Abstract
Rationale: Indirect acute lung injury (ALI) is associated with high morbidity and mortality. No specific therapies have been developed, because the underlying pathophysiological processes remain elusive.
Objectives: To investigate the contribution of Fas-induced apoptotic and nonapoptotic/inflammatory signaling to the pathology of indirect ALI.
Methods: A mouse model of indirect ALI, induced by successive exposure to hemorrhagic shock and cecal ligation and puncture, was used. Quantification of active caspase-3 and the short splice variant of FLICE-inhibitory protein, (FLIP)short, was performed by Western blotting and immunohistochemistry, and cytokines/chemokines were assessed by cytometric bead array or ELISA. M30 immunostaining was done to evaluate epithelial cell apoptosis. Lung injury was assessed on the basis of myeloperoxidase activity, bronchoalveolar lavage protein, and lung histology.
Measurements and Main Results: Twelve hours after insult, lung monocyte chemoattractant protein-1, keratinocyte-derived chemokine, macrophage inflammatory protein-2, IL-6, tumor necrosis factor-α, and caspase-3 were increased and FLIPshort was decreased. Fas- and Fas ligand–deficient mice showed marked protection from lung inflammation and apoptosis and decreased ALI. This was associated with a 10-day survival benefit. Similarly, 4 hours after pulmonary instillation of Fas-activating antibody in vivo, lung chemokines were markedly elevated in background mice and, interestingly, to a similar degree in macrophage-deficient animals. Fas activation on lung epithelial cells in vitro led to chemokine production that was dependent on extracellular signal–regulated kinase.
Conclusions: Activation of apoptotic and nonapoptotic/inflammatory Fas signaling is an early important pathophysiological event in the development of indirect ALI after hemorrhagic shock and sepsis, in which lung epithelial cells appear to play a central role.
Keywords: hemorrhagic shock, sepsis, epithelial cell, cell death, death receptors
AT A GLANCE COMMENTARY
Scientific Knowledge on the Subject
The Fas pathway of apoptotic cell death has been implicated in the pathogenesis of acute lung injury in humans and animal models, but existing studies have focused on activation of the Fas pathway in the airspaces and alveolar epithelium. The role of Fas activation in the vascular compartment is less clear.
What This Study Adds to the Field
Activation of apoptotic and nonapoptotic/inflammatory Fas signaling is an important early pathophysiological event in the development of acute lung injury after hemorrhagic shock and sepsis, with lung epithelial cells appearing to play a central role.
Acute lung injury (ALI) affects about 15 to 65 per 100,000 inhabitants per year (1, 2). Lethality associated with ALI ranges between 32 and 55% (3, 4). Data from the ALIVE (Acute Lung Injury Verification of Epidemiology) study indicate that adult respiratory distress syndrome (ARDS)/ALI affects about 7% of all intensive care unit admissions and that 54% of patients with mild ALI develop full-blown ARDS within 24 hours (3). Thus far, no specific therapies exist for ALI/ARDS. This is, at least in part, to be blamed on the lack of understanding of the underlying pathophysiological processes, which itself is aggravated by the deficiency of clear definitions and the heterogeneity of the diseases summarized under the concept of ALI. To overcome this deficit, a disease entity–based subgrouping (5) and a reevaluation of the definition of ARDS (6) have been demanded. In this respect, it has been recognized that ALI can be differentiated into direct ALI (ALIdirect) and indirect ALI (ALIindirect) by taking into account potentially dissimilar pathophysiology, different radiological manifestations and respiratory mechanics, as well as the disparate susceptibility to ventilatory strategies (5, 7–11). Epidemiologically, ALIdirect accounts for about 57% and is caused mainly by pneumonia, aspiration, and lung trauma; ALIindirect accounts for the residual 43%, with nonpulmonary sepsis and trauma being the most frequent underlying diseases (4). Current understanding of the development of ALI is based on two concepts: the “neutrophil hypothesis” suggests that, early in the development of ALI, neutrophils in circulation and in the lung become activated, experiencing a delay in apoptosis and an increase in respiratory burst. This is likely to be mediated through proinflammatory mediators such as granulocyte- and granulocyte/macrophage colony-stimulating factors and various chemokines (12–14). This results in the prolonged presence of activated neutrophils in the lung, their delayed phagocytosis, and consequently the postponed switch from a proinflammatory to an antiinflammatory environment after their phagocytosis by macrophages (15, 16). The “epithelial hypothesis” is based on observations that lung epithelial cells undergo apoptosis during ARDS/ALI (17–19), thus contributing to destruction of the pulmonary epithelium and compromised barrier function. This theory is supported by the fact that increased expression of Fas on epithelial cells, along with enhanced extravasation of Fas ligand (FasL)–expressing cells, can be observed during ALI (19–21). However, these concepts have been built mainly around models of ALIdirect. In fact, it has been proposed that endothelial rather than epithelial damage is the major pathophysiological event for ALIindirect (7, 10).
Thus, the underlying pathological mechanisms for ALIindirect remain controversial and insufficiently elucidated. In this regard, it is not clear whether programmed cell death plays an important role in the pathogenesis of ALIindirect (as has been suggested for ALIdirect [19, 22]), nor whether the pathways and cell types involved are sufficiently elucidated. In our previous studies, we have demonstrated that hemorrhage-primed neutrophils are capable of inducing ALIindirect in a septic environment, identifying them as a major contributor to the pathology of indirect ALI and supporting the neutrophil hypothesis (12, 23, 24). However, the upstream mechanisms that lead to the release of the major chemokines attracting these primed neutrophils, and potentially other leukocytes, as well as the cellular source of these chemotactic mediators, are unclear. In this regard, it appears that activation of Fas in the lung is also associated with a release of inflammatory mediators and particularly chemokines (25, 26). However, the underlying cell types and signal transduction pathways remain elusive. On a single-cell level, macrophages as well as epithelial cells appear to possess the potential to produce inflammatory mediators on Fas activation (27–30). For extrapulmonary epithelial cells the mitogen-activated protein kinase (MAPK)/extracellular signal–regulated kinase (ERK) pathway has been suggested to play a role in Fas-mediated inflammation (30).
In this context and based on the questions formulated above, we tested the hypothesis that activation of the extrinsic death receptor pathway via Fas contributes to the pathogenesis of indirect acute lung injury by regulating both apoptosis and inflammation of lung epithelial cells in a clinically relevant model of ALIindirect induced by a two-hit model of hemorrhagic shock followed by polymicrobial sepsis.
Some of the results of these studies have been previously reported in the form of an abstract (31, 32).
METHODS
Animals
Male mutant mice, expressing nonfunctional Fas receptor (B6.MRL-Faslpr/J [lpr]) or Fas ligand (B6Smn.C3-Faslgld/J [gld]), both 8 weeks old, or deficient in monocytes/macrophages (B6C3Fe a/a-Csf1op/J [Csf1op]), 3 weeks old, and age-matched controls (C57BL/6J [C57]) (all from Jackson Laboratory, Bar Harbor, ME) were used. Experiments were done in accordance with National Institutes of Health (Bethesda, MD) guidelines and were approved by the local animal use committee. See Table E1 in the online supplement for an overview of the experimental groups.
Indirect ALI
Indirect ALI (ALIindirect) was induced as described previously (12, 24, 33, 34) by hemorrhagic shock (HEM) followed by cecal ligation and puncture (CLP) 24 hours thereafter. Importantly, while we show only the sham group as our control (which we have not found to differ from HEM or CLP alone) for the studies here, we have previously documented that neither HEM nor CLP alone is capable of inducing substantial/consistent increases in indices of lung inflammation, apoptosis, or injury (12, 24, 33, 34).
Intratracheal Instillation
Intratracheal instillation of purified hamster anti-mouse Fas monoclonal antibody Jo2 (BD Biosciences, San Jose, CA) was performed as described previously (33, 35).
Experimental Groups and Sample Acquisition for In Vivo Experiments
Blood, lungs, and plasma were harvested 12 or 24 hours after sepsis (i.e., 36 or 48 h after HEM). In a separate set of experiments survival of lpr and C57 animals was assessed for 10 days. In a separate set lungs were instilled in vivo with 10% buffered formaldehyde (30 μl/g body weight), excised, and stored for 24 hours in 10% formaldehyde. In a separate set, mice were exsanguinated 12 hours after CLP and bronchoalveolar lavage was performed. Macrophage-deficient mice underwent intratracheal instillation of anti-mouse Fas monoclonal antibody Jo2 (2 μg/g body weight; BD Biosciences) and were killed 4 hours thereafter.
Cell Culture of Epithelial Cell Lines
LA-4 (CCL-196; American Type Culture Collection [ATCC], Manassas, VA) and MLE 12 (CRL-2110; ATCC) cells were cultured with or without 10 μM Ras/Raf inhibitor FTI-277 or 30 μM mitogen-activated protein (MAP) kinase kinase inhibitor PD98059 (Calbiochem; EMD Biosciences, San Diego, CA) (36) and stimulated with a 50-ng/ml concentration of Fas monoclonal antibody (Jo2) or isotype control (both from BD Biosciences).
Cell Proliferation Assay
Proliferation of LA-4 and MLE 12 cells was assessed with a CyQUANT cell proliferation assay kit (Invitrogen Molecular Probes, Eugene, OR).
ERK1/2 Phosphorylation Quantification
ERK1/2 phosphorylation was quantified with a cellular activation of signaling ELISA kit (CASE, SuperArray; Bioscience Corporation, Frederick, MD) (37).
Quantification of Cytokines/Chemokines and Myeloperoxidase Activity
Mouse keratinocyte-derived chemokine (KC) and macrophage inflammatory protein (MIP)-2 (both from R&D Systems, Minneapolis, MN) and monocyte chemoattractant protein (MCP)-1 (BD Biosciences) were determined by ELISA as described previously (33, 35, 38). Mouse tumor necrosis factor (TNF)-α, IL-6, IFN-γ, IL-12, MCP-1, and IL-10 levels were quantified by the cytometric bead array technique (BD cytometric bead array mouse inflammation kit; BD Biosciences) as described previously (33). Lung myeloperoxidase (MPO) was quantified as described previously (34).
Active Caspase-3, FLIP, and β-Actin Western Blotting
Membranes were incubated with Fas-associated death domain (FADD)–like IL-1β–converting enzyme inhibitory protein (FLIP) antibody (Cell Signaling Technology, Inc., Beverly, MA) at a concentration of 1:1,000 or with cleaved caspase-3 (Asp175) antibody (Cell Signaling Technology, Inc.) at a concentration of 1:500 at 4°C overnight and subsequently with ECL rabbit IgG, horseradish peroxidase–linked whole antibody from donkey (GE Health Care Bio-Sciences, Piscataway, NJ). Membranes were developed using enhanced chemiluminescence technique (ChemiGlow; Alpha Innotech, San Leandro, CA). Membranes were reincubated with polyclonal rabbit anti-mouse β-actin (Abcam, Cambridge, MA) at a concentration of 1:10,000 and with ECL rabbit IgG, horseradish peroxidase–linked whole antibody and again developed.
Immunohistochemistry, TUNEL Staining, and Hematoxylin–Eosin Staining
Active caspase-3 and M30 immunohistochemistry, terminal deoxynucleotidyltransferase biotin-dUTP nick end labeling (TUNEL) staining, and lung hematoxylin and eosin staining were performed as described previously (33, 39).
Statistical Analysis
Data are presented as means ± SEM. Statistical analysis was performed by one-way analysis of variance (ANOVA) or two-way ANOVA followed by the Student-Newman-Keuls test, and by Fisher's exact test for survival. P < 0.05 was considered significant.
RESULTS
Lung Apoptosis in ALIindirect
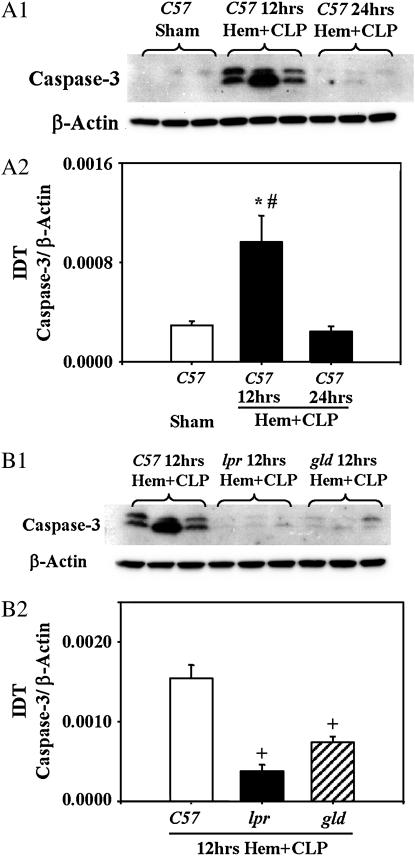
Lung active caspase-3.
Active caspase-3 was virtually absent in sham-treated animals (Figure 1, A1 and A2). However, 12 hours after hemorrhagic shock followed by cecal ligation and puncture (HEM+CLP) a marked increase in pulmonary caspase-3 activity was noticed (Figure 1, A1 and A2). These elevated caspase-3 levels returned to baseline within 24 hours after the insult (Figure 1, A1 and A2). Moreover, caspase-3 was markedly decreased in gld animals and even more in lpr animals 12 hours after HEM+CLP when compared with background animals (Figure 1, B1 and B2).
Figure 1.
(A1) Pulmonary caspase-3 in sham-treated background (C57) mice and C57 mice 12 and 24 hours after hemorrhagic shock and sepsis (HEM+CLP). (A2) Integrated density (IDT) values of active caspase-3 relative to IDT values of β-actin of n = 6 animals per group. Quantification was done by Western blotting and densitometry. Statistical analysis involved one-way analysis of variance (ANOVA) followed by the Student-Newman-Keuls test. *p < 0.05 versus corresponding sham group, #P < 0.05 versus corresponding 24 hours HEM+CLP. (B1) Pulmonary caspase-3 in background (C57) mice, Fas-deficient (lpr) mice, and Fas ligand (gld) mice 12 hours after HEM+CLP (B1). (B2) IDT values of active caspase-3 relative to IDT values of β-actin of n = 6 animals per group. Quantification was done by Western blotting and densitometry. Statistical analysis involved one-way ANOVA followed by the Student-Newman-Keuls test. +P < 0.05 versus C57 HEM+CLP.
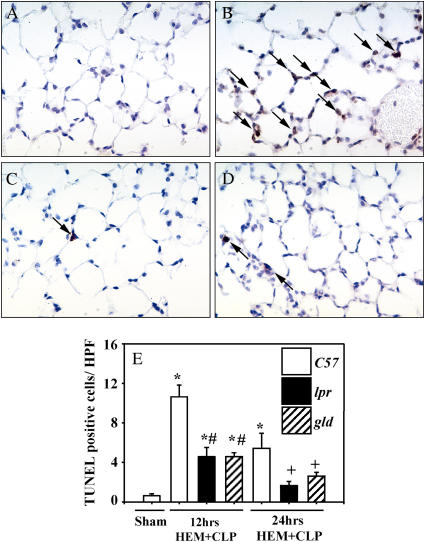
Lung caspase-3 immunohistochemistry and TUNEL.
Virtually no active caspase-3–positive cells (fewer than one per high-power field) were found in the lungs of animals having undergone sham procedures (Figure 2A). Twelve hours after HEM+CLP lung cells staining positive for active caspase-3 were substantially increased in background C57 animals (Figure 2B). lpr (Figure 2C) and gld (Figure 2D) animals showed substantially fewer cells with positive staining at this time point. At 24 hours after HEM+CLP virtually no positive cells were seen in any experimental group (data not shown). In addition, TUNEL-positive cells were rare in sham-treated animals but experienced a substantial increase 12 and 24 hours after HEM+CLP in background animals (Figure 2E). In lpr and gld animals, the number of TUNEL-positive cells was markedly decreased at both time points when compared with sham-treated animals (Figure 2E).
Figure 2.
(A–D) Representative active caspase-3 immunohistochemistry of lung tissue samples from (A) a sham-treated animal and from (B) background (C57), (C) Fas-deficient (lpr), and (D) Fas ligand–deficient (gld) animals 12 hours after hemorrhagic shock and sepsis (HEM+CLP). Arrows indicate active caspase-3–positive cells. Original magnification, ×400. (E) Terminal deoxynucleotidyltransferase biotin-dUTP nick end labeling (TUNEL)–positive cells per high-power field (HPF) 12 and 24 hours after insult in the same experimental groups. * P< 0.05 versus sham group, #P < 0.05 versus C57 24 hours after HEM+CLP, +P < 0.05 versus C57 24 hours after HEM+CLP.
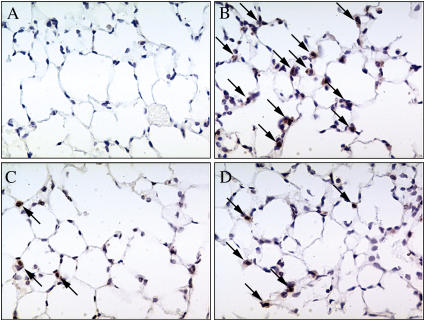
Lung M30 immunohistochemistry.
M30 is a neo-epitope that is revealed when the intermediate filament protein cytokeratin-18 in epithelial cells is cleaved by caspase-3/-6/-9 at Asp-396 (40), thus indicating epithelial cell–specific expression of apoptosis. Virtually no M30-positive cells (fewer than one per high-power field) were found in the lungs of sham-treated animals (Figure 3A). At 12 hours after insult, lung cells staining positive for M30 were substantially increased in background C57 animals (Figure 3B). lpr (Figure 3C) and gld (Figure 3D) animals showed substantially fewer cells with positive staining for M30 at this time point. At 24 hours after HEM+CLP, the same results were observed as seen at 12 hours after the insult; however, in all groups less overall staining was evident (data not shown).
Figure 3.
Representative M30 immunohistochemistry of lung tissue samples from (A) sham-treated, (B) background (C57), (C) Fas-deficient (lpr), and (D) Fas ligand–deficient (gld) mice 12 hours after hemorrhagic shock and sepsis. Arrows indicate M30-positive cells. Original magnification, ×400.
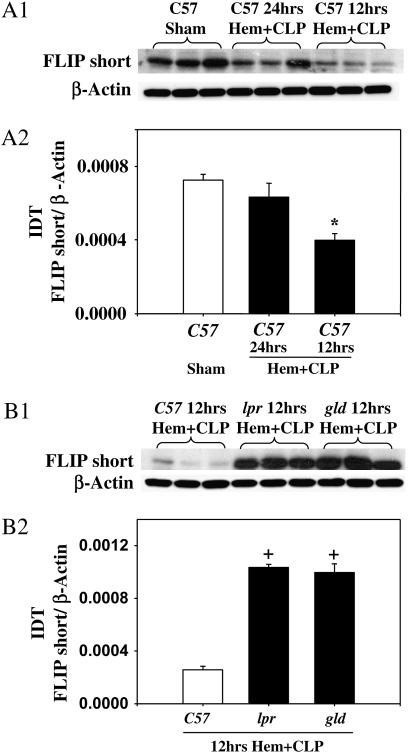
Pulmonary FLIPshort.
The short splice variant of FLIP, FLIPshort, abundantly present in sham-treated lungs, experiencing a significant decrease in response to HEM+CLP 12 hours, and to a lesser degree 24 hours, after the insult (Figure 4, A1 and A2). Interestingly, 12 hours after HEM+CLP there was significantly more inhibitory FLIPshort present in the lungs of lpr and gld animals when compared with C57 background animals (Figure 4, B1 and B2).
Figure 4.
(A1) Pulmonary FLIPshort (the short splice variant of FLICE-inhibitory protein) in sham background (C57) mice, and in C57 mice 12 and 24 hours after hemorrhagic shock and sepsis (HEM+CLP). (A2) Integrated density (IDT) values of FLIPshort relative to IDT values of β-actin of n = 5 animals per group. Quantification was done by Western blotting and densitometry. Statistical analysis involved one-way ANOVA followed by the Student-Newman-Keuls test. *P < 0.05 versus corresponding sham group. (B1) Pulmonary FLIPshort in C57, Fas-deficient (lpr), and Fas ligand–deficient (gld) mice 12 hours after HEM+CLP. (B2) IDT values of active caspase-3 relative to IDT values of β-actin of n = 6 animals per group. Quantification was done by Western blotting and densitometry. Statistical analysis involved one-way ANOVA followed by the Student-Newman-Keuls test. +P < 0.05 versus C57 HEM+CLP.
Lung Injury and Survival in ALIindirect
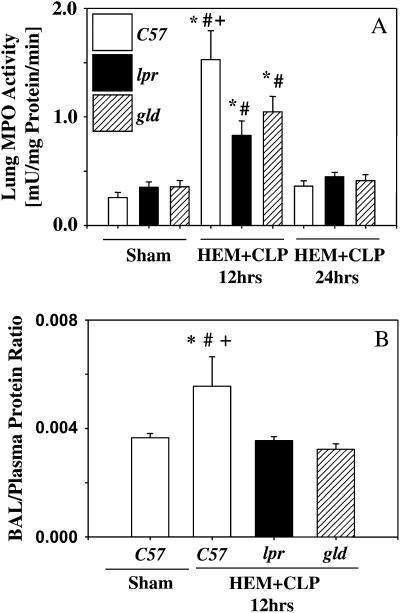
Lung MPO activity and bronchoalveolar lavage protein.
Lung MPO activity was markedly increased 12 hours after HEM+CLP in background mice (Figure 5A). lpr animals showed a marked decrease, whereas gld animals exhibited a trend toward lower levels of lung MPO activity, although MPO activity in lpr and gld animals was still significantly increased when compared with the corresponding sham-treated animals (Figure 5A). Bronchoalveolar lavage (BAL) fluid protein was quantified 12 hours after the insult (Figure 5B). The BAL fluid:plasma protein ratio was substantially augmented in background animals at this time point, whereas lpr or gld animals did not demonstrate such an increase (Figure 5B).
Figure 5.
(A) Lung myeloperoxidase (MPO) activity concentrations in Fas-deficient (lpr), Fas ligand–deficient (gld), and wild-type (C57) mice 12 and 24 hours after hemorrhagic shock and sepsis (HEM+CLP). n = 8 per group. Statistical analysis involved two-way ANOVA followed by the Student-Newman-Keuls test. *P < 0.05 versus corresponding sham group, #P < 0.05 versus corresponding group 24 hours after HEM+CLP, +P < 0.05 versus lpr 12 hours after HEM+CLP. (B) Quantification of total bronchoalveolar lavage (BAL) protein in Fas-deficient (lpr), Fas ligand–deficient (gld), and wild-type (C57) mice 12 hours after HEM+CLP. n = 6 per group. Statistical analysis involved one-way ANOVA followed by the Student-Newman-Keuls test. *P < 0.05 versus sham group, #P < 0.05 versus lpr, +P < 0.05 versus gld.
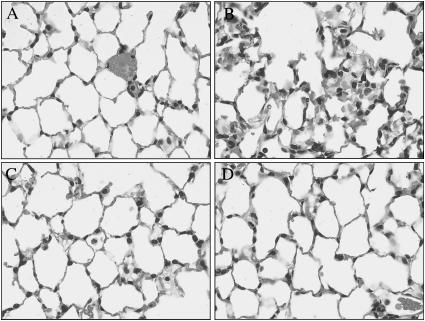
Lung histology.
Lung hematoxylin and eosin–prepared sections displayed lung congestion, disrupted alveolar architecture, and increased numbers of neutrophils within the alveolar walls in background animals 12 hours after HEM+CLP (Figure 6B) when compared with sham-treated animals (Figure 6A). Sections from lpr (Figure 6C) and gld (Figure 6D) animals showed marked protection after the insult. Lung histology at 24 hours showed fewer numbers of neutrophils within the alveolar walls when compared with the 12-hour time point, although alveolar thickening and disrupted alveolar architecture were still present to a greater extent in background animals compared with lpr and gld animals.
Figure 6.
(A–D) Representative hematoxylin and eosin–stained preparations of lung tissue from animals 12 hours after hemorrhagic shock and sepsis (HEM+CLP). (A) Sham animals display regular lung histology. (B) Twelve hours after HEM+CLP background animals displayed typical signs of congestion, disruption of alveolar architecture, and increased numbers of neutrophils within the alveolar walls. (C) Fas-deficient (lpr) and (D) Fas ligand (FasL)–deficient (gld) animals were largely protected from these alterations. Original magnification, ×400.
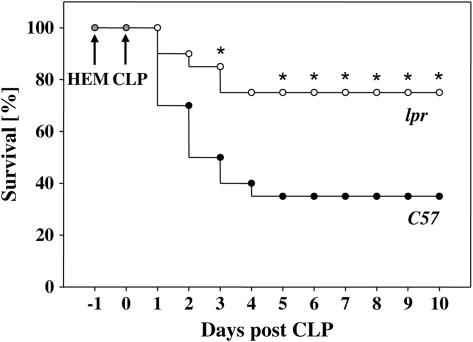
Survival.
After HEM+CLP, a marked survival benefit was observed in lpr animals when compared with their backgrounds (n = 20 per group) (Figure 7). The observed survival benefit was obvious on Day 3 after CLP and lasted until the end of the observation period (Day 10). It should be noted that HEM, when followed by sham CLP, produces no mortality (as this is a nonlethal model of shock) and that when CLP follows sham HEM, the survival at 7 days post-CLP was 70% (12).
Figure 7.
Ten-day survival in Fas-deficient (lpr) and background (C57) animals after hemorrhagic shock (HEM) and subsequent cecal ligation and puncture (CLP) 24 hours thereafter. *P < 0.05 versus C57 (Fisher's exact test of n = 20 animals per group).
Inflammation in ALIindirect
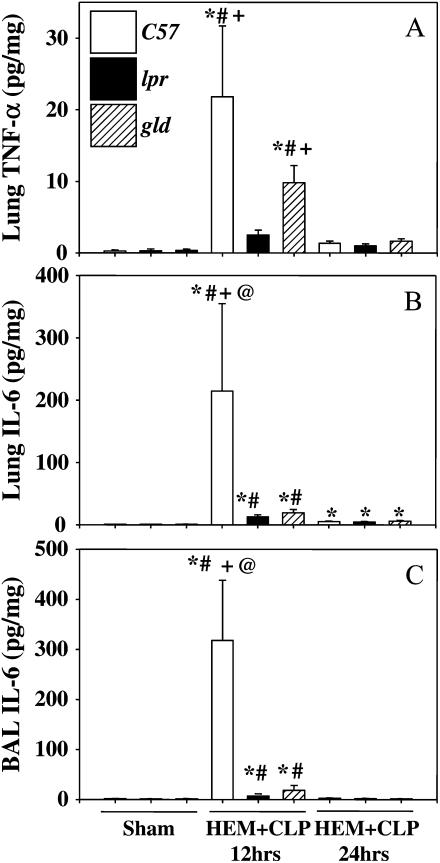
Lung and BAL cytokines.
Twelve hours after sepsis (i.e., 36 h posthemorrhage) a marked increase in lung TNF-α (Figure 8A) and IL-6 (Figure 8B) and in BAL fluid IL-6 (Figure 8C) was noticed in background (C57) animals when compared with sham-treated animals. Interestingly, lpr and gld mice showed a marked decrease in these mediator concentrations at this time point when compared with background animals. At 24 hours after the insult, lung IL-6 but not lung TNF-α or BAL fluid IL-6 was still markedly elevated in C57, lpr, and gld animals when compared with sham-treated animals. TNF-α in BAL fluid was detectable only in 75% of the animals. In addition, TNF-α concentrations, even when detectable, were evident only at the low end of the standard curve.
Figure 8.
(A) Lung tumor necrosis factor (TNF)-α, (B) lung IL-6, and (C) bronchoalveolar lavage (BAL) IL-6 concentrations in Fas-deficient (lpr), Fas ligand–deficient (gld), and wild-type (C57) mice 12 and 24 hours after hemorrhagic shock and sepsis (HEM+CLP). Quantification was done by ELISA or cytometric bead assay (CBA). n = 8 per group for lung and n = 6 per group for BAL. Statistical analysis involved two-way ANOVA followed by the Student-Newman-Keuls test. *P < 0.05 versus corresponding sham group, #P < 0.05 versus corresponding group 24 hours after HEM+CLP, +P < 0.05 versus lpr 12 hours after HEM+CLP, @P < 0.05 versus gld 12 hours after HEM+CLP.
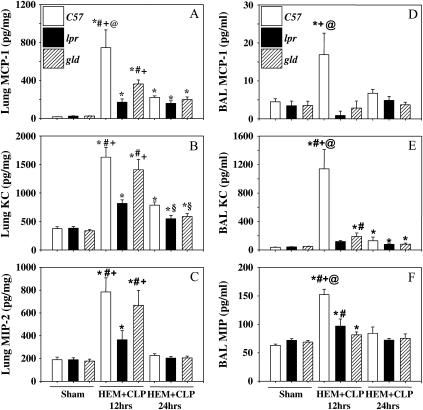
Lung and BAL fluid chemokines.
Twelve hours after sepsis, a marked increase in lung and BAL fluid MCP-1 (Figures 9A and 9D), KC (Figures 9B and 9E), and MIP-2 (Figures 9C and 9F) was noticed in background animals when compared with sham-treated animals. Interestingly, lpr mice showed a marked decrease in all chemokines at this time point when compared with background animals. gld mice exhibited a significant decrease in lung MCP-1 (Figure 9A) and BAL fluid MCP-1 (Figure 9D), KC (Figure 9E), and MIP-2 (Figure 9F) at the 12-hour time point. At 24 hours after the insult, lung MCP-1 (Figure 9A), KC (Figure 9B), and BAL fluid KC (Figure 9E) were still markedly elevated in C57 animals; however, lung KC levels were substantially reduced in lpr and gld animals compared with their controls.
Figure 9.
Lung and bronchoalveolar lavage (BAL) fluid macrophage chemoattractant protein (MCP)-1 (A and D), keratinocyte-derived chemokine (KC) (B and E), and macrophage inflammatory protein (MIP)-2 (C and F) concentrations in Fas-deficient (lpr), Fas ligand–deficient (gld), and wild-type (C57) mice 12 and 24 hours after hemorrhagic shock and sepsis (HEM+CLP). Quantification was done via ELISA or cytometric bead assay. n = 8 per group for lung and n = 6 per group for BAL. Statistical analysis involved two-way ANOVA followed by the Student-Newman-Keuls test. *P < 0.05 versus corresponding sham group, #P < 0.05 versus corresponding group 24 hours after HEM+CLP, +P < 0.05 versus lpr 12 hours after HEM+CLP, @P < 0.05 versus gld 12 hours after HEM+CLP, §P < 0.05 versus C57 24 hours after HEM+CLP.
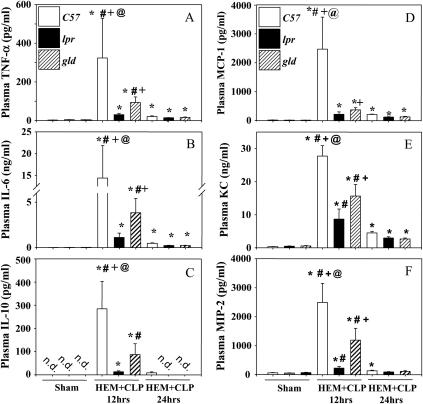
Plasma cytokines/chemokines.
Plasma cytokines TNF-α (Figure 10A), IL-6 (Figure 10B), and IL-10 (Figure 10C) and chemokines MCP-1 (Figure 10D), KC (Figure 10E), and MIP-2 (Figure 10F) were all markedly elevated in background animals 12 hours after HEM+CLP. Both lpr and gld animals showed a marked decrease in all mentioned plasma mediators. Plasma TNF-α, IL-6, MCP-1, KC, and MIP-2, but not IL-10, were still markedly elevated 24 hours after the insult, with no significant differences between C57, lpr, and gld animals.
Figure 10.
Plasma tumor necrosis factor (TNF)-α (A), IL-6 (B), IL-10 (C), macrophage chemoattractant protein (MCP)-1 (D), keratinocyte-derived chemokine (KC) (E), and macrophage inflammatory protein (MIP)-2 (F) in Fas-deficient (lpr), Fas ligand–deficient (gld), and wild-type mice (C57) 12 and 24 hours after hemorrhagic shock and sepsis (HEM+CLP). Quantification was done by ELISA or cytometric bead assay. n = 8 per group. Statistical analysis involved two-way ANOVA followed by the Student-Newman-Keuls test. *P < 0.05 versus corresponding sham group, #P < 0.05 versus corresponding group 24 hours after HEM+CLP, +P < 0.05 versus lpr 12 hours after HEM+CLP, @P < 0.05 versus gld 12 hours after HEM+CLP.
Fas-mediated Inflammation In Vitro
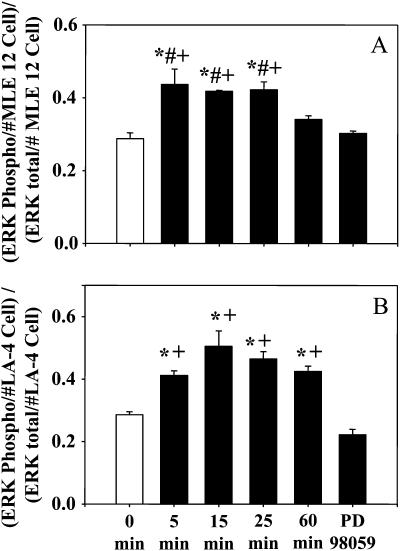
Fas-induced ERK1/2 phosphorylation in cultured pulmonary epithelial cells.
The preceding studies examining lung M30 antigen expression, as well as our prior investigations silencing pulmonary Fas expression, suggested that lung epithelial cells might be an important player modulating the Fas-driven pathology seen here. Thus, we decided to examine the effects of in vitro Fas ligation on inflammatory cell signaling in mouse epithelial cells.
Activation of Fas by incubation of epithelial cells with Jo2 antibody led to a significant increase in ERK1/2 phosphorylation as early as 5 minutes after exposure, leading to an early peak at 5 to 25 minutes in MLE 12 cells (Figure 11A) and at 15 minutes in LA-4 cells (Figure 11B). After 60 minutes, ERK1/2 phosphorylation was still increased in LA-4 cells (Figure 11B) and had already returned to baseline in MLE 12 cells (Figure 11A). Preincubation with the ERK1/2 inhibitor PD 98059 prevented ERK1/2 phosphorylation in both cell lines (Figures 11A and 11B).
Figure 11.
Time course of Fas-induced activation of extracellular signal–regulated kinase (ERK)1/2 (as illustrated by the increase in the ratio of phosphorylated to total ERK) in (A) MLE 12 cells and (B) LA-4 cells after exposure to Jo2 antibody (50 ng/ml). n = 4 per group. Statistical analysis involved one-way ANOVA followed by the Student-Newman-Keuls test. * P< 0.05 versus 0 minutes, #P < 0.05 versus 60 minutes, +P < 0.05 versus PD 98059.
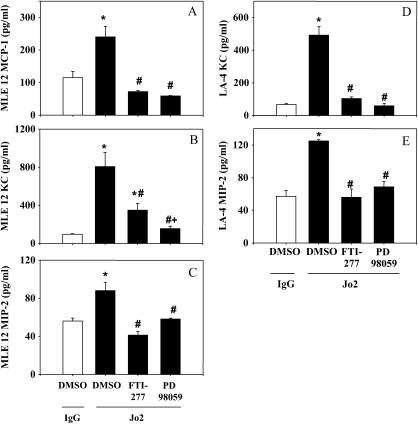
Fas-induced chemokine production in cultured pulmonary epithelial cells.
Activation of Fas on MLE 12 cells (Figures 12A–12C) and LA-4 cells (Figures 12D and 12E), by administering Jo2 for 4 hours, led to a marked increase in MLE 12 MCP-1 (Figure 12A), MLE 12 KC (Figure 12B), MLE 12 MIP-2 (Figure 12C), LA-4 KC (Figure 12D), and LA-4 MIP-2 (Figure 12E), respectively, in cell supernatants, when compared with isotype-stimulated controls. Up- or downstream inhibition of ERK1/2, with FTI-277 or PD 98059, respectively, markedly abrogated chemokine production in these cells (Figures 12A–12E). Incubation of epithelial cells with Jo2 for 4 hours, however, did not affect proliferation of the cells, demonstrating that the observed differences in chemokine production were not the result of differences in cell proliferation/cell death (data not shown).
Figure 12.
Chemokine production by MLE 12 cells (A–C) and LA-4 cells (D and E) 4 hours after activation of Fas (Jo2 monoclonal antibody at 50 ng/ml). n = 4 per group. Statistical analysis involved one-way ANOVA followed by the Student-Newman-Keuls test. *P < 0.05 versus DMSO/IgG, #P < 0.05 versus DMSO/Jo2, +P < 0.05 versus FTI-277/Jo2.
Fas-mediated Inflammation In Vivo
Activation of Fas-induced chemokine production in macrophage-deficient animals.
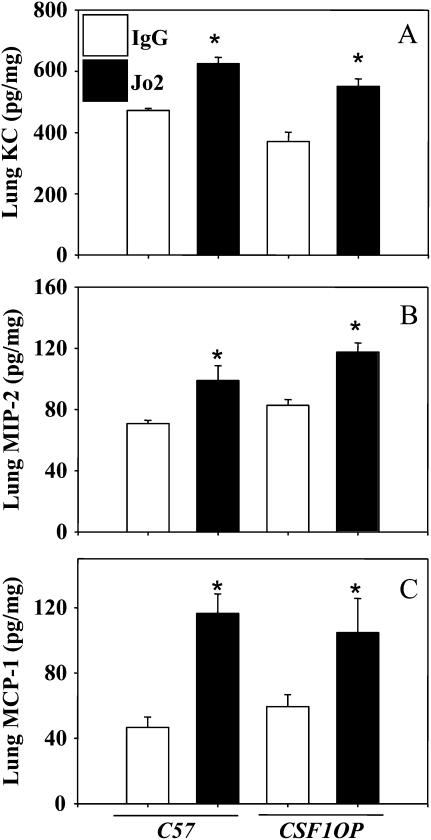
Finally, to determine the extent to which the in vitro observations outlined above translate back to the intact, in vivo situation and in an attempt to learn about the contribution of local lung macrophages to this Fas-triggered inflammatory response, we examined the in vivo chemokine response of C57 background animals as compared with macrophage-deficient CSF1op mice (as noted in the online supplement and as we have previously reported [34], the number of macrophages in CSF1op mice was reduced by a magnitude of 70 to 75% when compared with background controls levels). In this regard, activation of Fas by intratracheal instillation of Jo2 in vivo led to a marked increase in KC (Figure 13A), MIP-2 (Figure 13B), and MCP-1 (Figure 13C) production in lung tissue in both background and macrophage-deficient animals when compared with their respective isotype controls.
Figure 13.
(A–C) Chemokine production in lungs of background (C57) and macrophage-deficient animals (CFS1OP) 4 hours after instillation of Fas-activating antibody Jo2. n = 4 or 5 per group. Statistical analysis involved one-way ANOVA followed by the Student-Newman-Keuls test. * P< 0.05 versus corresponding IgG.
DISCUSSION
Here, we have investigated whether apoptosis of lung epithelial cells and production of chemokines via activation of the Fas receptor–driven pathway were pathophysiologically relevant in the development of ALIindirect after hemorrhagic shock and sepsis (HEM+CLP) and how the effects were mediated.
Our results indicate that apoptosis in the lung appears to be a relevant and early pathophysiological event after HEM+CLP. The absence of key elements of the Fas receptor–driven pathway decreased the extent of lung epithelial cell apoptosis, suggesting that the extrinsic death receptor pathway is a primary route by which lung epithelial cells undergo cell death under these circumstances. Beyond the establishment of proof for this more classic feature of Fas ligation, that is, apoptosis of pulmonary epithelial cells, we noted substantial evidence for nonapoptotic signaling and its potential pathophysiological relevance in this scenario of ALIindirect. In this regard, the production and release of lung cytokines/chemokines were ameliorated in Fas- and Fas ligand–deficient animals. This was also associated with reduced recruitment of neutrophils into the lung. These findings were allied with improved lung histology and a decrease in the extent of ALI, as determined by protein leakage, resulting in a marked survival benefit in animals lacking the Fas receptor. To the extent that these changes might be a result of concomitant alterations in Fas- and FasL-mediated proinflammatory signaling events, our in vitro data demonstrate that when challenging lung epithelial cells with Fas-activating antibody this results in phosphorylation of ERK1/2 and early production of chemokines. This increase in chemokine release appears to be mediated through Fas activation of the Ras/Raf and MAP/ERK kinase (MEK) pathways. Furthermore, the production of MCP-1, MIP-2, and KC in lung tissue, in vivo, after Fas activation was tissue macrophage/monocyte independent, whereas the release of KC and MIP-2, but not MCP-1, into the BAL appeared to require the presence of macrophages/monocytes.
So far the role of the Fas–FasL system in the pathogenesis of ALIindirect has remained elusive. In contrast, the relevance of Fas activation in the development of direct ALI (ALIdirect) has been previously indicated. In this regard, lung epithelial cells overexpress Fas during ALIdirect (19) or ARDS (41, 42). Soluble Fas ligand (sFasL) is also present in the injured lung/ARDS in increased concentrations and correlates with poor outcome (19, 43). The activation of Fas in the lung in vivo induces alveolar epithelial cell apoptosis (26, 43, 44). In particular, distal alveolar epithelial cells are susceptible to Fas-induced cell death (45). The absence of a functional Fas–FasL system in mice or the administration of Fas-blocking antibodies decreases the severity of ALIdirect (22) and diminishes epithelial cell apoptosis and pulmonary inflammation (19), respectively. Thus, epithelial cell apoptosis mediated through Fas appears to be relevant not only in the pathogenesis of ALIdirect but also in ALIindirect, as our data indicate that after HEM+CLP an early and robust activation of caspase-3 via Fas occurs.
The cell-specific relevance of Fas activation in macrophages versus epithelial cells is not completely understood so far. Matute-Bello and colleagues have addressed this issue in a setting in which pulmonary Fas was activated via instillation of Fas-activating antibody Jo2 in chimeric mice that carried the Fas receptor on either myeloid cells or nonmyeloid cells only (46). They indicated that induction of apoptosis via Fas on nonmyeloid but not myeloid cells induced acute lung injury, emphasizing the role of lung parenchymal cell apoptosis in the pathogenesis of acute lung injury. Our findings corroborate these results in a clinically relevant double-hit model of indirect ALI as we observed decreased apoptosis in epithelial cells being associated with a decreased severity of ALI and increased capacity to survive after hemorrhagic shock and sepsis. Furthermore, these findings are in line with our previous observation that silencing of Fas in lung epithelial cells ameliorates ALI by decreasing epithelial cell apoptosis and thus preventing major pulmonary histological changes (33). Interestingly, although qualitatively showing the same trends, lpr and gld animals were subtly different in their response to the insult. gld animals showed slightly more apoptosis and higher levels for several lung and plasma cytokines/chemokines when compared with lpr animals in response to hemorrhagic shock and sepsis, although they were still markedly protected when compared with background animals. One possibility is that other pathways of FADD activation, such as activation of the TNF-receptor I (p55), might mediate these effects (47).
In addition to these observations, our data demonstrate that the release of inflammatory mediators is also associated with the engagement of Fas and FasL. Our data indicate that, in the absence of Fas or FasL, the pulmonary production and release of inflammatory mediators is greatly diminished and so is, consequently, the recruitment of inflammatory leukocytes into the lung. Furthermore, when Fas-activating antibody was instilled into macrophage-deficient animals, the production of chemokines in the lung was almost identical to that seen in wild-type mice. In addition, early after direct incubation with Jo2 in vitro, lung epithelial cells produced MIP-2, KC, and MCP-1. These data corroborate the findings of Wortinger and coworkers, who found that instillation of recombinant FasL into the lung induces production of KC and MIP-2 and the recruitment of neutrophils into the lung (25). However, the source for these mediators remained elusive. Furthermore, Matute-Bello and coworkers delineated that Fas activation in vivo resulted in acute lung epithelial injury, lung inflammation, and recruitment of neutrophils (26) and that Fas also modulated LPS-induced lung inflammation (48). Thus, FasL-induced inflammation appears to be frequently followed by neutrophil immigration. In this regard, it has been found that overexpressing FasL in tumor cells initiates their rejection and this appears to be mediated by neutrophils (49). Moreover, intraperitoneal injection of FasL induces chemokine production in resident macrophages, consequently causing neutrophil extravasation (27). It is tempting to speculate that recruitment of neutrophils after epithelial Fas activation in the lung could link our current observations with the previously described deleterious role that has been ascribed to primed neutrophils in mediating ALIindirect (12).
However, the cell types as well as the signaling cascades involved in the production of chemokines after activation of the Fas death receptor pathway remained unclear. In this regard, Neff and colleagues have demonstrated that in a model of direct acute lung injury not only lung apoptosis, but also the production of KC and MIP-2, were markedly diminished in Fas-deficient animals (50). Incubation of a murine alveolar macrophage cell line with Fas-activating antibodies resulted in increased release of MIP-2 (50). Although their experiments clearly indicate a role for the alveolar macrophage in the inflammatory response to Fas, they do not exclude a role for epithelial cells. Interestingly, no increased release of KC was noticed in these in vitro experiments, suggesting that this might be cell population specific as well as macrophage independent. Previous data from our own laboratory also indicate that deficiency of macrophages decreases pulmonary chemokines and cytokines in ALIindirect (34). Captivatingly, Matute-Bello and colleagues indicated that Fas expression restricted to either myeloid or nonmyeloid cells of the lung did not lead to marked production of chemokines on Fas stimulation (46), suggesting that perhaps both cell types contribute to the production of chemokines seen after Fas activation in the lung (26). Interestingly, our results also demonstrate that the production of chemokines in the lung in vivo after activation of Fas was independent of the presence of alveolar macrophages. With respect to their sources, several cell types have been implicated as being capable of producing chemokines in response to Fas activation. Hohlbaum and coworkers indicated that preapoptotic resident peritoneal macrophages produce MIP-2 in response to FasL (27). Human vascular smooth muscle cells react with increased transcription of MCP-1 and IL-8, when challenged with an agonistic Fas antibody (51). Isolated human monocytes and macrophages released IL-8 when incubated with Fas ligand regulated by FLIP and nuclear factor (NF)-κB (28). However, it has also been demonstrated that FLIP is capable of activating ERK via signaling through death domain receptor-interacting protein (RIP) as well as Raf-1 and MEK in human T lymphocytes (52). Human endothelial cells are also known to generate IL-8 and MCP-1 when incubated with recombinant FasL or Fas agonistic antibody CH-11 (53). In addition, it has been demonstrated that Fas induces secretion of IL-8 in vitro in bronchiolar epithelial cells after 6 hours of incubation (29). O'Brien and coworkers reported that IL-8 production in colon epithelial cells in response to Fas activation was ERK1/2 and p38 MAPK dependent (30). In our experiments, inhibiting ERK1/2 signaling abrogated the release of KC, MIP-2, and MCP-1 in pulmonary epithelial cells after Fas activation. Thus, in light of our findings and the current literature the existence of an alternative Fas-driven proinflammatory signaling cascade in various parenchymal and nonparenchymal cells can be suggested. This cascade involves the activation of FLIP rather than caspase-8 and the subsequent activation of TNF receptor–associated factor (TRAF)1/2 and NF-κB and/or Raf/Ras, MEK, and ERK1/2, resulting in increased transcription and release of chemokines and other proinflammatory mediators (52, 54, 55). One potential limitation of our in vitro studies is the specificity of the inhibitors used. Although PD 98059 and FTI-277 have been widely tested and demonstrated to possess high specificity, there always remains the small possibility of off-target effects at some level (56–58). In the Fas signaling cascade FLIPshort appears to have inhibitory effects. FLIPshort lacks the caspase-like domain, which leaves it with two dual death effector domains only, rendering it enzymatically inactive. This inhibits further processing of caspase-8 (54, 59). Our experiments support this inhibitory effect of cellular FLIPshort as pulmonary FLIPshort correlated inversely with active caspase-3, in that high FLIPshort levels in sham-treated animals markedly decreased in response to HEM+CLP, whereas active caspase-3 significantly increased in the injured lung.
On the basis of the data presented here and our previous observations (12, 33–35), we propose the following pathogenic mechanism in the early development of indirect ALI resultant from hemorrhagic shock and sepsis: initially, early activation of the Fas receptor on pulmonary epithelial cells appears to take place. This, in turn, not only induces the onset of apoptosis in some of these cells but also appears to trigger a chemotactic/inflammatory response, in which epithelial cells produce chemokines and attract neutrophils and monocytes and thus potentially arrange their own removal, anticipating their apoptotic death. However, it appears that the invasion of these phagocytes is not solely beneficial, in particular with respect to primed neutrophils, which are capable of further promoting the development of acute lung injury. This is in contrast to the current concept of lung epithelial cells being the victim in ALI. Alternatively, we suggest that they actively participate in the development of ALIindirect by producing chemokines and thus eventually recruiting activated neutrophils and/or activating neighboring cells, such as macrophages. Consequently, inhibiting Fas activation on pulmonary epithelial cells appears to be a promising therapeutic principle for mitigating the development of indirect acute lung injury, as our data indicate that the Fas system is uniquely positioned to regulate pulmonary epithelial cell apoptosis and inflammation as well as mediate the invasion of potentially harmful trafficking leukocytes.
Supplementary Material
Acknowledgments
The authors thank Paul Monfils and Virginia Hovanesian for excellent technical assistance.
Supported by a grant from the National Institutes of Health (HL73525 to A.A.) and by research funds from Lifespan/Rhode Island Hospital.
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.200611-1743OC on June 28, 2007
Conflict of Interest Statement: None of the authors has a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
- 1.Frutos-Vivar F, Nin N, Esteban A. Epidemiology of acute lung injury and acute respiratory distress syndrome. Curr Opin Crit Care 2004;10:1–6. [DOI] [PubMed] [Google Scholar]
- 2.MacCallum NS, Evans TW. Epidemiology of acute lung injury. Curr Opin Crit Care 2005;11:43–49. [DOI] [PubMed] [Google Scholar]
- 3.Brun-Buisson C, Minelli C, Bertolini G, Brazzi L, Pimentel J, Lewandowski K, Bion J, Romand JA, Villar J, Thorsteinsson A, et al. Epidemiology and outcome of acute lung injury in European intensive care units: results from the ALIVE Study. Intensive Care Med 2004;30:51–61. [DOI] [PubMed] [Google Scholar]
- 4.Bersten AD, Edibam C, Hunt T, Moran J. Incidence and mortality of acute lung injury and the acute respiratory distress syndrome in three Australian states. Am J Respir Crit Care Med 2002;165:443–448. [DOI] [PubMed] [Google Scholar]
- 5.Takeda S, Ishizaka A, Fujino Y, Fukuoka T, Nagano O, Yamada Y, Takezawa J. Time to change diagnostic criteria of ARDS: towards the disease entity-based subgrouping. Pulm Pharmacol Ther 2005;18:115–119. [DOI] [PubMed] [Google Scholar]
- 6.Abraham E, Matthay MA, Dinarello CA, Vincent JL, Cohen J, Opal SM, Glauser M, Parsons P, Fisher CJ Jr, Repine JE. Consensus conference definitions for sepsis, septic shock, acute lung injury, and acute respiratory distress syndrome: time for a reevaluation. Crit Care Med 2000;28:232–235. [DOI] [PubMed] [Google Scholar]
- 7.Menezes SL, Bozza PT, Faria Neto HC, Laranjeira AP, Negri EM, Capelozzi VL, Zin WA, Rocco PR. Pulmonary and extrapulmonary acute lung injury: inflammatory and ultrastructural analyses. J Appl Physiol 2005;98:1777–1783. [DOI] [PubMed] [Google Scholar]
- 8.Pelosi P, Gattinoni L. Acute respiratory distress syndrome of pulmonary and extra-pulmonary origin: fancy or reality? Intensive Care Med 2001;27:457–460. [DOI] [PubMed] [Google Scholar]
- 9.Gattinoni L, Pelosi P, Suter PM, Pedoto A, Vercesi P, Lissoni A. Acute respiratory distress syndrome caused by pulmonary and extrapulmonary disease: different syndromes? Am J Respir Crit Care Med 1998;158:3–11. [DOI] [PubMed] [Google Scholar]
- 10.Callister ME, Evans TW. Pulmonary versus extrapulmonary acute respiratory distress syndrome: different diseases or just a useful concept? Curr Opin Crit Care 2002;8:21–25. [DOI] [PubMed] [Google Scholar]
- 11.Pelosi P, D'Onofrio D, Chiumello D, Paolo S, Chiara G, Capelozzi VL, Barbas CS, Chiaranda M, Gattinoni L. Pulmonary and extrapulmonary acute respiratory distress syndrome are different. Eur Respir J Suppl 2003;42:48s–56s. [DOI] [PubMed] [Google Scholar]
- 12.Ayala A, Chung CS, Lomas JL, Song GY, Doughty LA, Gregory SH, Cioffi WG, LeBlanc BW, Reichner J, Simms HH, et al. Shock-induced neutrophil mediated priming for acute lung injury in mice: divergent effects of TLR-4 and TLR-4/FasL deficiency. Am J Pathol 2002;161:2283–2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matute-Bello G, Liles WC, Radella F, Steinberg KP, Ruzinski JT, Hudson LD, Martin TR. Modulation of neutrophil apoptosis by granulocyte colony-stimulating factor and granulocyte/macrophage colony-stimulating factor during the course of acute respiratory distress syndrome. Crit Care Med 2000;28:1–7. [DOI] [PubMed] [Google Scholar]
- 14.Aggarwal A, Baker CS, Evans TW, Haslam PL. G-CSF and IL-8 but not GM-CSF correlate with severity of pulmonary neutrophilia in acute respiratory distress syndrome. Eur Respir J 2000;15:895–901. [DOI] [PubMed] [Google Scholar]
- 15.Teder P, Vandivier RW, Jiang D, Liang J, Cohn L, Pure E, Henson PM, Noble PW. Resolution of lung inflammation by CD44. Science 2002;296:155–158. [DOI] [PubMed] [Google Scholar]
- 16.Fadok VA, Bratton DL, Konowal A, Freed PW, Westcott JY, Henson PM. Macrophages that have ingested apoptotic cells in vitro inhibit proinflammatory cytokine production through autocrine/paracrine mechanisms involving TGF-β, PGE2, and PAF. J Clin Invest 1998;101:890–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bardales RH, Xie SS, Schaefer RF, Hsu SM. Apoptosis is a major pathway responsible for the resolution of type II pneumocytes in acute lung injury. Am J Pathol 1996;149:845–852. [PMC free article] [PubMed] [Google Scholar]
- 18.Guinee D Jr, Brambilla E, Fleming M, Hayashi T, Rahn M, Koss M, Ferrans V, Travis W. The potential role of BAX and BCL-2 expression in diffuse alveolar damage. Am J Pathol 1997;151:999–1007. [PMC free article] [PubMed] [Google Scholar]
- 19.Kitamura Y, Hashimoto S, Mizuta N, Kobayashi A, Kooguchi K, Fujiwara I, Nakajima H. Fas/FasL-dependent apoptosis of alveolar cells after lipopolysaccharide-induced lung injury in mice. Am J Respir Crit Care Med 2001;163:762–769. [DOI] [PubMed] [Google Scholar]
- 20.Martin TR, Nakamura M, Matute-Bello G. The role of apoptosis in acute lung injury. Crit Care Med 2003;31:S184–S188. [DOI] [PubMed] [Google Scholar]
- 21.Martin TR, Hagimoto N, Nakamura M, Matute-Bello G. Apoptosis and epithelial injury in the lungs. Proc Am Thorac Soc 2005;2:214–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matute-Bello G, Frevert CW, Liles WC, Nakamura M, Ruzinski JT, Ballman K, Wong VA, Vathanaprida C, Martin TR. Fas/Fas ligand system mediates epithelial injury, but not pulmonary host defenses, in response to inhaled bacteria. Infect Immun 2001;69:5768–5776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parsey MV, Kaneko D, Shenkar R, Abraham E. Neutrophil apoptosis in the lung after hemorrhage or endotoxemia: apoptosis and migration are independent of IL-1β. Clin Immunol 1999;91:219–225. [DOI] [PubMed] [Google Scholar]
- 24.Lomas-Neira JL, Chung CS, Grutkoski PS, Miller EJ, Ayala A. CXCR2 inhibition suppresses hemorrhage-induced priming for acute lung injury in mice. J Leukoc Biol 2004;76:58–64. [DOI] [PubMed] [Google Scholar]
- 25.Wortinger MA, Foley JW, Larocque P, Witcher DR, Lahn M, Jakubowski JA, Glasebrook A, Song HY. Fas ligand–induced murine pulmonary inflammation is reduced by a stable decoy receptor 3 analogue. Immunology 2003;110:225–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Matute-Bello G, Winn RK, Jonas M, Chi EY, Martin TR, Liles WC. Fas (CD95) induces alveolar epithelial cell apoptosis in vivo: implications for acute pulmonary inflammation. Am J Pathol 2001;158:153–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hohlbaum AM, Gregory MS, Ju ST, Marshak-Rothstein A. Fas ligand engagement of resident peritoneal macrophages in vivo induces apoptosis and the production of neutrophil chemotactic factors. J Immunol 2001;167:6217–6224. [DOI] [PubMed] [Google Scholar]
- 28.Park DR, Thomsen AR, Frevert CW, Pham U, Skerrett SJ, Kiener PA, Liles WC. Fas (CD95) induces proinflammatory cytokine responses by human monocytes and monocyte-derived macrophages. J Immunol 2003;170:6209–6216. [DOI] [PubMed] [Google Scholar]
- 29.Hagimoto N, Kuwano K, Kawasaki M, Yoshimi M, Kaneko Y, Kunitake R, Maeyama T, Tanaka T, Hara N. Induction of interleukin-8 secretion and apoptosis in bronchiolar epithelial cells by Fas ligation. Am J Respir Cell Mol Biol 1999;21:436–445. [DOI] [PubMed] [Google Scholar]
- 30.O'Brien D, O'Connor T, Shanahan F, O'Connell J. Activation of the p38 MAPK and ERK1/2 pathways is required for Fas-induced IL-8 production in colonic epithelial cells. Ann N Y Acad Sci 2002;973:161–165. [DOI] [PubMed] [Google Scholar]
- 31.Perl M, Lomas-Neira J, Perl U, Chung CS, Ayala A. Contribution of nonapoptotic and apoptotic Fas signaling to the pathology of extrapulmonary acute lung injury [abstract]. Shock 2006;25(Suppl 1):1.16775883 [Google Scholar]
- 32.Perl M, Chung CS, Lomas-Neira J, Perl U, Biffl WL, Cioffi WG, Ayala A. Role of lung epithelial cells in Fas mediated inflammation during extrapulmonary acute lung injury [abstract]. Inflamm Res 2007;56:S70–S71. [Google Scholar]
- 33.Perl M, Chung CS, Lomas-Neira J, Rachel TM, Biffl WL, Cioffi WG, Ayala A. Silencing of Fas, but not caspase-8, in lung epithelial cells ameliorates pulmonary apoptosis, inflammation, and neutrophil influx after hemorrhagic shock and sepsis. Am J Pathol 2005;167:1545–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lomas-Neira J, Chung CS, Perl M, Gregory S, Biffl W, Ayala A. Role of alveolar macrophage and migrating neutrophils in hemorrhage-induced priming for ALI subsequent to septic challenge. Am J Physiol Lung Cell Mol Physiol 2006;290:L51–L58. [DOI] [PubMed] [Google Scholar]
- 35.Lomas-Neira JL, Chung CS, Wesche DE, Perl M, Ayala A. In vivo gene silencing (with siRNA) of pulmonary expression of MIP-2 versus KC results in divergent effects on hemorrhage-induced, neutrophil-mediated septic acute lung injury. J Leukoc Biol 2005;77:846–853. [DOI] [PubMed] [Google Scholar]
- 36.Guo Z, Zhang M, Tang H, Cao X. Fas signal links innate and adaptive immunity by promoting dendritic-cell secretion of CC and CXC chemokines. Blood 2005;106:2033–2041. [DOI] [PubMed] [Google Scholar]
- 37.Versteeg HH, Nijhuis E, van den Brink GR, Evertzen M, Pynaert GN, van Deventer SJ, Coffer PJ, Peppelenbosch MP. A new phosphospecific cell-based ELISA for p42/p44 mitogen-activated protein kinase (MAPK), p38 MAPK, protein kinase B and cAMP-response-element-binding protein. Biochem J 2000;350:717–722. [PMC free article] [PubMed] [Google Scholar]
- 38.Perl M, Gebhard F, Brückner UB, Ayala A, Braumüller S, Büttner C, Kinzl L, Knoferl MW. Pulmonary contusion causes impairment of macrophage and lymphocyte immune functions and increases mortality associated with a subsequent septic challenge. Crit Care Med 2005;33:1351–1358. [DOI] [PubMed] [Google Scholar]
- 39.De Paepe ME, Mao Q, Chao Y, Powell JL, Rubin LP, Sharma S. Hyperoxia-induced apoptosis and Fas/FasL expression in lung epithelial cells. Am J Physiol Lung Cell Mol Physiol 2005;289:L647–L659. [DOI] [PubMed] [Google Scholar]
- 40.Leers MP, Kolgen W, Bjorklund V, Bergman T, Tribbick G, Persson B, Bjorklund P, Ramaekers FC, Bjorklund B, Nap M, et al. Immunocytochemical detection and mapping of a cytokeratin 18 neo-epitope exposed during early apoptosis. J Pathol 1999;187:567–572. [DOI] [PubMed] [Google Scholar]
- 41.Albertine KH, Soulier MF, Wang Z, Ishizaka A, Hashimoto S, Zimmerman GA, Matthay MA, Ware LB. Fas and Fas ligand are up-regulated in pulmonary edema fluid and lung tissue of patients with acute lung injury and the acute respiratory distress syndrome. Am J Pathol 2002;161:1783–1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hashimoto S, Kobayashi A, Kooguchi K, Kitamura Y, Onodera H, Nakajima H. Upregulation of two death pathways of perforin/granzyme and FasL/Fas in septic acute respiratory distress syndrome. Am J Respir Crit Care Med 2000;161:237–243. [DOI] [PubMed] [Google Scholar]
- 43.Matute-Bello G, Liles WC, Steinberg KP, Kiener PA, Mongovin S, Chi EY, Jonas M, Martin TR. Soluble Fas ligand induces epithelial cell apoptosis in humans with acute lung injury (ARDS). J Immunol 1999;163:2217–2225. [PubMed] [Google Scholar]
- 44.Matute-Bello G, Liles WC, Frevert CW, Nakamura M, Ballman K, Vathanaprida C, Kiener PA, Martin TR. Recombinant human Fas ligand induces alveolar epithelial cell apoptosis and lung injury in rabbits. Am J Physiol Lung Cell Mol Physiol 2001;281:L328–L335. [DOI] [PubMed] [Google Scholar]
- 45.Nakamura M, Matute-Bello G, Liles WC, Hayashi S, Kajikawa O, Lin SM, Frevert CW, Martin TR. Differential response of human lung epithelial cells to Fas-induced apoptosis. Am J Pathol 2004;164:1949–1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Matute-Bello G, Lee JS, Liles WC, Frevert CW, Mongovin S, Wong V, Ballman K, Sutlief S, Martin TR. Fas-mediated acute lung injury requires Fas expression on nonmyeloid cells of the lung. J Immunol 2005;175:4069–4075. [DOI] [PubMed] [Google Scholar]
- 47.Park HH, Lo YC, Lin SC, Wang L, Yang JK, Wu H. The death domain superfamily in intracellular signaling of apoptosis and inflammation. Annu Rev Immunol 2007;25:561–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Matute-Bello G, Winn RK, Martin TR, Liles WC. Sustained lipopolysaccharide-induced lung inflammation in mice is attenuated by functional deficiency of the Fas/Fas ligand system. Clin Diagn Lab Immunol 2004;11:358–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Seino K, Kayagaki N, Okumura K, Yagita H. Antitumor effect of locally produced CD95 ligand. Nat Med 1997;3:165–170. [DOI] [PubMed] [Google Scholar]
- 50.Neff TA, Guo RF, Neff SB, Sarma JV, Speyer CL, Gao H, Bernacki KD, Huber-Lang M, McGuire S, Hoesel LM, et al. Relationship of acute lung inflammatory injury to Fas/FasL system. Am J Pathol 2005;166:685–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schaub FJ, Han DK, Liles WC, Adams LD, Coats SA, Ramachandran RK, Seifert RA, Schwartz SM, Bowen-Pope DF. Fas/FADD-mediated activation of a specific program of inflammatory gene expression in vascular smooth muscle cells. Nat Med 2000;6:790–796. [DOI] [PubMed] [Google Scholar]
- 52.Kataoka T, Budd RC, Holler N, Thome M, Martinon F, Irmler M, Burns K, Hahne M, Kennedy N, Kovacsovics M, et al. The caspase-8 inhibitor FLIP promotes activation of NF-κB and ERK signaling pathways. Curr Biol 2000;10:640–648. [DOI] [PubMed] [Google Scholar]
- 53.Yamaoka-Tojo M, Yamaguchi S, Nitobe J, Abe S, Inoue S, Nozaki N, Okuyama M, Sata M, Kubota I, Nakamura H, et al. Dual response to Fas ligation in human endothelial cells: apoptosis and induction of chemokines, interleukin-8 and monocyte chemoattractant protein-1. Coron Artery Dis 2003;14:89–94. [DOI] [PubMed] [Google Scholar]
- 54.Thome M, Tschopp J. Regulation of lymphocyte proliferation and death by FLIP. Nat Rev Immunol 2001;1:50–58. [DOI] [PubMed] [Google Scholar]
- 55.Golks A, Brenner D, Krammer PH, Lavrik IN. The c-FLIP-NH2 terminus (p22-FLIP) induces NF-κB activation. J Exp Med 2006;203:1295–1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dudley DT, Pang L, Decker SJ, Bridges AJ, Saltiel AR. A synthetic inhibitor of the mitogen-activated protein kinase cascade. Proc Natl Acad Sci USA 1995;92:7686–7689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lerner EC, Qian Y, Blaskovich MA, Fossum RD, Vogt A, Sun J, Cox AD, Der CJ, Hamilton AD, Sebti SM. Ras CAAX peptidomimetic FTI-277 selectively blocks oncogenic Ras signaling by inducing cytoplasmic accumulation of inactive Ras–Raf complexes. J Biol Chem 1995;270:26802–26806. [DOI] [PubMed] [Google Scholar]
- 58.Sun J, Qian Y, Hamilton AD, Sebti SM. Ras CAAX peptidomimetic FTI 276 selectively blocks tumor growth in nude mice of a human lung carcinoma with K-Ras mutation and p53 deletion. Cancer Res 1995;55:4243–4247. [PubMed] [Google Scholar]
- 59.Krueger A, Schmitz I, Baumann S, Krammer PH, Kirchhoff S. Cellular FLICE-inhibitory protein splice variants inhibit different steps of caspase-8 activation at the CD95 death-inducing signaling complex. J Biol Chem 2001;276:20633–20640. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.