Abstract
Cognitive–behavioral therapy (CBT) and pharmacotherapy are similarly effective for treating panic disorder with mild or no agoraphobia, but little is known about the mechanism through which these treatments work. The present study examined some of the criteria for cognitive mediation of treatment change in CBT alone, imipramine alone, CBT plus imipramine, and CBT plus placebo. Ninety-one individuals who received 1 of these interventions were assessed before and after acute treatment, and after a 6-month maintenance period. Multilevel moderated mediation analyses provided preliminary support for the notion that changes in panic-related cognitions mediate changes in panic severity only in treatments that include CBT.
Keywords: mediation, cognitive–behavioral therapy, pharmacotherapy, imipramine, panic disorder
Cognitive–behavioral therapy (CBT) for panic disorder has been found to be effective in a number of well-controlled clinical studies (e.g., Mitte, 2005). These treatment protocols are based on the same basic rationale and assume that extinction to internal and external anxiogenic cues and reduction of catastrophic cognitions are responsible for short-term and long-term changes in panic symptomatology.
One of the largest randomized controlled trials comparing CBT and pharmacotherapy was conducted by Barlow, Gorman, Shear, and Woods (2000). One of the primary measures used was the Panic Disorder Severity Scale (PDSS; Shear et al., 1997). The results of this study showed that imipramine and CBT were significantly more effective than placebo (as assessed by the PDSS) after the acute treatment phase and also after the 6-month maintenance phase. The efficacy of CBT was comparable to that of imipramine on nearly all measures during treatment, and it showed better maintenance of gains after treatment discontinuation.
Despite the demonstrated efficacy of these interventions, little is known about the mechanism of treatment change. The CBT model predicts that changes in panic-related cognitions mediate treatment changes in panic symptomatology and that greater changes in cognitions occur during the course of CBT than during other interventions, such as pharmacotherapy (e.g., Barlow, 2002; Clark, 1986). Therefore, the CBT model implies a moderated mediational relationship between panic-related cognitions and panic symptomatology in which the strength of cognitive mediation is greater during CBT than during pharmacotherapy. The empirical literature, so far, provides very little empirical support for these crucial assumptions.
Factor analytic studies point to the existence of three main categories of anxiogenic panic-related cognitions (e.g., Chambless, Caputo, Bright, & Gallagher, 1984; Telch, Brouillard, Telch, Agras, & Taylor, 1989). These categories comprise thoughts related to physical catastrophes (such as heart attack), thoughts related to mental catastrophes (such as going crazy), and thoughts related to social catastrophes (such as making a fool of oneself). More recently, Hicks and colleagues (2005) examined cognitions as predictors of treatment outcome and reported that fears of social catastrophes before and following treatment with CBT or pharmacotherapy predict poor outcome. This study, which was based on the same data set as reported here, suggests that prior catastrophic cognitions predict treatment outcome. Another important question, which speaks directly to the validity of the cognitive model of treatment change, is whether changes in cognitions mediate CBT and whether these changes are modality specific (for a comprehensive discussion of the distinction between mediation and moderation, see Baron & Kenny, 1986).
The purpose of the present study was to explore the mechanism of treatment change in CBT as compared with pharmacological treatment and combined treatment of panic disorder. We hypothesized that changes in cognitions mediate changes in panic severity during treatments that included CBT (CBT only, CBT plus imipramine, and CBT plus placebo) but not in treatments that include only pharmacotherapy (imipramine only).
Method
Study Design
The data set of the present analyses was part of the Multicenter Comparative Treatment Study of Panic Disorder (MCCTSPD). The main results and methods were reported elsewhere (Barlow et al., 2000). In the present study, we examined all available data from this trial to study cognitive mediation of treatment change. Specifically, we examined 91 individuals who were part of the following treatment conditions: (a) CBT alone (n = 24), (b) up to 300 mg/day of imipramine alone (IMI; n = 18), (c) the combination of CBT plus imipramine (CBT + IMI; n = 27), and (d) the combination of CBT plus a pill placebo (CBT + PLA; n = 22).1
Participants
All participants with available data (including nonresponders) were included in the analysis. Responder status was defined by a rating of “much improved” or “very much improved” on the Clinical Global Impression Scale (Guy, 1976) at posttreatment (80 out of 91 individuals). The four treatment groups did not differ in the responder rates (CBT: 21 out of 24; IMI: 15 out of 18; CBT + IMI: 23 out of 27; CBT + PLA: 21 out of 22), χ2(3) = 1.73, p > .6. The sample in the present study consisted of 36 men and 55 women. Eight-three of these participants were White, 3 were African American, 2 were Hispanic, and 3 identified themselves as “other.” On average, participants were 37.56 years old (range = 19 − 65, SD = 10.54). The four treatment groups did not differ on any of the demographic variables.
Treatments
CBT
The CBT protocol used in this study was based on the panic control treatment manual (Barlow & Craske, 2000). Similar to other CBT protocols, a number of treatment components, including cognitive restructuring, psychoeducation, relaxation, controlled breathing procedures, and exposure techniques, were included in this approach (Barlow & Craske, 2000). Protocol adherence and therapist competence measures of this intervention were reported elsewhere (Barlow et al., 2000). Treatment consisted of 11 sessions over the course of 12 weeks. Each CBT session lasted approximately 50 min.
Pharmacotherapy
The pharmacotherapy protocol consisted of administering imipramine in a double-blind, flexible-dose design according to a manual developed specifically for the MCCTSPD. The initial dose of imipramine was 10 mg/day. The dosage was then increased every other day by 10 mg until a dose of 50 mg/day was reached and increased more rapidly afterward, with the goal of reaching 100 mg/day by the end of Week 3 and 200 mg/day by Week 5. This goal was pursued even if the patient became symptom free earlier, unless adverse effects became intolerable. If the patient was not symptom free at 200 mg/day, the dosage could be increased up to 300 mg/day by Week 5. The number and spacing of pharmacotherapy sessions were identical to those of the CBT sessions. Each drug treatment session lasted approximately 30 min. In the combined condition, patients met first with the pharmacotherapist and then with the CBT therapist.
Assessments
Thoughts Rating Form (TRF)
The TRF is a self-report questionnaire that measures the degree of catastrophic cognitions associated with panic attacks. The instrument was specifically developed for use in the MCCTSPD. Participants were asked to rate how much they believed a number of common cognitions about physical, social, and mental events. Each of these beliefs was rated on a scale ranging from 0 (not at all) to 8 (extremely). Hicks and colleagues (2005) identified three factors that were labeled physical catastrophes cognitions (TRF–P), mental catastrophes cognitions (TRF–M), and social catastrophes cognitions (TRF–S). Internal consistencies and test–retest reliabilities were acceptable for all three factors (see Hicks et al., 2005). This instrument was administered at pretest, at posttest, and after the 6-month maintenance phase.
PDSS
The PDSS (Shear et al., 1997) is a seven-item clinician-rated scale to measure the severity of panic disorder. It was the primary continuous outcome measure in the MCCTSPD. The PDSS shows excellent psychometric characteristics (Shear et al., 1997). It was administered at pretest, posttest, and the 6-month follow-up assessment.
Mediation Test
The data were analyzed using a multilevel model (Raudenbush, Bryk, Cheong, & Congdon, 2004) in which the three measurement time points (pretest, posttest, and follow-up) were nested within individuals (e.g., Kenny, Korchmaros, & Bolger, 2003; Smits, Rosenfield, McDonald, & Telch, 2006). Specifically, we examined the effect of time (pretest, posttest, and follow-up, coded 0, 1, and 2) on PDSS (at the three time points) and expected this effect to be partially mediated by cognitions as measured by the subscales of the TRF (e.g., Moscovitch, Hofmann, Suvak, & In-Albon, 2005).2 Because we were testing for cognitive mediation by each of the TRF subscales (TRF–P, TRF–M, and TRF–S), we performed these hierarchical linear modeling (HLM) mediation analyses separately for each subscale. Furthermore, we predicted that the relationships between TRF and time, and between PDSS and its predictors (time and TRF), would be moderated by treatment modality (see Figure 1). The Level 2 model allows for all of these relations to vary as a function of treatment condition.3
Figure 1.
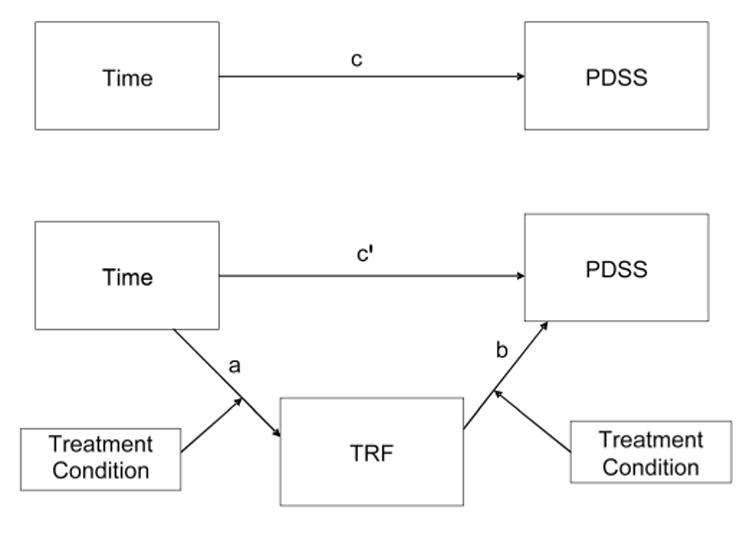
Paths a (predictor [time] to mediator [Thoughts Rating Form; TRF]), b (mediator to outcome [Panic Disorder Severity Scale; PDSS] when controlling for the predictor), c (predictor to outcome), and c′ (predictor to outcome when controlling for the mediator) represent the relationships involved in mediation. The impact of the “Treatment Condition” boxes on faths a and b represent the moderating effect of treatment condition on mediation (i.e., moderated mediation). The test of mediation is the significance of the joint path (a × b) from time to PDSS through TRF (MacKinnon et al., 2002) for each treatment condition. The joint path may be significant even if the individual paths are not (MacKinnon et al., 2002). Moderated mediation is indicated by differences in the joint path a × b across treatment conditions.
We predicted that the cognitive mediators (TRF–P, TRF–M, and TRF–S) would partially mediate the relationship between time and PDSS in the CBT treatment conditions but that they would not mediate the relation between time and PDSS in the imipramine-only condition. We used the Sobel test to examine the significance of the joint mediated pathway in each treatment condition.4 We also calculated PM (Shrout & Bolger, 2002) and Cohen's d following the recommendations by Kirk (1996) as an indication of effect size. PM is the proportion of the total effect of the independent variable (time) on the dependent variable (PDSS) that is accounted for by the mediator.
Results
The results of the moderated mediation models are shown in Table 1. Included in the table are all the path coefficients for each treatment group, plus the direct tests of the mediated pathway (a × b) for each treatment.5 The findings indicate that all three of the TRF subscales were significant partial mediators of the relationship between time and anxiety severity (PDSS) for individuals in the CBT treatments conditions. In the model using TRF–P as the mediator, the indirect effect of time on PDSS through TRF–P was significant for those in the CBT condition (z = −2.55, p < .004), those in CBT + PLA (z = −3.34, p < .004), and those in CBT + IMI (z = −2.28, p < .004), but not for those in the IMI condition (z = −0.44, ns). For the model using TRF–M as the mediator, the indirect effect of time on PDSS through TRF–M was significant for those in the CBT condition (z = −2.72, p < .004), those in the CBT + IMI condition (z = −2.39, p < .004), and those in the CBT + PLA condition (z = −1.88, p < .004), but there was no significant effect for individuals in the IMI condition (z = −1.35, ns). Finally, for the model using TRF–S as the mediator, the indirect effect of time on PDSS through TRF–S was significant for those in the CBT condition (z = −2.93, p < .004) and the CBT + PLA condition (z = −2.20, p < .004), but not for those in the IMI condition (z = 1.52, ns) or those receiving CBT + IMI (z = −0.18, ns).
Table 1.
Path Coefficients for Each Treatment Through Each Mediator
| Treatment | c | (d) | c′ | (d) | a | (d) | b | (d) | a × ba | (d) | PM |
|---|---|---|---|---|---|---|---|---|---|---|---|
| TRF–P | |||||||||||
| CBT only | −0.51* | (1.61) | −0.38* | (0.83) | −1.06* | (1.48) | 0.13 | (0.47) | −0.14* | (0.44) | .27 |
| CBT + PLA | −0.63* | (2.62) | −0.50* | (1.76) | −1.33* | (1.82) | 0.10* | (0.92) | −0.13* | (0.82) | .21 |
| CBT + IMI | −0.67* | (2.17) | −0.59* | (1.55) | −1.10* | (1.23) | 0.07 | (0.49) | −0.08* | (0.46) | .12 |
| IMI only | −0.71* | (1.84) | −0.70* | (1.50) | −0.94* | (0.99) | 0.02 | (0.11) | −0.02 | (0.11) | .02 |
|
| |||||||||||
| TRF–M | |||||||||||
| CBT only | −0.51* | (1.61) | −0.39* | (.86) | −1.06* | (1.89) | 0.12* | (0.34) | −0.13* | (0.33) | .25 |
| CBT + PLA | −0.63* | (2.62) | −0.51* | (1.68) | −1.51* | (1.58) | 0.08 | (0.42) | −0.12* | (0.40) | .19 |
| CBT + IMI | −0.67* | (2.17) | −0.56* | (1.45) | −1.57* | (1.48) | 0.07 | (0.58) | −0.11* | (0.54) | .18 |
| IMI only | −0.71* | (1.84) | −0.65* | (1.77) | −1.09* | (1.05) | 0.06 | (0.33) | −0.06 | (0.31) | .09 |
|
| |||||||||||
| TRF–S | |||||||||||
| CBT only | −0.51* | (1.61) | −0.36* | (0.81) | −0.84* | (1.40) | 0.18* | (0.62) | −0.15* | (0.56) | .29 |
| CBT + PLA | −0.63* | (2.62) | −0.52* | (2.10) | −1.17* | (1.18) | 0.10 | (0.53) | −0.11* | (0.49) | .18 |
| CBT + IMI | −0.67* | (2.17) | −0.66* | (1.96) | −1.18* | (1.39) | 0.01 | (0.06) | −0.01 | (0.06) | .01 |
| IMI only | −0.71* | (1.84) | −0.66* | (1.98) | −0.62* | (0.69) | 0.08 | (0.31) | −0.06 | (0.28) | .08 |
Note. TRF = Thought Rating Form (TRF–P = physical catastrophe cognitions; TRF–M = mental catastrophe cognitions; TRF–S = social catastrophe cognitions); CBT = cognitive-behavioral therapy; PLA = placebo; IMI = imipramine; c = slope relating time to Panic Disorder Severity Scale (PDSS); d = Cohen's d; c′ = slope relating time to PDSS, controlling for the mediator; a = slope relating time to the mediator (TRF); b = slope relating mediator (TRF) to PDSS, controlling for time; a × b = size of mediated pathway; PM = proportion of the relationship between time and PDSS mediated by the mediator (TRF).
For the mediated pathways (a × b), the p levels reported are derived from the simulation study reported by MacKinnon et al. (2002; see Footnote 4).
p < .004 (.004 is the Bonferroni corrected alpha level for the present study).
Discussion
In order to explore the mechanism of action in the treatment of panic disorder with mild or moderate agoraphobia, we analyzed the data of a large multicenter study (Barlow et al., 2000) by using multilevel analyses to study moderated mediation. Although we examined the same measures in the same data set as Hicks and colleagues (2005), the analytic strategy that was used in this study (a moderated mediation test) was very different from the predictor tests by Hicks et al. Those authors reported that catastrophic cognitions related to social events at pretest were associated with poor treatment outcome. In contrast, cognitions related to physical and mental catastrophes were unrelated to outcome. In the present study, we examined the same self-report questionnaire to measure catastrophic cognitions (the TRF) in order to test a moderated mediation model. The findings suggest that all three of the TRF subscales were significant mediators of treatment change only for individuals who received CBT, either alone or in combination with pharmacotherapy. Although all catastrophic cognitions appear to mediate the effects of CBT, we observed consistently strong mediation (in the medium range) for the catastrophic cognitions related to physical symptoms. This may suggest that CBT, whether with or without adjunctive pharmacotherapy, is particularly efficacious for reducing panic symptom if the treatment focuses on catastrophic cognitions related to physical symptoms. These results support and expand the findings on cognitive mediation reported by Smits, Powers, Cho, and Telch (2004), who showed that the effects of CBT on agoraphobia and panic symptoms were partially mediated by reductions of fear, but they too were unable to test for temporal precedence of the mediator in relation to the dependent variable. In addition, their analysis precluded the calculation of effect size for their mediation. We were able to determine that the cognitive mediators generally accounted for about 20%–30% of the change in fear obtained during our CBT treatment.
Our analyses are consistent with the notion that cognitive variables specifically mediate the effects of CBT on the reduction in panic severity. We found cognitions to significantly mediate this effect in eight of the nine possible (Type I error controlled) tests of mediation involving CBT, but in none of the tests involving imipramine. The results are consistent with our hypothesis that cognitions are modality-specific mediators. These findings are in accordance with a study by Smits et al. (2004) suggesting that CBT exerts its effects on panic disorder symptoms by reducing fearful responses to anxiety-related symptoms.
One must recognize, however, that our results do not conclusively prove that cognitive mediation occurred because we could not establish temporal precedence of the mediator (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002; Kraemer, Wilson, Fairburn, & Agras, 2002). More specifically, in order to conduct an adequate test of mediation, it is necessary to collect longitudinal data in order to capture the changes in the proposed mediator that are believed to causally affect the changes in the dependent variable. For a variable to act as a treatment mediator, it has to change before the dependent variable changes; concurrent assessments of the proposed mediator and the dependent variable do not provide any clear support the mediation model. Unfortunately, the spacing of the assessment points in this study (pretest, posttest, and 6-month follow-up) were inadequate for such tests. However, the specificity of the mediation effect to the conditions involving CBT indicate that the mediation relationship between TRF and PDSS is not a result of reverse causation (PDSS mediating changes in TRF) because such a mechanism would result in significant relationships between TRF and PDSS in the imipramine condition as well as in the CBT conditions. We recommend that future treatment trials include more frequent assessment points in order to directly test the causal ordering of the mediators and the outcomes (see Smits et al., 2006, for an example of such a test). Furthermore, the cognitions that were measured here only partially mediated CBT. Therefore, it remains uncertain whether cognitions are the only, or even the primary mechanism through which treatment change happens. A number of common/unspecific variables are conceivable and have been discussed in the psychotherapy research literature (such as working alliance). Future studies should examine whether cognitive mediation is also modality specific when compared with other forms of psychotherapy and should examine other potential mediators. The results of studies on treatment mediation can potentially lead to the further improvement of psychological treatments by identifying and emphasizing the most important ingredients of therapy.
In sum, the results suggest that changes in cognitions are causally related and modality specific to CBT. This is in line with other studies on anxiety disorders (Hofmann, 2004) and depression (Hollon, Evans, & DeRubeis, 1990) and supports the psychological model of panic disorder (Barlow, 2002; Clark, 1986; Sanderson, Rapee, & Barlow, 1989).
Footnotes
The MCCTSPD trial also included a placebo-only condition. However, only 5 patients in this condition had complete data for the present analyses and are, therefore, not included in this report. Duplicate analyses were conducted including the placebo-only participants. The results of these analyses were virtually identical to the results reported here. Note that the Thoughts Rating Form (described in the Assessments section) was added at a later point during the study, which explains the relatively small number of participants. Because individuals were randomly assigned, these data are missing at random.
A recent simulation study of lower level mediation by Pituch, Whittaker, and Stapleton (2005) showed that the Sobel test had a power of over .87 to detect a medium effect size and a power of over .57 to detect a small effect size in their simulations that were most comparable to the present study (see also MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). In addition, the Sobel test has a conservative Type I error rate; that is, a Sobel z that is sufficiently large to generate a p < .05 based on a normally distributed z statistic (z > 1.96) actually has a Type I error rate less than .002 because the Sobel statistic is not normally distributed (MacKinnon et al., 2002). The Sobel test also has the advantage of directly testing the significance of the mediated pathway, thus being able to detect significant mediation even if the components composing the pathway (a and b) are not significant (MacKinnon et al., 2002). Because we performed multiple tests of mediation (12), we used the Bonferroni correction to adjust for the multiple significance tests. We therefore set the alpha level for this study at .05/12 (.004). Because the Sobel z is not normally distributed, the alpha levels we reported in our study were derived from those found by MacKinnon et al. in their simulation study, not those based on the z distribution.
The total magnitude of an indirect (mediated) effect in lower level mediation has been shown to include an additional term (over and above a × b) related to the possibility that slopes a and b may covary (Bauer, Preacher, & Gil, 2006; Kenny et al., 2003). In all of our models, the variance of the b slope (mediator to outcome) was not significant. As a result, the final models were run with the b slope fixed. Thus, the covariances between the a and b slopes were 0, and the size of the mediated pathways became simply a × b.
Contributor Information
Stefan G. Hofmann, Department of Psychology, Boston University
Michael K. Suvak, Department of Psychology, Boston University
David H. Barlow, Department of Psychology, Boston University
M. Katherine Shear, School of Social Work, Columbia University.
Alicia E. Meuret, Department of Psychology, Southern Methodist University
David Rosenfield, Department of Psychology, Southern Methodist University.
Jack M. Gorman, Department of Psychiatry, Mount Sinai School of Medicine
Scott W. Woods, Department of Psychiatry, Yale University School of Medicine
References
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2. New York: Guilford Press; 2002. [Google Scholar]
- Barlow DH, Craske MG. Mastery of your anxiety and panic (MAP–3): Client workbook for anxiety and panic (treatments that work) Oxford, England: Oxford University Press; 2000. [Google Scholar]
- Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive–behavioral therapy, imipramine, or their combination for panic disorder: A randomized controlled trial. Journal of the American Medical Association. 2000;283:2529–2536. doi: 10.1001/jama.283.19.2529. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bauer DJ, Preacher KJ, Gil KM. Conceptualizing and testing random indirect effects and moderated mediation in multilevel models: New procedures and recommendations. Psychological Methods. 2006;10:142–163. doi: 10.1037/1082-989X.11.2.142. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Caputo GC, Bright P, Gallagher R. Assessment of fear of fear in agoraphobics: The Body Sensations Questionnaire and the Agoraphobic Cognitions Questionnaire. Journal of Consulting and Clinical Psychology. 1984;52:1090–1097. doi: 10.1037//0022-006x.52.6.1090. [DOI] [PubMed] [Google Scholar]
- Clark DM. A cognitive approach to panic. Behaviour Research and Therapy. 1986;24:461–470. doi: 10.1016/0005-7967(86)90011-2. [DOI] [PubMed] [Google Scholar]
- Guy W. ECDEU assessment manual for psychopharmacology. Washington, DC: U.S. Department of Health, Education and Welfare; 1976. (Publication No. ADM 76–338) [Google Scholar]
- Hicks TV, Leitenberg H, Barlow DH, Gorman JM, Shear MK, Woods SW. Physical, mental, and social catastrophic cognitions as prognostic factors in cognitive–behavioral and pharmacological treatments for panic disorder. Journal of Consulting and Clinical Psychology. 2005;73:506–514. doi: 10.1037/0022-006X.73.3.506. [DOI] [PubMed] [Google Scholar]
- Hofmann SG. Cognitive mediation of treatment change in social phobia. Journal of Consulting and Clinical Psychology. 2004;72:392–399. doi: 10.1037/0022-006X.72.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollon SD, Evans MD, DeRubeis RJ. Cognitive mediation of relapse prevention following treatment for depression: Implications of differential risk. In: Ingram RE, editor. Contemporary psychological approaches to depression. New York: Plenum Press; 1990. pp. 117–136. [Google Scholar]
- Kenny DA, Korchmaros JD, Bolger N. Lower level mediation in multilevel models. Psychological Methods. 2003;8:115–128. doi: 10.1037/1082-989x.8.2.115. [DOI] [PubMed] [Google Scholar]
- Kirk RE. Practical significance: A concept whose time has come. Educational and Psychological Measurement. 1996;56:746–759. [Google Scholar]
- Kraemer HC, Wilson T, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets VA. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitte K. A meta-analysis of the efficacy of psycho- and pharmacotherapy in panic disorder with and without agoraphobia. Journal of Affective Disorders. 2005;88:27–45. doi: 10.1016/j.jad.2005.05.003. [DOI] [PubMed] [Google Scholar]
- Moscovitch DA, Hofmann SG, Suvak M, In-Albon T. Mediation of changes in anxiety and depression during treatment for social phobia. Journal of Consulting and Clinical Psychology. 2005;75:945–952. doi: 10.1037/0022-006X.73.5.945. [DOI] [PubMed] [Google Scholar]
- Pituch KA, Whittaker TA, Stapleton LM. A comparison of methods to test for mediation in multisite experiments. Multivariate Behavioral Research. 2005;40:1–23. doi: 10.1207/s15327906mbr4001_1. [DOI] [PubMed] [Google Scholar]
- Raudenbush S, Bryk A, Cheong YF, Congdon R. HLM 6: Hiearchical linear and non-linear modeling. Lincolnwood, IL: Scientific Software International; 2004. [Google Scholar]
- Sanderson WC, Rapee RM, Barlow DH. The influence of an illusion of control on panic attacks induced via inhalation of 5.5% carbon dioxide-enriched air. Archives of General Psychiatry. 1989;46:157–162. doi: 10.1001/archpsyc.1989.01810020059010. [DOI] [PubMed] [Google Scholar]
- Shear MK, Brown TA, Barlow DH, Money R, Shlomskas DE, Woods SW, et al. Multicenter collaborative Panic Disorder Severity Scale. American Journal of Psychiatry. 1997;154:1571–1575. doi: 10.1176/ajp.154.11.1571. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Smits JA, Powers MB, Cho Y, Telch MJ. Mechanism of change in cognitive–behavioral treatment of panic disorder: Evidence for the fear of fear mediational hypothesis. Journal of Consulting and Clinical Psychology. 2004;72:646–652. doi: 10.1037/0022-006X.72.4.646. [DOI] [PubMed] [Google Scholar]
- Smits JA, Rosenfield D, McDonald R, Telch MJ. Cognitive mechanisms of social anxiety reduction: An examination of specificity and temporality. Journal of Consulting and Clinical Psychology. 2006;74:1203–1212. doi: 10.1037/0022-006X.74.6.1203. [DOI] [PubMed] [Google Scholar]
- Tein JY, Sandler IM, MacKinnon DP, Wolchik SA. How did it work? Who did it work for? Mediation in the context of a moderated prevention effect for children of divorce. Journal of Consulting and Clinical Psychology. 2004;72:617–624. doi: 10.1037/0022-006X.72.4.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telch MJ, Brouillard M, Telch CF, Agras WS, Taylor CB. Role of cognitive appraisal in panic-related avoidance. Behaviour Research and Therapy. 1989;27:373–383. doi: 10.1016/0005-7967(89)90007-7. [DOI] [PubMed] [Google Scholar]


