Abstract
Proopiomelanocortin (POMC) deficiency causes severe obesity through hyperphagia of hypothalamic origin. However, low glucocorticoid levels caused by adrenal insufficiency mitigate against insulin resistance, hyperphagia and fat accretion in Pomc−/− mice. Upon exogenous glucocorticoid replacement, corticosterone-supplemented (CORT) Pomc−/− mice show exaggerated responses, including excessive fat accumulation, hyperleptinaemia and insulin resistance. To investigate the peripheral mechanisms underlying this glucocorticoid hypersensitivity, we examined the expression levels of key determinants and targets of glucocorticoid action in adipose tissue and liver. Despite lower basal expression of 11β-hydroxysteroid dehydrogenase type 1 (11β-HSD1), which generates active glucocorticoids within cells, CORT-mediated induction of 11β-HSD1 mRNA levels was more pronounced in adipose tissues of Pomc−/− mice. Similarly, CORT treatment increased lipoprotein lipase mRNA levels in all fat depots in Pomc−/− mice, consistent with exaggerated fat accumulation. Glucocorticoid receptor (GR) mRNA levels were selectively elevated in liver and retroperitoneal fat of Pomc−/− mice but were corrected by CORT in the latter depot. In liver, CORT increased phosphoenolpyruvate carboxykinase mRNA levels specifically in Pomc−/− mice, consistent with their insulin-resistant phenotype. Furthermore, CORT induced hypertension in Pomc−/− mice, independently of adipose or liver renin–angiotensin system activation. These data suggest that CORT-inducible 11β-HSD1 expression in fat contributes to the adverse cardiometabolic effects of CORT in POMC deficiency, whereas higher GR levels may be more important in liver.
Introduction
Glucocorticoids exert pleiotrophic effects on metabolism and energy partitioning. Centrally, they increase food intake and reduce energy expenditure, whilst peripherally, they promote insulin resistance, fat accumulation (Dallman et al. 1993, Kellendonk et al. 2002) and hypertension (Saruta 1996, Whitworth et al. 2001). Polymorphisms in the human glucocorticoid receptor NR3c1 gene (GR) are associated with glucocorticoid hypersensitivity, visceral obesity, hypertension and increased cardiovascular disease risk (Buemann et al. 1997, Rosmond et al. 2000, Dobson et al. 2001, Ukkola et al. 2001a,b, van Rossum et al. 2003). Many rodent models of obesity are characterised by hypercorticosteronaemia, with weight gain normalised following adrenalectomy and reinstated by glucocorticoid replacement (Debons et al.1982, Freedman et al. 1986, Sainsbury et al.1997, Makimura et al. 2000). Although plasma glucocorticoid levels are normal in human idiopathic obesity (Flier 2004), it has been proposed that intra-adipose glucocorticoid action is selectively increased, through increased adipose expression of 11β-hydroxysteroid dehydrogenase type 1 (11β-HSD1), the intracellular enzyme that regenerates active glucocorticoids from intrinsically inert 11-keto-glucocorticoids (Kotelevtsev et al. 1997, Jamieson et al. 2000, Andrew et al. 2002).
Obese humans (Rask et al. 2001, Paulmyer-Lacroix et al. 2002, Lindsay et al. 2003, Kannisto et al. 2004) and some rodent models of obesity (Livingstone et al. 2000, Masuzaki et al. 2001) have selectively increased adipose levels of 11β-HSD1 and transgenic overexpression of 11β-HSD1 in adipocytes causes hyperphagia, obesity, insulin resistance and hypertension despite unchanged systemic glucocorticoid levels (Masuzaki et al. 2001, 2003). Hepatic overexpression of 11β-HSD1 has no effect on adiposity, but causes hypertension and insulin resistance (Paterson et al. 2004). Conversely, mice deficient in 11β-HSD1 are insulin sensitised and resist the adverse metabolic effects of a high-fat diet (Kotelevtsev et al. 1997, Morton et al. 2001, 2004).
Proopiomelanocortin (POMC) is a polypeptide precursor which undergoes extensive post-translational modification to yield a range of smaller, biological active peptides. These include α-, β- and γ-melanocyte-stimulating hormone and adrenocorticotrophic hormone (ACTH), collectively known as melanocortins. Inactivating mutations of the POMC gene in humans and mice result in a complex phenotype. Loss of melanocortin signalling within the hypothalamus causes hyperphagia and obesity (Krude et al. 1998, Yaswen et al.1999, Challis et al. 2004). Further, a failure to produce ACTH within the anterior pituitary causes adrenal insufficiency with low or absent circulating glucocorticoids (Krude et al. 1998, Yaswen et al.1999, Challis et al. 2004). Pomc−/− mice are therefore unusual amongst rodent models in that obesity develops in the absence of circulating glucocorticoids. However, glucocorticoid treatment exacerbates hyperphagia and obesity in adult Pomc−/− mice and induces severe insulin resistance, hyperleptinaemia and diabetes (Coll et al. 2005).
We have tested the hypothesis that increased glucocorticoid action in peripheral tissues of glucocorticoid-treated Pomc−/− mice contributes to their apparent glucocorticoid hypersensitivity and exaggerated metabolic syndrome-like phenotype. We further demonstrate that glucocorticoid replacement induces hypertension in Pomc−/− mice, independently of renin–angiotensin system (RAS) activation.
Materials and Methods
Animals and CORT replacement
The generation of Pomc−/− mice on a 129/SvEv background has been described previously (Challis et al. 2004). All mice were housed in standard conditions on a 12 h light:12 h darkness cycle (lights on 0070 h) with ad libitum access to water and chow (4·5% fat diet, Special Diet Services, Witham, UK). Eight-week-old male mice (n=5 per group) were treated with corticosterone (25 μg/ml) in their drinking water, a dose that results in similar plasma glucocorticoid levels and hypothalamic corticotrophin releasing hormone (CRH) mRNA levels in Pomc−/− and wild-type mice (Coll et al. 2005). All animal protocols used in these studies were approved under the auspices of the UK Home Office Animals (Scientific Procedures) Act 1986.
Blood pressure measurement
Systolic blood pressure was measured photoelectrically in the tail of restrained conscious mice using an IITC model 179 analyser (Woodland Hills, CA, USA). Prior to recording measurements, all mice underwent three periods of training to accustom them to the procedure. Mice were warmed at 32 °C for 30 min before taking ten consecutive readings. The first five were discounted and a mean value of systolic blood pressure was calculated from the last five readings. Five mice from each treatment group were measured. All analogue recordings were analysed by an independent observer who was blinded to the genotype of the mice and any treatment they had received.
Plasma hormone and lipid measurements
Animals were killed between 0800 and 0900 h by cervical dislocation. Trunk blood samples were collected into EDTA-coated tubes (Sarstedt, Leicester, UK), centrifuged at 6000 g for 10 min and plasma stored at −80 °C until required for assay. Non-esterified fatty acid (NEFA) and triglyceride levels were determined by commercial kits (NEFA, Roche Diagnostics; triglyceride, Dade Behring, Marburg, Germany). Plasma renin and angiotensinogen concentrations were determined as previously described (Morton et al. 2005).
Tissue morphology and hepatic triglyceride levels
Neutral lipids, cholesterol and fatty acids were identified by light microscopy at 40× magnification in cryostat liver sections (30 μm) stained with oil red O (Sigma) and counter stained with haematoxylin as previously described (Morton et al. 2005). Hepatic triglycerides were extracted by homogenisation in isopropanol (ten volumes) and then incubated at 37 °C for 45 min and measured spectrophotometrically in supernatants (3000 g for 10 min) using reagent TR224221 (Alpha Laboratories, Eastleigh, Hampshire, UK).
RNA extraction and northern blot analysis
Pieces of liver and adipose tissues (inguinal, retroperitoneal and epididymal) were rapidly frozen in dry ice, stored at −80 °C and then homogenised in Trizol reagent (Invitrogen). Total RNA was purified using a binding matrix (RNaid Plus kit, BIO 101; Anachem, UK) and eluted in diethylpyrocarbonate-treated water containing 400 U/ml RNasin (Promega) and 10 mmol/l dithiothreitol. RNA (5–10 μg) was blotted and hybridised to 32P-labelled cDNA probes for mouse 11β-HSD1, GR, angiotensinogen, phosphoenolpyruvate carboxykinase (PEPCK), lipoprotein lipase (LPL) and 18S as previously described (Morton et al. 2005). Specific mRNAs were quantified using a phosphorimager (Fuji BAS FLA 2000, Raytek, Sheffield, UK) and Aida image analysis software (Raytek) and are expressed in arbitrary units relative to 18S RNA.
Statistical analyses
The effects of genotype and corticosterone interactions were assessed by two-way ANOVA followed by post hoc Tukey's tests for group differences. Significance was set at P<0·05. Values are means±s.e.m.
Results
Pomc−/− mice have reduced intra-adipose GC action but exaggerated CORT-mediated GC amplification
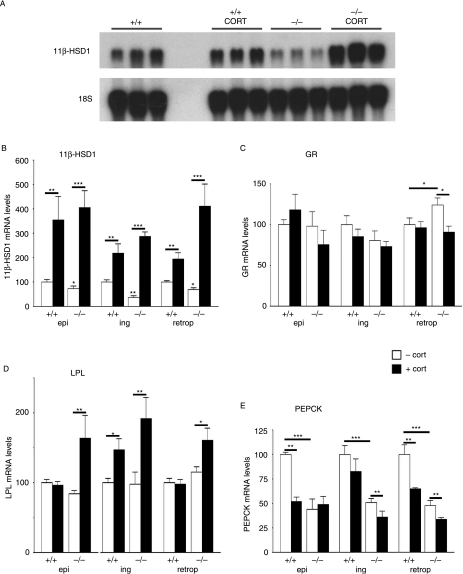
Corticosterone-treated Pomc−/− and wild-type mice had similar plasma corticosterone levels and hypothalamic CRH mRNA levels (Coll et al. 2005). To examine potential mechanisms of corticosterone hypersensitivity in Pomc−/− mice, 11β-HSD1 and GR mRNA levels were measured in epididymal, inguinal and retroperitoneal adipose depots. Adipose 11β-HSD1 mRNA expression was lower in all untreated Pomc−/− compared with wild-type mice (Fig. 1A) and was dramatically increased by corticosterone in both genotypes (Fig. 1A), with larger increases (two- to four-fold greater) in Pomc−/− mice.
Figure 1.
Mediators of GC action in adipose tissue of Pomc−/− mice and effects of CORT treatment on GC target genes. (A) Representative northern blot showing levels of 11β-HSD1 mRNA and 18S RNA in epididymal adipose tissue of Pomc−/− (−/−) and wild-type (+/+) mice, either untreated or treated for 10 days with corticosterone (cort). (B–E) Quantitation of adipose tissue-specific 11β-HSD1 (B), GR (C), LPL (D) and PEPCK (E) mRNA levels in experimental mice. Epi, epididymal fat; ing, inguinal fat; retro, retroperitoneal fat. Data are presented as percentage of the value in untreated wild-type mice (100%) and are the means±s.e.m.; n=5 per group. Significance *P<0·05, **P<0·01 and ***P<0·001.
Adipose expression of GR mRNA was higher in the retroperitoneal fat of Pomc−/− mice and restored to wild-type levels by corticosterone treatment (Fig. 1B). GR mRNA levels did not differ in inguinal and epididymal fat between Pomc−/− and wild-type mice, and were unaffected by corticosterone treatment in either genotype (Fig. 1B).
To investigate mechanisms downstream of 11β-HSD1/GR by which corticosterone treatment selectively increases fat mass in Pomc−/− mice, adipose levels of mRNA encoding LPL, a glucocorticoid-regulated gene (Fried et al. 1993), were measured. Although LPL mRNA levels were the same in untreated Pomc−/− and wild-type mice in all depots, adipose LPL expression in Pomc−/− mice was markedly increased by corticosterone treatment (Fig. 1C) consistent with increased triglyceride uptake, and fat mass in Pomc−/− mice. In wild-type mice, corticosterone treatment increased LPL mRNA only in the inguinal depot, and to a lesser extent than in Pomc−/− mice (Fig. 1C), suggesting adipose depot-dependent regulation of LPL by glucocorticoids in non-obese mice, consistent with previous data in rats (Freedman et al. 1986).
PEPCK is an enzyme essential for gluconeogenesis in liver and glycerol synthesis in adipose tissue (Pilkis & Granner 1992, Reshef et al. 2003). PEPCK is a classical glucocorticoid target gene which is positively regulated by glucocorticoids in hepatocytes and negatively regulated in adipocytes (Sasaki et al.1984, Nechushtan et al. 1987). Consistent with this, adipose PEPCK mRNA levels were decreased in epididymal and retroperitoneal fat by corticosterone treatment in wild-type mice (Fig. 1D). Surprisingly, given their glucocorticoid deficiency, Pomc−/− mice had lower levels of PEPCK mRNA in adipose tissue than in wild-type (Fig. 1D). However, although corticosterone treatment in Pomc−/− mice decreased PEPCK expression in inguinal and retroperitoneal adipose tissue (significantly lower than in corticosterone-treated wild-type mice; P=0·01), it had no effect on PEPCK mRNA levels in epididymal adipose tissue, suggesting that other regulatory factors dominate PEPCK expression in adipose tissue of Pomc−/− mice (Fig. 1D).
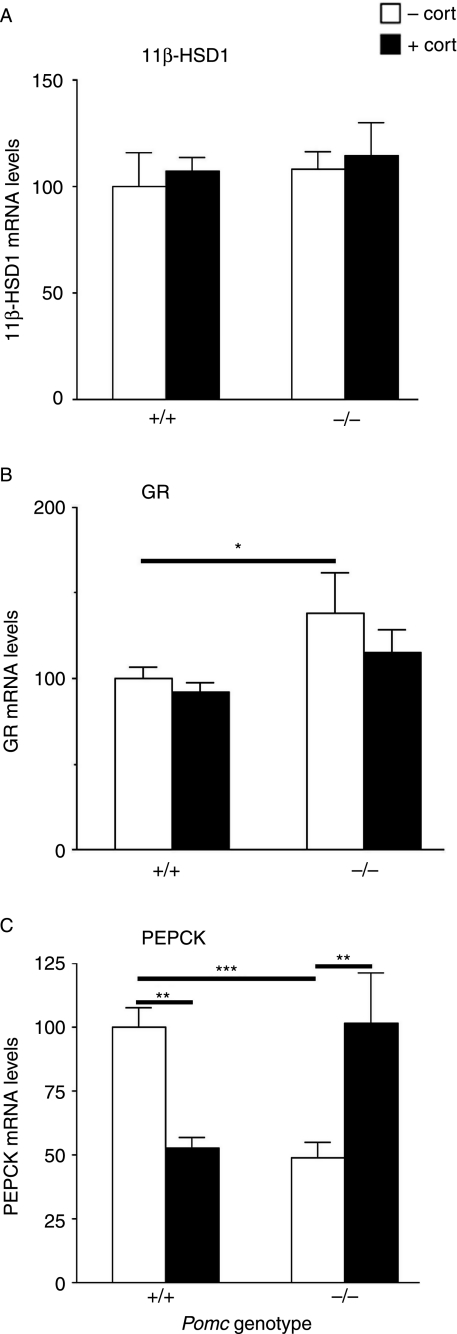
Pomc−/− mice are dyslipidaemic, and have unaltered hepatic 11β-HSD1 but higher GR mRNA levels
Hepatic 11β-HSD1 mRNA levels were similar between the two genotypes (Fig. 2A) and unaffected by corticosterone (Fig. 2A). Hepatic GR mRNA levels were higher in Pomc−/− compared with wild-type mice (Fig. 2B), but again corticosterone had no effect on GR mRNA levels (Fig. 2B).
Figure 2.
Mediators of GC action in the liver of Pomc−/− mice and effects of CORT treatment on GC target genes. Liver mRNA expression of (A) 11β-HSD1, (B) GR and (C) PEPCK in Pomc−/− (−/−) and wild-type (+/+) mice, either untreated or treated for 10 days with corticosterone (cort). Data are presented as percentages of the value in untreated control mice (100%) and are the means±s.e.m.; n=5 per group. Significance *P<0·05, **P<0·01 and ***P<0·001.
Hepatic PEPCK expression was lower in Pomc−/− than in wild-type mice (Fig. 2C) and was increased by corticosterone treatment to levels equivalent to untreated wild-type mice. In contrast, corticosterone decreased hepatic PEPCK mRNA levels in wild-type mice (Fig. 2C).
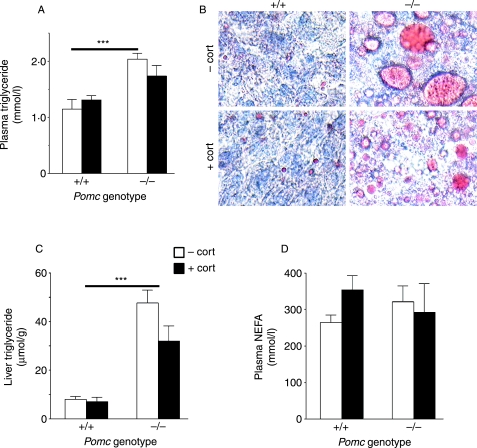
Pomc−/− mice showed markedly higher circulating triglyceride levels (Fig. 3A) and hepatic lipid accumulation than wild-type mice (Fig. 3B), with sixfold higher levels of hepatic triglyceride (P<0·001; Fig. 3C). However, corticosterone had no effect on plasma triglyceride levels in either genotype (Fig. 3A), nor did it worsen the liver phenotype (Fig. 3C). Pomc−/− and wild-type mice had similar plasma NEFA levels which were unaffected by corticosterone (Fig. 3D).
Figure 3.
Dyslipidaemia and fatty liver in Pomc−/− mice. (A) Plasma triglyceride levels in Pomc−/− (−/−) and wild-type (+/+) mice, either untreated or treated for 10 days with corticosterone (cort). (B) Oil Red O staining of neutral lipid in liver sections of wild-type mice (+/+, left upper panel), CORT-treated wild-type mice (+/+, left bottom panel), Pomc−/− (−/−, right upper panel) and CORT-treated Pomc−/− (−/−, right bottom panel). Magnification is 40×; red, oil red O; blue, haematoxylin (nuclei). (C) Hepatic triglyceride content in Pomc−/− (−/−) and wild-type (+/+) mice, either untreated or treated for 10 days with corticosterone (cort). (D) Plasma levels of non-esterified fatty acids (NEFA) in Pomc−/− (−/−) and wild-type (+/+) mice, either untreated or treated for 10 days with corticosterone (cort). Data are means±s.e.m.; (n=6 per group). Significance ***P<0·001.
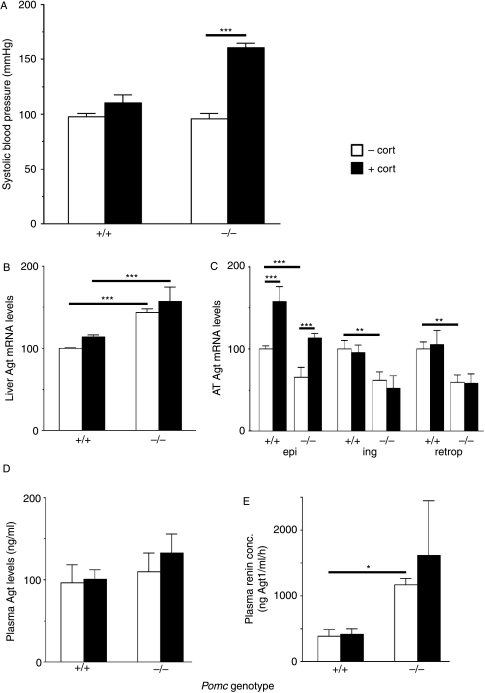
CORT drives hypertension in Pomc−/− mice independently of adipose and liver RAS activation
Pomc−/− mice had similar blood pressure to wild-type mice (Fig. 4A). Corticosterone markedly increased blood pressure only in Pomc−/− mice (Fig. 4A). Since hypertension following transgenic expression of 11β-HSD1 in adipose or liver is associated with increased levels of angiotensinogen in each of these tissues respectively (Masuzaki et al. 2001, Paterson et al. 2004), we hypothesised that a similar mechanism may drive corticosterone-mediated hypertension in Pomc−/− mice. We therefore examined key components of the RAS (Guyton 1991). Pomc−/− mice had higher hepatic angiotensinogen mRNA levels than controls (Fig. 4B). However, corticosterone did not alter hepatic angiotensinogen mRNA levels in either genotype (Fig. 4B). Consistent with lower intra-adipose GC action, adipose angiotensinogen mRNA levels were lower in Pomc−/− mice in all adipose depots (Fig. 4C). Corticosterone increased angiotensinogen mRNA levels specifically in epididymal adipose tissue of both genotypes (twofold increase; P<0·001; Fig. 4C) but had no effect on angiotensinogen mRNA levels in inguinal or retroperitoneal adipose tissue of either genotype (Fig. 4C). Plasma angiotensinogen concentrations did not differ with genotype or corticosterone (Fig. 4D). As has been found in another model of glucocorticoid-deficient obesity (Morton et al. 2005), plasma renin concentration was markedly higher in Pomc−/− mice (Fig. 4E) but this was unaffected by corticosterone (Fig. 4E).
Figure 4.
Corticosterone treatment increases blood pressure in Pomc−/− mice: effect of CORT treatment on the Renin-angiotensin system. Effect of 10 days corticosterone treatment (cort) on (A) systolic blood pressure, (B) renin concentration, (C) plasma angiotensinogen, (D) angiotensinogen (Agt) mRNA in adipose tissue (AT), and (E) angiotensinogen (Agt) mRNA levels in liver in wild-type (+/+) and Pomc−/− (−/−) mice. Epi, epididymal fat; ing, inguinal fat; retro, retroperitoneal fat. Data are means±s.e.m., and for transcript levels are expressed relative to levels in untreated wild-type mice (100%); n=5 per group. Significance *P<0·05, **P<0·01 and ***P<0·001.
Discussion
Increased glucocorticoid action specifically in adipose (Masuzaki et al. 2001) or liver (Paterson et al. 2004) produces distinct metabolic syndromes with hypertension. Increased GR sensitivity is also associated with altered fat distribution, hypertension and cardiometabolic disease (Buemann et al. 1997, Rosmond et al. 2000, Dobson et al. 2001, Ukkola et al. 2001a,b, van Rossum et al. 2003). We hypothesised that altered tissue regeneration of active glucocorticoid and/or peripheral tissue sensitivity to GCs might explain in part the exaggerated fat accumulation, insulin resistance (Coll et al. 2005) and the hypertension observed in Pomc−/− mice with glucocorticoid replacement.
With fixed circulating glucocorticoid levels, 11β-HSD1 and GR expression levels are the key determinants of GC action. Pomc−/− mice had lower adipose but similar hepatic levels of 11β-HSD1 mRNA levels to wild-type mice. Corticosterone treatment dramatically and more markedly increased 11β-HSD1 in the adipose tissue of Pomc−/− mice. This was accompanied by a marked increase in the expression of the glucocorticoid-inducible (Fried et al. 1993) gene LPL, which is consistent with the exaggerated accumulation of fat in these mice. Intriguingly, these data suggest that, at least in adipose tissue, 11β-HSD1 itself is a glucocorticoid target gene. This finding is consistent with most (Hammami & Siteri 1991, Jamieson et al. 1995, Voice et al. 1996, Bujalska et al. 1999), but not all (Napolitano et al. 1998) previous reports of glucocorticoid induction of 11β-HSD1 in a variety of cell types. Although not specifically measured here, increased adipose 11β-HSD1 activity is predicted to selectively amplify intra-adipose glucocorticoid concentrations, particularly when circulating levels of substrate are high. On the other hand, our data suggest that congenital glucocorticoid deficiency has little impact upon hepatic 11β-HSD1 levels in vivo and is not regulated by corticosterone. In contrast, 11β-HSD1 mRNA levels are highly and positively regulated by glucocorticoids in adipose tissue.
GR levels are another major determinant of cellular glucocorticoid sensitivity (Vanderbilt et al. 1987, Geley et al. 1996). Small differences in GR mRNA levels can markedly alter glucocorticoid responsiveness (Geley et al. 1996, Reichardt et al. 2000). Pomc−/− mice had elevated GR mRNA levels in liver and retroperitoneal adipose tissue, suggesting increased glucocorticoid sensitivity selectively in these depots. Following corticosterone replacement in Pomc−/− mice, GR mRNA levels were restored to wild-type levels in retroperitoneal adipose tissue but not in liver, consistent with tissue- and time-specific differences in GR autoregulation (Kalinyak et al. 1987, Dong et al. 1988, Sheppard et al. 1990, Holmes et al., 1995, 1997, Reichardt et al. 2000).
Corticosterone had no additional effects on the hypertriglyceridaemia and fatty liver of the Pomc−/− mice, and did not affect plasma NEFAs, which were normal in Pomc−/− mice. The corticosterone-driven caloric excess in Pomc−/− mice may drive a further increase in the flux of triglycerides from the liver, that, coupled with increased adipose uptake via LPL, maintains the circulating and liver triglyceride levels constant and is consistent with increased adipose tissue mass in corticosterone-treated Pomc−/− mice (Coll et al. 2005).
Adipose PEPCK is critical for glyceroneogenesis and is thus a key regulator of the level of fatty acid re-esterification (reviewed in Reshef et al. 2003). Unexpectedly, since glucocorticoids reduce adipose PEPCK, glucocorticoid-deficient Pomc−/− mice had lower levels of PEPCK mRNA in all adipose depots. This was further decreased by corticosterone treatment. The lower level of PEPCK mRNA in untreated Pomc−/− mice may be due to their higher fed blood glucose levels (Nechushtan et al. 1987, Opherk et al. 2004), thus reducing the need for glyceroneogenesis to generate glycerol phosphate for fatty acid re-esterification. Pomc−/− mice have lower hepatic expression of PEPCK. This may not be due to the lack of glucocorticoid signalling in liver, as mice with a liver-specific knockout of GR have normal levels of PEPCK in liver (Opherk et al. 2004), but may be related to the higher circulating levels of insulin in Pomc−/− mice compared with wild-type (Coll et al. 2005). Insulin dominantly and negatively suppresses hepatic PEPCK in the fed state (Pilkis & Granner 1992). In corticosterone-treated wild-type mice, the repressive effect of insulin predominated. Indeed, the decreased levels of PEPCK in these mice compared with untreated wild-type mice may reflect the increase in insulin levels following corticosterone (Coll et al. 2005). In contrast, hepatic PEPCK mRNA levels doubled following corticosterone treatment in Pomc−/− mice, consistent with hepatic insulin resistance and marked hyperinsulinaemia (Coll et al. 2005).
Blood pressure in Pomc−/− mice is normal despite their hypoadrenal state. This implies that secondary mechanisms are invoked to maintain cardiovascular function when circulating aldosterone and corticosterone concentrations are chronically reduced (Coll et al. 2004). It seems likely that the increased renin activity which we have observed in Pomc−/− mice is part of this adaptive process. However, corticosterone replacement did not normalise renin activity and selectively increased blood pressure in Pomc−/− mice. This was not attributed to a further activation of the circulating RAS, since neither renin nor its substrate angiotensinogen was increased. Indeed, the expression of angiotensinogen mRNA in liver and adipose tissues did not correlate with blood pressure. It seems likely that corticosterone augmented existing mechanisms that were already sustaining vascular function. Apart from renin, these secondary processes are likely to involve the hyperinsulinaemic (Sowers 2004) state of Pomc−/− mice (which is exacerbated by corticosterone treatment; Coll et al. 2005), the sympathetic nervous system (Rascher et al. 1979; which is thought to explain glucocorticoid-induced hypertension in normal mice) or structural adaptation of the vasculature (Wallerath et al. 2004).
In summary, we show that increased adipose tissue-specific sensitivity to glucocorticoids in Pomc−/− mice may result in part from exaggerated induction of 11β-HSD1 in adipose tissue with corticosterone administration. Whilst acknowledging that mRNA changes do not always translate to altered protein (or enzyme activity) levels, these data nevertheless suggest that 11β-HSD1 might be a more potent mediator of intra-adipose GC action than the GR levels, whereas in liver, higher GR levels contribute to the diabetogenic phenotype of the Pomc−/− mice.
Acknowledgements
We thank Keith Burling for assistance with plasma hormone and lipid measurements and members of the Endocrinology Unit, QMRI for helpful comments and discussions. The authors declare that there is no conflict of interest that would prejudice the impartiality of this scientific work.
Funding
This work has been supported by the Wellcome Trust Programme grant (J R S and K EC), by separate MRC Programme grants to S O'R and C J K and by the EU Sixth Framework Programme Diabesity. Z M is supported by the Wellcome Trust PhD studentship, A P C by an MRC Clinician Scientist Award and N M M by the Wellcome Trust Research Career Development Fellowship.
References
- Andrew R, Smith K, Jones G.C, Walker B.R. Distinguishing the activities of 11β-hydroxysteroid dehydrogenases in vivo using isotopically labeled cortisol. Journal of Clinical Endocrinology and Metabolism. 2002;87:277–285. doi: 10.1210/jcem.87.1.8157. [DOI] [PubMed] [Google Scholar]
- Buemann B, Vohl M.C, Chagnon M, Chagnon Y.C, Gagnon J, Perusse L, Dionne F, Despres J.P, Tremblay A, Nadeau A, et al. Abdominal visceral fat is associated with a BclI restriction fragment length polymorphism at the glucocorticoid receptor gene locus. Obesity Research. 1997;5:186–192. doi: 10.1002/j.1550-8528.1997.tb00292.x. [DOI] [PubMed] [Google Scholar]
- Bujalska I.J, Kumar S, Hewison M, Stewart P.M. Differentiation of adipose stromal cells: the roles of glucocorticoids and 11β-hydroxysteroid dehydrogenase. Endocrinology. 1999;140:3188–3196. doi: 10.1210/endo.140.7.6868. [DOI] [PubMed] [Google Scholar]
- Challis B.G, Coll A.P, Yeo G.S, Pinnock S.B, Dickson S.L, Thresher R.R, Dixon J, Zahn D, Rochford J.J, White A, et al. Mice lacking pro-opiomelanocortin are sensitive to high-fat feeding but respond normally to the acute anorectic effects of peptide-YY3-36. PNAS. 2004;101:4695–4700. doi: 10.1073/pnas.0306931101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coll A.P, Challis B.G, Yeo G.S, Snell K, Piper S.J, Halsall D, Thresher R.R, O'Rahilly S. The effects of pro-opiomelanocortin deficiency on murine adrenal development and responsiveness to adrenocorticotropin. Endocrinology. 2004;145:4721–4727. doi: 10.1210/en.2004-0491. [DOI] [PubMed] [Google Scholar]
- Coll A.P, Challis B.G, Lopez M, Piper S, Yeo G.S, O'Rahilly S. Proopiomelanocortin-deficient mice are hypersensitive to the adverse metabolic effects of glucocorticoids. Diabetes. 2005;54:2269–2276. doi: 10.2337/diabetes.54.8.2269. [DOI] [PubMed] [Google Scholar]
- Dallman M.F, Strack A.M, Akana S.F, Bradbury M.J, Hanson E.S, Scribner K.A, Smith M. Feast and famine: critical role of glucocorticoids with insulin in daily energy flow. Frontiers in Neuroendocrinology. 1993;14:303–347. doi: 10.1006/frne.1993.1010. [DOI] [PubMed] [Google Scholar]
- Debons A.F, Siclari E, Das K.C, Fuhr B. Gold thioglucose-induced hypothalamic damage, hyperphagia, and obesity: dependence on the adrenal gland. Endocrinology. 1982;110:2024–2029. doi: 10.1210/endo-110-6-2024. [DOI] [PubMed] [Google Scholar]
- Dobson M.G, Redfern C.P, Unwin N, Weaver J.U. The N363S polymorphism of the glucocorticoid receptor: potential contribution to central obesity in men and lack of association with other risk factors for coronary heart disease and diabetes mellitus. Journal of Clinical Endocrinology and Metabolism. 2001;86:2270–2274. doi: 10.1210/jcem.86.5.7465. [DOI] [PubMed] [Google Scholar]
- Dong Y, Poellinger L, Gustafsson J-Å, Okret S. Regulation of glucocorticoid receptor expression: evidence for transcriptional and posttranslational mechanisms. Molecular Endocrinology. 1988;2:1256–1264. doi: 10.1210/mend-2-12-1256. [DOI] [PubMed] [Google Scholar]
- Flier J.S. Obesity wars: molecular progress confronts an expanding epidemic. Cell. 2004;116:337–350. doi: 10.1016/s0092-8674(03)01081-x. [DOI] [PubMed] [Google Scholar]
- Freedman M.R, Horwitz B.A, Stern J.S. Effect of adrenalectomy and glucocorticoid replacement on development of obesity. American Journal of Physiology. 1986;250:R595–R607. doi: 10.1152/ajpregu.1986.250.4.R595. [DOI] [PubMed] [Google Scholar]
- Fried S.K, Russell C.D, Grauso N.L, Brolin R.E. Lipoprotein lipase regulation by insulin and glucocorticoid in subcutaneous and omental adipose tissues of obese women and men. Journal of Clinical Investigation. 1993;92:2191–2198. doi: 10.1172/JCI116821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geley S, Hartmann B.L, Hala M, Strasser-Wozak E.M, Kapelari K, Kofler R. Resistance to glucocorticoid-induced apoptosis in human T-cell acute lymphoblastic leukemia CEM-C1 cells is due to insufficient glucocorticoid receptor expression. Cancer Research. 1996;56:5033–5038. [PubMed] [Google Scholar]
- Guyton A.C. Blood pressure control: special role of the kidneys and body fluids. Science. 1991;252:1813–1816. doi: 10.1126/science.2063193. [DOI] [PubMed] [Google Scholar]
- Hammami M.M, Siiteri P.K. Regulation of 11β-hydroxysteroid dehydrogenase activity in human skin fibroblasts: enzymatic modulation of glucocorticoid action. Journal of Clinical Endocrinology and Metabolism. 1991;73:326–334. doi: 10.1210/jcem-73-2-326. [DOI] [PubMed] [Google Scholar]
- Holmes M.C, Yau J.L.W, French K.L, Seckl J.R. The effect of adrenalectomy on 5-hydroxytryptamine and corticosteroid receptor subtype messenger RNA expression in rat hippocampus. Neuroscience. 1995;64:327–337. doi: 10.1016/0306-4522(94)00407-v. [DOI] [PubMed] [Google Scholar]
- Holmes M.C, French K.L, Seckl J.R. Dysregulation of diurnal rhythms of serotonin 5-HT2C and corticosteroid receptor gene expression in the hippocampus with food restriction and glucocorticoids. Journal of Neuroscience. 1997;17:4056–4065. doi: 10.1523/JNEUROSCI.17-11-04056.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamieson P.M, Chapman K.E, Edwards C.R.W, Seckl J.R. 11β-Hydroxysteroid dehydrogenase is an exclusive 11β-reductase in primary cultures of rat hepatocytes: effect of physicochemical and hormonal manipulations. Endocrinology. 1995;136:4754–4761. doi: 10.1210/endo.136.11.7588203. [DOI] [PubMed] [Google Scholar]
- Jamieson P.M, Walker B.R, Chapman K.E, Andrew R, Rossiter S, Seckl J.R. 11β-Hydroxysteroid dehydrogenase type 1 is a predominant 11β-reductase in the intact perfused rat liver. Journal of Endocrinology. 2000;165:685–692. doi: 10.1677/joe.0.1650685. [DOI] [PubMed] [Google Scholar]
- Kalinyak J.E, Dorin R.I, Hoffman A.R, Perlman A.J. Tissue-specific regulation of glucocorticoid receptor mRNA by dexamethasone. Journal of Biological Chemistry. 1987;262:10441–10444. [PubMed] [Google Scholar]
- Kannisto K, Pietilainen K.H, Ehrenborg E, Rissanen A, Kaprio J, Hamsten A, Yki-Jarvinen H. Overexpression of 11β-hydroxysteroid dehydrogenase-1 in adipose tissue is associated with acquired obesity andfeatures of insulin resistance: studies in young adult monozygotic twins. Journal of Clinical Endocrinology and Metabolism. 2004;89:4414–4421. doi: 10.1210/jc.2004-0153. [DOI] [PubMed] [Google Scholar]
- Kellendonk C, Eiden S, Kretz O, Schutz G, Schmidt I, Tronche F, Simon E. Inactivation of the GR in the nervous system affects energy accumulation. Endocrinology. 2002;143:2333–2340. doi: 10.1210/endo.143.6.8853. [DOI] [PubMed] [Google Scholar]
- Kotelevtsev Y, Holmes M.C, Burchell A, Houston P.M, Schmoll D, Jamieson P, Best R, Brown R, Edwards C.R.W, Seckl J.R, et al. 11β-Hydroxysteroid dehydrogenase type 1 knockout mice show attenuated glucocorticoid inducible responses and resist hyperglycaemia on obesity or stress. PNAS. 1997;94:14924–14929. doi: 10.1073/pnas.94.26.14924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krude H, Biebermann H, Luck W, Horn R, Brabant G, Gruters A. Severe early-onset obesity, adrenal insufficiency and red hair pigmentation caused by POMC mutations in humans. Nature Genetics. 1998;19:155–157. doi: 10.1038/509. [DOI] [PubMed] [Google Scholar]
- Lindsay R.S, Wake D.J, Nair S, Bunt J, Livingstone D.E, Permana P.A, Tataranni P.A, Walker B.R. Subcutaneous adipose 11β-hydroxysteroid dehydrogenase type 1 activity and messenger ribonucleic acid levels are associated with adiposity and insulinemia in Pima Indians and Caucasians. Journal of Clinical Endocrinology and Metabolism. 2003;88:2738–2744. doi: 10.1210/jc.2002-030017. [DOI] [PubMed] [Google Scholar]
- Livingstone D.E.W, Jones G.C, Smith K, Jamieson P.M, Andrew R, Kenyon C.J, Walker B.R. Understanding the role of glucocorticoids in obesity: tissue-specific alterations of corticosterone metabolism in obese Zucker rats. Endocrinology. 2000;141:560–563. doi: 10.1210/endo.141.2.7297. [DOI] [PubMed] [Google Scholar]
- Makimura H, Mizuno T.M, Roberts J, Silverstein J, Beasley J, Mobbs C.V. Adrenalectomy reverses obese phenotype and restores hypothalamic melanocortin tone in leptin-deficient ob/ob mice. Diabetes. 2000;49:1917–1923. doi: 10.2337/diabetes.49.11.1917. [DOI] [PubMed] [Google Scholar]
- Masuzaki H, Paterson J, Shinyama H, Morton N.M, Mullins J.J, Seckl J.R, Flier J.S. A transgenic model of visceral obesity and the metabolic syndrome. Science. 2001;294:2166–2170. doi: 10.1126/science.1066285. [DOI] [PubMed] [Google Scholar]
- Masuzaki H, Yamamoto H, Kenyon C.J, Elmquist J.K, Morton N.M, Paterson J.M, Shinyama H, Sharp M.G, Fleming S, Mullins J.J, et al. Transgenic amplification of glucocorticoid action in adipose tissue causes high blood pressure in mice. Journal of Clinical Investigation. 2003;112:83–90. doi: 10.1172/JCI17845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton N.M, Holmes M.C, Fiévet C, Staels B, Tailleux A, Mullins J.J, Seckl J.R. Improved lipid and lipoprotein profile, hepatic insulin sensitivity, and glucose tolerance in 11β-hydroxysteroid dehydrogenase type 1 null mice. Journal of Biological Chemistry. 2001;276:41293–41300. doi: 10.1074/jbc.M103676200. [DOI] [PubMed] [Google Scholar]
- Morton N.M, Paterson J.M, Masuzaki H, Holmes M.C, Staels B, Fievet C, Walker B.R, Flier J.S, Mullins J.J, Seckl J.R. Novel adipose tissue mediated resistance to diet-induced visceral obesity in 11β-hydroxysteroid dehydrogenase type 1-deficient mice. Diabetes. 2004;53:931–938. doi: 10.2337/diabetes.53.4.931. [DOI] [PubMed] [Google Scholar]
- Morton N.M, Densmore V, Wamil M, Ramage L, Nichol K, Bunger L, Seckl J.R, Kenyon C.J. A polygenic model of the metabolic syndrome with reduced circulating and intra-adipose glucocorticoid action. Diabetes. 2005;54:3371–3378. doi: 10.2337/diabetes.54.12.3371. [DOI] [PubMed] [Google Scholar]
- Napolitano A, Voice M.W, Edwards C.R.W, Seckl J.R, Chapman K.E. 11β-Hydroxysteroid dehydrogenase 1 in adipocytes: expression is differentiation-dependent and hormonally regulated. Journal of Steroid Biochemistry and Molecular Biology. 1998;64:251–260. doi: 10.1016/s0960-0760(97)00200-8. [DOI] [PubMed] [Google Scholar]
- Nechushtan H, Benvenisty N, Brandeis R, Reshef L. Glucocorticoids control phosphoenolpyruvate carboxykinase gene expression in a tissue specific manner. Nucleic Acids Research. 1987;15:6405–6417. doi: 10.1093/nar/15.16.6405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opherk C, Tronche F, Kellendonk C, Kohlmuller D, Schulze A, Schmid W, Schutz G. Inactivation of the glucocorticoid receptor in hepatocytes leads to fasting hypoglycemia and ameliorates hyperglycemia in streptozotocin-induced diabetes mellitus. Molecular Endocrinology. 2004;18:1346–1353. doi: 10.1210/me.2003-0283. [DOI] [PubMed] [Google Scholar]
- Paterson J.M, Morton N.M, Fiévet C, Kenyon C.J, Holmes M.C, Staels B, Seckl J.R, Mullins J.J. Metabolic syndrome without obesity: hepatic overexpression of 11β-hydroxysteroid dehydrogenase type 1 in transgenic mice. PNAS. 2004;101:7088–7093. doi: 10.1073/pnas.0305524101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulmyer-Lacroix O, Boullu S, Oliver C, Alessi M.C, Grino M. Expression of the mRNA coding for 11β-hydroxysteroid dehydrogenase type 1 in adipose tissue from obese patients: an in situ hybridization study. Journal of Clinical Endocrinology and Metabolism. 2002;87:2701–2705. doi: 10.1210/jcem.87.6.8614. [DOI] [PubMed] [Google Scholar]
- Pilkis S.J, Granner D.K. Molecular physiology of the regulation of hepatic gluconeogenesis and glycolysis. Annual Review of Physiology. 1992;54:885–909. doi: 10.1146/annurev.ph.54.030192.004321. [DOI] [PubMed] [Google Scholar]
- Rascher W, Dietz R, Schomig A, Burkart G, Luth J.B, Mann J.F, Weber J. Modulation of sympathetic vascular tone by prostaglandins in corticosterone-induced hypertension in rats. Clinical Science. 1979;57:235s–237s. doi: 10.1042/cs057235s. [DOI] [PubMed] [Google Scholar]
- Rask E, Olsson T, Söderberg S, Andrew R, Livingstone D.E, Johnson O, Walker B.R. Tissue-specific dysregulation of cortisol metabolism in human obesity. Journal of Clinical Endocrinology and Metabolism. 2001;86:1418–1421. doi: 10.1210/jcem.86.3.7453. [DOI] [PubMed] [Google Scholar]
- Reichardt H.M, Umland T, Bauer A, Kretz O, Schütz G. Mice with an increased glucocorticoid receptor gene dosage show enhanced resistance to stress and endotoxic shock. Molecular and Cellular Biology. 2000;20:9009–9017. doi: 10.1128/mcb.20.23.9009-9017.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reshef L, Olswang Y, Cassuto H, Blum B, Croniger C.M, Kalhan S.C, Tilghman S.M, Hanson R.W. Glyceroneogenesis and the triglyceride/fatty acid cycle. Journal of Biological Chemistry. 2003;278:30413–31416. doi: 10.1074/jbc.R300017200. [DOI] [PubMed] [Google Scholar]
- Rosmond R, Chagnon Y.C, Holm G, Chagnon M, Pérusse L, Lindell K, Carlsson B, Bouchard C, Björntorp P. A glucocorticoid receptor gene marker is associated with abdominal obesity, leptin, and dysregulation of the hypothalamic–pituitary–adrenal axis. Obesity Research. 2000;8:211–218. doi: 10.1038/oby.2000.24. [DOI] [PubMed] [Google Scholar]
- van Rossum E.F, Koper J.W, van den Beld A.W, Uitterlinden A.G, Arp P, Ester W, Janssen J.A, Brinkmann A.O, de Jong F.H, Grobbee D.E, et al. Identification of the BclI polymorphism in the glucocorticoid receptor gene: association with sensitivity to glucocorticoids in vivo and body mass index. Clinical Endocrinology. 2003;59:585–592. doi: 10.1046/j.1365-2265.2003.01888.x. [DOI] [PubMed] [Google Scholar]
- Sainsbury A, Cusin I, Rohner-Jeanrenaud F, Jeanrenaud B. Adrenalectomy prevents the obesity syndrome produced by chronic central neuropeptide Y infusion in normal rats. Diabetes. 1997;46:209–214. doi: 10.2337/diab.46.2.209. [DOI] [PubMed] [Google Scholar]
- Saruta T. Mechanism of glucocorticoid-induced hypertension. Hypertension Research. 1996;19:1–8. doi: 10.1291/hypres.19.1. [DOI] [PubMed] [Google Scholar]
- Sasaki K, Cripe T.P, Koch S.R, Andreone T.L, Petersen D.D, Beale E.G, Granner D.K. Multihormonal regulation of phosphoenolpyruvate carboxykinase gene transcription. The dominant role of insulin. Journal of Biological Chemistry. 1984;259:15242–15251. [PubMed] [Google Scholar]
- Sheppard K.E, Roberts J.L, Blum M. Differential regulation of type II corticosteroid receptor messenger ribonucleic acid expression in the rat anterior pituitary and hippocampus. Endocrinology. 1990;127:431–439. doi: 10.1210/endo-127-1-431. [DOI] [PubMed] [Google Scholar]
- Sowers J.R. Insulin resistance and hypertension. American Journal of Physiology. Heart and Circulatory Physiology. 2004;286:H1597–H1602. doi: 10.1152/ajpheart.00026.2004. [DOI] [PubMed] [Google Scholar]
- Ukkola O, Pérusse L, Weisnagel S.J, Bergeron J, Després J.P, Rao D.C, Bouchard C. Interactions among the glucocorticoid receptor, lipoprotein lipase, and adrenergic receptor genes and plasma insulin and lipid levels in the Quebec Family Study. Metabolism. 2001a;50:246–252. doi: 10.1053/meta.2001.18572. [DOI] [PubMed] [Google Scholar]
- Ukkola O, Rosmond R, Tremblay A, Bouchard C. Glucocorticoid receptor Bcl I variant is associated with an increased atherogenic profile in response to long-term overfeeding. Atherosclerosis. 2001b;157:221–224. doi: 10.1016/s0021-9150(00)00712-7. [DOI] [PubMed] [Google Scholar]
- Vanderbilt J.N, Miesfeld R, Maler B.A, Yamamoto K.R. Intracellular receptor concentration limits glucocorticoid-dependent enhancer activity. Molecular Endocrinology. 1987;1:68–74. doi: 10.1210/mend-1-1-68. [DOI] [PubMed] [Google Scholar]
- Voice M.W, Seckl J.R, Edwards C.R.W, Chapman K.E. 11β-Hydroxysteroid dehydrogenase type 1 expression in 2S-FAZA hepatoma cells is hormonally regulated; a model system for the study of hepatic glucocorticoid metabolism. Biochemical Journal. 1996;317:621–625. doi: 10.1042/bj3170621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallerath T, Godecke A, Molojavyi A, Li H, Schrader J, Forstermann U. Dexamethasone lacks effect on blood pressure in mice with a disrupted endothelial NO synthase gene. Nitric Oxide. 2004;10:36–41. doi: 10.1016/j.niox.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Whitworth J.A, Schyvens C.G, Zhang Y, Mangos G.J, Kelly J.J. Glucocorticoid-induced hypertension: from mouse to man. Clinical and Experimental Pharmacology and Physiology. 2001;28:993–996. doi: 10.1046/j.1440-1681.2001.03584.x. [DOI] [PubMed] [Google Scholar]
- Yaswen L, Diehl N, Brennan M.B, Hochgeschwender U. Obesity in the mouse model of pro-opiomelanocortin deficiency responds to peripheral melanocortin. Nature Medicine. 1999;5:1066–1070. doi: 10.1038/12506. [DOI] [PubMed] [Google Scholar]