Abstract
Substantial evidence suggests the involvement of oxidative stress in the pathophysiology of congestive heart failure and its antecedent conditions such as cardiac hypertrophy and adverse remodelling after MI. Oxidative stress describes an imbalance between antioxidant defences and the production of reactive oxygen species (ROS), which at high levels cause cell damage but at lower levels induce subtle changes in intracellular signalling pathways (termed redox signalling). ROS are derived from many sources including mitochondria, xanthine oxidase, uncoupled nitric oxide synthases and NADPH oxidases. The latter enzymes are especially important in redox signalling, being implicated in the pathophysiology of hypertension and atherosclerosis, and activated by diverse pathologically relevant stimuli. We review the contribution of ROS to heart failure pathophysiology and discuss potential therapies that may specifically target detrimental redox signalling. Indeed, drugs such as ACE inhibitors and statins may act in part through such mechanisms. A better understanding of redox signalling mechanisms may enable the development of new targeted therapeutic strategies rather than the non‐specific antioxidant approaches that have to date been disappointing in clinical trials.
Increased oxidative stress is involved in the pathophysiology of diverse diseases such as atherosclerosis, neurodegeneration, renal disease and cancer. Over the past 20 years, significant evidence has suggested a role for increased oxidative stress in the pathophysiology of congestive heart failure (CHF).1 Indirect evidence of increased oxidative stress in patients with established CHF includes the increase of oxidative stress markers both systemically and in pericardial fluid.2 A significant correlation is reported between level of oxidative stress and severity of heart failure. Increased oxidative stress is implicated in most types of CHF, including that resulting from ischaemic and non‐ischaemic cardiomyopathy, pressure and volume overload, tachycardiomyopathy and chemotherapy‐induced failure.
Traditionally, the main pathological effects of oxidative stress have been considered to be free radical‐induced oxidation and damage, resulting in cell dysfunction, necrosis and/or apoptosis. In the context of CHF, most of these free radicals were thought to emanate from inefficient mitochondrial metabolism and/or impaired antioxidant defences. More recently, however, it has become evident that oxidative stress and reactive oxygen species (ROS) may have much more subtle effects—for example, the highly specific modulation of intracellular signalling pathways and proteins, which involves the stimulated production of ROS by various highly specialised enzymes.3,4 These effects are relevant not only to CHF but also to its predisposing conditions, such as left ventricular hypertrophy (LVH) and adverse remodelling after myocardial infarction. In this article, we review some of the recent advances in our understanding of how oxidative stress influences different aspects of the phenotype of the failing heart (eg, hypertrophy, fibrosis, chamber remodelling, contractile dysfunction and endothelial dysfunction) and consider how this knowledge might be applied to develop new therapeutic approaches.
ROS, oxidative stress and the pathophysiological actions of ROS
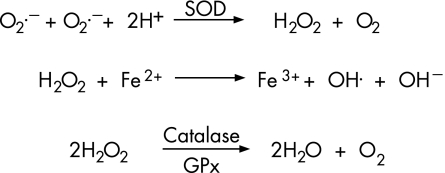
ROS are oxygen‐based chemical species characterised by their high reactivity. They include free radicals (ie, species with ⩾1 unpaired electrons, such as superoxide (O2.−) and hydroxyl (OH.) and non‐radicals capable of generating free radicals (eg, hydrogen peroxide (H2O2); fig 1). If present in excess, free radicals can induce oxidation and damage to DNA, membranes, proteins and other macromolecules. Diverse specific and non‐specific antioxidant defence systems therefore exist to scavenge and degrade ROS to non‐toxic molecules.5 The balance between ROS production and their removal by antioxidant systems describes the “redox state” of a cell; a pathological imbalance in favour of excess ROS is termed oxidative stress. A small amount of O2.− is normally produced as a byproduct of the use of molecular oxygen during mitochondrial oxidative phosphorylation. A family of superoxide dismutase enzymes rapidly converts O2.− to H2O2, which is itself broken down by glutathione peroxidase and catalase to water. Under pathological conditions, the single‐electron reduction of H2O2 may lead to the formation of highly reactive OH radicals (fig 1).
Figure 1 Key reactions underlying the formation and degradation of hydrogen peroxide (H2O2). O2.−, superoxide; OH., hydroxyl; SOD, superoxide dismutase; GPx, glutathione peroxidase.
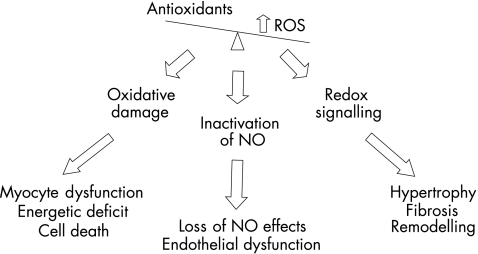
The pathophysiological effects of ROS depend on the type, concentration and specific site of production and involve three broad types of action (fig 2). When the local levels of ROS are high, they tend to react with numerous protein centres, DNA, cell membranes and other molecules, causing considerable cellular damage as well as generating other more reactive radicals. At lower concentrations, however, local targeted production of ROS serves as a second‐messenger system that transmits biological information through the highly specific modulation of intracellular signalling molecules, enzymes and proteins. This so‐called redox signalling function is especially true for the ROS, H2O2, which is more stable and diffusible than radical species such as O2.−, but also applies to nitric oxide. Redox signalling processes are involved in the activation of many signal transduction protein kinases and transcription factors, the stimulation of DNA synthesis and expression of growth‐related genes,3,5 and the regulation of myocardial excitation–contraction coupling.6 The third general ROS‐related pathophysiological mechanism involves the reaction of O2.− with the signalling molecule nitric oxide, which in health has a central role in vascular homeostasis as well as in modulating cardiac function. The reaction between O2.− and nitric oxide leads to inactivation of nitric oxide and loss of its biological activity as well as the generation of the peroxynitrite (ONOO−) species.5 The reaction is especially likely to occur when both O2.− and nitric oxide levels are high and antioxidant activity is low. Interestingly, although high levels of ONOO− may induce non‐specific toxic effects, at lower levels this species is itself capable of modulating signalling events in vivo, indicating an additional level of complexity.
Figure 2 Main pathophysiological effects of oxidative stress in heart failure. ROS, reactive oxygen species; NO, nitric oxide.
Sources of ROS
There are several potential sources of ROS in LVH and CHF (box 1), which have varying effects on pathophysiology as discussed later.
Box 1: Main sources of reactive oxygen species
Mitochondria
Inflammatory cells
Xanthine oxidase
Uncoupled NO synthases
-
NADPH oxidases
-
-
Nox1, vascular smooth muscle
-
-
Nox2, cardiomyocytes, endothelial cells, fibroblasts and inflammatory cells
-
-
Nox3, not reported in the cardiovascular system
-
-
Nox4, all cardiovascular cell types
-
-
Nox5, human endothelial cells/vascular smooth muscle
-
-
Cytochrome P450 reductases
Cyclo‐oxygenases.
Excessive ROS derived from mitochondria have been shown in cardiomyocytes from experimental models of myocardial infarction and rapid pacing‐induced heart failure.7 The enzyme xanthine oxidase produces O2.− as a byproduct of the terminal steps of purine catabolism and recent studies suggest that it contributes to oxidative stress in CHF. Xanthine oxidase expression and activity are increased in experimental models of CHF as well as in human end‐stage CHF.8 Nitric oxide synthase enzymes normally generate nitric oxide, but may instead generate O2.− if they become “uncoupled”, a state that is especially likely to occur in the setting of deficiency of the NOS cofactor BH4 or the NOS substrate l‐arginine.9 NOS uncoupling and subsequent O2.− production are implicated in the genesis of vascular endothelial dysfunction in patients with heart failure.10 Infiltrating inflammatory cells may also be important sources of oxidative stress, especially in conditions such as myocarditis and in the early stages after myocardial infarction. Recent evidence suggests that complex enzymes called NADPH oxidases are especially important with regard to redox signalling in CHF and its antecedent conditions.11,12 These enzymes catalyse electron transfer from NADPH to molecular oxygen, resulting in the formation of O2.−. NADPH oxidase activity has been found to be increased in experimental models of LVH and CHF as well as in end‐stage failing human myocardium.13,14,15 Interestingly, ROS produced by NADPH oxidases can promote ROS generation by other sources, thereby amplifying total levels of ROS. For example, O2.− from NADPH oxidase may oxidise and degrade BH4, thereby leading to NOS uncoupling, and this mechanism has been shown in diabetes and experimental hypertension.9 Similarly, NADPH oxidase‐derived ROS may also activate xanthine oxidase.5
The NADPH oxidase superfamily
NADPH oxidases are of particular interest because they seem to be the only enzymes specifically designed for “purposeful” ROS production. Furthermore, the complexity of their regulation suggests that they may be attractive targets for new treatments. The classic NADPH oxidase was characterised in neutrophils where the O2.− generated on oxidase activation plays an essential role in phagocytosis and microbial killing.11 However, similar enzymes are present in numerous other cell types, including endothelial cells, fibroblasts, vascular smooth muscle and cardiomyocytes. These oxidases are specifically activated by diverse stimuli that are important in cardiovascular pathology—for example, angiotensin II, endothelin 1, cytokines, growth factors, oxidised LDL, shear stress, mechanical stretch and others.5,11 Notably, important roles have been shown for NADPH oxidases in redox signalling events involved in hypertension, atherosclerosis, endothelial activation and angiogenesis, as well as in endothelial dysfunction.
All NADPH oxidases contain a core catalytic subunit called Nox. Five distinct Nox isoforms, each encoded for by separate genes, have been described (box 1),11 of which Nox2 and Nox4 are the most abundant in the heart and are expressed in cardiomyocytes, endothelial cells and fibroblasts.12 Nox2 and Nox4‐based oxidases seem to be differentially activated and may exert distinct signalling effects, even when expressed in the same cell type. Of potential therapeutic interest, the Nox2‐based oxidase requires binding to several additional regulatory subunits, including Rac1, before its activation. As treatment with statins can inhibit enzymatic reactions that require Rac1 translocation, Nox2 activation could potentially be targeted by these drugs. By contrast, it seems that Rac1 is not required for activation of the Nox4‐based oxidase.
Effects of ROS on development of hypertrophy
Cardiac hypertrophy is a key component of the phenotype of the failing heart, regardless of the underlying cause. Growing evidence implicates redox‐sensitive pathways in the development of cardiac hypertrophy either in response to neurohumoral stimuli or chronic pressure overload. In cultured cardiomyocytes, hypertrophy induced by angiotensin II, endothelin 1, norepinephrine, tumour necrosis factor α or pulsatile mechanical stretch has been shown to involve intracellular ROS production and to be inhibited by antioxidants.12 The mechanism involves ROS‐mediated activation of various mitogen activated protein kinases and the transcription factor nuclear factor‐κB. In vivo, the development of experimental pressure overload LVH in mice or guinea pigs is attenuated by antioxidants, implying a role for ROS.
Recently, NADPH oxidases have been suggested to be key sources of these ROS. In experimental pressure overload LVH, increases in NADPH oxidase activity parallel MAPK activation.13 More direct evidence for a role of NADPH oxidase in LVH comes from studies in gene‐modified mice lacking the Nox2 subunit of NADPH oxidase. It was found that experimental LVH induced by short‐term subpressor infusion of angiotensin II as well as the associated rises in atrial natriuretic factor expression (a molecular marker commonly associated with LVH) were inhibited in Nox2 knockout mice, indicating that angiotensin II‐induced hypertrophy is critically dependent on Nox2.16 In keeping with this, angiotensin II‐induced hypertrophy of isolated cardiomyocytes was also found to be dependent on Nox2.17
On the other hand, Nox2‐deficient mice subjected to aortic banding to induce pressure overload developed the same degree of LVH as wild‐type mice, suggesting that Nox2 is not central to development of hypertrophy under these conditions.18,19 However, it was suggested that the Nox4 oxidase might be an important mediator of LVH induced by pressure overload.18 Alternatively, a recent experimental study reported that ROS production by uncoupled nitric oxide synthase may contribute to the development of LVH during chronic pressure overload.20 Consistent with a role for ROS in pressure overload LVH, chronic treatment of mice with the antioxidant N‐acetyl‐cysteine attenuated LVH.18
ROS and contractile dysfunction
Contractile impairment is a central feature of CHF and has a multifactorial basis, involving changes in cardiomyocyte function as well as altered chamber structure and properties. In vitro studies have shown that myocyte contractile function may be impaired by increased ROS through several mechanisms, including disruption of calcium cycling, altered myofilament responsiveness to calcium, and deleterious effects on cellular metabolism and energetics.6,7,12
Experimental evidence supports an important contribution of increased oxidative stress to contractile dysfunction in CHF. In pacing‐induced heart failure, increased mitochondrial ROS generation was correlated with the degree of contractile dysfunction, and this relationship was suggested to be causal.7 In other studies, increased xanthine oxidase‐derived O2.− was suggested to contribute to left ventricle contractile impairment in CHF, as the xanthine oxidase inhibitor, allopurinol, improved function along with a decrease in myocardial oxygen consumption.8 These deleterious effects of xanthine oxidase may involve inactivation of nitric oxide as the nitric oxide molecule has been shown to reduce myocardial oxygen consumption and improve cardiac efficiency.
Nox2 NADPH oxidase‐derived ROS have been suggested to contribute to contractile dysfunction in pressure overload LVH. Grieve et al21 reported that Nox2 knockout mice with LVH had better preserved function than wild‐type mice with the same degree of LVH, suggesting that Nox2‐derived ROS contribute to contractile dysfunction in this setting. Similarly, another study implicated NADPH oxidase‐derived ROS in the genesis of left ventricle diastolic dysfunction in LVH, through the inactivation of endothelial‐derived nitric oxide.22
ROS and interstitial cardiac fibrosis
Excess interstitial fibrosis is an important detrimental aspect of chronic LVH and CHF. Oxidative stress is well known to be pro‐fibrotic in many organs and this seems to be true in the heart. Recent work suggests that Nox2 oxidase‐derived ROS are centrally involved in the development of interstitial cardiac fibrosis. In Nox2‐deficient mice subjected to angiotensin II infusion, interstitial fibrosis was virtually abolished compared with wild‐type mice.16 A similar inhibition of interstitial fibrosis was found in a model of aldosterone infusion, either in Nox2 knockout mice or in animals treated with an NADPH oxidase inhibitor, apocynin.23,24 Interstitial cardiac fibrosis was also inhibited in Nox2 knockout mice subjected to aortic banding.21 Multiple underlying mechanisms are likely to be involved in these Nox2‐dependent pro‐fibrotic effects, including increased expression of pro‐fibrotic growth factors and genes, increased activation of NF‐κB, activation of matrix metalloproteinases, and inflammatory cell infiltration. These data suggest that Nox2 oxidase may be an attractive target for therapies to prevent or treat fibrosis.
Adverse remodelling after myocardial infarction
Adverse remodelling of the left ventricle after initial recovery from myocardial infarction is the most common cause of CHF in the western world. Despite the benefits of treatments such as ACE inhibitors and β‐blockers, the condition remains an important problem. Growing evidence suggests an important role for increased oxidative stress in adverse left ventricular remodelling after myocardial infarction.1 An increase in oxidative stress after myocardial infarction is well recognised, and in experimental models it has been shown that various antioxidant approaches (eg, probucol, dimethylthiourea or genetic manipulation) can ameliorate the adverse remodelling. The beneficial effects of these experimental approaches extend to improved contractile function, reduced left ventricle dilatation and lower mortality. A significant factor for the detrimental effect of ROS in this setting is the activation of matrix metalloproteinases, which drive matrix turnover and promote left ventricle dilatation.
The increase in ROS may be driven by stimuli such as activation of the renin angiotensin system, cytokine activation, local inflammation and mechanical stimuli. As these stimuli activate NADPH oxidase, an involvement of this enzyme is plausible. Indeed, an increased cardiac expression of NADPH oxidase components has been reported after experimental myocardial infarction in an animal model and in myocardial samples from patients who died of acute myocardial infarction.25,26 More recently, preliminary studies in our laboratory have indicated that adverse left ventricle remodelling after myocardial infarction is significantly reduced in Nox2 knockout mice.27 On the other hand, another study reported that the xanthine oxidase inhibitor allopurinol significantly reduced adverse left ventricle remodelling after myocardial infarction in a mouse model.28
Other effects of ROS in CHF
Oxidative stress may be critical in the activation of apoptosis, which is thought to be an important contributor to the progression of CHF especially in its advanced stages. Increased ROS production is also an important underlying mechanism in the development of vascular endothelial dysfunction in CHF, which contributes to systemic vasoconstriction and increased cardiac loading. This generally involves a reduction in nitric oxide bioavailability and can be corrected acutely by administration of antioxidants such as vitamin C.29 The sources of ROS responsible for endothelial dysfunction may include xanthine oxidase, which has been implicated in human CHF,30 as well as NADPH oxidase.12,22
Treatments to target oxidative stress and detrimental redox signalling
The data discussed above strongly suggest important pathophysiological roles for increased oxidative stress in the genesis of several aspects of the phenotype of the failing heart. In experimental settings, many studies have shown beneficial effects of antioxidants (eg, vitamin C and vitamin E), especially in the short term. However, larger prospective randomised trials in humans looking at hard cardiovascular end‐points have been disappointing. For example, neither the Heart Outcomes Prevention Evaluation Study nor the Heart Protection Studies found any evidence for a beneficial effect of antioxidants.31,32
Does this mean that antioxidant approaches have no role in prevention or treatment in CHF? The data discussed in this article suggest that this would be a spurious conclusion. In fact, it is clear that the term oxidative stress covers a diverse array of complex biological actions ranging from highly specific redox signalling involving specialised enzymes to interactions with nitric oxide to more straightforward effects such as “damage” to cells, membranes and macromolecules. Therefore, it is hardly surprising that the use of non‐specific antioxidants (eg, vitamins) did not produce the desired results. Furthermore, these agents are relatively inefficient and have generally been used without any assessment of the target population for levels of oxidative stress. What may be needed are much more specific agents that can target defined ROS sources and deleterious redox‐dependent signalling pathways. It may also be necessary to do this in a more cell‐, tissue‐ and pathway‐specific manner at appropriate points during the disease process. Some of the complexities of enzymes such as the NADPH oxidase family offer the tantalising possibility that detrimental aspects of the phenotype of the failing heart (eg, fibrosis, dilatation and contractile dysfunction) could be specifically targeted in isolation from potentially beneficial components (eg, compensatory hypertrophy).
Meanwhile, the idea that specific targeting of certain ROS‐dependent pathways may be beneficial receives support from the effects of some successful drugs that are already in use. It is noteworthy that ACE inhibitors and angiotensin receptor blockers are highly effective inhibitors of angiotensin II‐dependent NADPH oxidase activation. Also, a major consequence of the use of statins is to inhibit the activation of small GTPases such as Rac, thereby affecting NADPH oxidase activity. Indeed, several experimental studies have indicated favourable effects of statins on both cardiac hypertrophy and remodelling after myocardial infarction, and preliminary studies in small numbers of patients with CHF have also been encouraging. A better understanding of the precise roles of oxidative stress and redox signalling pathways in different components of the process of heart failure may therefore provide the basis for devising new therapeutic strategies for this condition.
Acknowledgements
Studies in the authors' laboratory are supported by the British Heart Foundation (BHF).
Abbreviations
CHF - congestive heart failure
LVH - left ventricular hypertrophy
ROS - reactive oxygen species
Footnotes
Competing interests: None declared.
References
- 1.Giordano F J. Oxygen, oxidative stress, hypoxia, and heart failure. J Clin Invest 2005115500–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mallat Z, Philip I, Lebret M.et al Elevated levels of 8‐iso‐prostaglandin F2α in pericardial fluid of patients with heart failure: a potential role for in vivo oxidant stress in ventricular dilatation and progression to heart failure. Circulation 1998971536–1539. [DOI] [PubMed] [Google Scholar]
- 3.Finkel T. Signal transduction by reactive oxygen species in non‐phagocytic cells. J Leukoc Biol 199965337–340. [DOI] [PubMed] [Google Scholar]
- 4.Shah A M, Channon K C. Free radicals and redox signalling in cardiovascular disease (mini‐symposium). Heart 200490485–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li J M, Shah A M. Endothelial cell superoxide generation: regulation and relevance for cardiovascular pathophysiology. Am J Physiol 2004287R1014–R1030. [DOI] [PubMed] [Google Scholar]
- 6.Gao W D, Liu Y, Marban E. Selective effects of oxygen free radicals on excitation‐contraction coupling in ventricular muscle: implications for the mechanism of stunned myocardium. Circulation 1996942597–2604. [DOI] [PubMed] [Google Scholar]
- 7.Ide T, Tsutsui H, Hayashidani S.et al Mitochondrial DNA damage and dysfunction associated with oxidative stress in failing hearts after myocardial infarction. Circ Res 200188529–535. [DOI] [PubMed] [Google Scholar]
- 8.Berry C E, Hare J M. Xanthine oxidoreductase and cardiovascular disease: molecular mechanisms and pathophysiological implications. J Physiol 2004555589–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verhaar M C, Westerweel P E, van Zonneveld A J.et al Free radical production by dysfunctional eNOS. Heart 200490494–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dixon L J, Morgan D R, Hughes S M.et al Functional consequences of endothelial nitric oxide synthase uncoupling in congestive cardiac failure. Circulation 20031071725–1728. [DOI] [PubMed] [Google Scholar]
- 11.Lambeth J D. NOX enzymes and the biology of reactive oxygen. Nat Rev Immunol 20044181–189. [DOI] [PubMed] [Google Scholar]
- 12.Cave A C, Grieve D J, Johar S.et al NADPH oxidase‐derived reactive oxygen species in cardiac pathophysiology. Philos Trans R Soc 20053602327–2334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li J M, Gall N P, Grieve D J.et al Activation of NADPH oxidase during progression of cardiac hypertrophy to failure. Hypertension 200240477–484. [DOI] [PubMed] [Google Scholar]
- 14.Heymes C, Bendall J K, Ratajczak P.et al Increased myocardial NADPH oxidase activity in human heart failure. J Am Coll Cardiol 2003412164–2171. [DOI] [PubMed] [Google Scholar]
- 15.Maack C, Kartes T, Kilter H.et al Oxygen free radical release in human failing myocardium is associated with increased activity of Rac1‐GTPase and represents a target for statin treatment. Circulation 20031081567–1574. [DOI] [PubMed] [Google Scholar]
- 16.Bendall J K, Cave A C, Heymes C.et al Pivotal role of a gp91phox‐containing NADPH oxidase in angiotensin II‐induced cardiac hypertrophy in mice. Circulation 2002105293–296. [DOI] [PubMed] [Google Scholar]
- 17.Nakagami H, Takemoto M, Liao J K. NADPH oxidase‐derived superoxide anion mediates angiotensin II‐induced cardiac hypertrophy. J Mol Cell Cardiol 200335851–859. [DOI] [PubMed] [Google Scholar]
- 18.Byrne J A, Grieve D J, Bendall J K.et al Contrasting roles of NADPH oxidase isoforms in pressure‐overload versus angiotensin II‐induced cardiac hypertrophy. Circ Res 200393802–805. [DOI] [PubMed] [Google Scholar]
- 19.Maytin M, Siwik D A, Ito M.et al Pressure overload‐induced myocardial hypertrophy in mice does not require gp91phox. Circulation 20041091168–1171. [DOI] [PubMed] [Google Scholar]
- 20.Takimoto E, Champion H C, Li M.et al Oxidant stress from nitric oxide synthase‐3 uncoupling stimulates cardiac pathologic remodeling from chronic pressure load. J Clin Invest 20051151221–1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grieve D J, Byrne J A, Siva A.et al Involvement of the nicotinamide adenosine dinucleotide phosphate oxidase isoform Nox2 in cardiac contractile dysfunction occurring in response to pressure overload. J Am Coll Cardiol 200647817–826. [DOI] [PubMed] [Google Scholar]
- 22.MacCarthy P A, Grieve D J, Li J M.et al Impaired endothelial regulation of ventricular relaxation in cardiac hypertrophy: role of reactive oxygen species and NADPH oxidase. Circulation 20011042967–2974. [DOI] [PubMed] [Google Scholar]
- 23.Johar S, Cave A C, Narayanapanicker A.et al Aldosterone mediates angiotensin II‐induced interstitial cardiac fibrosis via a Nox2‐containing NADPH oxidase. FASEB J 2006201546–1548. [DOI] [PubMed] [Google Scholar]
- 24.Park Y M, Park M Y, Suh Y L.et al NADH oxidase inhibitor prevents blood pressure elevation and cardiovascular hypertrophy in aldosterone‐infused rats. Biochem Biophys Res Commun 2004313812–817. [DOI] [PubMed] [Google Scholar]
- 25.Fukui T, Yoshiyama M, Hanatani A.et al Expression of p22‐phox and gp91‐phox, essential components of NADPH oxidase, increases after myocardial infarction. Biochem Biophys Res Commun 20012811200–1206. [DOI] [PubMed] [Google Scholar]
- 26.Krijnen P A J, Meischl C, Hack C E.et al Increased Nox2 expression in human cardiomyocytes after acute myocardial infarction. J Clin Pathol 200356194–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Looi Y H, Grieve D J, Siva A.et al A Nox2‐containing NADPH oxidase contributes to cardiac remodeling after myocardial infarction [abstract]. Circulation 2005112(Suppl)11–18. [Google Scholar]
- 28.Engberding N, Spiekermann S, Schaefer A.et al Allopurinol attenuates left ventricular remodeling and dysfunction after experimental myocardial infarction: a new action for an old drug? Circulation 20041102175–2179. [DOI] [PubMed] [Google Scholar]
- 29.Hornig B, Arakawa N, Kohler C.et al Vitamin C improves endothelial function of conduit arteries in patients with chronic heart failure. Circulation 199897363–368. [DOI] [PubMed] [Google Scholar]
- 30.Farquharson C A J, Butler R, Hill A.et al Allopurinol improves endothelial dysfunction in chronic heart failure. Circulation 2002106221–226. [DOI] [PubMed] [Google Scholar]
- 31.The Heart Outcomes Prevention Evaluation Study Investigators Vitamin E supplementation and cardiovascular events in high‐risk patients. N Engl J Med 2000342154–160. [DOI] [PubMed] [Google Scholar]
- 32.Heart Protection Study Collaborative G. MRC/BHF Heart Protection Study of antioxidant vitamin supplementation in 20 536 high‐risk individuals: a randomised placebo‐controlled trial. Lancet 200236023–33. [DOI] [PubMed] [Google Scholar]