Abstract
Background
Neutrophil gelatinase‐associated lipocalin (NGAL) is a member of the lipocalin family. Recently, an elevated NGAL expression was reported in several types of cancers. However, the characteristics of NGAL expression in oesophageal squamous cell carcinoma (ESCC) are still unknown.
Aim
To demonstrate the role of NGAL in ESCC.
Methods
NGAL expression in 81 paraffin sections, including ESCC, normal mucosa, simple hyperplasia and dysplasia, and in 73 fresh specimens of ESCC was analysed by immunohistochemistry, western blot and gelatin zymography.
Results
On immunohistochemical study, ESCC showed a diverse staining pattern for NGAL. However, only a weak positive signal was present within a restricted cytoplasmic area in the normal oesophageal epithelium. In dysplasia, altered NGAL expression could also be observed. On western blot study, NGAL expression level was found to be significantly higher in ESCC than in normal mucosa (p = 0.030), and to be positively correlated with cell differentiation. However, no significant association was observed between NGAL expression and cell proliferation. In addition, the enzymic activity of the NGAL/matrix metalloproteinase 9 complex was much higher in ESCC than in normal mucosa, and was significantly correlated with the depth of tumour invasion in zymography analysis (p = 0.006).
Conclusions
The findings suggest that NGAL is involved in the differentiation pathway and invasive progression of ESCC.
Oesophageal squamous cell carcinoma (ESCC) makes up >90% of all oesophageal tumours in the Far East.1 In China, ESCC is the fourth most common malignancy, with a relatively higher mortality rate. It is hard to diagnose ESCC at the early stage, and advanced ESCC frequently presents with unresectable or metastatic cancers.2 This is one of the important reasons for the poor prognosis of ESCC. Hence, the early identification of people at a high risk of developing ESCC offers the best chance for cure.3 Our previous work has identified that neutrophil gelatinase‐associated lipocalin (NGAL), also known as lipocalin 2, was overexpressed in the progression of malignant transformation from human immortalised oesophageal epithelial cell line SHEE to oesophageal carcinoma cell line SHEEC.4,5 This suggested that NGAL might be involved in the carcinogenesis of ESCC.
NGAL, a member of the lipocalin family, was originally found as a protein stored in specific granules of the human neutrophil.6 Besides the neutrophil, NGAL is expressed in most tissues normally exposed to micro‐organisms, and induced in epithelial cells during inflammation.7,8 NGAL binds bacterial siderophores, preventing bacteria from retrieving iron from this source.9,10 Also, NGAL may be important in delivering iron to cells during the formation of the tubular epithelial cells of the primordial kidney.11 Furthermore, NGAL is suggested as an acute‐phase protein that can protect against acute ischaemic renal injury, and is implicated in apoptosis as a survival factor.12,13 Another study indicates that NGAL is involved in extracellular matrix remodelling and is capable of protecting matrix metalloproteinase 9 (MMP‐9) from degradation by interacting with this protein.14,15 Elevated NGAL expression is also observed in human cancers such as colorectal,7 breast,16 pancreatic17 and ovarian cancers.18 However, the characteristics of NGAL expression in ESCC are still unknown. To demonstrate the role of NGAL in the transformation and development of ESCC, in the present study, NGAL expression, activity of the NGAL/MMP‐9 complex, and their correlations with cell proliferation and clinicopathological features in ESCC were examined.
Materials and methods
Patients and surgical specimens
Eighty‐one paraffin sections, including 18 cases of normal mucosa, 6 cases of simple hyperplasia, 29 cases of dysplasia and 30 cases of ESCC, were acquired from the Pathology Department of the Medical College of Shantou University (Shantou, People's Republic of China), collected from 2001 to 2003.
Tumour and corresponding normal tissues were obtained for western blot from 73 patients with primary ESCC who underwent surgery in the First Affiliated Hospital of Shantou University from 2003 to 2005. A small portion from each resected tissue sample was immediately frozen in liquid nitrogen and stored at −70°C. None of the patients received radiotherapy or chemotherapy before surgery. Information on gender, age, stage of disease and histopathological factors were retrieved from the medical records. Patients' data are summarised in table 1.
Table 1 Patients and tumour characteristics.
| Total (n = 73) | n |
|---|---|
| Mean age, years (range) | 57 (37–74) |
| <57 | 37 |
| >57 | 36 |
| Gender | |
| Male | 62 |
| Female | 11 |
| Primary tumour | |
| T1/T2 | 19 |
| T3/T4 | 54 |
| Regional lymph node | |
| No | 36 |
| N1 | 37 |
| Distant metastasis | |
| M0 | 69 |
| M1 | 4 |
| Stage | |
| I/IIA/IIB | 33 |
| III/IV | 40 |
| Histopathology | |
| Well differentiated (G1) | 14 |
| Moderately differentiated (G2) | 46 |
| Poorly differentiated (G3) | 13 |
All of the cases were classified according to the fifth edition of the tumour–node–metastasis classification of the International Union against Cancer. Evaluation of tumour differentiation was based on histological criteria of the guidelines of the WHO Pathological Classification of Tumors.19
The study was approved by the ethical committee of the First Affiliated Hospital of Shantou University, and written informed consent was obtained from all surgical patients to use resected samples for research.
Recombinant human NGAL protein production and isolation
Recombinant human NGAL protein (rNGAL) for use as a standard positive control for western blot was produced in a bacterial expression system. The plasmid pGEX‐NGAL was kindly provided by Dr Cowland.20 The coding region of NGAL, without its leader sequence and stop codon, was subcloned into the pET‐DsbA2.0 expression vector system, expressed as a fusion protein with His‐tag in bacteria, affinity purified by adsorption to Ni‐chelating sepharose (Pharmacia) and released by cleaving the adsorbed fusion protein with human thrombin. Protein measurement was performed using the Bradford method.
Immunohistochemical staining
Briefly, each tissue section was deparaffinated, rehydrated and then incubated with fresh 3% hydrogen peroxide for 10 min. After rinsing with phosphate‐buffered saline (PBS), antigen retrieval from the tissue was carried out by autoclaving in 0.01 M citrate buffer (pH 6.0) at 120°C for 3 min. Next, sections were incubated with 10% normal goat serum in PBS for 15 min at room temperature. After rinsing with PBS, slides were incubated overnight at 4°C with rat anti‐human NGAL monoclonal antibody (1:50 dilution in PBS, R&D Systems, Minneapolis, Minnesota, USA). After rinsing with PBS, tissue sections were incubated for 20 min at room temperature with horseradish peroxidase‐linked goat anti‐rat antibody (Jackson ImmunoResearch, Newmarket, UK). Subsequently, they were stained with 0.003% 3,3‐diaminobenzide tetrahydrochloride and 0.005% hydrogen peroxide in 0.05 M Tris‐HCl (pH 7.2), counterstained with Mayer's haematoxylin, dehydrated and mounted.
Negative controls were prepared by substituting PBS for primary antibody. An oesophagitis section, shown previously to have immunoreactivity of infiltrative neutrophils, was used as a positive control to confirm the immunoreactivity in each series of experiments.
NGAL‐positive samples were defined as those showing brown signals in the cytoplasm. When >5% of the cells in a given specimen were positively stained, we defined it as a positive case. All sections were evaluated independently by two investigators without any prior knowledge of patients' clinical information. When the opinions of the two evaluators were different, agreement was reached by careful discussion.
Western blot analysis
Tissues were lysed in a sample buffer (50 mM Tris‐HCl, pH 8.0, 150 mM NaCl, 1% Triton X‐100, 100 μg/ml phenylmethylsulphonyl fluoride) on ice for 30 min. Then the lysates were centrifuged for 5 min (12 000 r.p.m., 4°C). The protein concentration was estimated by the Bradford method. An equal amount of tissue lysates (100 μg) was electrophoresed on 12% polyacrylamide gel and transferred onto polyvinylidene difluoride membranes (Millipore, Bedford, Massachusetts, USA ). The membranes were then blocked with 5% skim milk‐phosphate‐buffered saline with bovine serum albumin for 1 h and incubated at room temperature for 1 h with the rat anti‐human NGAL monoclonal antibody (R&D Systems). The membrane was subsequently incubated at room temperature for 1 h with horseradish peroxidase‐linked goat anti‐rat immunoglobulin G (Jackson ImmunoResearch) and analysed using Western Blotting Luminol Reagent (Santa Cruz Biotechnology, San Diego, California, USA). Image acquisition and quantitative analysis were carried out using the FluorChem 8900 image analysis system (Alpha Innotech, St San Leandro, California, USA). To evaluate the approximate proliferation level of the cells, the proliferating cell nuclear antigen (PCNA) level was measured with anti‐PCNA monoclonal antibody (DAKO Biot, Glostrup, Denmark). To verify the relative amounts of protein in each lane, the β‐actin level as an internal control was measured with anti‐β‐actin monoclonal antibody (Sigma). The protein expression levels in tumour and the corresponding normal tissue were calculated from the signal intensity. The NGAL expression level was evaluated by comparing the band densities of samples with recombinant NGAL protein controls. The level of PCNA expression was finally evaluated by the ratio of their presence in the tumour to their presence in the corresponding normal epithelial tissue (T/N ratio).
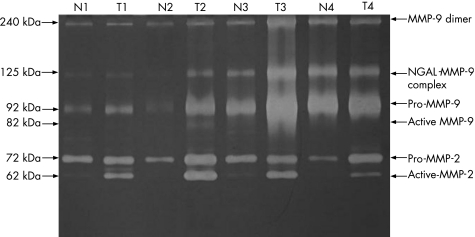
Gelatin zymography
Forty‐eight randomly selected cases of tumour and corresponding normal tissues were analysed by gelatin zymography. Gelatin zymography was performed as described previously, with some modifications.21,22 Briefly, tissue extracts were subjected to SDS‐PAGE through 10% polyacrylamide gels containing 0.1% gelatin under non‐denaturing conditions. Gels were rinsed in washing buffer (50 mM Tris‐HCl, pH 7.5, 2.5% Triton X‐100) at room temperature for 1 h and incubated overnight at 37°C in incubation buffer (50 mM Tris‐HCl, pH 7.5, 10 mM CaCl2 and 150 mM NaCl). Gels were fixed and stained with 0.1% Coomassie blue R250. After destaining, gelatinolytic activity was visualised as a clear band against a blue background of stained gelatin. MMP‐9 and the NGAL/MMP‐9 complex were detected by the clear band appearing at 92 and at 125 kDa, respectively. Gelatinolytic signals were quantified by densitometry using the FluorChem 8900 image analysis system. Matrix metalloproteinase activity was finally evaluated by the ratio of their presence in the tumour to their presence in the corresponding normal tissue (T/N ratio).
Statistical evaluations
Statistical analyses of the data were performed with SPSS V10.0 software. The statistical association between protein expression/matrix metalloproteinases activity and various clinicopathological parameters was analysed by independent sample t test and paired sample t test. p<0.05 was considered as significant.
Results
Immunostaining for NGAL in normal epithelium, simple hyperplasia and dysplasia of oesophagus
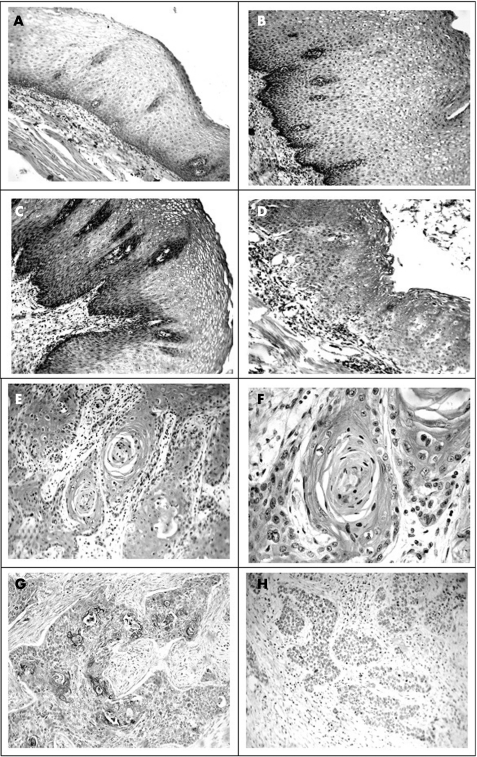
In normal epithelium (18 cases) and simple hyperplasia (6 cases) of oesophagus, weak immunostaining for NGAL only was located in the restricted intracellular area close to the cytomembrane almost throughout the full thickness of the epithelium (fig 1A and B). Nevertheless, the basal layer cells were always negative for NGAL. In mild dysplasia (fig 1C), epithelial cells of parabasal layers presented weak to moderate whole‐cytoplasmic immunostaining for NGAL (10/13, the numerator represents the whole‐cytoplasmic staining cases and the denominator represents the total sections examined). Moreover, more intense whole‐cytoplasmic immunostaining for NGAL was apparent in the progression from mild (10/13) to moderate (11/12, fig 1D) to severe dysplasia (4/4). However, the NGAL‐positive cells were reduced and distributed in more superficial layers of the epithelium with progression of dysplasia.
Figure 1 Immunohistochemical staining of neutrophil gelatinase‐associated lipocalin (NGAL) expression in normal epithelium, simple hyperplasia, dysplasia of oesophagus and tissue from oesophageal squamous cell carcinoma (ESCC). In normal oesophageal epithelium (A, ×200) and simple hyperplasia (B, ×200), weak immunostaining for NGAL was only located in a restricted area close to the cytomembrane almost throughout the full thickness of epithelium except the basal layer. In mild dysplasia (C, ×200), epithelial cells of suprabasal layers presented weak to moderate whole‐cytoplasmic immunostaining for NGAL. While in the progression from mild to moderate (D, ×200) to severe dysplasia, more intense whole‐cytoplasmic immunostaining for NGAL was apparent. However, the NGAL‐positive cells were reduced and distributed in a more superficial area of the epithelium in this progression. In well‐differentiated ESCC (E, ×200; F, ×400), intense immunoreactivity for NGAL was presented in the cytoplasm of most of the cancer cells, and the most intense immunostaining for NGAL could be seen in the area around the horny pearl. However, the periphery of the cancer nest was always negative for NGAL. In 56% (10/18) of the moderately differentiated ESCC (G, ×200), only a small subset of tumour cells was apparent with very intense immunostaining for NGAL. In the poorly differentiated ESCC (H, ×200), almost all the cancer cells were negative for NGAL.
NGAL expression in ESCC
In the immunohistochemical study, weak to intense whole‐cytoplasmic immunostaining was present in the cancer cells. ESCC showed a diverse staining pattern that varied from strong homogeneous positivity in most malignant cells to very focal staining in a small subset of tumour cells (fig 1E–G). Only 23% (7/30) cases of ESCC were negative for NGAL (fig 1H).
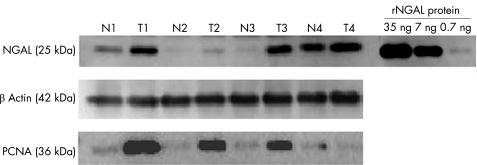
In agreement with the immunohistochemical study, a wide range of NGAL expression was observed by western blot. By comparing the band densities of tumour samples with those of recombinant NGAL protein controls, it was estimated that between 0 and 4.16 ng of NGAL protein was present per 100 μg of total protein loaded (fig 2). According to the western blot study, NGAL expression level was significantly higher in ESCC (mean (SD), 0.874 (1.002) ng) than in the normal mucosa (0.549 (0.918) ng; p = 0.030; table 2). NGAL expression was increased in 59% (43/73) of ESCC cases in comparison with the corresponding normal epithelium.
Figure 2 Western blot analysis of neutrophil gelatinase‐associated lipocalin (NGAL) and proliferating cell nuclear antigen (PCNA) expression in four oesophageal carcinoma tissues (T) and the corresponding normal oesophageal tissues (N). The molecular weights (kDa) of the immunoreactivity are shown on the left. Human recombinant NGAL (rNGAL) protein served as a standard positive control of NGAL expression, and the expression of β‐actin was simultaneously tested as an internal control for an equal loading.
Table 2 Relationship between clinicopathological features and neutrophil gelatinase‐associated lipocalin expression level in oesophageal squamous cell carcinoma by western blot.
| Parameters | NGAL expression level (ng/100 μg, mean (SD)) | p Value |
|---|---|---|
| Mean age, years (range) | ||
| <57 | 0.990 (1.036) (n = 37) | 0.364 |
| >57 | 0.775 (0.973) (n = 36) | |
| Gender | ||
| Male | 0.931 (1.039) (n = 62) | 0.345 |
| Female | 0.618 (0.765) (n = 11) | |
| Primary tumour | ||
| T1/T2 | 0.571 (0.669) (n = 19) | 0.126 |
| T3/T4 | 0.981 (1.081) (n = 54) | |
| Regional lymph node | ||
| N0 | 0.938 (1.806) (n = 36) | 0.593 |
| N1 | 0.812 (0.930) (n = 37) | |
| Distant metastasis | ||
| M0 | 0.906 (1.013) (n = 69) | 0.436 |
| M1 | 0.500 (0.867) (n = 4) | |
| Stage | ||
| I/IIA/IIB | 0.793 (0.955) (n = 33) | 0.486 |
| III/IV | 0.959 (1.049) (n = 40) | |
| Histopathology | ||
| Normal tissue | 0.549 (0.918) (n = 73) | 0.030 |
| ESCC tissue | 0.874 (1.002) (n = 73) | |
| Well differentiated (G1) | 1.504 (1.209) (n = 14) | p1/2 = 0.017 |
| Moderately differentiated (G2) | 0.751 (0.934) (n = 46) | p2/3 = 0.677 |
| Poorly differentiated (G3) | 0.632 (0.766) (n = 13) | p1/3 = 0.036 |
ESCC, oesophageal squamous cell carcinoma; NGAL, neutrophil gelatinase‐associated lipocalin.
Correlation between NGAL expression level and the clinicopathological features in ESCC
In immunohistochemical study, the expression of NGAL was obviously associated with the differentiation of ESCC. All the well‐differentiated ESCC cases (seven cases) showed strong homogeneous positivity in most cancer cells, and the most intense immunostaining for NGAL could be seen in the cells around the horny pearl (fig 1E and F). The moderately differentiated group (n = 18) showed very focal staining in a small subset of tumour cells in 10 cases (fig 1G), strong homogeneous positivity in 6 cases and negative staining in 2 cases. Finally, five cases of poorly differentiated ESCC were all negative for NGAL (fig 1H).
In western blot study, a significant correlation was also observed between NGAL expression level and degree of cancer cell differentiation. The more poor the ESCC differentiation was, the lower the NGAL expression became (p = 0.017; table 2). This result was in agreement with the finding in the immunohistochemical study.
The correlation between NGAL expression and other clinicopathological factors, such as pathological tumour–node–metastasis classification and stage grouping, was simultaneously investigated. However, there was no significant association between NGAL expression level and these factors (table 2).
Correlation between the expression level of NGAL and PCNA in ESCC by western blot
We used western blot to examine the expression level of PCNA in 48 cases of ESCC (fig 2). Overexpression of PCNA was observed in 87.5% (42/48) of tumour tissue compared with the corresponding normal epithelium. No significant difference could be observed between the PCNA expression level in the upregulated NGAL expression group and that in the low NGAL expression group (p = 0.400; table 3).
Table 3 Relationship between expression level of neutrophil gelatinase‐associated lipocalin and proliferating cell nuclear antigen in oesophageal squamous cell carcinoma by western blot.
| Group | PCNA expression level (T/N ratio, mean (SD)) | p Value |
|---|---|---|
| NGAL | 0.400 | |
| >0.55 ng | 8.27 (8.13) (n = 25) | |
| <0.55 ng | 10.58 (10.62) (n = 23) |
NGAL, neutrophil gelatinase‐associated lipocalin; PCNA, proliferating cell nuclear antigen; T/N ratio, ratio of tumour/corresponding normal tissue.
Correlation between the activity of NGAL/MMP‐9 complex and the clinicopathological features in ESCC by zymography analysis
We used gelatin zymography to examine the activity of the NGAL/MMP‐9 complex in 48 cases of ESCC (fig 3). The activity of the NGAL/MMP‐9 complex in ESCC was 6.969 (8.548) (mean (SD)) times that in the normal epithelium (n = 48, p<0.0001; table 4; fig 3). In total, 92% (44/48) cases of ESCC had higher activity of NGAL/MMP‐9 complex than that in corresponding normal mucosa. A significant correlation could be seen between the activity of NGAL/MMP‐9 complex and the depth of tumour invasion (T, primary tumour). The deeper the tumour invasion, the higher the enzymatic activity (p = 0.006; table 4). However, there was no significant association between the activity of the NGAL/MMP‐9 complex and other factors in the present study.
Figure 3 Gelatin zymography analysis of matrix metalloproteinase activity in four oesophageal carcinoma tissues (T) and the corresponding normal oesophageal tissues (N). The molecular weights (kDa) of the matrix metalloproteinase 9 (MMP‐9) dimer, NGAL/MMP‐9 complex, pro‐MMP‐9, active‐MMP‐9, pro‐MMP‐2 and active‐MMP‐2 are shown on the left. NGAL, neutrophil gelatinase‐associated lipocalin.
Table 4 Relationship between clinicopathological features and activity of neutrophil gelatinase‐associated lipocalin/matrix metalloproteinase 9 complex in oesophageal squamous carcinoma by zymography.
| Parameters | Complex activity level (T/N ratio, mean (SD)) | p Value |
|---|---|---|
| Mean age, years (range) | ||
| <58 | 5.316 (6.735) (n = 22) | 0.222 |
| >58 | 8.367 (9.739) (n = 26) | |
| Gender | ||
| Male | 6.563 (8.076) (n = 39) | 0.500 |
| Female | 8.724 (10.734) (n = 9) | |
| Primary tumour | ||
| T1/T2 | 3.007 (2.273) (n = 9) | 0.006 |
| T3/T4 | 7.883 (9.199) (n = 39) | |
| Regional lymph node | ||
| N0 | 6.222 (7.581) (n = 21) | 0.599 |
| N1 | 7.549 (9.332) (n = 27) | |
| Distant metastasis | ||
| M0 | 7.112 (8.683) (n = 46) | 0.582 |
| M1 | 3.665 (4.320) (n = 2) | |
| Stage | ||
| I/IIA/IIB | 6.290 (7.949) (n = 19) | 0.661 |
| III/IV | 7.412 (9.029) (n = 29) | |
| Histopathology | ||
| Well differentiated (G1) | 9.531 (8.825) (n = 13) | p1/2 = 0.181 |
| Moderately differentiated (G2) | 5.852 (7.840) (n = 30) | p2/3 = 0.780 |
| Poorly differentiated (G3) | 7.0040 (6.193) (n = 5) | p1/3 = 0.630 |
T/N ratio, ratio of tumour/corresponding normal tissue.
Discussion
The expression of NGAL has been demonstrated in several types of cancers, such as carcinoma of colon, lung, pancreas and breast.7,8,16,17 In the present study, a broad range of NGAL expression in ESCC was observed in immunohistochemistal study and western blot. NGAL expression was higher in 59% (43/73) of ESCC than in the corresponding normal oesophageal epithelium. Consistent with our study, Steven et al16 reported that 39% (11/28) of breast carcinoma were positive for NGAL with a diverse staining pattern, and that 250 cases of breast carcinoma showed a wide range of NGAL expression, by western blot. Moreover, altered distribution of NGAL expression was evident in ESCC. In the normal oesophageal epithelium, only weak NGAL expression was identified in the restricted intracellular area close to the cytomembrane, while in NGAL‐positive ESCC cells, strong immunostaining for NGAL with an obvious whole‐cytoplasmic staining pattern was demonstrated. These results suggested that not only the upregulation but also the altered subcellular distribution of NGAL were involved in ESCC carcinogenesis.
In our study, NGAL expression was positively associated with the degree of differentiation of ESCC, both in immunohistochemisty and in western blot analysis. All the well‐differentiated ESCC cases showed strong positivity for NGAL in most cancer cells (fig 1B), whereas in poorly differentiated ESCC, almost all the cancer cells were negative for NGAL (fig 1D). Mallbris et al23 reported that a strong induction of NGAL was seen in a variety of skin disorders characterised by dysregulated epithelial differentiation. In ESCC, loss of terminal differentiation was one of the characteristics of cancer cells even in the well‐differentiated cases, and the way in which cancer cells were differentiated was quite different from the normal non‐keratinised squamous epithelium.24 As only weak NGAL expression was present in the normal oesophageal epithelium, upregulation of NGAL with altered subcellular distribution in ESCC might also imply the dysregulated differentiated properties of cancer cells.
Human ESCC typically develops through a sequence of histopathological changes. In the present study, we found that in the progression from mild to moderate to severe dysplasia of the oesophageal epithelium, the whole‐cytoplasmic immunostaining for NGAL was decreased in the quantity of labelled cells and increased in the intensity of immunostaining. However, the normal oesophageal epithelium never showed whole‐cytoplasmic labelling for NGAL. These results indicated that altered expression of NGAL occurred in the early stages of ESCC transformation. Genetic alterations could frequently be detected in the basal layer cells of precancerous lesions of ESCC, and the well‐differentiated cells in the superficial layers were all differentiated from the basal layer cells.24,25 Hence, the changes in NGAL expression in the superficial layers of the dysplastic epithelium correlated not only with the well‐differentiated status but also with the dysregulated differentiated property of these cells. Therefore, this result was in good agreement with our findings in ESCC.
Nevertheless, in accordance with previous findings in colorectal and breast cancer, no significant correlation was observed between expression level of NGAL and several prognostic factors, such as lymph node metastasis and tumour stage in our study.
In immunohistochemical study, we found immunostaining for NGAL was mainly distributed in the superficial layers of the oesophageal epithelium and in the inner side of the cancer nest. However, the basal layer of the oesophageal epithelium and the peripheral area of the cancer nest, which usually contain the cells with high proliferative status, were always negative for NGAL. Furthermore, we also found that NGAL expression level was not significantly correlated with cancer cell proliferative status, by examining the PCNA level in the same specimens. These results validated our previous finding that the proliferative status of the ESCC cells did not change markedly after the NGAL expression level of ESCC cells was altered by the antisense blocking RNA technique.5
NGAL was originally purified from human neutrophils and existed in monomeric and homo‐ and heterodimeric forms, the latter as a dimer with human neutrophil gelatinase B (pro‐MMP‐9).6 Fernandez et al26 found that the NGAL/MMP‐9 complex was detected in 19 of 22 (86.36%) of the urine samples from patients with breast cancer but not in those from healthy controls. In the present study, we found that 92% (44/48) of ESCC tissues had a higher enzymatic activity of NGAL/MMP‐9 complex than that in the corresponding normal mucosa, and that the activity of the NGAL/MMP‐9 complex correlated significantly with the depth of tumour invasion (p = 0.006; table 4), by using gelatin zymography. Although the expression level of NGAL was not significantly associated with the depth of tumour invasion in western blot analysis, we could still observe that the average expression of NGAL in the T3/T4 group was higher than that in the T1/T2 group (table 2). Note that non‐reducing electrophoresis was used in gelatin zymography analysis; the results of gelatin zymography may more truly reflect the natural forms of NGAL and MMP‐9 in vivo.
Matrix metalloproteinases were known to play an important role in extracellular matrix remodelling during the process of tumour invasion. Recent reports have found that the formation of the NGAL/MMP‐9 complex could protect MMP‐9 from autodegradation, and that NGAL‐overexpressing MCF‐7 cancer cells exhibited increased expression levels of MMP‐9.14,27 On the other hand, there was a contradictory report in colon cancer cell lines.28 As for ESCC, our previous work has demonstrated that downregulation of NGAL expression in ESCC cells could significantly suppress MMP‐9 activity and the invasion of these cells in nude mice.5 Combining the findings of our present study, it can be concluded that NGAL in complex with MMP‐9 might play an important role in the invasive progression of ESCC.
In summary, NGAL was upregulated in ESCC in a heterogeneous pattern, and the expression level of NGAL correlated positively with cell differentiation. In addition, the alteration of NGAL expression occurred early in the precancerous lesion. Furthermore, the enzymatic activity of the NGAL/MMP‐9 complex was much higher in ESCC than in normal mucosa and may play an important role in tumour invasion. Thus, our findings suggest that NGAL is involved in the transformation and progression of ESCC.
Take‐home messages
Immunohistochemical study revealed that oesophageal squamous cell carcinoma (ESCC) showed a diverse staining pattern for neutrophil gelatinase‐associated lipocalin (NGAL).
Western blot study showed that NGAL expression level was significantly higher in ESCC than in normal mucosa and that it positively correlated with cell differentiation. No significant association was observed between NGAL expression and cell proliferation.
The enzymic activity of the NGAL/matrix metalloproteinase 9 complex was much higher in ESCC than in normal mucosa, and significantly correlated with the depth of tumour invasion in zymography analysis.
Abbreviations
ESCC - oesophageal squamous cell carcinoma
MMP‐9 - matrix metalloproteinase 9
NGAL - neutrophil gelatinase‐associated lipocalin
PBS - phosphate‐buffered saline
PCNA - proliferating cell nuclear antigen
Footnotes
Funding: This work was supported by grants from the National Natural Science Foundation of China (No. 39900069, No. 30170428, No. 30370641, No. 30570849); Specialised Research Fund for the Doctoral Program of Higher Education of China (No. 20050560002, No. 20050560003); Guangdong Scientific Fund Key Items (No. 37788, No. 05104541); and Natural Science Foundation of Guangdong Province (No. 010431).
Competing interests: None.
This study was approved by the ethical committee of the First Affiliated Hospital of Shantou University (Shantou City, Guangdong Province, People's Republic of China), and written informed consent was obtained from all patients undergoing surgery to use resected samples for research.
References
- 1.Koshy M, Esiashvilli N, Landry J C.et al Multiple management modalities in esophageal cancer: epidemiology, presentation and progression, work‐up, and surgical approaches. Oncologist 20049137–146. [DOI] [PubMed] [Google Scholar]
- 2.Enzinger P C, Mayer R J. Esophageal cancer. N Engl J Med 20033492241–2252. [DOI] [PubMed] [Google Scholar]
- 3.Brooks‐Brunn J A. Esophageal cancer: an overview. Medsurg Nurs 20009248–254. [PubMed] [Google Scholar]
- 4.Shen Z, Cen S, Shen J.et al Study of immortalization and malignant transformation of human embryonic esophageal epithelial cells induced by HPV18 E6E7. J Cancer Res Clin Oncol 2000126589–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li E M, Xu L Y, Cai W J.et al Functions of neutrophil gelatinase‐associated lipocalin in the esophageal carcinoma cell line SHEEC. Sheng Wu Hua Xue Yu Sheng Wu Wu Li Xue Bao (Shanghai) 200335247–254. [PubMed] [Google Scholar]
- 6.Kjeldsen L, Johnsen A H, Sengelov H.et al Isolation and primary structure of NGAL, a novel protein associated with human neutrophil gelatinase. J Biol Chem 199326810425–10432. [PubMed] [Google Scholar]
- 7.Nielsen B S, Borregaard N, Bundgaard J R.et al Induction of NGAL synthesis in epithelial cells of human colorectal neoplasia and inflammatory bowel diseases. Gut 199638414–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Friedl A, Stoesz S P, Buckley P.et al Neutrophil gelatinase‐associated lipocalin in normal and neoplastic human tissues. Cell type‐specific pattern of expression. Histochem J 199931433–441. [DOI] [PubMed] [Google Scholar]
- 9.Goetz D H, Holmes M A, Borregaard N.et al The neutrophil lipocalin NGAL is a bacteriostatic agent that interferes with siderophore‐mediated iron acquisition. Mol Cell 2002101033–1043. [DOI] [PubMed] [Google Scholar]
- 10.Flo T H, Smith K D, Sato S.et al Lipocalin 2 mediates an innate immune response to bacterial infection by sequestrating iron. Nature 2004432917–921. [DOI] [PubMed] [Google Scholar]
- 11.Gwira J A, Wei F, Ishibe S.et al Expression of neutrophil gelatinase‐associated lipocalin regulates epithelial morphogenesis in vitro. J Biol Chem 20052807875–7882. [DOI] [PubMed] [Google Scholar]
- 12.Mori K, Lee H T, Rapoport D.et al Endocytic delivery of lipocalin–siderophore–iron complex rescues the kidney from ischemia–reperfusion injury. J Clin Invest 2005115610–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tong Z, Wu X, Ovcharenko D.et al Neutrophil gelatinase‐associated lipocalin as a survival factor. Biochem J 2005391(Part 2)441–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yan L, Borregaard N, Kjeldsen L.et al The high molecular weight urinary matrix metalloproteinase (MMP) activity is a complex of gelatinase B/MMP‐9 and neutrophil gelatinase‐associated lipocalin (NGAL). Modulation of MMP‐9 activity by NGAL. J Biol Chem 200127637258–37265. [DOI] [PubMed] [Google Scholar]
- 15.Sousa M M, do Amaral J B, Guimaraes A.et al Up‐regulation of the extracellular matrix remodeling genes, biglycan, neutrophil gelatinase‐associated lipocalin, and matrix metalloproteinase‐9 in familial amyloid polyneuropathy. FASEB J 200519124–126. [DOI] [PubMed] [Google Scholar]
- 16.Stoesz S P, Friedl A, Haag J D.et al Heterogeneous expression of the lipocalin NGAL in primary breast cancers. Int J Cancer 199879565–572. [DOI] [PubMed] [Google Scholar]
- 17.Furutani M, Arii S, Mizumoto M.et al Identification of a neutrophil gelatinase‐associated lipocalin mRNA in human pancreatic cancers using a modified signal sequence trap method. Cancer Lett 1998122209–214. [DOI] [PubMed] [Google Scholar]
- 18.Bartsch S, Tschesche H. Cloning and expression of human neutrophil lipocalin cDNA derived from bone marrow and ovarian cancer cells. FEBS Lett 1995357255–259. [DOI] [PubMed] [Google Scholar]
- 19.Sobin L H, Wittekind C h. eds. TNM classification of malignant tumours. 6th edn. New York: John Wiley & Sons, Inc, 2002
- 20.Cowland J B, Sorensen O E, Sehested M.et al Neutrophil gelatinase‐associated lipocalin is up‐regulated in human epithelial cells by IL‐1 beta, but not by TNF‐alpha. J Immunol 20031716630–6639. [DOI] [PubMed] [Google Scholar]
- 21.Xie J J, Xu L Y, Zhang H H.et al Role of fascin in the proliferation and invasiveness of esophageal carcinoma cells. Biochem Biophys Res Commun 2005337355–362. [DOI] [PubMed] [Google Scholar]
- 22.Forsyth P A, Wong H, Laing T D.et al Gelatinase‐A (MMP‐2), gelatinase‐B (MMP‐9) and membrane type matrix metalloproteinase‐1 (MT1‐MMP) are involved in different aspects of the pathophysiology of malignant gliomas. Br J Cancer 1999791828–1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mallbris L, O'Brien K P, Hulthen A.et al Neutrophil gelatinase‐associated lipocalin is a marker for dysregulated keratinocyte differentiation in human skin. Exp Dermatol 200211584–591. [DOI] [PubMed] [Google Scholar]
- 24.van Dorst E B, van Muijen G N, Litvinov S V.et al The limited difference between keratin patterns of squamous cell carcinomas and adenocarcinomas is explicable by both cell lineage and state of differentiation of tumour cells. J Clin Pathol 199851679–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kitamura K, Kuwano H, Yasuda M.et al What is the earliest malignant lesion in the esophagus? Cancer 199677(Suppl)1614–1619. [DOI] [PubMed] [Google Scholar]
- 26.Shi S T, Yang G Y, Wang L D.et al Role of p53 gene mutations in human esophageal carcinogenesis: results from immunohistochemical and mutation analyses of carcinomas and nearby non‐cancerous lesions. Carcinogenesis 199920591–597. [DOI] [PubMed] [Google Scholar]
- 27.Fernandez C A, Yan L, Louis G.et al The matrix metalloproteinase‐9/neutrophil gelatinase‐associated lipocalin complex plays a role in breast tumor growth and is present in the urine of breast cancer patients. Clin Cancer Res 2005115390–5395. [DOI] [PubMed] [Google Scholar]
- 28.Lee H J, Lee E K, Lee K J.et al Ectopic expression of neutrophil gelatinase‐associated lipocalin suppresses the invasion and liver metastasis of colon cancer cells. Int J Cancer 20061182490–2497. [DOI] [PubMed] [Google Scholar]