Abstract
Causes of the burgeoning cardiovascular epidemic in developing countries (DC) are known. Whilst there are many prevention strategies and policies demonstrated to be effective in reducing the trends of cardiovascular disease in developed countries, applying them in DCs is challenging and complex. To utilize resources efficiently, two key decisions have to be made by policy makers in all DCs. The first is to decide on the appropriate mix of population and high-risk interventions. The second is to determine the threshold for implementing high-risk interventions. In making such decisions, due consideration needs to be given to scientific evidence, affordability, sustainability, opportunity costs, and social and political realities. High-risk approaches can be made cost-effective if individuals that are most likely to benefit from treatment can be identified through risk stratification systems. Although several such risk prediction systems are available, they have limited applicability to non-Western populations. Further, health systems in DCs do not have basic infrastructure facilities to support resource intensive risk prediction tools, particularly in primary healthcare. The World Health Organization has developed a flexible cardiovascular disease risk management package that is implemented in a range of less resourced settings. A risk prediction tool that enables more accurate prediction of cardiovascular risk in DCs is in development.
Keywords: prevention, cardiovascular risk prediction, developing countries
Cardiovascular disease (CVD) is a major cause of mortality and morbidity worldwide. Currently, 80% of deaths and 87% of disability due to CVD occur in developing countries (WHO 2002a, 2003a). CVD is already placing a heavy burden on the health services of developing countries, which are barely coping with communicable diseases. Effective strategies for the prevention and control of CVD are imperative.
Causes of CVD are known
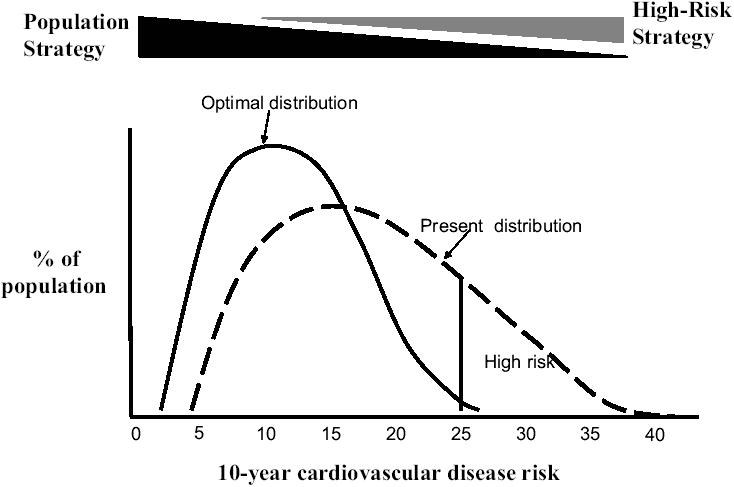
Tobacco use, physical inactivity, and unhealthy diet and their intermediate manifestations – hypertension, hyperlipidemia, and hyperglycemia – explain at least 75% of the CVD burden (Magnus and Beaglehole 2001; Emberson et al 2004; Yusuf et al 2004). Other established risk factors for CVD include age, gender, obesity, personal history of CVD, family history of CVD, and socioeconomic position. These risk factors often cluster together (Ebrahim 2004). At any given time, about 5%–10% of the population are at very high risk of developing cardiovascular events (Figure 1). A much larger segment of the population is at moderate risk. If no preventive action is taken, individuals at the tail end of the distribution will develop fatal and nonfatal cardiovascular events. Many more events will occur in the segment of the population with modest elevation of risk, as the number of individuals in this segment is larger. As such, it is essential that population-based strategies are used to shift the risk distribution of the whole population to the left, and that high-risk strategies are used to deal with those at very high risk and for whom drug treatment may be indicated (WHO 2001, 2003b). These preventive strategies are complimentary and synergistic, and dovetail into each other in terms of targeting risk groups. The World Health Report (2002) examined the cost-effectiveness of several population-wide strategies to reduce cardiovascular risk (WHO 2002a). The combination of population-based cholesterol reduction strategies with interventions to reduce salt intake at the population level was found to be very cost-effective in all settings. The most attractive population-wide strategies were salt reduction at a population level through legislation and voluntary agreements, health education through mass media focusing on blood pressure cholesterol and body mass, and promoting fruit and vegetable intake through national education campaigns (WHO 2002a).
Difficulties in implementing what is known
For effective prevention and control of CVD there are two major policy questions that need to be addressed upfront. The first question is how to strike an appropriate balance between population-based and high-risk approaches. The second is where to place the threshold for implementing high-risk strategies. There are no blueprints for the process, and the answers will depend on the economic, political, and social realities of each country. For example, very low-income countries may have to decide to place the threshold for implementing high-risk strategies at a 10-year risk of CVD at 30%. Other countries with additional resources may lower it to 20%. As the threshold is lowered, health benefits increase and costs escalate. Making these decisions is so challenging that decision makers often avoid addressing the above questions through an explicit and transparent process.
Given the limited healthcare resources, high-risk approaches also need to be prioritized. They need to first target the following segments of the population who are in greatest need and are most likely to benefit. This includes people with:
established coronary heart disease, cerebrovascular disease, peripheral vascular disease, and other types of heart disease;
diabetes and nephropathy;
genetic lipid disorders such as familial hyper-cholesterolemia;
no apparent CVD but at high risk of developing atherosclerotic disease because of markedly elevated single risk factors (eg, total cholesterol ≥ 8 mmol/L or blood pressure ≥ 180/110 mmHg);
no apparent CVD but at high risk of developing atherosclerotic vascular disease due to a combination of cardiovascular risk factors;
metabolic syndrome.
At present in most developing countries there are no organized schemes for detecting the above categories of individuals. Primary care has an important role to play in the effective delivery of high-risk strategies as the majority of the population has contact with primary care for their health needs. However, currently, human resource and infrastructure capacity at primary care level in most developing countries is grossly inadequate to serve this function (Mendis et al 2004). With current levels of healthcare expenditure, most developing countries are also in no position to upgrade primary healthcare facilities to take on these tasks of screening, diagnosis, and effective intervention for chronic conditions that need lifelong care. Further, if due to resource constraints such services do not cover the entire population, it may result in widening of inequities in the distribution of resources for health.
Recommended approach to cardiovascular risk assessment
As alluded to above, risk factors often cluster together and the majority of cardiovascular events occur in individuals with modest elevations of several risk factors than in individuals with marked elevation of a single risk factor. Therefore, focusing on cholesterol or blood pressure levels separately to identify high-risk individuals is not cost-effective. A more cost-effective approach is to base treatment decisions on each individual's risk of a cardiovascular event in the foreseeable future (WHO 2003a). This approach enables the selection of those that are most likely to benefit from treatment through risk stratification and improves health outcomes. It is of particular importance to settings with scarce resources.
To date, several risk prediction equations have been developed to measure an individual's absolute risk of a cardiovascular event over a specified time period. These equations have largely been derived from highly selected populations. The Framingham coronary heart disease risk function is the most widely used method for assessment of cardiovascular risk. It is derived by observing the cumulative number of cardiovascular events in the original Framingham cohort and subjects of the Framingham offspring study who were followed for 4–12 years (Anderson et al 1990). The Framingham analysis forms the basis of some commonly used guidelines and risk tables such as the Sheffield and New Zealand tables. Although Framingham risk equations give an acceptable prediction of risk in North American populations, they have been shown to substantially overestimate the risk for other populations (Brindle et al 2003). The European SCORE project has developed risk assessment charts using pooled data from 12 European cohorts, and these are applicable only to European populations (Conroy et al 2003).
Applying risk prediction systems in developing countries
There are complex challenges in applying cardiovascular risk prediction systems in developing countries. Health systems in low-income countries do not have basic infrastructure facilities to support resource intensive risk prediction tools, particularly in primary healthcare. WHO has developed a flexible CVD risk management package that can be implemented with the infrastructure available in a range of less resourced settings (WHO 2002c, 2002d). This package enables cardiovascular risk to be stratified into low, medium, and high-risk categories based on history, blood pressure measurement, and urine analysis.
A risk prediction tool that enables more accurate prediction of cardiovascular risk in non-Western populations is been developed. It uses gender, blood pressure, smoking status, diabetes, and total cholesterol to quantify the 10-year cardiovascular risk. In settings where total cholesterol assay is not routinely available average values derived from national surveys could be used as default concentrations. Serum lipid assays could then be done only in those with an initial coronary risk above a predetermined cutoff level (eg, 30% or more risk of CVD in 10 years). This would help to further select those who would benefit most from treatment, and guide the intensity and nature of drug treatment. Developing a simple and accurate risk prediction tool that is sufficiently flexible to be used in a variety of resource settings is a challenge. Due consideration also needs to be given to opportunity costs and service consequences that may entail the application of such a tool.
CVD is already a leading cause of death and disability in most developing countries except those in sub-Saharan Africa. Tobacco smoking, physical inactivity, unhealthy diet, and accompanying obesity are responsible for at least 75% of CVD, mainly through their effects on blood pressure, blood sugar, and blood lipids. These conventional cardiovascular risk factors are becoming more prevalent in all populations of the developing world. Strategies targeting the primary and secondary prevention of high-risk individuals are urgently required to contain the epidemic. Such strategies are necessary to exert an immediate measurable impact on the current cardiovascular morbidity and mortality rates. However, investment in population-based strategies, which have the potential to prevent the epidemic in the long-term, is essential and is affordable even to low income countries. Developing and implementing balanced public health policies that address the cardiovascular risk at individual and population-wide level are urgently required to curb the burgeoning cardiovascular epidemic in developing countries.
References
- Anderson KM, Odell PM, Wilson PWF, et al. Cardiovascular disease risk profiles. Am Heart J. 1990;121:293–8. doi: 10.1016/0002-8703(91)90861-b. [DOI] [PubMed] [Google Scholar]
- Brindle P, Emberson J, Lampe F, et al. Predictive accuracy of the Framingham coronary risk score in British men: prospective cohort study. BMJ. 2003;327:1267–70. doi: 10.1136/bmj.327.7426.1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy RM, Pyorala K, Fitzgerald AP, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24:987–1003. doi: 10.1016/s0195-668x(03)00114-3. [DOI] [PubMed] [Google Scholar]
- Ebrahim S, Montaner D, Lawlor DA. Clustering of risk factors and social class in childhood and adulthood in British women's heart and health study: cross sectional analysis. BMJ. 2004;10:861. doi: 10.1136/bmj.38034.702836.55. [Erratum: BMJ, 2004, 328:1104.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emberson JR, Whincup PH, Morris RW, et al. Extent of regression dilution for established and novel coronary risk factors: results from the British Regional Heart Study. Eur J Cardiovasc Prev Rehabil. 2004;11:125–34. doi: 10.1097/01.hjr.0000114967.39211.e5. [DOI] [PubMed] [Google Scholar]
- Magnus P, Beaglehole R. The real contribution of the major risk factors to the coronary epidemics: time to end the “only-50%” myth. Arch Intern Med. 2001;161:2657–60. doi: 10.1001/archinte.161.22.2657. [DOI] [PubMed] [Google Scholar]
- Mendis S. Challenges for the management of hypertension in low-resource settings. Ethn Dis. 2003;13(2 Suppl 2):S67–70. [PubMed] [Google Scholar]
- Mendis S, Abegunde D, Oladapo O, et al. Barriers to management of cardiovascular risk in a low-resource setting using hypertension as an entry point. J Hypertens. 2004;22:59–64. doi: 10.1097/00004872-200401000-00013. [DOI] [PubMed] [Google Scholar]
- [WHO] World Health Organization . World Health Report 2002: reducing risks, promoting healthy life. Geneva: WHO; 2002a. [DOI] [PubMed] [Google Scholar]
- [WHO] World Health Organization . Secondary prevention of noncommunicable diseases in low and middle-income countries through community-based and health service interventions. Geneva: WHO; 2002b. Report of Wellcome Trust meeting, August 2001. (WHO/EDM/2000.1) [Google Scholar]
- [WHO] World Health Organization . Reduction of cardiovascular burden through cost effective integrated management of comprehensive cardiovascular risk. Geneva: WHO; 2002c. [Google Scholar]
- [WHO] World Health Organization . CVD-risk management package for low- and medium-resource settings. Geneva: WHO; 2002d. [Google Scholar]
- [WHO] World Health Organization . The World Health Report 2003: shaping the future. Geneva: WHO; 2003a. [Google Scholar]
- [WHO] World Health Organization . Prevention of recurrent heart attacks and strokes in low and middle income populations. Evidence based recommendations for policy makers and health professionals. Geneva: WHO; 2003b. [Google Scholar]
- Yusuf S, Hawken S, Ounpuu S, et al. INTERHEART Study Investigators Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]


