Abstract
Background
Despite the considerable mortality and morbidity associated with cardiovascular disease (CVD) many developing countries lack reliable surveillance of these ailments and their risk factors to guide intervention. This study aims to provide the first population-based estimates of CVD morbidity and mortality among adults in Aleppo-Syria and the distribution of their risk factors.
Methods
A cross-sectional survey of adults 18-65 years old residing in Aleppo-Syria was carried out in 2004 involving 2038 household representatives (45.2% men, mean age 35.3 years, response rate 86%). Main outcomes of interest were physician-diagnosed CVD (infarction, angina, failure, stroke) among survey participants, and past 5 year mortality due to CVD among their household members > 20 years of age (n=6252, 49.5% men). Measurement of blood pressure (BP), height and weight, and smoking history were obtained as well.
Findings
Prevalence of CVD was 4.8% for heart disease and 1.0% for stroke. CVD was responsible for 45.0% of overall mortality reported in the past 5 years, whereby 49% of CVD deaths occurred before the age of 65 year. Mean age of death was 62.6 years (63.6 years for HD and 61.4 years for stroke). Annual crude death rate due to CVD was 314 per 100,000 (95%CI: 215-414), of these 179 were due to heart disease, and 135 due to stroke. More men died from heart disease than women, while the opposite was true for stroke. Hypertension was detected in 40.6% (47.7% men, 34.9%women), obesity in 38.2% (28.8% men, 46.4% women), and smoking (cigarettes or waterpipe) in 38.7% (63.6% men, 19.2% women) of participants. Of those surveyed, 39.3% had 1 CVD risk factor, 27.4% had 2 risk factors, and 8.3% had 3 risk factors. Main predictors of clustering of risk factors were older age, male gender, and low education.
Conclusions
Syria is currently undergoing a stage, where morbidity and mortality from CVD are high but likely to increase based on the population's risk profile. CVD risk distribution in the Syrian society highlights the non-generalizability of CVD models from developed societies, and calls for local studies to inform effective interventions and policies.
Introduction
Cardiovascular disease (CVD) (coronary heart disease, stroke) is the leading cause of morbidity and mortality worldwide, and is increasing alarmingly in developing countries. Currently, CVD is responsible for about 30% of all deaths worldwide, and is projected to cause 24 million deaths by 2020 (1-3). While the developing world bears most of the burden of these deaths, there are still no signs of success in halting the CVD epidemic there (1-3). Moreover, deaths from CVD in developing countries occur at a younger age compared to developed ones, further hindering their social and economic development (4).
Four out of the 10 leading risk factors to health are related to CVD; hypertension, smoking, high cholesterol levels, and obesity (5). These risk factors explain at least 75% of new cases of coronary heart disease, reflecting in part a population shift in the energy intake-consumption balance (5,6). Cardiovascular risk factors tend to cluster together, leading to multiplication of risks, but also providing an opportunity to reduce multiple risk factors by addressing their common behavioral roots (7,8).
Addressing the epidemic of CVD in developing countries requires acting on the root causes of its risk factors, an approach that is likely feasible across diverse socioeconomic settings (5,7-10). However, many developing countries lack reliable surveillance data regarding the size, composition, and trends in CVD and their risk factors in their societies. Collecting these data is a crucial initial step for planning and monitoring the success of CVD intervention strategies (11). For example, the Eastern Mediterranean Region (EMR) is recognized as a hot spot for CVD, where projections of its burden exceed those of other regions, yet local data to inform health policy is inadequate (12-14). Specifically, as of 2005, the global cardiovascular InfoBase of WHO had no CVD related morbidity and mortality estimates for Syria (15). Therefore, establishing reliable surveillance for CVD and related risk factors seems an essential first step toward devising an action plan to curb the CVD epidemic in the EMR (16,17). This study, based on the Aleppo Household Survey (AHS) conducted in 2004 by the Syrian Center for Tobacco Studies (SCTS), aims to provide the first population estimates of CVD morbidity and mortality in Syria, as well as to characterize the population distribution of CVD and their determinants.
Methods
Population, sampling, procedures
AHS is a population-based survey conducted among a representative sample of households in Aleppo (2nd largest city in Syria with a population of ≈ 2,500,000). AHS aims to characterize major health problems/risks among adults in Syria and is described in details elsewhere (18,19). AHS employed stratified cluster sampling, whereby Aleppo was divided into two strata; formal and informal residential neighborhoods based on the official enumeration of the municipal registry. Informal neighborhoods represent about half of Aleppo's population and were characterized by residences that were built illegally or a land that was not designated for housing. From each stratum, residential neighborhoods were randomly selected with probability proportional to size (PPS). Within each neighborhood, households were selected with equal probability and an adult was randomly selected from each household, giving a total sample of 2038 household representatives age 18-65 years. Informed written consent was obtained from all participants prior to the survey.
Responses to questionnaire items were recorded by mixed gender interviewer teams using notebook computers. The questions used were based on instruments developed internationally (18,19). However, anticipating the literacy level and other issues related to our target population involving many low socio-economic communities, we opted for simple items and have conducted extensive formative work and piloting with members of the target population to better understand their health needs as well as tailor the study instrument and procedures (18-20). In addition to the questionnaire, all study participants underwent objective measurement of height using a sliding wall meter (Seca, Germany), body weight using digital scales (Camry, China, equipped with High Precision Strain-Gauge Sensor), and blood pressure (BP) using digital arm-cuff monitors (ALR K2, Japan, with ±3mmHg accuracy). Two seated BP measurements were made 5 minutes apart, and a third one was taken when the difference between the two was ≥10 mmHg for either systolic or diastolic values. The mean value of BP measurements was used in the analysis eventually.
Outcomes
The prevalence of CVD was assessed based on self-reported physician-diagnosed heart disease (angina, infarction, and heart failure), and stroke of any type (ischemic, hemorrhagic). Annual mortality estimates were calculated based on participant-reported deaths occurring in the past 5 years among their adult (≥ 20 years) household members. When such an event was reported, a verbal autopsy was performed by asking participants to name the main condition leading to that death from the following categories; heart disease, respiratory failure, stroke, cancer, TB, pneumonia, injury, and other. We also inquired about the smoking status of the diseased in the 5-year period prior to their death.
Hypertension was defined as having either systolic pressure >140 mmHg or diastolic pressure > 90 mmHg or reported the use of anti-hypertensive drugs at the time of survey (21). Smoking was defined based on self-reported past month cigarette or waterpipe smoking. BMI was calculated by dividing weight in kg by the square of height in meters, and obesity was defined as having BMI ≥ 30 (22).
Explanatory variables
In addition to demographic variables used in the analysis (Table 1), scores for socioeconomic status (SES), vegetable and fruit consumption, and physical activity (PA) were derived from multiple inquiries, and were categorized for use in the analysis as outlined in Appendix 1.
Table 1.
Basic description of the study's sample (n=2038)
| N (%) | |
|---|---|
| Neighborhood | |
| Non-formal | 1021 (50.1) |
| Formal | 1017 (49.9) |
| Age | |
| 18-29 years | 736 (36.1) |
| 30-45 years | 874 (42.9) |
| 46-65 years | 428 (21.0) |
| Sex | |
| Men | 921 (45.2) |
| Women | 1117 (54.9) |
| Religion | |
| Muslim | 1938 (95.3) |
| Non-Muslim | 95 (4.7) |
| Marital status | |
| Single, divorced, widowed | 494 (24.2) |
| Married | 1544 (75.8) |
| Education | |
| ≤9 years | 1556 (76.3) |
| ≥9 years | 482 (23.7) |
| Work status | |
| Student | 119 (5.8) |
| Employed | 938 (46.0) |
| House-person, retired | 981 (48.1) |
| Socioeconomic status (SES score) | |
| Low | 791 (38.8) |
| Middle | 710 (34.8) |
| High | 537 (26.3) |
Analysis
The survey sample was weighted to account for the complex sampling strategy (e.g. at the city, neighborhood, and household levels). Sampling weights were obtained according to the method described in (23) and reported by our group previously (24). Crude CVD prevalence and mortality rates with the 95% confidence intervals were estimated based on sampling weights using SAS PROC SURVEYMEANS procedure (Table 2). For the calculation of annual death rate among household members ≥ 20 years, the numerator consisted of the number of all reported CVD deaths of household members ≥ 20 years in the past 5 years, while the denominator consisted of the total number of persons ≥ 20 living in these households in the past 5 years plus all reported deaths. Since we did not inquire about the date of death, we assumed a mid point-occurrence (2.5 years) for reported fatalities in order to calculate their contribution to the person-years within the 5-year observation period. Age adjusted annual death rates for the age group 45-74 years (n=1837) were calculated according to the WHO standard world population assuming equal gender distribution (25) to allow for comparison with other populations (26).
Table 2.
Crude and age-adjusted morbidity and mortality rates due to CVD among adults in Aleppo, Syria
| Men | Women | Total | |
|---|---|---|---|
| Morbidity estimates* (N=2038) | % (95% CI) | % (95% CI) | % (95% CI) |
| Prevalence | |||
| Heart disease (n=96) | 6.2 (3.6-10.5) | 3.7 (2.5-5.5) | 4.8 (3.5-6.8) |
| Stroke (n=22) | 0.9 (0.5-1.7) | 1.0 (0.5-2.1) | 1.0 (0.6-1.7%) |
| All (n=108) | 6.5 (3.9-10.7) | 4.6 (3.3-6.5) | 5.4 (4.0-7.3) |
| Mortality estimates** (N=6252) | per 100,000 (95% CI) | per 100,000 (95% CI) | per 100,000 (95% CI) |
| Crude rates | |||
| Heart disease (n=53) | 215 (107-323) | 144 (28-261) | 179 (96-262) |
| Stroke (n=42) | 115 (58-172) | 155 (48-262) | 135 (74-197) |
| All (n=95) | 330 (207-453) | 299 (148-450) | 314 (215-414) |
| Age-adjusted rates† (45-74 years) (N=1837) | |||
| Heart disease | 433 (193-672) | 398 (10-805) | 418 (164-673) |
| Stroke | 246 (78-414) | 424 (19-829) | 322 (130-514) |
| All | 679 (392-966) | 822 (254-1390) | 740 (430-1051) |
based on participants' self-report of physician-diagnosed condition
based on participants' self-report of deaths among their household members ≥20 years in the previous 5 years
adjusted for the WHO world population as a standard and assuming equal gender distribution
Prevalence estimates were computed for major CVD risk factors (hypertension, obesity, smoking), and the chi-square test was used to determine demographic and socio-behavioral correlates of these risk factors (Table 3). Missing values for hypertension, obesity or smoking led to the exclusion of these cases from the analysis (total 74 excluded). Multinomial logistic regression analysis was performed to assess correlates of clustering of CVD risk factors with the 0 risk factor group being the reference. Independent variables entered in the model were; neighborhood (formal, informal), age, sex, religion, marital status, education, work status, SES score, physical activity score, and fruit-vegetable consumption score as shown in Table 3. All analyses were done using SAS (version 8.02)
Table 3.
Prevalence of major CVD risk factors according to different demographic and socioeconomic parameters among adults in Aleppo, Syria (n=2038)
| Hypertension % (n) |
Smoking % (n) |
Obesity % (n) |
|
|---|---|---|---|
| Total | 40.6 (747) | 38.7 (898) | 38.2 (778) |
| Neighborhood | |||
| Non-formal | 40.1 (390) | 37.6 (429) | 37.0 (377) |
| Formal | 41.0 (357) | 39.5 (469) | 39.9 (401) |
| Age | |||
| 18-29 years | 26.8 (176) | 35.7 (278) | 15.8 (119) |
| 30-45 years | 36.7 (304) | 43.2 (445) | 44.7 (392) |
| 46-65 years | 66.3*(267) | 37.3 (175) | 63.2*(267) |
| Sex | |||
| Men | 47.4 (400) | 63.6 (613) | 28.8 (261) |
| Women | 34.9*(347) | 19.2*(285) | 46.4*(517) |
| Religion | |||
| Muslims | 41.2 (711) | 38.2 (844) | 38.7 (743) |
| Non-Muslim | 28.8* (33) | 48.7* (51) | 34.6 (33) |
| Marital status | |||
| Married | 43.8 (591) | 42.3 (719) | 44.5 (679) |
| Single, divorced, widowed | 34.1 (156) | 31.2*(179) | 20.5* (99) |
| Education | |||
| ≤9 yrs | 42.1 (589) | 40.1 (703) | 41.3 (617) |
| >9 yrs | 36.5 (158) | 34.7 (195) | 28.8*(161) |
| Work status | |||
| Student | 18.5 (31) | 20.6 (35) | 10.2 (13) |
| Employed | 45.2 (379) | 58.9 (583) | 30.2 (277) |
| House-person, retired | 39.9* (337) | 22.5* (280) | 50.3* (488) |
| Socioeconomic status (SES score) | |||
| Low | 44.8 (295) | 27.7 (269) | 46.3 (358) |
| Middle | 36.7 (260) | 39.3 (353) | 33.8 (240) |
| High | 41.3 (192) | 47.8*(276) | 34.3*(180) |
| Fruit-vegetable consumption score | |||
| Low | 37.0 (162) | 38.7 (205) | 28.5 (144) |
| Middle | 40.6 (371) | 37.2 (424) | 39.9 (367) |
| High | 43.0 (214) | 40.7 (269) | 41.6 (267) |
| Physical activity score | |||
| Low | 39.6 (256) | 32.8 (288) | 40.6 (306) |
| Middle | 43.1 (403) | 40.8 (475) | 38.9 (392) |
| High | 33.7 (88) | 48.1 (135) | 30.9 (80) |
p<0.05 according to Χ2 test
Results
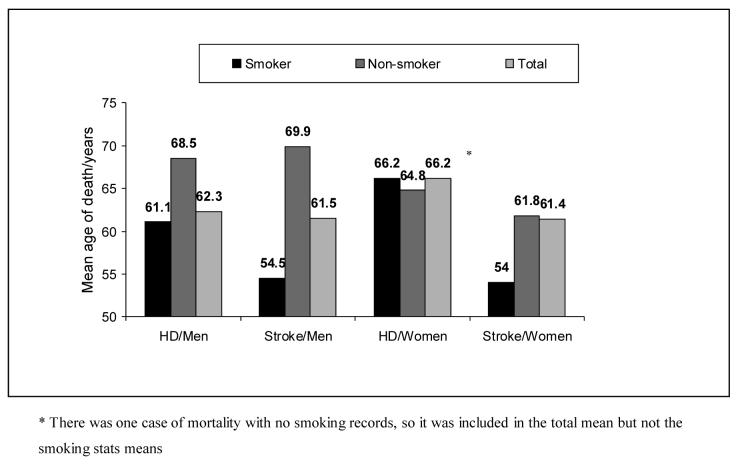
Full socio-demographic characteristics of the study sample are shown in Table 1. The study sample included 2038 household representatives (45.2% men, mean age±SD 35.3±12.1 years, age range 18-65 years, response rate 86%). Prevalence of CVD was 4.8% (95%CI 3.5-6.8) for heart disease, and 1.0% (95%CI 0.6-1.7) for stroke (Table 2). Mortality data were collected on all household members > 20 years (n=6252, 49.5% men), whereby 209 deaths were reported in the past 5 years. Of these deaths, 45.5% (95 cases) were due to CVD, making it the leading cause of mortality in our population. Annual crude death rate due to CVD was 314 per 100,000 (95%CI 215-414), while CVD age-adjusted mortality rate among 45-74 years was 740 per 100,000 (418 for men and 322 for women) (Table 2). Men in general suffered more heart disease mortality, while women suffered more from stroke mortality (Table 2). Mean age of death was 62.6±15.1 years for CVD (63.6±15 years for HD and 61.4±15.3 years for stroke, p>0.05). Generally, smokers' mean age of death was 5 years lower (59.9±15.0 years) than non-smokers' (65±14.2 years), but the difference was not significant, as was the gender-based difference in mean age of HD or stroke, perhaps due to small sample size (Figure 1). About half of CVD deaths (49.0%) in our population occurred before the age of 65 years.
Figure 1.
Mean age of death for household members diseased in the 5 years prior to the survey according to their smoking status during the 5 years leading to their death.
The prevalence of detected hypertension was 40.6%, compared to 11.8% who reported physician-diagnosed hypertension, and 8.6% who were taking antihypertensive treatment at the time of survey. The prevalence of obesity was 38.2%, and the prevalence of smoking (cigarettes or waterpipe) was 38.7%. In men, 51.4% were daily cigarette smokers who consumed on average 20.8±14.0 cig/day. The distribution of these risk factors according to different socioeconomic and behavioral attributes studied is given in (Table 3). The prevalence of clustering of these risk factors was 39.3% for 1 risk factor, 27.4% for 2 risk factors, and 8.3% for 3 risk factors. Only 24.9% of adult participants had none of the three risk factors at the time of survey. According to multinomial logistic regression, older, men, less educated, and those with high consumption of fruits-vegetables were more likely to have clustering of CVD risk factors (Table 4).
Table 4.
Correlates of clustering of CVD risk factors among adults in Aleppo, Syria (n=1958).
| Single risk factor OR (95% CI) |
Two risk factors OR (95% CI) |
Three risk factors OR (95% CI) |
|
|---|---|---|---|
| Neighborhoods | |||
| Non-formal | 0.84 (0.64-1.11) | 1.10 (0.80-1.50) | 0.92 (0.60-1.43) |
| Formal | Ref | Ref | Ref |
| Age | 1.06 (1.04-1.07)* | 1.11 (1.10-1.13)* | 1.11 (1.09-1.13)* |
| Sex | |||
| Men | 3.13 (2.13-4.60)* | 3.79 (2.44-5.90)* | 6.78 (3.58-12.9)* |
| Women | Ref | Ref | Ref |
| Religion | |||
| Muslims | 0.92 (0.50-1.69) | 0.93 (0.49-1.83) | 0.88 (0.35-2.22) |
| Non-Muslim | Ref | Ref | Ref |
| Marital status | |||
| Single, divorced, widowed | 0.93 (0.68-1.28) | 0.96 (0.66-1.40) | 0.62 (0.33-1.14) |
| Married | Ref | Ref | Ref |
| Education | |||
| ≤9 yrs | 1.83 (1.26-2.65)* | 1.83 (1.20-2.78)* | 2.01 (1.14-3.55)* |
| >9 yrs | Ref | Ref | Ref |
| Work status | |||
| Student | 0.74 (0.40-1.40) | 1.24 (0.57-2.66) | 0.37 (0.07-1.94) |
| Employed | 1.03 (0.67-1.58) | 0.76 (0.47-1.23) | 0.57 (0.29-1.12) |
| House-person, retired | Ref | Ref | Ref |
| Socioeconomic status (SES score) | |||
| Low | 1.06 (0.70-1.61) | 1.01 (0.63-1.62) | 0.81 (0.42-1.57) |
| Middle | 0.93 (0.65-1.33) | 0.85 (0.57-1.28) | 1.02 (0.59-1.75) |
| High | Ref | Ref | Ref |
| Fruit-vegetable consumption score | |||
| Low | 0.89 (0.63-1.26) | 0.72 (0.48-1.08) | 0.44 (0.24-0.80)* |
| Middle | 0.93 (0.69-1.25) | 0.86 (0.61-1.21) | 0.79 (0.50-1.24) |
| High | Ref | Ref | Ref |
| Physical activity score | |||
| Low | 0.84 (0.56-1.28) | 1.04 (0.64-1.69) | 0.71 (0.37-1.33) |
| Middle | 0.73 (0.49-1.08) | 0.96 (0.61-1.53)0.54 | (0.30-0.97)* |
| High | Ref | Ref | Ref |
P<0.05 according to multinomial logistic regression with all listed variables included in the model for each OR
Discussion
This study puts Syria on the map for the first time in terms of population-derived estimates of CVD burden and its risk factors in this society. This cross-sectional survey was conducted in Aleppo, which is the second largest city in Syria with population of ≈ 2,500,000. It shows that CVD/risks are the leading cause of morbidity and mortality in the society. The CVD profile in Aleppo is characterized by a predominance of heart disease compared to stroke, and greater morbidity and mortality from heart disease among men compared to women, while the opposite was noticed for stroke. Men, moreover, have worse CVD risk profile, except for obesity, which affected women more in the Syrian society. Cardiovascular risk factors did not show a clear relationship with socioeconomic status among the studied population, but people with low education had worse risk profiles compared to their counterparts. Smokers generally died about 5 years younger than non-smokers.
The mortality toll from CVD in our population accounting for almost half (45%) of all deaths indicates the progress of the cardiovascular epidemic in Syria in comparison to other developing countries (averaging about 25% of all deaths) (27). In neighboring Jordan, CVD is currently responsible for about 35% of overall deaths (28). Compared to more developed countries, age-adjusted CVD mortality estimates of adults 45-74 years in Syria were higher than those reported in societies with notoriously high CVD burden. For example, stroke mortality rate among women in Syria (424 per 100,000) was higher than in the Ukraine (408 per 100,000) (26), signaling the gravity of this health problem among Syrian women. The predominance of CVD morbidity and mortality among men compared to women, with the exclusion of stroke, has been reported in other populations (3,26,28-31). Among Lebanese adults (> 50 years) for example, men have more than double the risk of dying from coronary heart disease compared to women, while women have about 60% increased risk of dying from stroke compared to men (30).
Observed patterns of CVD morbidity and mortality in Syria likely reflect unequal distributions of CVD risk factors. Heavy smoking, for example, is known to be a strong predictor of myocardial infarction mortality (32,33). In our population, men smoke more than women and are predominantly heavy smokers. Obesity on the other hand, is a known risk factor for stroke in women increasing its risk by 50% (34). As expected, age was a major determinant of CVD morbidity and mortality. However, about half of CVD mortality in our population occurred before the age of 65 years compared to only one fifth occurring before the age 70 years in developed countries (35). This is likely due to a combination of earlier onset and inadequate management.
Hypertension, smoking, and obesity were widely spread among adults in Aleppo, affecting about three quarters of adults in the studied population. Hypertension and smoking were more common among men, while obesity was more a problem of women, affecting almost half of them. Hypertension estimates were comparable to those reported from other Arab countries as well as from developed countries affecting about a third of adults (36-38). However, the fact that most hypertension cases in our population were not diagnosed or treated is alarming, and requires attention of health authorities to this major treatable CVD risk factor.
On the other hand, obesity among women has reached epidemic proportions surpassing those reported in other Arab countries, including the affluent societies of the Arabian Peninsula (37,39-43). To grasp the magnitude of this problem, suffice it to compare our findings (46.3% obesity among women) with estimates from other Mediterranean countries, which share many climatic and nutritional patterns with Syria such as Spain (15.2%), Greece (15%), and Turkey (29.4%) (44-46). On the other hand, obesity among women of Arab origin in the US is lower than that reported in Aran countries (47), indicating the importance of the local environments. Obesity among women in Syria is likely rooted in the social norms and gender roles of traditional Arab societies, whereby women are mainly looked at as child bearer-rearers. Confined to their homes, either due to societal traditions or their pressing household duties, women may have little chance for recreational or sport activities (48). Women in our study had generally lower level of reported physical activity than men (data not shown).
Smoking, traditionally a men's problem in Syria and other Arab societies (49), is gaining ground among women too; nearly a quarter of women currently smoke and 11.5% of them are daily smokers. Cigarette smoking among men has reached dramatic proportions, whereby 51.4% of men are daily cigarette smokers consuming on average more than one pack a day. These figures may help to explain the predominance of CVD morbidity and mortality among men, and point to the seriousness of this risk factor in Syria and similar societies in the EMR.
Because clustering of risk factors has a multiplicative effect on CVD morbidity and mortality (32,33), identification of groups with coexisting risk factors can help predict the course of CVD epidemic within the society as well as plan intervention strategies. In our population, only a quarter of adults were free from the assessed CVD risk factors at the time of survey, which is comparable to recent estimates from the United Arab Emirates (50). Expectedly, age and gender were the main determinants of CVD risk factors as well as their clustering, but what was particularly interesting in our results was the role of education. Low educated people in our population had the worst risk profile, mostly due to obesity and hypertension. But unlike patterns noticed in developed countries (15), higher socioeconomic status in our population was not associated with decreased probability of CVD risk factors. Education in our population therefore, seems to be influencing CVD risks through increased access to health information and adoption of healthy lifestyles rather than access to quality health care. Another sharp contrast with data from developed countries (51) is that increased consumption of fruits and vegetables was associated with a trend for increased CVD risk factors in our population. This paradox is likely rooted in the difference between the Syrian and similar Arab societies from industrialized ones. Fruits and vegetables can be widely affordable in Syria, while information about their beneficial effects on cardiovascular health is not widespread in the society. Frequent consumption of these food items in such setting therefore, may reflect more an indulging lifestyle rather that health-oriented behavior (52). This notion is supported by the high rate of obesity among those with high consumption of fruits/vegetables compared to others in our study. The value of fruit/vegetable consumption as a marker for cardiovascular health therefore, may depend on the level of information about cardiovascular health within the society.
Some limitations of this study involve the survey being conducted in one major urban center in Syria, which affects the generalizability of the results to the whole country. The cross sectional design of this study moreover, while optimal for the assessment of the spread of CVD and risk factors, is less though for the assessment of predictors of these health problems. However, given the lack of published standardized data about CVD and their risk factors in Syria and much of the Arab world, our study of a major urban center (Aleppo), including its large informal neighborhoods harboring much of rural immigrants (18,19), provides important insights about the morbidity and mortality of CVD and their risk factors in Syria. The use of self-reports to identify cases of CVD among participants and mortality cases among their households is another limitation of this study. However, because most CVD are symptomatic and deaths due to heart disease or stroke are likely to be recognized by attending physicians, we think that our estimates reflect to a good extent clinically relevant CVD morbidity and mortality in the studied population. Self-reporting also mandated that we applied common terms used by doctors in our population to describe CVD rather than standard definitions.
Applying population-based sampling and objective measures of risk factors, our data from Aleppo suggest that Syria is likely to be undergoing a dynamic stage, where morbidity and mortality from CVD are high but likely to increase further based on the population's risk factors profile. The study highlights the fact that the behavioral basis of CVD, in terms of over-nutrition/under-activity and smoking, are widespread within the Syrian society. Social traditions and gender roles moreover, may be predisposing women in particular to increased risk of obesity by restricting their recreational activities and physical exercise. The lack of a clear socioeconomic gradient in CVD risk factors suggests that the shift from CVD being the problem of the rich to it being the problem of the poor has not yet occurred in the Syrian society. Our data suggests that those with access to information may be able to modify their behavior to avoid CVD. While the debate of what are the optimal solutions to curb the CVD epidemic in developing countries continues (53), having reliable estimates of CVD and their risk factors in the population is the first essential step to being able to mount an adequate response to this escalating epidemic.
Acknowledgement
This work was supported by US Public Health Service grants R01 TW05962 and R21TW006545.
Appendix 1
variables used to construct the socioeconomic status, fruit-vegetable consumption, and physical activity scores.
| value 0 | value 1 | value 2 | |
|---|---|---|---|
| Socioeconomic status score (0-12) | |||
| Education | illiterate | ≤ 9 years | > 9 years |
| Employment | unemployed, student | employed (manual, private, government), retired |
employer, private business |
| Items ownership (phone, mobile phone, PC, AC, private car, TV, satellite dish) |
≤2 | 3-4 | > 4 or private car |
| Household members with paid job | 0 | 1 | > 1 |
| Self reported monthly income | < 10,000 SL | 10,000-20,000 | > 20,000 |
| Density index (household/rooms) | ≥ 2.3 | 1.5-2.3 | < 1.5 |
| Fruit-vegetable consumption score (0-4) | |||
| Frequency of vegetable intake/past month | Little (1-2 times/week) | Frequent, but less than daily | At least once daily |
| Frequency of fruit consumption/past month | Little (1-2 times/week) | Frequent, but less than daily | At least once daily |
| Physical activity score (0-4) | |||
| Regular practice of sports | No | Yes (<3 times/week) | Yes (≥3 times/week) |
| Frequency of >10 minutes walk/past month | None or rarely | 1-2 days/week | 3 or more days/week |
Footnotes
Conflict of interest statement
We declare that we have no conflict of interest related to this study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997;349:1498–504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 3.Reddy KS. Cardiovascular disease in non-western countries. N Eng J Med. 2004;350:2438–40. doi: 10.1056/NEJMp048024. [DOI] [PubMed] [Google Scholar]
- 4.Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular disease. Part I: general considerations, the epidemiologic transition, risk factors and the impact of urbanization. Circulation. 2001;104:2746–2753. doi: 10.1161/hc4601.099487. [DOI] [PubMed] [Google Scholar]
- 5.World health Organization . The world health report 2002: reducing risks, promoting healthy lifestyles. WHO; Geneva: 2003. [DOI] [PubMed] [Google Scholar]
- 6.Canto JG, Iskandrian AE. Major risk factors for cardiovascular disease: debunking the “only 50%” myth. JAMA. 2003;290:947–9. doi: 10.1001/jama.290.7.947. [DOI] [PubMed] [Google Scholar]
- 7.Keil U. Coronary artery disease: the role of lipids, hypertension and smoking. Basic Res Cardiol. 2000;95(Suppl 1):152–8. doi: 10.1007/s003950070010. [DOI] [PubMed] [Google Scholar]
- 8.Assmann G, Carmena R, Cullen P, et al. Coronary heart disease: reducing the risk: a worldwide view. International Task Force for the Prevention of Coronary Heart Disease. Circulation. 1999;100:1930–8. doi: 10.1161/01.cir.100.18.1930. [DOI] [PubMed] [Google Scholar]
- 9.Cheng A, Braunstein JB, Dennison C, et al. Reducing global risk for cardiovascular disease: using lifestyle changes and pharmacotherapy. Clin Cardiol. 2002;25:205–12. doi: 10.1002/clc.4950250503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuulasmaa K, Tunstall-Pedoe H, Dobson A, et al. Estimation of contribution of changes in classic risk factors to trends in coronary-event rates across the WHO MONICA Project populations. Lancet. 2000;355:675–87. doi: 10.1016/s0140-6736(99)11180-2. [DOI] [PubMed] [Google Scholar]
- 11.Beaglehole R, Saracci R, Panico S. Cardiovascular diseases: causes, surveillance and prevention. Int J Epidemiol. 2001;30(Suppl 1):S1–4. doi: 10.1093/ije/30.suppl_1.s1. [DOI] [PubMed] [Google Scholar]
- 12.World health Organization . The world health report 1999: shaping the future. WHO; Geneva: 1999. [Google Scholar]
- 13.Murray CJ, Lopez AD, editors. The Global Burden of Disease: A Comprehensive assessment of mortality and disability from disease, injuries and risk factors in 1990 and projected to 2020. Harvard University Press; Cambridge: 1996. [Google Scholar]
- 14.Alwan AA. Cardiovascular diseases in the eastern Mediterranean region. World Health Stat Q. 1993;46:97–100. [PubMed] [Google Scholar]
- 15.Global Cardiovascular Infobase. Available at: http://www.who.int/topics/cardiovascular_diseases/en/ (accessed May 7, 2005)
- 16.Giampaoli S, Palmieri L, Capocaccia R, et al. Estimating population-based incidence and prevalence of major coronary events. Int J Epidemiol. 2001;30(Suppl 1):S5–10. doi: 10.1093/ije/30.suppl_1.s5. [DOI] [PubMed] [Google Scholar]
- 17.Beaglehole R, Bonita R, Horton R, et al. Public health in the new era: improving health through collective action. Lancet. 2004;363:2084–6. doi: 10.1016/S0140-6736(04)16461-1. [DOI] [PubMed] [Google Scholar]
- 18.Maziak W, Ward KD, Rastam S, et al. Extent of exposure to environmental tobacco smoke (ETS) and its dose-response relation to respiratory health among adults. Respir Res. 2005;6:13. doi: 10.1186/1465-9921-6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maziak W, Ward KD, Mzayek F, et al. Mapping the health and environmental situation in informal zones in Aleppo, Syria: report from the Aleppo household survey. Int Arch Occup Environ Health. 2005;78:547–58. doi: 10.1007/s00420-005-0625-7. [DOI] [PubMed] [Google Scholar]
- 20.Hammal F, Mock J, Ward KD, Fouad MF, Beech BM, Maziak W. Settling with danger: conditions and health problems in peri-urban neighbourhoods in Aleppo, Syria. Environment & Urbanization. 2005;17:113–26. [Google Scholar]
- 21.Maziak W, Keil U, Doring A, Hense HW. Determinants of poor hypertension management in the community. J Hum Hypertens. 2003;17:215–7. doi: 10.1038/sj.jhh.1001535. [DOI] [PubMed] [Google Scholar]
- 22.Bray GA. Definition, measurement and classification of the syndrome of obesity. Int J Obes. 1978;2:99–112. [PubMed] [Google Scholar]
- 23.United Nations Statistics Division: Household Sample Surveys in Developing and Transition Countries. Available www.unstats.un.org/unsdhhsurveys, accessed on 8/22/06.
- 24.Maziak W, Ward KD, Rastam S. Injuries in Aleppo, Syria; first population-based estimates and characterization of predominant types. BMC Public Health. 2006;6:63. doi: 10.1186/1471-2458-6-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJL, Lozano R, Inoue M. Age standardization of rates: a new WHO standard. World Health Organization; (GPE Discussion Paper Series: No.31). Available at: http://whosea.org/healthreport/pdf/paper31.pdf (accessed July 10, 2005) [Google Scholar]
- 26.Sans S, Kesteloot H, Kromhout D. The burden of cardiovascular diseases mortality in Europe. Task Force of the European Society of Cardiology on Cardiovascular Mortality and Morbidity Statistics in Europe. Eur Heart J. 1997;18:1231–48. [PubMed] [Google Scholar]
- 27.Reddy KS, Yusuf S. Emerging epidemic of cardiovascular disease in developing countries. Circulation. 1998;97:596–601. doi: 10.1161/01.cir.97.6.596. [DOI] [PubMed] [Google Scholar]
- 28.Khasawneh NF, Al-Safi S, Albsoul-Younes A, Borqan ON. Clustering of coronary artery disease risk factors in Jordanian hypertensive patients. Saudi Med J. 2005;26:215–9. [PubMed] [Google Scholar]
- 29.Fletcher A. The epidemiology of cardiovascular disease in women. Vascular Med Rev. 1995;313:491–98. [Google Scholar]
- 30.Sibai AM, Fletcher A, Hills M, Campbell O. Non-communicable disease mortality rates using the verbal autopsy in a cohort of middle aged and older populations in Beirut during wartime, 1983-93. J Epidemiol Community Health. 2001;55(4):271–6. doi: 10.1136/jech.55.4.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Al-Nozha MM, Arafah MR, Al-Mazrou YY, et al. Coronary artery disease in Saudi Arabia. Saudi Med J. 2004;25:1165–71. [PubMed] [Google Scholar]
- 32.Keil U, Liese AD, Hense HW, et al. Classical risk factors and their impact on incident non-fatal and fatal myocardial infarction and all-cause mortality in southern Germany. Results from the MONICA Augsburg cohort study 1984-1992. Monitoring Trends and Determinants in Cardiovascular Diseases. Eur Heart J. 1998;19:1197–207. doi: 10.1053/euhj.1998.1089. [DOI] [PubMed] [Google Scholar]
- 33.Njolstad I, Arnesen E. Preinfarction blood pressure and smoking are determinants for a fatal outcome of myocardial infarction: a prospective analysis from the Finnmark Study. Arch Intern Med. 1998;158:1326–32. doi: 10.1001/archinte.158.12.1326. 22. [DOI] [PubMed] [Google Scholar]
- 34.Kurth T, Gaziano JM, Rexrode KM, et al. Prospective study of body mass index and risk of stroke in apparently healthy women. Circulation. 2005;111:1992–8. doi: 10.1161/01.CIR.0000161822.83163.B6. [DOI] [PubMed] [Google Scholar]
- 35.Reddy KS. Cardiovascular diseases in the developing countries: dimensions, determinants, dynamics and directions for public health action. Public Health Nutr. 2002;5(1A):231–7. doi: 10.1079/phn2001298. [DOI] [PubMed] [Google Scholar]
- 36.Bener A, Al-Suwaidi J, Al-Jaber K, et al. The prevalence of hypertension and its associated risk factors in a newly developed country. Saudi Med J. 2004;25:918–22. [PubMed] [Google Scholar]
- 37.Galal OM. The nutrition transition in Egypt: obesity, undernutrition and the food consumption context. Public Health Nutr. 2002;5(1A):141–8. doi: 10.1079/PHN2001286. [DOI] [PubMed] [Google Scholar]
- 38.Wolf -Maier K, Cooper RS, Banegas JR, et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA. 2003;289:2363–9. doi: 10.1001/jama.289.18.2363. [DOI] [PubMed] [Google Scholar]
- 39.Al-Lawati J, Jousilahti P. Prevalence and 10-year secular trend of obesity in Oman. Saudi Med J. 2004;25:346–351. [PubMed] [Google Scholar]
- 40.Musaiger AO, al-Roomi KA. Prevalence of risk factors for cardiovascular diseases among men and women in an Arab Gulf community. Nutr Health. 1997;11:149–57. doi: 10.1177/026010609701100302. [DOI] [PubMed] [Google Scholar]
- 41.Carter AO, Saadi HF, Reed RL, Dunn EV. Assessment of obesity, lifestyle, and reproductive health needs of female citizens of Al Ain, United Arab Emirates. J Health Popul Nutr. 2004;22:75–83. [PubMed] [Google Scholar]
- 42.al-Nuaim AA, Bamgboye EA, al-Rubeaan KA, al-Mazrou Y. Overweight and obesity in Saudi Arabian adult population, role of socio-demographic variables. J Community Health. 1997;22:211–23. doi: 10.1023/a:1025177108996. [DOI] [PubMed] [Google Scholar]
- 43.el Mugamer IT, Ali Zayat AS, Hossain MM, Pugh RN. Diabetes, obesity and hypertension in urban and rural people of bedouin origin in the United Arab Emirates. J Trop Med Hyg. 1995;98:407–15. [PubMed] [Google Scholar]
- 44.Aranceta Bartrina J. Prevalence of obesity in developed countries: current status and perspectives. Nutr Hosp. 2002;17(Suppl 1):34–41. [PubMed] [Google Scholar]
- 45.Erem C, Arslan C, Hacihasanoglu A, et al. Prevalence of obesity and associated risk factors in a Turkish population (trabzon city, Turkey) Obes Res. 2004;12:1117–27. doi: 10.1038/oby.2004.140. [DOI] [PubMed] [Google Scholar]
- 46.Pitsavos C, Panagiotakos DB, Chrysohoou C, Stefanadis C. Epidemiology of cardiovascular risk factors in Greece: aims, design and baseline characteristics of the ATTICA study. BMC Public Health. 2003;3:32. doi: 10.1186/1471-2458-3-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hatahet W, Khosla P, Fungwe TV. Prevalence of risk factors to coronary heart disease in an Arab-American population in southeast Michigan. Int J Food Sci Nutr. 2002;53:325–35. doi: 10.1080/09637480220138124. [DOI] [PubMed] [Google Scholar]
- 48.Maziak W. Health in the Middle East. BMJ. 2006;333(7573):815–6. doi: 10.1136/bmj.39006.478796.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Maziak W. Smoking in Syria: profile of a developing Arab country. Int J Tuberc Lung Dis. 2002;6:183–91. [PubMed] [Google Scholar]
- 50.Malik M, Bakir A, Saab BA, Roglic G, King H. Glucose intolerance and associated factors in the multi-ethnic population of the United Arab Emirates: results of a national survey. Diabetes Res Clin Pract. 2005;69:188–95. doi: 10.1016/j.diabres.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 51.Lock K, Pomerleau J, Causer L, et al. The global burden of disease attributable to low consumption of fruit and vegetables: implications for the global strategy on diet. Bull WHO. 2005;83:100–8. [PMC free article] [PubMed] [Google Scholar]
- 52.Fouad MF, Rastam S, Ward KD, Maziak W. Prevalence of obesity and its associated factors in Aleppo, Syria. Prevention & Control. 2006;2:85–94. doi: 10.1016/j.precon.2006.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ebrahim S, Smith GD. Exporting failure? Coronary heart disease and stroke in developing countries. Int J Epidemiol. 2001;30:201–5. doi: 10.1093/ije/30.2.201. [DOI] [PubMed] [Google Scholar]