone, 2001), and tougher regulations. However, none of these efforts has yet led to broad-based improvement (Wunderlich & Kohler, 2001). Problems in adapting any knowledge in a systemized way in a nursing home, point directly to the need for effective management practices (Wunderlich & Kohler, 2001). For example, Reinhard and Stone (2001), in evaluating the Wellspring model, identified existing authoritative management practices as “stumbling blocks” and found these difficult to overcome.
Indeed, there is a growing body of knowledge available to suggest that management practices can be employed to achieve better outcomes, but these practices are not based on top down, authoritative, management styles (Anderson & McDaniel, 1999). Rather, emerging theory and research (McDaniel & Driebe, 2001) suggests that management practices that change how people relate to one another, such as communication, participation in decision making, and relationship-oriented leadership, result in better outcomes. The purpose of this study was to explore the relationship between such management practices and resident outcomes in nursing homes while controlling for organizational context and manager characteristics.
Conceptual Foundation and Literature Review
Nursing Homes as Complex Adaptive Systems
Self-organization is a central theme in complexity theory that is well documented in the physical (Prigogine, 1997) and biological (Capra, 1996) sciences. Increasingly, complexity science has been applied in health care (McDaniel & Driebe, 2001), revealing health care organizations to be complex adaptive systems. Complex adaptive systems are nonlinear systems in which diverse agents interact with each other and are capable of undergoing spontaneous self-organization (Cilliers, 1998). Self-organization is a property of all social systems that operates whether we recognize it or not. By recognizing it, however, managers can begin to influence it to facilitate better outcomes. Self-organizing is the process by which people mutually adjust their behaviors in ways needed to cope with changing internal and external environmental demands (Cilliers, 1998). As depicted in Figure 1, self-organization depends on at least three system parameters: the rate of information flow throughout the system, the nature of connections among people, and diversity of cognitive schema (Stacey, 1996). Higher levels of these system parameters provide conditions that allow people to create and recreate meaning of events; provide opportunities for higher-order learning that changes beliefs as opposed to simply knowing facts or rules; allow creativity; provide positive feedback (feedback that moves a system away from its present position); and provide opportunities for reflection and evaluation of performance. Thus, these system parameters alter the conditions necessary for self-organization, from which effective behaviors emerge. Understanding system parameters and self-organizing processes may explain why certain management practices work better than others.
Figure 1.
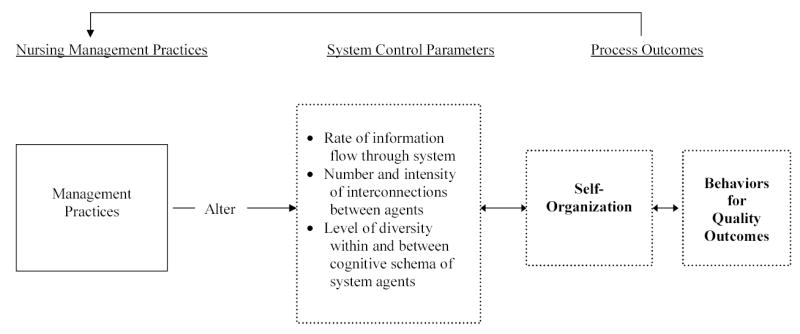
Conceptual model of depicting the expected relationship between nursing management practices, system control parameters, and self-organization. The concepts in boxes with broken-line borders were not directly measured in this study.
Management Practices and Outcomes
In this study, we view management practices as tools for altering system parameters; that is, they increase the rate of information flow, change the nature of interconnections, and provide cognitive diversity (Figure 1). The system parameters are the fuel of self-organization, from which new behaviors emerge. Thus, management practices that increase the level of the system parameters should relate to better resident outcomes. In nursing homes, because a large portion of the staff is unskilled or semi-skilled, many believe that an authoritative approach, with hierarchical (top-down) communication channels, is best. Such traditional bureaucratic approaches to management, however, impose barriers to the freedom of interaction needed for effective self-organization (Stacey, 1996). Such approaches will not stop self-organizing behavior; they will merely starve self-organizing processes of new information, diversity of perspectives or cognitive skills, and the richness of interactions required to develop useful behavior for the demands at the moment (Weick, 1993). Thus, by using primarily bureaucratic management practices, the manager is less likely to facilitate the quality of interactions needed for effectiveness. Self-organization will occur nonetheless, but the outcome is not as likely to be in a direction in keeping with organizational goals or high-quality outcomes. This does not mean that mangers should throw out all forms of structure and traditional management practices. Instead, it suggests that managers find a place between too much and too little structure where interaction, learning, and innovation are fostered. For example, a recent national IOM study (Institute of Medicine, 2001) of healthcare quality suggests a few simple rules to guide system change and a focus on relationships, interdependencies, and cooperation.
While self-organization in organizations lacks empirical indicators, management practices are empirically observable. Thus, in this study, we examine the relationship between management practices and resident outcomes, understanding that the mechanism for each relationship is through self-organization, as shown in Figure 1. Management practices included in this study, communication patterns, participation in decision making, leadership behaviors, and formalization (reliance on rules), were chosen for their theoretical potential to alter one or more system parameter (Figure 1). Figure 2 depicts the testable theoretical relationships that are derived from complexity theory.
Figure 2.
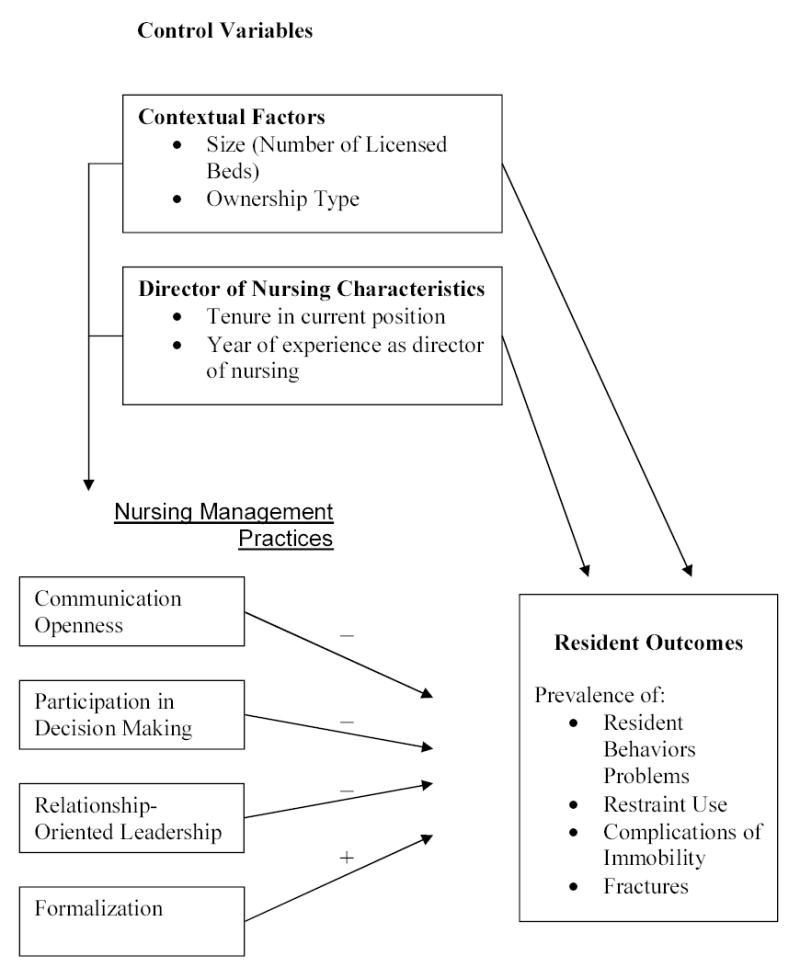
Testable theoretical model depicting the relationships between nursing management practices and resident outcomes while controlling for organizational and director of nursing characteristics.
Communication Openness.
Organizational communication is defined as the process of information flow and exchange through which explicit and tacit knowledge is conveyed. Through interaction information gains new meaning, thus, new knowledge is created, learning occurs, and new, more effective, behaviors ensue (Ashmos, Duchon, McDaniel, & Huonker, 2002). Managers who promote communication openness, therefore, will increase the rate of useful information flow among people in the organization (Figure 1), leading to better resident outcomes (Figure 2). Although we found no studies that related communication to resident outcomes, communication, research has shown its relationship to staff turnover. Moen and Nievaard (1997) found that communication skills—talking and listening—were better among managers of nursing homes and hospitals that retained their job than those that were terminated and credited success to effective communication networks. Alexander (1988), found frequency of patient care conferences were related to registered nurse (RN) turnover in hospitals. We hypothesize that:
Hypothesis 1: Greater communication openness will relate to lower prevalence of resident behavior problems, restraint use, complications of immobility, and fractures.
Participation in decision making.
Participation in decision making is the use of organizational connections and relationships to exchange information in decision making (Anderson & McDaniel, 1999). It is a strategy for altering all three system parameters (Figure 1). By increasing the number of people involved and the number of activities in which they participate, participation will increase information flow and the number and intensity of connections among people (Ashmos et al., 2002). Managers can also use participation to ensure a diversity of cognitive schema by including a variety of perspectives in decisions (Anderson & McDaniel, 1999). When more people participate, decision outcomes are created that otherwise would not have been possible (Ashmos et al., 1998). Thus resident outcomes are likely to be better (Figure 2). In prior research, participation in decision making by RNs was related to improved resident outcomes in nursing homes (Anderson & McDaniel, 1999). Mitchell, Armstrong, Simpson and Lentz (1989) conducted an in-depth case study of an intensive care unit and concluded that participation in decision making was a factor that contributed to a low mortality ratio, no new complications, and high patient satisfaction. We hypothesize that:
Hypothesis 2: Greater RN participation in decision making will relate to lower prevalence of resident behavior problems, restraint use, complications of immobility, and fractures.
Relationship-Oriented Leadership.
Leadership is traditionally defined as actions intended to influence worker behaviors. Leadership can be viewed, however, as the product of human interaction (Gardner & Avolio, 1998). Leader behaviors that are relationship oriented will foster interconnections and enhance information flow needed for effective self-organization (Figure 1) and better resident outcomes (Figure 2). In prior research, Sheridan, White, and Fairchild, (1992) found that leadership behaviors did not explain whether nursing homes failed or passed state recertification. Harris (1989), however, found that leadership behaviors contributed to fewer patient falls . We hypothesize that:
Hypothesis 3: Higher scores on relationship-oriented leadership will relate to lower prevalence of resident behavior problems, restraint use, complications of immobility, and fractures.
Formalization. Formalization is a form of centralized control whereby job descriptions, surveillance, and procedures and rules are used to ensure predictability of performance (Hage & Aiken, 1969). Nursing home managers commonly use rules because the industry is highly regulated and much of the work force is unskilled or semi-skilled. However, formalization is likely to suppress system parameters (Figure 1) because when rules exist there is no need to talk to decide what action to take and everyone is encouraged to think and act in a similar manner. Thus, self-organization is likely to be devoid of the information, connections and diversity of thought needed for effectiveness and better resident outcomes (Figure 2). We hypothesize that:
Hypothesis 4: Lower formalization will relate to higher prevalence of resident behavior problems, restraint use, complications of immobility, and fractures.
Contextual Factors and Manager’s Experience
Contextual factors are the conditions under which the organization operates. In this study, context includes size and ownership type (Figure 2). In prior research, size was found to be related to higher-than-expected pressure ulcer rates and restraint use (Zinn, Aaronson, & Rosko, 1993) but was not associated with outcomes in other studies (Anderson, Hsieh, & Su, 1998; Cherry, 1991; Spector & Takada, 1991). Some prior research has found a relationship between non-profit ownership and better residents outcomes (Aaronson, Zinn, & Rosko, 1994) while others found no relationship (Anderson et al., 1998; Intrator, Castle, & Mor, 1999). In a large study, Harrington et al. (2001) found that investor-owned nursing homes had deficiency rates on state inspection that were 43% higher than both nonprofit and public homes.
The length of tenure and experience as a director of nursing (DON) in a nursing home are likely to influence quality of resident care and are included in the study as control variables (Figure 2). The longer the DONs’ tenure, the more opportunity they have to learn the strengths and weaknesses of staff and to install and refine management practices that will positively influence resident outcomes. DONs are the primary clinical leader, they coordinate care for residents, manage nursing personnel, and attend to complex regulations (Mueller, 1998). Experience in the role, therefore, may be a critical factor in a DON’s ability to influence outcomes. A prior study found that experience of nursing home managers was related to better quality of care (Bravo, DeWals, Dubois, & Charpentier, 1999).
Methods
Sample
Proportional, stratified, random sampling was used to select a sample to represent the distribution of profits and nonprofits and geographic and racial diversity of the major metropolitan areas in Texas. We included only nursing homes that employed one or more registered nurse (RN) full-time equivalents. We invited 380 nursing homes to participate. Of those, 195 (51%) participated and 164 (43%) provided sufficient data for this analysis.
Data Collection
Secondary data were obtained from Texas Medicaid Nursing Facility 1995 Cost Reports and the Client Assessment Review and Evaluation Form 3652-A, which is part of the Texas nursing home Minimum Data Set (MDS). The cost reports provided data about size and ownership. The MDS data provided measures of resident outcomes. A procedure was in place as part of the Texas Case Mix Project to test and improve interrater reliability of the MDS data. Earlier studies of the average interrater reliability of the items from Form 3652-A were over 94% (Wilson et al., 1990).
Primary data collection consisted of survey data from nursing home staff. An investigator visited each nursing home to collect data. We presented a continuing education (CE) program as incentive to participate and asked the nursing home administrator to schedule the CE program at the most convenient times for staff to attend. Those attending were asked to complete the study questionnaire prior to the CE program.
The DONs and RNs acted as key informants, responding about patterns of behavior that they would expect in their organization, a method suggested by Seidler (1974). DONs (n = 164) provided demographic data about themselves and the nursing home. DONs and staff RNs (n= 201) provided data about their perceptions of communication openness, participation in decision making, and formalization. Staff RNs provided perceptions of relationship-oriented leadership.
Variable Measurement
Control variables.
Size was measured by the number of total licensed beds. Ownership type was measured using a dichotomous variable (0 = profit and 1 = nonprofit). DON tenure was measured by self-reported years in current position. DON years of experience was measured by self-reported total years of experience as a DON either in this nursing home or elsewhere.
Management practices.
Communication openness was defined as the extent to which people in the organization perceive that they can speak clearly and directly without fear of repercussions or misunderstanding. Communication openness was measured using the mean score from an established five item, five-point scale (Roberts & O’Reilly, 1974). Good internal consistency has been reported in previous studies with alpha coefficients ranging from .79 to .88 (Roberts & O’Reilly, 1974; Torkelson, Anderson, & McDaniel, 1996). These studies also provided evidence of construct validity through factor analysis or hypothesis testing. The alpha coefficient in our study’s sample was .83 (Table 1).
Table 1.
Independent Variables, Means,* Standard Deviations and Reliability Coefficients (N= 154–164)**
| Variable Name | M | SD | Alpha |
|---|---|---|---|
| Size (log) | 113.00 | 54.00 | |
| Owner type (% profit) shown) | 84% | ||
| DON tenure (log) | 2.70 | 4.14 | |
| DON yrs experience (log) | 5.85 | 6.50 | |
| Communication openness | 3.52 | .45 | .83 |
| Participation | 6.53 | .97 | .92 |
| Relationship-oriented lead. | 3.55 | .49 | .90 |
| Formalization | 4.05 | .42 | .83 |
Participation in decision making was defined as the extent to which RNs are involved in existing or new organizational connections and relationships for exchanging information in organizational decision making. It was measured using the Participation in Decision Making Instrument (Anderson, Ashmos, McDaniel, & Hsieh, 1997), an established measure that has demonstrated reliability (Anderson & McDaniel, 1999; Ashmos, Huonker, & McDaniel, 1998) and construct validity through factor analysis (Anderson, Issel, & McDaniel, 1997) and hypothesis testing (Ashmos et al., 1998). The instrument contains four items to measure the scope (depth and breadth) and the intensity (activities and mechanisms) of participation in decision making. The four items were repeated for each of 12 decisions commonly made in nursing homes and the resulting 48 items were averaged to obtain the scale score. Items were oriented to the professional group of RNs and thus provided an organizational level indicator. In this sample, the alpha coefficient was .92 (Table 1).
Relationship-oriented leadership was defined as the extent to which RNs perceive that their immediate supervisor (DON) comments on good job performance, considers staff feelings, and maintains good relationships with them. We used a subscale from a leadership scale previously used in nursing home research (Sheridan et al., 1992). The 28 item scale, which demonstrated reliability as well as construct validity through hypothesis testing in a nursing home study (Sheridan et al., 1992), measures several dimensions of leadership. This study used the mean score for eight, five-point items that measured relationship-oriented leadership. We obtained an alpha coefficient of .90 (Table 1).
Formalization was defined as the degree to which job descriptions, surveillance, and procedures and rules are used to ensure predictability of performance. It was measured using the mean score from six, five-point items developed by Hage and Aiken (Hage & Aiken, 1969). Validity and reliability of this measure has been demonstrated previously (Anderson et al., 1997). An alpha coefficient of .83 was obtained in this sample (Table 1).
Data aggregation
The independent measures in the study all captured the organization as the focal unit of analysis. The items in the measures of communication, participation and formalization were anchored to the organization. The items on the leadership measure asked RNs about the behavior of their immediate supervisor, the DON. Therefore, the scale scores for each measure were averaged to create one score for each nursing home. Aggregation to the organizational level was justified (Florin, Giamartino, Kenny, & Wandersman, 1990) by eta squares of .54 for communication (F = 1.45, p = .007), .54 for participation (F = .145, p = .007), .65 for leadership (F = 1.70, p = .005), and .46 for formalization although the ANOVA was not statistically significant (F = 1.07, p = .33).
Resident Outcomes.
Ten resident outcomes were included in the study as defined in Table 2. The mean scores reflect the average facility-level prevalence rate for each outcome. Prevalence was calculated as the n of residents with the condition divided by the n of residents in the nursing home. Two measures for each of the 10 outcome indicators were available at 6-month intervals in the 1995 MDS data. To reduce the influence of natural variation over time, we averaged values for each indicator from the two periods. Four outcome variables were created from the 10 items. The items are described on Table 2. We averaged three items each to measure resident behaviors, restraint use, and complications of immobility. Fractures was measured using a single item. The validity of combining these items to create the outcome variables has been demonstrated previously by Anderson et al. (1999).
Table 2.
Definitions, Means†, and Standard Deviations of the Resident Outcome Indicators (N = 164)
| Variable names | Definitions | M | SD |
|---|---|---|---|
| Percentage of residents in the facility: | |||
| Resident Behaviors | |||
| Verbal aggression | Displaying verbal aggression within last 4 weeks | 12.29 | 8.99 |
| Physical aggression | Displaying physical aggression within last 4 weeks | 8.16 | 7.09 |
| Other disruptive behavior | Displaying other disruptive behavior within last 4 weeks | 12.72 | 10.67 |
| Mean | Average prevalence of verbal, physical & other disruptive behaviors | 11.06 | 8.14 |
| Restraint Use | |||
| Geriatric-chair | For whom geriatric chair restraints were used within last 4 weeks | 7.57 | 6.11 |
| Vest-belt restraint | For whom vest-belt restraints were used within last 4 weeks | 17.93 | 9.43 |
| Wrist-mitten restraint | For whom wrist-mitten restraints were used within last 4 weeks | .69 | 1.11 |
| Mean | Average prevalence of chair, vest & wrist restraint use | 8.73 | 4.07 |
| Complications of Immobility | |||
| Decubitus ulcer | Exhibiting stage I or higher decubitus ulcer in last 4 weeks | 7.68 | 4.30 |
| Contractures | Exhibiting contracture in one or more extremities in past 4 weeks | 18.21 | 8.69 |
| Urinary tract infection | Exhibiting urinary tract infection in past 4 weeks | 3.63 | 4.30 |
| Mean | Average prevalence of decubitus contractures, & urinary tract infection | 9.84 | 4.20 |
| Fractures | For whom fracture(s) occurred within past 3 months | 2.86 | 2.83 |
Note:
Unadjusted means – interpreted as percentage of residents with the condition
We used a conservative approach for casemix adjustment to avoid unjustly attributing poor quality to a nursing home for outcomes that might actually be due to differing resident characteristic between homes (Anderson et al., 1999). To adjust for casemix, prior to analysis we removed the variance in outcomes that was due to 22 resident characteristics considered risk factors for poor outcomes. We controlled for nursing home level prevalence of problems with mobility-ambulation, dressing-grooming, transferring, eating, toileting, bladder control, bowel control, vision, hearing, functional communication, orientation-memory, seizures, level of consciousness, dyspnea, edema, tremors, stasis ulcer, amputation in past 6 months, hemi or paraplegia, quadriplegia, internal bleeding, and terminal illness. We regressed the outcome indicator on the risk factors and saved the residual as a risk-adjusted outcome variable. As has been done in prior research (Anderson et al., 1998; Anderson et al., 1999; Zinn et al., 1993), this strategy of saving residuals for analysis allowed us to control for several resident characteristics without cutting into statistical power.
Data Analysis
All variables were tested for skewness and kurtosis using the Kolmogorov-Smirnov (K-S) Test with an alpha level of p ≥ .001, considered conservative in small to moderate size samples (Tabachnick & Fidell, 1989). If the K-S was significant, the variable was transformed using a natural log. Raw mean scores are shown on the tables for ease of interpretation. Multiple linear regression models were tested for each of the four resident outcomes. Contextual variables and DON characteristics were entered first as control variables. An alpha level of p < .05 indicated statistical significance of regression results.
Results
Sample Description
The nursing homes had an average of 113 beds and 14% were non-profit (Table 1). Most of the DONs respondents were female (91%), 40 years of age or older (73%), white (83.5%), and held less than a Bachelors’ degree (67.5%). On average the DONs were in their positions for 2.70 years (SD = 4.14) with a total DON experience of 5.85 years (SD = 6.50). Most of the RN respondents were female (93%), 40 years of age or older (55%), white (54%), and held less than a Bachelors’ degree (62%). On average the RNs were in their positions for 2.49 years (SD = 5.01) and had practiced in a nursing home for 6.31 years (SD = 9.41).
Because only 43% of invited nursing homes participated in the study, we tested sample representativeness. We used independent sample t-tests to assess the differences between values for the population (n = 981, all nursing homes in Texas employing one or more RN FTE that are not part of the study sample) and the sample for resident outcomes variables and nursing home characteristics. We used Bonferroni’s adjustment to account for increased rate of Type I error due to multiple comparisons. None of the resident outcomes differed between the sample and the population. In addition, ownership type, number of licensed beds, occupancy rates, percent of private pay, and hours per resident day for RNs, licensed vocational nurses (LVNs), and certified nurse assistants (CNAs) did not differ between the sample and population. Thus, the sample represents nursing homes in Texas on the study’s dependent variables (resident outcomes) and nursing home characteristics, two of which were independent variables in this study (size and ownership type). We were not able to test for differences on the remaining independent variables because primary data were not available for the population and therefore we cannot be certain that sample does not differ from the population on these important variables.
Regression Results
The predictor variables accounted for 15% of the variance in aggressive/disruptive behavior problems (Table 3). Having more beds and greater levels of RN participation in decision making explained lower prevalence of behavior problems.
Table 3.
Regression Results: Resident Outcomes Regressed on Nursing Home Characteristics, Manager Characteristics, and Management Practices
|
Resident Behaviors (N=154) |
Restraint Use(N=152) |
Complications of Immobility(N=155) |
Fracture(N=153) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | βSE | Beta | β | βSE | Beta | β | βSE | Beta | β | βSE | Beta | |
| Log of number beds | −.043 | .015 | −.246** | −2.102 | .608 | −.287*** | −.010 | .009 | −.087 | −.009 | .005 | −.151 |
| Ownership Type | .026 | .017 | .119 | 1.285 | .715 | .135 | −.011 | .011 | −.078 | −.001 | .006 | −.014 |
| DON tenure in current position | −.001 | .004 | −.018 | −.411 | .180 | −.189* | −.001 | .003 | −.032 | .001 | .002 | .075 |
| Years experience as DON | .003 | .005 | .043 | −.481 | .219 | −.184* | −.011 | .004 | −.261** | −.001 | .002 | −.024 |
| Communication openness | −.037 | .016 | −.212 | −1.585 | .607 | −.226* | .012 | .010 | .108 | .011 | .006 | .178 |
| RN participation in decision making | −.002 | .006 | −.026* | −.061 | .244 | −.020 | .000 | .004 | .005 | −.001 | .002 | −.019 |
| Relationship oriented leadership | .004 | .013 | .026 | −.315 | .525 | −.049 | −.022 | .008 | −.222** | −.013 | .005 | −.242** |
| Formalization | −.031 | .016 | −.168 | .212 | .621 | .029 | .034 | .010 | .288** | −.004 | .007 | −.056 |
| F | 3.304 | 4.704 | 3.152 | 2.704 | ||||||||
| R square | .154 | .207 | .146 | .106 | ||||||||
| Adjusted R Square | .108 | .163 | .100 | .057 | ||||||||
| Significance level | .002 | .000 | .003 | .035 | ||||||||
p<.05
p<.01
p<.001
The predictor variables accounted for 21% of the variance in use of restraints (Table 3). Having more beds, a more experienced DON with longer tenure, and greater levels of communication openness explained lower use of resident restraints.
The predictor variables accounted for 15% of the variance in the prevalence of complications from immobility (Table 3). Employing a DON with more experience, greater relationship-oriented leadership, and less formalization explained a lower prevalence of complications of immobility.
The predictor variables accounted for 11% of the variance in the prevalence of fractures (Table 3). Greater relationship-oriented leadership explained a lower prevalence of fractures.
Discussion
Using complexity science as a framework, we explored the relationship between management practices (communication patterns, participation in decision making, leadership behaviors, and formalization) and resident outcomes (prevalence of aggressive behavior, restraint use, complications of immobility, and fractures) in 164 nursing homes. We controlled for casemix, size, ownership, and director of nursing (DON) tenure and experience. Results supported each of the hypotheses about the influence of management practices for at least one of the four resident outcomes suggesting that management practices that facilitate self-organization contribute to better resident outcomes. The results also suggest that more experience and longer tenure of the DON are important factors in achieving better resident outcomes. Complexity science is used to explain these results.
Using the theory of self-organization in complex adaptive systems, we argued that successful management practices would not be based on top down, authoritative, management. Instead, we suggested that effective self-organization requires management practices that change how people relate to one another (Ashmos et al., 2002). In particular, management practices that influence the system parameters (Stacey, 1996) for self organization—the rate of information flow through the system, the nature of connections among people, and the diversity of cognitive schema—were hypothesized to be related to better resident outcomes. While not every management practice explained every outcome, the pattern of results demonstrates that management practices that support constructive self-organization can lead to better outcomes. The fact that different management practices related to different types of resident outcomes, suggests that a variety of management practices are needed to assure better resident outcomes in nursing homes.
All four resident outcomes were explained by one or more management practice. The management practices that we studied are particularly salient to creating connection, fostering interaction among agents in a self-organizing system, and increasing cognitive diversity and they do not reflect a top-down style of management. The general culture in the nursing home industry, however, is authoritarian and top down in large part because it is a highly regulated industry and nursing homes are watched to see that they are following the rules. They are fined or even shut down if rules are violated and so attending to the rules has become part and parcel to nursing home management. In addition, the primary caregivers, certified nurse assistants (CNAs), are unskilled workers with only short training and orientation programs. Using traditional and accepted views of management, many believe that such conditions call for authoritarian management in which the rules are clear and the manager’s job is to be sure that they are followed. The results of this study, however, suggest that a different type of management is required for better outcomes, confirming the theory that effective management practices are those that support self-organization.
Specifically, greater communication openness, defined as being able to say what you mean without fear of retribution, was related to lower use of restraints. RN participation in decision making, defined as the use of existing or creation of new organizational connections and relationships to exchange information in decision making, was related to lower prevalence of aggressive/disruptive behavior among residents. Greater use of relationship-oriented leadership, defined as giving constructive feedback, helping staff resolve conflict, generating trust and being approachable, was related to two of the four resident outcomes (prevalence of complications of immobility and fractures). Formalization, defined as specifying work procedures and rules in combination with surveillance to ensure that they are followed, was higher in homes with a higher prevalence of complications of immobility.
These findings debunk the idea that top-down leadership is key to better resident outcomes. Instead, the study suggests that developing alternative management strategies—ones that increase connections and interaction among people and increase cognitive diversity—are needed. Importantly, this study also suggests that strategies for improving resident outcomes need to look beyond the traditional emphasis on clinical processes and the skills of care providers . Management practices provide a critical new lever that contributes directly to better resident outcomes.
The study also suggests that DON characteristics influence resident outcomes. Included in the models as control variables, DON tenure in current position was related to lower use of restraints and DON years of experience was related to lower prevalence of restraint use and complications of immobility. The findings suggest that when in the role of DON for a longer time, a DON is likely to accrue knowledge and expertise in both clinical and management aspects of nursing home care. These findings may be explained by looking at the role of the DON through the lens of complexity science. An experienced DON may possess a greater variety and depth of knowledge about clinical and management issues related to resident care and use her advanced knowledge to alter the type and richness of information flowing through the system, change the nature of relationships among people and to increase the diversity of alternatives available for resident care, thus supporting effective self-organization. Also, DONs with longer tenure may be better able to influence these system parameters because they are more familiar with the unique aspects of their nursing home’s staff relationships, interactions, and diversity than DONs with shorter tenure.
Finally, we found that larger size was a predictor of lower prevalence of aggressive behavior and restraint use, which is inconsistent with prior research (Zinn et al., 1993). While this finding may seem counter intuitive, complexity science provides an explanation. Larger size may facilitate constructive self-organization because size influences all three system-parameters. A greater number of connections are possible because there are more people, increasing the number of potential interactions. There is greater potential for new information flowing through the system because more people can serve as information sources and processors. When there are more people, there is a greater potential that people with different cognitive schema will interact, particularly when management practices support self-organization.
We acknowledge that our study has limitations. We cannot make statements about causation because of the correlational design. The study included nursing homes from only one state, and therefore, generalizations to nursing homes outside of Texas should be made cautiously. However, the use of a stratified random sampling procedure helped to ensure representation of geographic and racial diversity that should increase the transferability of the findings. Another limitation of the study is that the analysis included only perceptions of staff RNs and DONs. The perceptions of other levels of nursing staff, such as LVNs and CNAs, may differ from RNs and the relationship between their perceptions and resident outcomes may also differ. This raises additional questions for research.
Use of administrative data (MDS) to estimate the resident outcome variables is a potential limitation. Measures created using MDS data are not as precise as measures created using data from clinical assessment or record review. Record review, however, was not feasible in this large-scale study. The prevalence measures of resident outcomes used in this study, however, have been shown to be valid measures of quality of care in nursing homes (Rantz et al., 2000). Finally, we explained a small proportion of variance (ranging from 11% to 22%) in the dependent variable. These results, however, should be interpreted in light of two major strengths of the study’s design. First, we use multiple sources of data, thereby eliminating potential sources of common methods variance that would artificially inflate the results. Second, we used a very conservative adjustment for casemix, eliminating a significant source of error variance that might otherwise have inflated the relationship between management practices and outcomes as suggested by Anderson et al. (1999). Thus, while the amount of explained variance in our results is small, the results have practice implications.
Summary
This study provides empirical evidence of a need for the culture of the nursing home industry to change to support better resident outcomes. Change will be difficult to promote, however, because of the pervading industry culture of authoritarian, rule-based management. The study suggests nursing home administrators need to be willing to go “counter culture” in developing patterns of relationships for effective self-organization. They then need to do things to maintain stability of those patterns without trying to capture the patterns in rules and procedures. Using management practices that reinforce relationship development, rather than creating rules about who should talk to whom about what, would help to accomplish this.
Acknowledgments
The authors wish to acknowledge funding for this research from the National Institute of Nursing Research, National Institutes of Health, Grant Number 1 RO1 NR03178-01A2 (Ruth A. Anderson, PI) and the support of the Trajectories of Aging and Care Center at Duke University funded by National Institute of Nursing Research (1 P20 NR07795-01, Elizabeth Clipp, PI). We thank the Texas Health Care Association for their generous logistical support in accomplishing this research.
Contributor Information
Ruth A. Anderson, Duke University, School of Nursing, Trent Drive, DUMC 3322, Durham, NC 27710, Voice: 919-668-5105, Fax: 919-668-6210,Ruth.Anderson@duke.edu.
L. Michele Issel, School of Public Health, University of Illinois at Chicago, Chicago, IL 60612.
Reuben R. McDaniel, Jr, Professor of Management Science and Information Systems and Charles and Elizabeth Prothro Chair in Health Care Management, College of Business, The University of Texas at Austin, Austin, Texas 78712.
References
- Aaronson WE, Zinn JS, Rosko MD. Do for-profit and not-for-profit nursing homes behave differently? Gerontologist. 1994;34(6):775–786. doi: 10.1093/geront/34.6.775. [DOI] [PubMed] [Google Scholar]
- Alexander JW. The effects of patient care unit organization on nursing turnover. Health Care Management Review. 1988;13(2):61–72. doi: 10.1097/00004010-198801320-00008. [DOI] [PubMed] [Google Scholar]
- Anderson, R. A., Ashmos, D. P., McDaniel, R. R., & Hsieh, P. C. (1997). Complexity theory view of participation in decision making: Conceptual and empirical analysis. Paper presented at the Proceedings 1997 Academy of management Annual Meeting, Boston MA.
- Anderson RA, Hsieh PC, Su HF. Resource allocation and resident outcomes in nursing homes: comparisons between the best and worst. Research in Nursing & Health. 1998;21(4):297–313. doi: 10.1002/(sici)1098-240x(199808)21:4<297::aid-nur3>3.0.co;2-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson RA, ssel LM, McDaniel RRJ. Nursing staff turnover in nursing homes: A new look. Public Administration Quarterly. 1997;21(1):69–95. [Google Scholar]
- Anderson RA, McDaniel RR. RN participation in organizational decision making and improvements in resident outcomes in nursing homes. Health Care Management Review. 1999;24(1):7–16. doi: 10.1097/00004010-199901000-00002. [DOI] [PubMed] [Google Scholar]
- Anderson RA, Su HF, Hsieh PC, Allred C, Owensby S, Joiner-Rogers G. Case mix adjustment in nursing systems research: The case of resident outcomes in nursing homes. Research in Nursing and Health. 1999;22:271–283. doi: 10.1002/(sici)1098-240x(199908)22:4<271::aid-nur2>3.0.co;2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashmos DP, Duchon D, McDaniel RR, Huonker JW. What a mess! Participation as a simple managerial rule to “complexify” organizations. Journal of Management Studies. 2002;39(2):189–206. [Google Scholar]
- Ashmos DP, Huonker JW, McDaniel RR. Participation as a complicating mechanism: The effect of clinical professional and middle manager participation on hospital performance. Health Care Management Review. 1998;23(4):7–20. doi: 10.1097/00004010-199802340-00002. [DOI] [PubMed] [Google Scholar]
- Bravo G, DeWals P, Dubois M-F, Charpentier M. Correlates of care quality in long-term care facilities: A multilevel analysis. Journal of Gerontology: Psychological Sciences. 1999;54B(3):P180–P188. doi: 10.1093/geronb/54b.3.p180. [DOI] [PubMed] [Google Scholar]
- Capra, F. (1996). The web of life New York: Anchor Books Doubleday.
- Cherry RL. Agents of nursing home quality of care: ombudsmen and staff ratios revisited. Gerontologist. 1991;31(3):302–308. doi: 10.1093/geront/31.3.302. [DOI] [PubMed] [Google Scholar]
- Cilliers, P. (1998). Complexity and postmodernism: Understanding complex systems New York: Routledge.
- Florin P, Giamartino GA, Kenny DA, Wandersman A. Levels of analysis and effects: Clarifying group influence and climate by separating individual and group effects. Journal of Applied Social Psychology. 1990;20:881–900. [Google Scholar]
- Gardner WL, Avolio BJ. The charismatic relationship: A dramaturgical perspective. Academy of Management Review. 1998;23(1):32–58. [Google Scholar]
- Hage J, Aiken M. Routine technology, social structure, and organization goals. Administrative Science Quarterly. 1969;14:366–376. [Google Scholar]
- Harrington C, Woolhandler S, Mullan J, Carrilllo H, Himmelstein DU. Does investor ownership of nursing homes compromise the quality of care? American Journal of Public Health. 2001;91(9):1452–1455. doi: 10.2105/ajph.91.9.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PB. Organizational and staff attitudinal determinants of falls in nursing home residents. Medical Care. 1989;27(7):737–749. doi: 10.1097/00005650-198907000-00007. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2001). Crossing the quality chasm: A new health system for the 21st century Washington DC: National Academy Press. [PubMed]
- Intrator O, Castle NG, Mor V. Facility characteristics associated with hospitalization of nursing home residents: results of a national study. Medical Care. 1999;37(3):228–237. doi: 10.1097/00005650-199903000-00003. [DOI] [PubMed] [Google Scholar]
- McDaniel, R. R., & Driebe, D. J. (2001). Complexity Science and Health Care Management. In G. T. Savage (Ed.), Advances in Health Care Management (Vol. 2, pp. 11–36). Stamford, CT: JAI Press.
- Mitchell PH, Armstrong S, Simpson TF, Lentz M. American Association of Critical-Care Nurses Demonstration Project: Profile of excellence in critical care nursing. Heart & Lung: Journal of Critical Care. 1989;18(3):219–237. [PubMed] [Google Scholar]
- Moen J, Nievaard AC. Orientational research into dismissed managers in health care. Health Care Management Review. 1997;22(3):92–96. [PubMed] [Google Scholar]
- Mueller CH. LTC directors of nursing define education needs. Nursing Management. 1998;29(11):39–42. [PubMed] [Google Scholar]
- Prigogine, I. (1997). The end of certainty: Time, chaos, and the new laws of nature New York: The Free Press.
- Rantz MJ, Mehr DR, Petroski GF, Madsen RW, Popejoy LL, Hicks LL, Conn VS, Grando VT, Wipke-Tevis DD, Bostick J, Porter R, Zwygart-Stauffacher M, Maas M. Initial field testing of an instrument to measure observable indicators of nursing home care quality. Journal of Nursing Care Quality. 2000;14(3):1–12. doi: 10.1097/00001786-200004000-00002. [DOI] [PubMed] [Google Scholar]
- Reinhard, S., & Stone, R. (2001). Promoting quality in nursing homes: The Wellspring Model (432). New York: The Commonwealth Fund.
- Roberts K, O’Reilly C. Measuring organizational communication. Journal of Applied Psychology. 1974;59:321–326. [Google Scholar]
- Seidler J. On using informants: Technique for collecting quantitative data and controlling measurement error in organization analysis. American Sociological Review. 1974;39:816–831. [Google Scholar]
- Sheridan JE, White J, Fairchild TJ. Ineffective staff, ineffective supervision, or ineffective administration? Why some nursing homes fail to provide adequate care. The Gerontologist. 1992;32(3):334–341. doi: 10.1093/geront/32.3.334. [DOI] [PubMed] [Google Scholar]
- Spector WD, Takada HA. Characteristics of nursing homes that affect resident outcomes. Journal of Aging and Health. 1991;3(4):427–454. doi: 10.1177/089826439100300401. [DOI] [PubMed] [Google Scholar]
- Stacey, R. D. (1996). Complexity and creativity in organizations San Francisco: Berrett-Koehler Publishers.
- Tabachnick, B. G., & Fidell, L. S. (1989). Using multivariate statistics (Second ed.). New York: Harper Collins Publishers.
- Torkelson DJ, Anderson RA, McDaniel RRJ. Interventions in response to chemically dependent nurses: Effect of context and interpretation. Research in Nursing & Health. 1996;19(2):153–162. doi: 10.1002/(SICI)1098-240X(199604)19:2<153::AID-NUR7>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- U. S. General Accounting Office. (1999). Nursing homes: Additional steps needed to strengthen enforcement of Federal quality standards. Report to the Special Committee on Aging, U.S. Senate (HEHS-99-46). Washington, DC: U.S. General Accounting Office.
- Weick KE. The collapse of sensemaking in organizations: The Mann Gulch disaster. Administrative Science Quarterly. 1993;38(4):628–652. [Google Scholar]
- Wilson, S., Boulter, C., McDonald-Robers, P., Buchanan, R., Godbout, R., Malitz, D., & Lorenzen, S. (1990). Texas nursing home case mix project: Quarterly progress report Austin TX: Texas Department of Human Services.
- Wunderlich, G. S., & Kohler, P. O. (2001). Improving quality in long-term care Washington, D.C.: National Academy Press, Division of Health Care Services.
- Zinn JS, Aaronson WE, Rosko MD. Variations in the outcomes of care provided in Pennsylvania nursing homes. Facility and environmental correlates Medical Care. 1993;31(6):475–487. doi: 10.1097/00005650-199306000-00001. [DOI] [PubMed] [Google Scholar]


