Abstract
Measurement of blood pressure in the clinic may provide a false impression of blood pressure control. Ambulatory blood pressure monitoring (ABPM) allows the automatic recording of the circadian variation in blood pressure and evaluation of the efficacy of antihypertensive medication throughout the dosing interval. Ambulatory blood pressure provides more effective prediction of cardiovascular risk; blood pressure control at the time of heightened risk in the early morning after waking and before taking the next dose of medication is becoming important in order to improve long-term prognosis. To achieve blood pressure control in the early morning, a long-acting antihypertensive agent is essential. Telmisartan, an angiotensin II receptor blocker, as well as having a terminal elimination halflife of 24 h, has a large volume of distribution due to its high lipophilicity. The efficacy of telmisartan 80 mg monotherapy has been demonstrated using ABPM, with superior reduction in mean values for the last 6 h of the dosing interval compared with ramipril 10 mg and valsartan 80 mg. In addition, telmisartan 80 mg provides superior blood pressure control after a missed dose compared with valsartan 160 mg. When combined with hydrochlorothiazide (HCTZ) 12.5 mg, telmisartan 40 mg and 80 mg is more effective than losartan/HCTZ (50/12.5 mg) at the end of the dosing interval. Furthermore, greater reductions in last 6 h mean systolic blood pressure (SBP) and diastolic blood pressure (DBP) are achieved with telmisartan/HCTZ (80/12.5 mg) than with valsartan/HCTZ (160/12.5 mg) in obese patients with type 2 diabetes and hypertension. Recent data from a large group of patients show that telmisartan 80 mg controls the early morning blood pressure surge more effectively than ramipril 5–10 mg and, thus, may have a greater beneficial effect on long-term cardiovascular risk. This supposition is being tested in the ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial (ONTARGET) programme
Keywords: angiotensin II receptor blocker, antihypertensive, cardiovascular disease, hypertension, morning, telmisartan
Introduction
Hypertension, which affects one in four adults worldwide (Kearney et al 2004), is an important cause of cardiovascular morbidity and mortality, and antihypertensive treatment is a common therapeutic intervention. Clinical guidelines have recommended threshold levels for the implementation of antihypertensive therapy, typically based on blood pressure levels assessed by the physician in an office environment (Chobanian et al 2003; Guidelines Committee 2003; Whitworth 2003). Increasingly, however, it is being recognized that such ‘in-clinic’ measurements do not identify accurately variations in daily activity and their impact on blood pressure. Such measurements can, therefore, miss true hypertension. Exact prevalence of so-called ‘reversed white-coat hypertension’, ‘masked hypertension’, or ‘white-coat normotension’ is difficult to establish, but four studies found incidences of between 9% and 23% (Pickering et al 2002). Masked hypertension carries an increased cardiovascular risk compared with the prognosis in individuals with well-controlled home or ambulatory blood pressure (Clement et al 2003; Bobrie et al 2004; Ohkubo et al 2005; Pierdomenico et al 2005). In the elderly, the cardiovascular risk in those with masked hypertension was equal to that in those with sustained hypertension (Bjorklund et al 2003).
The problem of masked hypertension can be exacerbated in individuals receiving treatment for hypertension, because many antihypertensive drugs have an effect at trough that is substantially lower than their peak effect. Indeed, in the 1990s when most currently used antihypertensives were evaluated, the US Food and Drug Administration's criterion for an effective antihypertensive agent was one with a trough–peak ratio of no less than 50% (Meredith and Elliott 1994). A fair comparison among various antihypertensive agents cannot be established solely on the basis of trough–peak ratios (Lefebvre et al 2002). Since the medication is usually administered once daily and taken in the morning to encourage patient compliance, peak efficacy is likely to occur around the time of morning blood pressure measurement in the physician's office. By contrast, the trough effect may coincide with the early morning period towards the end of the dosing interval. Consequently, patients with treated hypertension often have relatively higher morning blood pressure compared with office blood pressure. An analysis of blood pressure control using ambulatory blood pressure monitoring (ABPM) found that, in 290 Spanish patients whose blood pressure was controlled according to clinic measurements, only 38% displayed control of morning blood pressure (Redon et al 2002).
In the evaluation of antihypertensive activity, ABPM is regarded as preferable because ambulatory values are more reproducible and established as more superior predictors of cardiovascular risk than clinic measurements (Parati and Lantelme 2002).
It has long been recognized that incidence of cardiovascular events vary at different times of the day and night; most strikingly, occurrences peak in the early morning soon after waking (Muller et al 1985; Marler et al 1989; Willich et al 1992; Elliott 1998). Analysis of data from 66 000 patients, for example, showed that myocardial infarction was increased by 40% between 6.00 am and midday (Cohen 1997). Hence, when prescribing an antihypertensive agent, it is important that a long-acting agent is given to ensure sustained control of blood pressure at the time of heightened risk. The importance of 24 h blood pressure control has been endorsed in the current European Society of Hypertension/European Society of Cardiology guidelines (Guidelines Committee 2003). The use of noninvasive ABPM allows blood pressure to be measured at regular pre-programmed intervals (usually every 15 or 20 minutes). Once the data are downloaded, circadian variations in systolic blood pressure (SBP) and diastolic blood pressure (DBP) can be analyzed and mean values for specific periods (eg, 24 h, morning, daytime, night-time, and last 6 h of the dosing interval) calculated.
Pharmacological properties of telmisartan
Angiotensin II receptor blockers (ARBs) are highly effective antihypertensive agents and are widely regarded as having tolerability profiles similar to that of placebo (Meredith 2005). Of the commercially available ARBs, telmisartan has the longest half-life of about 24 h (Burnier and Maillard 2001; Brunner 2002). This suggests that telmisartan should have a long duration of action, thus ensuring blood pressure control throughout the once-daily dosing interval. Another feature distinguishing telmisartan from other ARBs is its high lipophilicity (Wienen et al 2000). This enhances tissue penetration, intracellular absorption and bioavailability. The high lipophilicity is reflected in the high volume of distribution of approximately 500 L (Stangier et al 2000). The high lipophilicity of telmisartan, in comparison with losartan, may confer vascular protection as has been demonstrated in an animal model (Takai et al 2005). Another feature that distinguishes telmisartan from the ARBs candesartan cilexetil, losartan, and olmesartan is that it is not a prodrug; thus antihypertensive potency is related to the activity of the parent compound (Wienen et al 2000).
Efficacy of telmisartan in the early morning hours
Monotherapy
The efficacy of telmisartan monotherapy has been extensively studied using ABPM to establish whether the long half-life translates into effective blood pressure control at the end of the once-daily dosing interval. In addition to double-blind studies, prospective, randomized open-label, blinded-endpoint (PROBE) studies have been employed in the evaluation of the duration of action of telmisartan. Although in PROBE studies investigators are aware of the treatment given, the automated and objective measurement of blood pressure minimizes the potential for observer bias. Meta-analysis has revealed that double-blind and PROBE studies are statistically equivalent in terms of ruling out a difference of ≥3 mm Hg in SBP and ≥2 mm Hg in DBP (Smith et al 2003).
In a study comparing telmisartan 40–120 mg with the long-acting calcium channel blocker amlopidine 5–10 mg, both treatments produced comparable reductions in clinical blood pressure after 12 weeks in patients with mild-tomoderate hypertension (Lacourcière et al 1998). Clinic measurements revealed that both telmisartan and amlodipine reduced trough blood pressure, with no significant difference between the two treatments. ABPM also showed that both antihypertensive drugs reduced mean SBP and DBP at all time periods compared with corresponding baseline values. However, telmisartan brought about a significantly greater reduction (p<0.05) in mean DBP during the night-time and during the last 4 h of the dosing interval. There was also a trend towards greater reduction of mean SBP with telmisartan for these periods, although statistical significance was not reached.
Telmisartan 80 mg displayed superior reduction in last 6 h mean SBP and DBP compared with ramipril 10 mg after 14 weeks' treatment in the Prospective Randomized Investigation of the Safety and efficacy of Micardis versus ramipril using ABPM (PRISMA) (Lacourcière, Neutel, et al 2004; Lacouricière et al 2006; Williams et al 2006). The two PROBE studies were identical in design, one study being conducted in the US and Canada (Lacourcière, Neutel, et al 2004; Lacouricière et al 2006) and the other in Europe (Williams et al 2006). Ambulatory blood pressure was recorded in a total of 634 patients treated with telmisartan and 619 receiving ramipril. Mean reductions in last 6 h mean SBP/DBP for telmisartan 80 mg were 12.0/8.4 mm Hg as opposed to 7.9/5.4 mm Hg for ramipril 10 mg (p<0.0001 for both SBP and DBP) (Williams et al 2005).
Compared with losartan 50 mg, telmisartan 40 mg or 80 mg demonstrated superior control of both SBP and DBP during the last 6 h of the dosing interval (Mallion et al 1999). The reductions in last 6 h mean SBP/DBP after 6 weeks' treatment with losartan were 6.0/3.7 mm Hg for losartan, whereas telmisartan 40 mg brought about reductions of 10.7/6.8 mm Hg (p<0.05 for both SBP and DBP) and reductions after telmisartan 80 mg treatment were 12.2/7.1 mm Hg (p<0.05 for both SBP and DBP). A distinction between the duration of action of telmisartan 10–40 mg and losartan 25–100 mg was also noted in a Japanese study using home blood pressure measurements performed soon after the patients got up in the morning. The home morning DBP was significantly lower in telmisartan-treated patients (Nishimura et al 2005).
Another PROBE study comparing telmisartan 80 mg with valsartan 80 mg after treatment for 8 weeks detected a significantly greater reduction in the last 6 h mean DBP in telmisartan-treated patients (7.5 mm Hg vs 5.2 mm Hg) (Littlejohn et al 2000). The dose of valsartan used was that recommended at the time. Subsequently, it was reported that the antihypertensive efficacy of valsartan was enhanced if the dose was increased to 160 mg (Verdecchia and Angeli 2004). This doubling of the dose did not, however, compromise the placebo-like tolerability profile. More recently, two identically designed multinational, randomized, double-blind, forced-titration studies compared telmisartan 40–80 mg with valsartan 80–160 mg (Lacourcière, Krzesinski, et al 2004). After 4 weeks of highdose treatment, patients received either 1 day's double-blind active therapy or placebo (ie, a missed dose). Following a further 2 weeks' active treatment, a cross-over was performed, such that patients who had previously received 1 day's placebo received active therapy and vice versa. Pooled data from 877 patients evaluated in the two studies demonstrated that, after active therapy, the last 6 h mean DBP was reduced by 7.6 mm Hg with telmisartan compared with 5.8 mm Hg with valsartan (p=0.0044). Telmisartan also proved superior to valsartan in reducing the last 6 h mean SBP (adjusted mean reduction, 11.1 mm Hg vs 9.1 mm Hg, respectively; p=0.0066). After a missed dose, the 24 h mean DBP was reduced by 7.2 mm Hg with telmisartan compared with 5.5 mm Hg with valsartan (p=0.0004). The reduction in 24 h mean SBP after a missed dose was 10.7 mm Hg with telmisartan and 8.7 mm Hg with valsartan (p=0.0024). It was also observed in one of the two studies that there was a notable trend for greater blood pressure reduction in the telmisartan group compared with the valsartan group in latter part of the dosing interval on the day on which a dose was missed (White et al 2004). These data indicate that the longer half-life of telmisartan (Stangier et al 2000) compared with valsartan (Markham and Goa 1997) confers more sustained blood control, especially at the end of the dosing period, and preserves efficacy in poorly compliant patients in the event of a missed dose.
To address the criticism that clinical trials in hypertension may not provide a fair assessment of the effectiveness of antihypertensive drugs in clinical practice, an ABPM study was performed in the community (White et al 2005). The Micardis® Community Ambulatory Monitoring Trial (MICCAT 2) evaluated telmisartan either alone or in combination with low-dose hydrochlorothiazide (HCTZ) 12.5 mg in hypertensive patients who were untreated or currently receiving antihypertensive medication. Telmisartan-based treatment produced highly significant reductions in the daytime and night-time mean blood pressures. During the first 4 h after waking, telmisartan reduced SBP/DBP by a mean of 11.5/7.0 mm Hg (p<0.0001 for both). In the long term, a 10 mm Hg lowering of SBP or a 5 mm Hg lowering of DBP would be associated with an approximately 40% lower risk of death from stroke and about a 30% lower risk of death from ischemic heart disease and other vascular causes (Lewington et al 2002).
In combination with HCTZ
In many patients, more than one antihypertensive drug may be required to achieve effective blood pressure control. By combining two different classes of antihypertensives, it may be possible to provide complementary, additive, or synergistic antihypertensive effects because of the drugs' different mechanisms of action. The use of low doses of two drugs may provide superior reduction of blood pressure to higher doses of one drug and may enhance tolerability, leading to improve compliance (Weir 1998). ARBs, by targeting the renin–angiotensin system (RAS), modulate the vasopressor activity of angiotensin II. In contrast, thiazide diuretics reduce blood pressure mainly because of their natriuretic mode of action (Motwani 2002). However, to compensate for sodium depletion, the RAS is stimulated by thiazide diuretics. Using an ARB offsets this stimulation and, hence, further reduces blood pressure. In addition, diuretic-induced potassium loss is redressed by co-administering an ARB because of the attenuation of angiotensin II-mediated aldosterone release. Clinical trials have shown that the tolerability of ARB monotherapy is maintained when the drug is combined with low-dose HCTZ (Meredith 2005).
Two PROBE studies have evaluated the efficacy of two fixed-dose telmisartan/HCTZ combinations (40/12.5 mg and 80/12.5 mg) versus a fixed-dose combination of losartan/HCTZ (50/12.5 mg) (Lacourcière et al 2003; Neutel et al 2005). In the study by Lacourcière et al (2003), after treatment for 6 weeks, losartan/HCTZ reduced last 6 h mean SBP/DBP by 15.0/9.7 mm Hg. The lower-dose telmisartan/HCTZ combination reduced last 6 h mean SBP/DBP by a further 2.5/1.8 mmHg (p<0.05 for both). For the higher-dose telmisartan/HCTZ combination, there was an additional reduction in last 6h mean SBP/DBP of 3.4/2.5 mm Hg (p<0.01 for both) compared with the losartan/HCTZ combination. In the second study, also involving 6 weeks' active treatment, both telmisartan/HCTZ fixed-dose combinations produced significantly greater reductions in the last 6 h mean DBP than losartan/HCTZ (50/12.5 mg). The adjusted mean difference from the losartan combination in favour of telmisartan/HCTZ 40/12.5 mg was −2.0 mm Hg (p=0.0031) (Neutel et al 2005). Telmisartan/HCTZ 80/12.5 mg also brought about significantly greater reductions in the last 6 h mean DBP compared with the losartan/HCTZ combination (adjusted mean difference −2.8 mm Hg; p=0.0003), In the case of last 6 h mean SBP, the adjusted mean differences compared with losartan/HCTZ were −2.6 mm Hg (p=0.0048) in favour of the lower-dose telmisartan/HCTZ combination and −3.5 mm Hg (p=0.0018) in favour of telmisartan/HCTZ 80/12.5 mg.
Achieving blood pressure control is important in patients with metabolic syndrome because of the heightened risk of target-organ damage (ADA 2002), leading to cardiovascular and renal disease (Cuspidi et al 2004). Being overweight is linked to hypertension (Heyden and Schneider 1990), and it has been shown that RAS activity is heightened in adipose tissue (Heyden and Schneider 1990; Rahmouni et al 2005). In the Study of Micardis in Obese/Overweight Type 2 diabetics with Hypertension (SMOOTH), patients received telmisartan 80 mg or valsartan 160 mg monotherapy for 4 weeks (Sharma et al 2005). Thereafter, HCTZ 12.5 mg was also given in addition to all patients for 6 weeks. The last 6 h mean SBP/DBP were reduced in the telmisartan/HCTZ group by 18.4/9.7 mm Hg and by 14.5/7.7 mm Hg in valsartan/HCTZ-treated patients. This represented a significant adjusted mean difference of −3.9 mm Hg (p<0.0001) for SBP and −2.0 mm Hg (p=0.0007) for DBP in favor of telmisartan/HCTZ.
In the elderly, systolic hypertension, in the absence of significant diastolic hypertension, is highly prevalent and is associated with an increased risk of cardiovascular death (Basile 2002). It has also been found that a high morning SBP surge in the elderly is significantly associated with the risk of silent cerebral infarct and stroke (Kario et al 2003). A force-titration PROBE study was performed in 638 elderly patients with systolic hypertension to compare telmisartan/HCTZ 80/12.5 mg with amlodipine/HCTZ 10/12.5 mg (Neldam et al 2005). The reduction from baseline in adjusted last 6 h mean SBP was 18.8 mm Hg for telmisartan/HCTZ and 17.7 mm Hg for amlodipine/HCTZ. The difference in favour of telmisartan/HCTZ of −1.1 mm Hg, confirms that telmisartan/HCTZ was at least as effective as amlodipine/HCTZ. The study also demonstrated that telmisartan/HCTZ produced a significantly greater reduction in 24 h mean (p=0.0010), daytime (p=0.0002) and morning SBP (p=0.0105) compared with amlodipine/HCTZ. In this study, the incidence of drug-related adverse events distinguished telmisartan-based therapy from that based on amlodipine: 8.0% in the telmisartan group but 33.4% amlodipine experienced one or more adverse events (p<0.0001). This was largely attributable to peripheral oedema, which was reported in 1.2% of telmisartan-group patients, but in 24.3% (p<0.0001) of amlodipine-group patients
Early morning blood pressure surge
In general, hypertensive and normotensive individuals exhibit a similar circadian variation in blood pressure, levels being highest during the daytime and lowest in the middle of the night (Staessen et al 1997). On awakening, the blood pressure surges, but the extent of this surge can vary in different individuals with some displaying morning hypertension (Gosse et al 2004). In other subjects, blood pressure is elevated at night and hypertension persists in the morning. A direct correlation exists between SBP on arising and left ventricular mass (Gosse et al 1997), and the SBP on arising has been shown to be significantly higher in the subjects who have cardiovascular complications (Gosse et al 2001, 2004). Multivariate analysis found that the association between early morning blood pressure and cardiovascular risk was independent of age and 24 h blood pressure. A relationship has also been demonstrated between a high early morning blood pressure surge and microalbuminuria (Polonia et al 2005).
In addition, a study conducted in elderly Japanese subjects showed that the incidence of silent and overt cerebrovascular lesions was highest in those with the greatest morning blood pressure surge (Kario et al 2003). In that study, an early morning blood pressure surge of ≥55 mm Hg was associated with a 2.5-fold increase in overt stroke and silent cerebral infarction. A recent meta-analysis has shown that, in clinical trials in hypertensive or high-risk patients, gradients in SBP accounted for most differences in outcome (Staessen et al 2005).
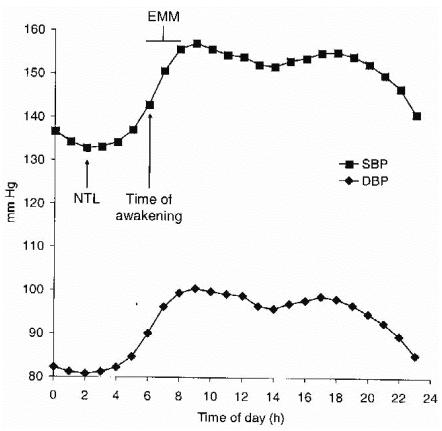
The PRISMA studies were novel in the fact that the time of waking was recorded for each patient (Lacourcière, Neutel, et al 2004; Lacouricière et al 2006; Williams et al 2006). The early morning blood pressure surge was determined as the difference between night-time low (mean of all measurements within a ±30-minute interval around the minimum blood pressure during sleeping) and early morning mean (mean during the 2 h after wakening) (Figure 1) (Eguchi et al 2003). Telmisartan 80 mg proved significantly superior to ramipril 10 mg in the reducing nighttime low and early morning mean SBP and DBP (p<0.0001 for all) compared with baseline values (Gosse et al 2005). Telmisartan reduced the overall mean systolic surge by 1.5 mm Hg, whereas ramipril caused an increase of 0.3 mm Hg (p=0.0049). The magnitude of surge reduction was greatest in the quartile with highest baseline early morning SBP surge: telmisartan −12.7 mm Hg, ramipril −7.8 mm Hg (p=0.0004). Telmisartan also reduced the surge compared with ramipril in dippers, but there were no differences between the two groups in non-dippers.
Figure 1.
Circadian pattern of blood pressure showing night-time low (NTL), time of waking, and early morning mean (EMM) for systolic blood pressure (SBP) and diastolic blood pressure (DBP).
Further evidence of telmisartan controlling the early morning blood pressure surge comes from the MICCAT 2 study (White et al 2005). Among the 1628 patients enrolled, 95 had a SBP surge of >30 mm Hg after waking. In these patients, the 4 h post-waking mean SBP/DBP fell by an average of 15.0/8.5 mm Hg with telmisartan monotherapy and by 19.4/11.6 mm Hg with combination therapy.
Conclusions
Elevated blood pressure in the early morning is associated with increased cardiovascular risk. It is crucial that antihypertensive medication controls blood pressure to minimize this risk at this time. Unfortunately some antihypertensives given once daily in the morning may not fulfil this requirement and may place the patient at increased risk. The ARB with the longest half-life is telmisartan. Its potential to reduce blood pressure in the risky early morning hours has been demonstrated in numerous clinical studies using ABPM. Also, of particular importance is the fact that telmisartan has been shown to reduce the early morning blood pressure surge.
The cardiovascular relevance of these observations is being tested in the ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial (ONTARGET) programme (Teo et al 2004). Currently, there is uncertainty about the role of ARBs when used alone or in combination with an ACE inhibitor in high-risk populations with controlled hypertension. The primary objectives of ONTARGET are to determine if the combination of the ARB telmisartan and the ACE inhibitor ramipril is more effective than ramipril alone, and if telmisartan is at least as effective as ramipril. The sister study is Telmisartan Randomized AssessmeNt Study in aCE iNtolerant subjects with cardiovascular Disease (TRANSCEND), which has been designed to establish whether or not telmisartan is superior to placebo in patients who are intolerant of ACE inhibitors. The primary outcome for both trials is the composite of cardiovascular death, myocardial infarction, stroke, or hospitalization for heart failure.
References
- [ADA] American Diabetes Association. Treatment of hypertension in adults with diabetes. Diabet Care. 2002;25:199–201. doi: 10.2337/diacare.25.1.199. [DOI] [PubMed] [Google Scholar]
- Basile J. Hypertension in the elderly: a review of the importance of systolic blood pressure elevation. J Clin Hypertens. 2002;4:108–12. doi: 10.1111/j.1524-6175.2001.00903.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjorklund K, Lind L, Zethelius B, et al. Isolated ambulatory hypertension predicts cardiovascular morbidity in elderly men. Circulation. 2003;107:1297–302. doi: 10.1161/01.cir.0000054622.45012.12. [DOI] [PubMed] [Google Scholar]
- Bobrie G, Chatellier G, Genes N, et al. Cardiovascular prognosis of “masked hypertension” detected by blood pressure self-measurement in elderly treated hypertensive patients. JAMA. 2004;291:1342–9. doi: 10.1001/jama.291.11.1342. [DOI] [PubMed] [Google Scholar]
- Brunner HR. The new oral angiotensin II antagonist olmesartan medoxomil: a concise overview. J Hum Hypertens. 2002;16(Suppl 2):S13–16. doi: 10.1038/sj.jhh.1001391. [DOI] [PubMed] [Google Scholar]
- Burnier M, Maillard M. The comparative pharmacology of angiotensin II receptor antagonists. Blood Press. 2001;10(Suppl 1):6–11. [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- Clement DL, De Buyzere ML, De Bacquer DA, et al. Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med. 2003;348:2407–15. doi: 10.1056/NEJMoa022273. [DOI] [PubMed] [Google Scholar]
- Cohen MC. Meta-analysis of the morning excess of acute myocardial infarction and sudden cardiac death. Am J Cardiol. 1997;79:1512–16. doi: 10.1016/s0002-9149(97)00181-1. [DOI] [PubMed] [Google Scholar]
- Cuspidi C, Meani S, Fusi V, et al. Metabolic syndrome and target organ damage in untreated essential hypertensives. J Hypertens. 2004;22:1991–8. doi: 10.1097/00004872-200410000-00023. [DOI] [PubMed] [Google Scholar]
- Eguchi K, Kario K, Shimada K. Comparison of candesartan with lisinopril on ambulatory blood pressure and morning surge in patients with systemic hypertension. Am J Cardiol. 2003;92:621–4. doi: 10.1016/s0002-9149(03)00739-2. [DOI] [PubMed] [Google Scholar]
- Elliott WJ. Circadian variation in the timing of stroke onset: a meta-analysis. Stroke. 1998;29:992–6. doi: 10.1161/01.str.29.5.992. [DOI] [PubMed] [Google Scholar]
- Gosse P, Ansoborlo P, Lemetayer P, et al. Left ventricular mass is better correlated with arising blood pressure than with office or occasional blood pressure. Am J Hypertens. 1997;10:505–10. doi: 10.1016/s0895-7061(96)00048-9. [DOI] [PubMed] [Google Scholar]
- Gosse P, Cipriano C, Bemurat L, et al. Prognostic significance of blood pressure measured on rising. J Hum Hypertens. 2001;15:413–17. doi: 10.1038/sj.jhh.1001187. [DOI] [PubMed] [Google Scholar]
- Gosse P, Lasserre R, Minifie C, et al. Blood pressure surge on rising. J Hypertens. 2004;22:1113–18. doi: 10.1097/00004872-200406000-00011. [DOI] [PubMed] [Google Scholar]
- Gosse P, Neutel JM, Schumacher H, et al. Reduction of early morning blood pressure surge with telmisartan compared with ramipril in mild-to-moderate hypertensive patients. J Hypertens. 2005;23(Suppl 2):S375–6. [Google Scholar]
- Guidelines Committee. European Society of Hypertension – European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003;21:1011–53. doi: 10.1097/00004872-200306000-00001. [DOI] [PubMed] [Google Scholar]
- Heyden S, Schneider KA. Obesity and hypertension: epidemiological aspects of the relationship. J Hum Hypertens. 1990;4:431–5. [PubMed] [Google Scholar]
- Kario K, Pickering TG, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107:1401–6. doi: 10.1161/01.cir.0000056521.67546.aa. [DOI] [PubMed] [Google Scholar]
- Kearney PM, Whelton M, Reynolds K, et al. Worldwide prevalence of hypertension: a systematic review. J Hypertens. 2004;22:11–19. doi: 10.1097/00004872-200401000-00003. [DOI] [PubMed] [Google Scholar]
- Lacourcière Y, Gil-Extremera B, Mueller O, et al. Efficacy and tolerability of fixed-dose combinations of telmisartan plus HCTZ compared with losartan plus HCTZ in patients with essential hypertension. Int J Clin Pract. 2003;57:273–9. [PubMed] [Google Scholar]
- Lacourcière Y, Krzesinski JM, White WB, et al. Sustained antihypertensive activity of telmisartan compared with valsartan. Blood Press Monit. 2004a;9:203–10. doi: 10.1097/00126097-200408000-00005. [DOI] [PubMed] [Google Scholar]
- Lacourcière Y, Lenis J, Orchard R, et al. A comparison of the efficacy and duration of action of the angiotensin II receptor blocker telmisartan to amlodipine. Blood Press Monit. 1998;3:295–302. [PubMed] [Google Scholar]
- Lacourcière Y, Neutel J, Koval SE, et al. A prospective, randomized investigation of the safety and efficacy of telmisartan vs ramipril in mild-to-moderate hypertensives using ambulatory blood pressure monitoring. Hypertension. 2004b;44:576. [Google Scholar]
- Lacourcière Y, Neutel J, Davidai G, et al. A multicenter, 14-week study of telmisartan and ramipril in patients with mild-to-moderate hypertension using ambulatory blood pressure monitoring. Am J Hypertens. 2006;19:104–12. doi: 10.1016/j.amjhyper.2005.10.001. [DOI] [PubMed] [Google Scholar]
- Lefebvre J, Poirier L, Lacourcière Y. Methodology to determine duration of action for antihypertensive drugs. Ann Pharmacother. 2002;36:874–81. doi: 10.1345/aph.10367. [DOI] [PubMed] [Google Scholar]
- Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- Littlejohn T, Mroczek W, Marbury T, et al. A prospective, randomized, open-label trial comparing telmisartan 80 mg and valsartan 80 mg in patients with mild-to-moderate hypertension using ambulatory blood pressure monitoring. Can J Cardiol. 2000;16:1123–32. [PubMed] [Google Scholar]
- Mallion JM, Siché JP, Lacourcière Y, et al. ABPM comparison of the antihypertensive profiles of the selective angiotensin II receptor antagonists telmisartan and losartan in patients with mild-to-moderate hypertension. J Hum Hypertens. 1999;13:657–64. doi: 10.1038/sj.jhh.1000925. [DOI] [PubMed] [Google Scholar]
- Markham A, Goa KL. Valsartan. A review of its pharmacology and therapeutic use in essential hypertension. Drugs. 1997;54:299–311. doi: 10.2165/00003495-199754020-00009. [DOI] [PubMed] [Google Scholar]
- Marler JR, Price TR, Clark GL, et al. Morning increase in onset of ischemic stroke. Stroke. 1989;20:473–6. doi: 10.1161/01.str.20.4.473. [DOI] [PubMed] [Google Scholar]
- Meredith PA. Angiotensin II receptor antagonists alone and combined with hydrochlorothiazide: potential benefits beyond the antihypertensive effect. Am J Cardiovasc Drugs. 2005;5:171–83. doi: 10.2165/00129784-200505030-00004. [DOI] [PubMed] [Google Scholar]
- Meredith PA, Elliott HL. FDA guidelines on trough: peak ratios in the evaluation of antihypertensive agents. United States Food and Drug Administration. J Cardiovasc Pharmacol. 1994;23(Suppl 5):S26–30. [PubMed] [Google Scholar]
- Motwani JG. Combining renin-angiotensin-aldosterone system blockade with diuretic therapy for treatment of hypertension. J Renin Angiotensin Aldosterone Syst. 2002;3:72–8. doi: 10.3317/jraas.2002.021. [DOI] [PubMed] [Google Scholar]
- Muller JE, Stone PH, Turi ZG, et al. Circadian variation in the frequency of onset of acute myocardial infarction. N Engl J Med. 1985;313:1315–22. doi: 10.1056/NEJM198511213132103. [DOI] [PubMed] [Google Scholar]
- Neldam S, for the ATHOS Group Telmisartan + hydrochlorothiazide versus amlodipine + hydrochlorothiazide in older patients with predominantly systolic hypertension. J Hypertens. 2005;23(Suppl 2):S116. [Google Scholar]
- Neutel JM, Littlejohn TW, Chrysant SGSA, et al. Telmisartan/hydrochlorothiazide in comparison with losartan/hydrochlorothiazide in managing patients with mild-to-moderate hypertension. Hypertens Res. 2005;28:555–63. doi: 10.1291/hypres.28.555. [DOI] [PubMed] [Google Scholar]
- Nishimura T, Hashimoto J, Ohkubo T, et al. Efficacy and duration of action of the four selective angiotensin II subtype 1 receptor blockers, losartan, candesartan, valsartan and telmisartan, in patients with essential hypertension determined by home blood pressure measurements. Clin Exp Hypertens. 2005;27:477–89. doi: 10.1081/CEH-200067668. [DOI] [PubMed] [Google Scholar]
- Ohkubo T, Kikuya M, Metoki H, et al. Prognosis of “masked” hypertension and “white-coat” hypertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J Am Coll Cardiol. 2005;46:508–15. doi: 10.1016/j.jacc.2005.03.070. [DOI] [PubMed] [Google Scholar]
- Parati G, Lantelme P. Blood pressure. J Hypertens. 2002;20:1725–9. doi: 10.1097/00004872-200209000-00014. [DOI] [PubMed] [Google Scholar]
- Pickering TG, Davidson K, Gerin W, et al. Masked hypertension. Hypertension. 2002;40:795–6. doi: 10.1161/01.hyp.0000038733.08436.98. [DOI] [PubMed] [Google Scholar]
- Pierdomenico SD, Lapenna D, Bucci A, et al. Cardiovascular outcome in treated hypertensive patients with responder, masked, false resistant, and true resistant hypertension. Am J Hypertens. 2005;18:1422–8. doi: 10.1016/j.amjhyper.2005.05.014. [DOI] [PubMed] [Google Scholar]
- Polonia J, Amado P, Barbosa L, et al. Morning rise, morning surge and daytime variability of blood pressure and cardiovascular target organ damage. A cross-sectional study in 743 subjects. Rev Port Cardiol. 2005;24:65–78. [PubMed] [Google Scholar]
- Rahmouni K, Correia ML, Haynes WG, et al. Obesity-associated hypertension: new insights into mechanisms. Hypertension. 2005;45:9–14. doi: 10.1161/01.HYP.0000151325.83008.b4. [DOI] [PubMed] [Google Scholar]
- Redon J, Rocha-Cusachs A, Mora-Macia J. Uncontrolled early morning blood pressure in medicated patients: the ACAMPA study. Blood Press Monit. 2002;7:111–16. doi: 10.1097/00126097-200204000-00004. [DOI] [PubMed] [Google Scholar]
- Sharma AM, Davidson JA, Gavin JR, III, et al. Comparison of the antihypertensive efficacy of telmisartan/hydrochlorothiazide vs valsartan/hydrochlorothiazide in high-risk overweight/obese patients with hypertension and type 2 diabetes [abstract, poster]. European Council for Cardiovascular Research Presented at the 10th Annual Meeting of the European Council for Cardiovascular Research (ECCR); 14–16 October 2005; Nice, France. 2005. [Google Scholar]
- Smith DH, Neutel JM, Lacourcière Y, et al. Prospective, randomized, open-label, blinded-endpoint (PROBE) designed trials yield the same results as double-blind, placebo-controlled trials with respect to ABPM measurements. J Hypertens. 2003;21:1291–8. doi: 10.1097/00004872-200307000-00016. [DOI] [PubMed] [Google Scholar]
- Staessen JA, Bieniaszewski L, O'Brien E, et al. Nocturnal blood pressure fall on ambulatory monitoring in a large international database. Hypertension. 1997;29:30–9. doi: 10.1161/01.hyp.29.1.30. [DOI] [PubMed] [Google Scholar]
- Staessen JA, Li Y, Thijs L, et al. Blood pressure reduction and cardiovascular prevention: an update including the 2003–2004 secondary prevention trials. Hypertens Res. 2005;28:385–407. doi: 10.1291/hypres.28.385. [DOI] [PubMed] [Google Scholar]
- Stangier J, Su C-APF, Roth W. Pharmacokinetics of orally and intravenously administered telmisartan in healthy young and elderly volunteers and in hypertensive patients. J Int Med Res. 2000;28:149–67. doi: 10.1177/147323000002800401. [DOI] [PubMed] [Google Scholar]
- Takai S, Kirimura K, Jin D, et al. Significance of angiotensin II receptor blocker lipophilicities and their protective effect against vascular remodeling. Hypertens Res. 2005;28:593–600. doi: 10.1291/hypres.28.593. [DOI] [PubMed] [Google Scholar]
- Teo K, Yusuf S, Anderson C, et al. Rationale, design, and baseline characteristics of 2 large, simple, randomized trials evaluating telmisartan, ramipril, and their combination in high-risk patients: the Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial/Telmisartan Randomized Assessment Study in ACE Intolerant Subjects with Cardiovascular Disease. (ONTARGET/TRANSCEND) trials. Am Heart J. 2004;148:52–61. doi: 10.1016/j.ahj.2004.03.020. [DOI] [PubMed] [Google Scholar]
- Verdecchia P, Angeli F. Assessment of the optimal daily dose of valsartan in patients with hypertension, heart failure, or both. Clin Ther. 2004;26:460–72. doi: 10.1016/s0149-2918(04)90049-5. [DOI] [PubMed] [Google Scholar]
- Weir MR. The rationale for combination versus single-entity therapy in hypertension. Am J Hypertens. 1998;11(Suppl 10):163S–9S. doi: 10.1016/s0895-7061(98)00189-7. [DOI] [PubMed] [Google Scholar]
- White WB, Lacourcière Y, Davidai G. Effects of the angiotensin II receptor blockers telmisartan versus valsartan on the circadian variation of blood pressure: impact on the early morning period. Am J Hypertens. 2004;17:347–53. doi: 10.1016/j.amjhyper.2004.02.016. [DOI] [PubMed] [Google Scholar]
- White WB, Weber MA, Davidai G, et al. Ambulatory blood pressure monitoring in the primary care setting: assessment of therapy on the circadian variation of blood pressure from the MICCAT-2 Trial. Blood Press Monit. 2005;10:157–63. doi: 10.1097/00126097-200506000-00008. [DOI] [PubMed] [Google Scholar]
- Whitworth JA. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;21:1983–92. doi: 10.1097/00004872-200311000-00002. [DOI] [PubMed] [Google Scholar]
- Wienen W, Entzeroth M, van Meel JCA, et al. A review on telmisartan: a novel, long-acting angiotensin II-receptor antagonist. Cardiovasc Drug Rev. 2000;18:127–56. [Google Scholar]
- Williams B, Gosse P, Lowe L, et al. The prospective, randomized investigation of the safety and efficacy of telmisartan versus ramipril using ambulatory blood pressure monitoring (PRISMA I) J Hypertens. 2006;24:193–200. doi: 10.1097/01.hjh.0000194364.11516.ab. [DOI] [PubMed] [Google Scholar]
- Williams B, Lacourcière Y, Schumacher H, et al. Telmisartan versus ramipril in 24-h ambulatory blood pressure: a pooled analysis of 2 prospective, randomized trials in mild-to-moderate hypertensive patients [abstract] J Hypertens. 2005;23(Suppl 2):S381, P3.372. [Google Scholar]
- Willich SN, Goldberg RJ, Maclure M, et al. Increased onset of sudden cardiac death in the first three hours after awakening. Am J Cardiol. 1992;70:65–8. doi: 10.1016/0002-9149(92)91391-g. [DOI] [PubMed] [Google Scholar]