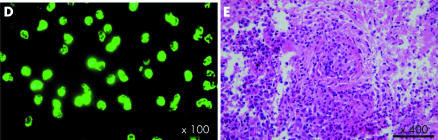
A 61‐year‐old man presented with a history of right‐sided facial palsy and haemoptysis over the previous two months. Upon admission, chest radiography showed ill defined patchy infiltrates in both lung fields. An initial ECG revealed third degree atrioventricular (AV) block and escape beats (35 beats/min) with right bundle branch block (RBBB, panel A). On the third day, the patient complained of increasing dyspnoea, and an ECG showed atrial fibrillation (AF) with complete AV block (panel B). At that time, the QRS morphology of the escape beats (32 beats/min) changed to a left bundle branch block pattern. Brain computed tomography (CT) revealed thickening of the mucosa in the left ethmoid sinus without any pathologic findings in the brain itself. A test for cytoplasmic antineutrophil cytoplasmic antibody (c‐ANCA) of anti‐proteinase‐3 was positive (panel D). A nasal mucosal biopsy revealed necrotising granulomatous vasculitis (panel E), leading to the diagnosis of Wegener's granulomatosis.
After establishing the diagnosis, pulse therapy with intravenous methylprednisone and cyclophosphamide, followed by high‐dose oral prednisolone, was begun. Subsequently, the patient's condition improved remarkably, and he recovered from the heart block and AF over the next five days. However, the first‐degree AV block (PR interval 320 ms) with RBBB remained (panel C) when seen one month after initiation of treatment.
When a patient presents with progressive cardiac conduction system disturbances combined with systemic symptoms, small vessel vasculitis including Wegener's granulomatosis should be considered in the differential diagnosis. Correct and early diagnosis may prove to be life saving, and it may obviate the need for pacemaker insertion.