Hyperbaric oxygen (HBO) has been reported as an adjunctive treatment for various corneal conditions.1,2 We report a case of contact‐lens associated Pseudomonas keratitis which we treated adjunctively with hyperbaric oxygen.
Case report
A 30‐year‐old female presented with pain and progressive blurring in the left eye. She was wearing daily disposable contact lenses when she was splashed with muddy water in the face whilst mountain‐biking.
Left visual acuity on presentation was 6/12. A 4 mm × 4 mm superior corneal ulcer with underlying infiltrate was noted. Corneal scrapings were obtained before commencing hourly topical gentamicin 0.9% and cephalothin 5%. A heavy growth of Pseudomonas aeruginosa sensitive to ceftazidime, gentamicin, ciprofloxacin, imipenem, piperacillin, ticarcillin and tobramycin was cultured.
On the second day of admission, visual acuity deteriorated to count fingers with increased corneal infiltrate and oedema. Topical ciprofloxacin and tobramycin in addition to oral moxifloxacin and intravenous ticarcillin were added while topical gentamicin was ceased.
On the third day, there was no improvement so we commenced daily adjuvant hyperbaric treatment. This consisted of 90 minutes at 2.0 atmospheres absolute pressure (2 ATA) breathing 100% oxygen in a monoplace chamber (Vickers Medical, Sidcup, UK). Twenty‐four hours later, visual acuity improved from count fingers to 6/24. Cephalothin and intravenous ticarcillin were ceased over the next two days. On the sixth day, visual acuity improved to 6/9 and hyperbaric therapy was ceased.
Topical antibiotics were continued for a total of 6 weeks at which point her visual acuity recovered to 6/6. There was mild scarring and thinning superiorly but she reported her vision was essentially normal.
Comment
Pseudomonas keratitis is a well documented complication of soft contact lens wear3 and is associated with poor outcomes including loss of the eye.4 In view of its virulence and the rapid clinical progression we decided to use HBO.
Well established as adjuvant treatment in certain bacterial infections5 HBO restores normoxia to hypoxic tissues or establishes hyperoxia in normoxic tissues. In vitro and in vivo animal experiments show HBO to be efficacious against Pseudomonas aeruginosa.6,7 Pharmacologically, HBO also prolongs the post‐antibiotic effect of tobramycin against Pseudomonas aeruginosa.8
HBO is known to be effective in treating Pseudomonas aeruginosa in malignant otitis externa in humans.9 However, we are aware of only two reports describing the use of HBO in human corneal pathology. One is from the French literature in 1970 but further details are not available to us.1 The other was a report of 32 patients with corneal disorders including “keratitis, traumatic injuries & ulcerations” treated with hyperbaric oxygen. The rationale was that “tissue oedema, hypoxia and ischaemia in these conditions are improved by hyperoxygenation” and it was found to be “beneficial in most of these cases”.2
The optimal dose of oxygen is unknown. In vitro studies suggest at least 1.6 ATA oxygen6 is required for efficacy against Pseudomonas aeruginosa and in vivo studies showed efficacy at 2.0 ATA.7 Higher oxygen concentrations may be used but this is limited to 3.0 ATA by systemic toxicity.10 Intermittent therapy also limits oxygen toxicity10 and improves bacterial clearance in vitro and in vivo compared with continuous exposure.6 The treatment protocol in our case was that used locally for osteomyelitis. Given that the cornea gains most of its oxygen supply via direct diffusion from the atmosphere, we used a monoplace or hood system that delivers oxygen both systemically and directly to the cornea.
Hyperbaric oxygen treatment is safe, has few contraindications and may have accelerated recovery in this case. Further studies are needed to establish the clinical efficacy of adjunctive hyperbaric oxygen in bacterial keratitis.
Figure 1 Left cornea two weeks after infection.
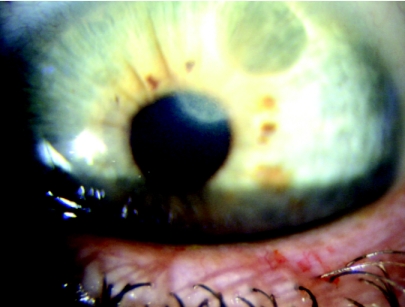
Figure 2 Left cornea six weeks after infection.
Footnotes
Informed consent was obtained for publication of the person's details in this report.
References
- 1.Saracco J B. Hyperbaric oxygentherapy and corneal pathology. [French] Annee Therapeutique et Clinique en Ophtalmologie 19702111–20. [PubMed] [Google Scholar]
- 2.Jain K K. Hyperbaric oxygen and ophthalmology. In: Textbook of Hyperbaric Medicine. Seattle: Hogrefe & Huber, 1999505–517.
- 3.Bourcier T, Thomas F, Borderie V.et al Bacterial keratitis: predisposing factors, clinical and microbiological review of 300 cases. Br J Ophthalmol 200487834–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cruz C S, Cohen E J, Rapuano C J. Microbial keratitis resulting in loss of the eye. Ophthalmic Surg Lasers 199829803–807. [PubMed] [Google Scholar]
- 5.Hampson N B, Bakker D J, Camporesi E M.et al Undersea & Hyperbaric Medical Society Approved Indications for Hyperbaric Oxygen Therapy. www.uhms.org/Indications/indications.htm
- 6.Park M K, Muhvich K H, Myers R A M.et al Effects of Hyperbaric Oxygen in Infectious Diseases: Basic Mechanisms. In: Hyperbaric Medicine Practice. Flagstaff, Arizona: Best Publishing Co, 1994141–172.
- 7.Luongo C, Imperatore F, Matera G.et al Effect of hyperbaric oxygen therapy in experimental subcutaneous and pulmonary infections due to Pseudomonas aeruginosa. Undersea and Hyperbaric Medical Society 19992621–25. [PubMed] [Google Scholar]
- 8.Park M K, Muhvich K H, Myers R A.et al Hyperoxia prolongs the aminoglycoside‐induced postantibiotic effect in Pseudomonas aeruginosa. Antimicrobial Agents and Chemotherapy 199135691–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martel J, Duclos J Y, Darrouzet V.et al [Malignant or necrotizing otitis externa: experience in 22 cases. ] [French] Annales d Oto‐Laryngologie et de Chirurgie Cervico‐Faciale 2000117291. [PubMed] [Google Scholar]
- 10.Hammarlund C. The physiological effects of hyperbaric oxygen. In: Hyperbaric Medicine Practice. Flagstaff, Arizona: Best Publishing Co, 199417–32.