Abstract
Background
Genetic factors and oxidative damage have been shown to have a role in the development of primary open angle glaucoma (POAG).
Aim
To determine the effects of genetic polymorphisms of glutathione S transferase (GST)M1 and GSTT1 on the risk of POAG in a Turkish population.
Methods
Using a multiplex polymerase chain reaction (PCR), GSTM1 and GSTT1 gene polymorphisms were analysed in 144 patients with POAG and in 121 otherwise healthy controls of similar age.
Results
The GSTM1 positive genotype and the GSTT1 null genotype had an increased risk of developing POAG (p<0.001, OR 2.93, 95% CI 1.66 to 5.20 and OR 4.25, 95% CI 2.30 to 7.80, respectively). The risk of glaucoma also increased significantly in subjects with a combination of GSTM1 positive and GSTT1 null genotypes (p<0.001, OR 3.46, 95% CI 1.64 to 7.38).
Conclusion
The GSTM1 positive genotype and GSTT1 null genotype or the combination of both may be associated with the increased risk of development of POAG in the Turkish population.
Primary open angle glaucoma (POAG) is the most common form of glaucoma. POAG is a complex chronic‐degenerative disease having a multifactorial aetiology including mechanical damage due to increased intraocular pressure (IOP), increased glutamate levels, mutations in specific genes, toxic effects and oxidative damage caused by reactive oxygen species (ROS). The pathogenic role of ROS in glaucoma is supported by various experimental findings. ROS‐mediated oxidative DNA damage has also been shown to be significantly increased in the trabecular meshwork of patients with glaucoma compared with controls. Oxidative stress also seems to be involved in the neuronal cell death affecting the optic nerve in POAG.1,2,3,4
Glutathione S transferases (GSTs) represent an important family of phase II drug metabolising enzymes. Besides detoxifying exogenous electrophilic xenobiotics, these transferases inactivate endogenous end products formed as secondary metabolites during oxidative stress.5,6,7,8
The GST isoenzymes expressed in human tissues comprise the alpha, mu, pi, theta, kappa, sigma, zeta and omega gene families.9 As many GST genes are polymorphic, there has been considerable interest in determining whether particular allelic variants are associated with altered risk (or outcome) of a variety of pathologies including cancers, cardiovascular diseases and respiratory diseases.5,6
Of these classes of GSTs, five (GSTM1, GSTM3, GSTT1, GSTP1 and GSTZ1) have been shown to be polymorphically distributed.10 Five mu‐class genes (GSTM1–GSTM5) are situated on chromosome 1.11 Polymorphisms identified in GSTM1 are GSTM1*0, GSTM1*A and GSTM1*B. GSTM1*0 is deleted, and homozygotes (GSTM1 null genotype) express no protein. GSTM1*A and GSTM1*B differ by a single base, and the catalytic effectiveness of the enzymes encoded by these alleles is similar. There are two theta‐class genes, GSTT1 and GSTT2, located on chromosome 22.6 GSTT1 is represented by two alleles: a functional or wild allele (GSTT1*1), and a non‐functional or null allele (GSTT1*0). Studies have shown that the GSTT1*0 allele corresponds to a total or partial deletion of the gene, causing a deficiency in enzymatic activity.12
In the current study, we investigated the distribution of the GSTM1 and GSTT1 polymorphisms in patients with POAG and controls to explore the possible association between different GST variants and the incidence of POAG.
Materials and methods
Patients and controls
This case–control study comprised 144 patients with POAG and 121 disease‐free controls. All were from Turkey. All subjects selected were non‐smokers and did not have diabetes mellitus or other systemic diseases. Informed consent was obtained from all subjects after explanation of the nature of the study.
Each subject underwent a complete ophthalmological examination. Patients with POAG were defined by the presence of an open angle, pathological cupping of the optic disc, a glaucoma hemifield test (GHT) outside normal limits with reproducible visual field defects at the same location on two consecutive visits, and an IOP >21 mm Hg without anti‐glaucoma drugs. The mean IOP level was 23.9 (1.2) mm Hg (range 22–29 mm Hg) at the time of diagnosis. Cup‐to‐disc ratios were between 0.4 and 0.9. Patients with a history of eye surgery before the diagnosis of glaucoma, or with evidence of secondary glaucoma, such as exfoliation, pigment dispersion or uveitis, were excluded. The patients with POAG who met the inclusion criteria were selected consecutively at the İstanbul University Cerrahpasa Medical Faculty Ophthalmology Department. The mean age of patients in the glaucoma group was 61.3 (6.9) years (range 48–79 years), and 70 (49%) of them were men.
Age‐matched healthy volunteers presenting to our outpatient department with non‐specific ocular complaints, such as conjunctivitis, blepharitis, burning, itching or presbyopia were selected randomly as a control group. They had clinically healthy appearing optic discs as shown by indirect ophthalmoscopy, with a cup‐to‐disc ratio of ⩽0.3 and GHT within normal limits. They also lived in the same city and had no family or personal history of glaucoma. The mean IOP level of the controls was 14.3 (2.3) mm Hg (range 8–20 mmHg). The mean age of subjects in the control group was 59.1 (5.8) years (range 51–75 years), and 66 (55%) of them were men.
Blood samples and DNA isolation
Venous blood samples were obtained and collected into sterile siliconised EDTA 5‐ml vacutainer tubes. Immediately after collection, whole blood was stored in aliquots at −20°C until use. Genomic DNA was extracted from whole blood using a NucleoSpin DNA purification kit (Macherey–Nagel GmbH, Duren, Germany) according to the manufacturer's instructions.
Analysis of GSTM1 and GSTT1 polymorphisms
The GSTM1 and GSTT1 genetic polymorphisms were evaluated using the multiplex polymerase chain reaction (PCR) technique as described previously.13 Primers for GSTM1 were 5′‐GAACTCCCTGAAAAGCTAAAGC‐3′ and 5′‐GTTGGGCTCAAATATACGGTGG‐3′, and those for GSTT1 were 5′‐TTCCTTACTGGTCCTCACATCTC‐3′ and 5′‐TCACCGGATCATGGCCAGCA‐3′. The β‐globin locus was used as an internal control to avoid false negative readings. Primers for β‐globin were 5′‐CAACTTCATCCACGTTCACC‐3′ and 5′‐GAAGAGCCAAGGACAGGTAC‐3′.
PCR was carried out in a total volume of 25 μl containing 10 pmol/l of each primer, 2.5 mmol/l of magnesium chloride, 0.2 mmol/l of each deoxynucleotide triphosphate, 1 U of Taq polymerase and 100 ng of genomic DNA. Amplification was performed with initial denaturation at 94°C for 5 min, followed by 30 cycles at 94°C for 1 min, 64°C for 1 min and 72°C for 1 min, and a final extension at 72°C for 7 min.
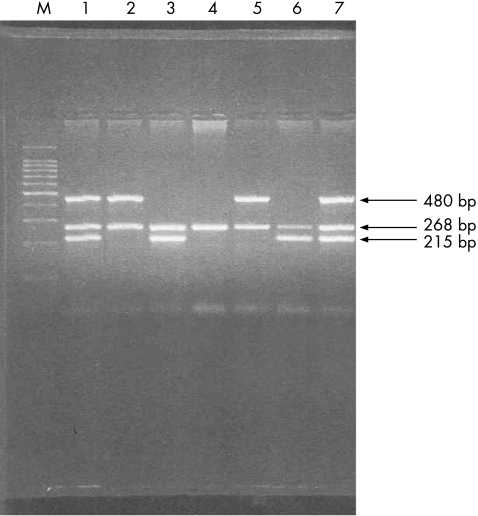
The amplified products were identified by electrophoresis in a 1.5% agarose gel and stained with 0.5 μg/ml ethidium bromide. The product lengths were 215, 480, and 268 bp for GSTM1, GSTT1 and β‐globin, respectively (fig 1). The absence of PCR product for GSTM1 or GSTT1 in the presence of the β‐globin band was indicative of a null genotype for GSTM1 or GSTT1. Individuals with one or two copies of the relevant gene were classified as a “present” genotype and those with homozygous deletions as a “null” genotype.
Figure 1 Polymerase chain reaction (PCR) analysis of glutathione S transferase (GST) gene polymorphism. The line with 480 bp stands for GSTT1, 268 bp for β globin and 215 bp for GSTM1. Column M represents a PCR weight marker, columns 1 and 7 GSTT1 positive/GSTM1 positive, columns 2 and 5 GSTT1 positive/GSTM1 null, columns 3 and 6 GSTT1 null/GSTM1 positive and column 4 GSTT1 null/GSTM1 null.
Statistical analysis
The ages of the patient and control groups were compared using Student's t test. The χ2 test was applied to compare differences in sex and GSTM1 and GSTT1 polymorphisms between patients and controls. Significance was set at p<0.05. Odd ratios (OR) and 95% confidence intervals (CI) were used to analyse the occurrence of frequencies of the GSTM1 and GSTT1 genotypes in patients with glaucoma compared with the controls group. All analyses were performed using SPSS V.11.5 statistical analysis software.
Results
Table 1 shows the demographic data of the patients. The groups were not significantly different with respect to age and sex (p>0.05).
Table 1 Demographic data of the study patients.
| Glaucoma group (n = 144) | Control group (n = 121) | |
|---|---|---|
| Number of patients | 144 | 121 |
| Sex | ||
| Male, n (%) | 70 (49) | 66 (55) |
| Female, n (%) | 74 (51) | 55 (45) |
| Age (years) | ||
| Mean (SD) | 61.3 (6.9) | 59.1 (5.8) |
| Range | 48–79 | 51–75 |
Table 2 shows the genotypes for each gene. The frequency of the GSTM1 positive genotype was significantly higher in patients with glaucoma (78.5%) than in controls (55%). The GSTM1 positive genotype had an increased risk of developing POAG (p<0.001, OR 2.93, 95% CI 1.66 to 5.20).
Table 2 Glutathione S transferase genotypes and the risk of developing primary open‐angle glaucoma.
| Genotype | Patients with glaucoma (n = 144) n (%) | Controls (n = 121) n (%) | OR (95% CI) |
|---|---|---|---|
| GSTM1 | |||
| Present | 113 (78.5) | 67 (55) | 1.00 (Reference) |
| Null | 31 (21.5) | 54 (45) | 2.93 (1.66 to 5.20) |
| GSTT1 | |||
| Present | 74 (51.3) | 99 (81.8) | 1.00 (Reference*) |
| Null | 70 (48.7) | 22 (18.2) | 4.25 (2.33 to 7.81) |
GST, glutathione S transferase.
*Carriers of at least one intact allele.
The frequency of the GSTT1 null genotype was significantly higher in patients with glaucoma (48.7%) than in controls (18.2%). The GSTT1 null genotype also had an increased risk of developing POAG (p<0.001, OR 4.25, 95% CI 2.30 to 7.80).
Table 3 shows the association between GST genotype profile and the development of POAG. The risk of glaucoma also increased statistically significantly in patients with a combination of GSTM1 positive and GSTT1 null genotypes (p<0.005, OR 3.46, 95% CI 1.64 to 7.38).
Table 3 Association between glutathione S transferase genotype profile and the development of primary open angle‐glaucoma.
| GSTM1 | GSTT1 | Patients with glaucoma n (%) | Controls n (%) | OR (95% CI) |
|---|---|---|---|---|
| Present | Present | 59 (40.9%) | 53 (43.8%) | 1 (Reference)* |
| Present | Null | 54 (37.5%) | 14 (11.5%) | 3.46 (1.64 to 7.38) |
| Null | Present | 15 (10.5%) | 46 (38.0%) | 0.29 (0.13 to 0.61) |
| Null | Null | 16 (11.1%) | 8 (6.7%) | 0.55 (0.20 to 1.52) |
GST, glutathione S transferase.
*Reference group; individuals with two putative low‐risk genotypes (the presence of GSTM1 (non‐deleted) and GSTT1 (non‐deleted)).
Discussion
Most genetic polymorphisms do not cause a recognisable change in the organism in which they occur. However, some either cause a disease or alter disease susceptibility.14 A large number of studies has attempted to show links between disease susceptibility and GST polymorphic variants. In addition, some studies have focused on the risk of association between the GST polymorphisms and ocular diseases including cataract,15,16,17,18 senile macular degeneration19 and glaucoma.3,10,20,21,22 In this study, we determined the effects of genetic polymorphisms of GSTM1 and GSTT1 on the risk of POAG in a Turkish population.
As the pathogenic role of ROS in glaucoma has been suggested by many studies, cellular defence mechanisms alleviating the toxic manifestations of oxidative insult must have an important role in protection against the development of glaucoma. As GST enzymes are one of the important families of enzymes against oxidative stress, their genetic polymorphisms may alter the critical function of the enzymes in protecting against electrophiles and the products of oxidative stress in glaucoma.
Izzotti et al3 reported that POAG was associated with the GSTM1 null genotype in an Italian population. In addition, in a recent study, the GSTM1 null genotype has been found to be associated with an increased incidence of POAG in a Turkish population.21 In contrast, another study by Jansson et al22 reported that there was no evidence of association between GSTM1 polymorphism and glaucoma in the Swedish population.
In this study, we found that the GSTM1 positive genotype was a risk factor for developing POAG. Juronen et al,10 who were the first to examine the possible association between the polymorphic GST genotypes and adult‐onset POAG, also found a similar relationship between the GSTM1 genotype and the incidence of POAG. They found that the frequency of GSTM1 positive individuals was significantly higher in the glaucoma group compared with the control group. They suggested that the GSTM1 positive phenotype might be a genetic risk factor for the development of POAG. Our results also show a correlation between the GSTM1 positive genotype and the incidence of POAG.
We believe that several factors might explain the association between the GSTM1 positive genotype and POAG. Although GST enzymes catalyse detoxification reactions, they also take part in reactions that result in toxic products, which may cause structural changes in the proteins present in the trabecular meshwork and aqueous humor. This can lead to aggregation or modification of the proteins in the trabecular meshwork and promote the development of POAG.10 In addition, subjects with the GSTM1 null genotype have been shown to express fewer GST mu‐class enzymes than subjects with the GSTM1 positive genotype.23,24 This may selectively cause stimulation of other non‐toxic end products producing biotransformation enzyme systems to detoxify the substrates that were originally detoxified by the GST enzymes.
Further evidence for involvement of GSTM in glaucoma comes from studies on autoimmunity. Yang et al showed that GST antigen was found in 52% of cases with glaucoma and in 20% of controls (p<0.05). The patients had significantly higher titres of anti‐GST antibody compared with controls. Furthermore, the related retinal antigen belonged to the GST mu class.25 Thus, it may be hypothesised that people who express GSTM1 are at increased risk of developing autoantibodies against this protein, which is connected to an increased risk of developing glaucoma. Interestingly, in this study, we also found that although the frequency of the GSTM1 positive genotype in the control group was similar to the other Caucasian populations of Europe,10,22,26 it was significantly higher in subjects with glaucoma.
The GSTT1 null genotype was also reported in some studies to be associated with an increased tendency for some diseases including cancers and precancerous lesions.5,27,28 Our study is the first to report a significant association between the GSTT1 null genotype and POAG. Previous studies on the association between the GSTT1 genotype and POAG did not find a significant relationship. As discussed earlier, as well as detoxifying exogenous electrophilic xenobiotics, GST enzymes including GSTT1 inactivate endogenous end products formed as secondary metabolites during oxidative stress. They are protective against many toxicants, and it may be important to reach a proper balance between the detrimental and beneficial effects of the enzyme. Altered GST activity due to genetic mutations has been shown to modulate an individual's susceptibility to environmental factor‐induced diseases, including cancers.7,29
The present study suggests that the GSTM1 positive genotype and GSTT1 null genotype may be genetic risk factors for development of POAG. Any combination of these two genotypes further increases the risk of POAG. It has already been suggested that the combination of the GST polymorphisms rather than individual polymorphisms makes humans more susceptible to genotoxic insults.26,29
Many factors might account for the difference in results between similar studies. Firstly, it may reflect the differences in the ethnic, genetic and environmental background of the populations studied. For instance, GSTT1 deficiency is less frequent than GSTM1 deficiency, but in both cases the frequency in the population varies between different ethnic groups.30 There may be differences even in the same population because of genetic and environmental factors. Studies on the Turkish population showed that the percentage of GSTM1 null genotype ranged from 16% to 51.9%, and that of GSTT1 null genotype between 17.3% and 20%.26 This may be one of the factors responsible for the different results in the study by Yıldırım et al,21 reporting that the GSTM1 null genotype was associated with an increased incidence of POAG in Turkish population. Whereas their study population lived in a small and closed city in the south of Turkey, our patients and controls were from a crowded and cosmopolitan city, which has a high number of migrants from other cities of Turkey. Thus, the subjects in our study may reflect more accurately the genetic status of the whole Turkish population.
Secondly, the differences in the number of subjects studied in genetic researches may also lead to different outcomes. Thirdly, methodological issues should also be considered. For example, Jansson et al,22 who reported that there was no evidence of association between GSTM1 and glaucoma in the Swedish population, used two methods for genotyping: multiplex PCR and pyrosequencing. In contrast, Juronen et al performed their analysis using only ELISA.10 The GST genes are located in complex genomic regions that could be affected by copy number variation and rearrangements, so different genotyping methods could give different results.
In conclusion, this study is only one in a series of case–control studies on the possible association between glaucoma and GST. Some found evidence of GST positive genotypes being predisposed to glaucoma, and others that GST positive genotypes are protected from glaucoma. These results imply that further studies of the precise mechanisms by which genetic polymorphisms of metabolising enzymes influence the nature and history of glaucoma development are merited.
Abbreviations
GHT - glaucoma hemifield test
GST - glutathione S transferase
IOP - intraocular pressure
PCR - polymerase chain reaction
POAG - primary open‐angle glaucoma
ROS - reactive oxygen species
Footnotes
Competing interests: None declared.
References
- 1.Izzotti A, Bagnis A, Sacca S C. The role of oxidative stress in glaucoma. Mutat Res 2006612105–114. [DOI] [PubMed] [Google Scholar]
- 2.Izzotti A, Di Marco B, De Flora S.et al Open angle glaucoma: epidemiology, pathogenesis and prevention. Recent Prog Med 20069737–45. [PubMed] [Google Scholar]
- 3.Izzotti A, Sacca S C, Cartiglia C.et al Oxidative deoxyribonucleic acid damage in the eyes of glaucoma patients. Am J Med 2003114638–646. [DOI] [PubMed] [Google Scholar]
- 4.Moreno M C, Campanelli J, Sande P.et al Retinal oxidative stress induced by high intraocular pressure. Free Radic Biol Med 200437803–812. [DOI] [PubMed] [Google Scholar]
- 5.Habdous M, Siest G, Herbeth B.et al Glutathione S‐transferases genetic polymorphisms and human diseases: overview of epidemiological studies. Ann Biol Clin (Paris) 20046215–24. [PubMed] [Google Scholar]
- 6.Strange R C, Spiteri M A, Ramachandran S.et al Glutathione‐S‐transferase family of enzymes. Mutat Res 200148221–26. [DOI] [PubMed] [Google Scholar]
- 7.Zhong S L, Zhou S F, Chen X.et al Relationship between genotype and enzyme activity of glutathione S‐transferases M1 and P1 in Chinese. Eur J Pharm Sci 20062877–85. [DOI] [PubMed] [Google Scholar]
- 8.Hayes J D, Flanagan J U, Jowsey I R. Glutathione transferases. Annu Rev Pharmacol Toxicol 20054551–88. [DOI] [PubMed] [Google Scholar]
- 9.Board P G, Baker R T, Chelvanayagam G.et al Zeta, a novel class of glutathione transferases in a range of species from plants to humans. Biochem J 1997328929–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Juronen E, Tasa G, Veromann S.et al Polymorphic glutathione S‐transferase M1 is a risk factor of primary open‐angle glaucoma among Estonians. Exp Eye Res 200071447–452. [DOI] [PubMed] [Google Scholar]
- 11.Xu S, Wang Y, Roe B.et al Characterization of the human class Mu glutathione S‐transferase gene cluster and the GSTM1 deletion. J Biol Chem 19982733517–3527. [DOI] [PubMed] [Google Scholar]
- 12.Pemble S, Schroeder K R, Spencer S R.et al Human glutathione S‐transferase theta (GSTT1): cDNA cloning and the characterization of a genetic polymorphism. Biochem J 1994300271–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arand M, Muhlbauer R, Hengstler J.et al A multiplex polymerase chain reaction protocol for the simultaneous analysis of the glutathione S‐transferase GSTM1 and GSTT1 polymorphisms. Anal Biochem 1996236184–186. [DOI] [PubMed] [Google Scholar]
- 14.Cohen C S, Allingham R R. The dawn of genetic testing for glaucoma. Curr Opin Ophthalmol 20041575–79. [DOI] [PubMed] [Google Scholar]
- 15.Saadat M, Farvardin‐Jahromi M. Occupational sunlight exposure, polymorphism of glutathione S‐transferase M1, and senile cataract risk. Occup Environ Med 200663503–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alberti G, Oguni M, Podgor M.et al Glutathione S‐transferase M1 genotype and age‐related cataracts. Lack of association in an Italian population. Invest Ophthalmol Vis Sci 1996371167–1173. [PubMed] [Google Scholar]
- 17.Hao Y, He S, Gu Z.et al Relationship between GSTM1 genotype and susceptibility to senile cataract. Zhonghua Yan Ke Za Zhi 199935104–106. [PubMed] [Google Scholar]
- 18.Sekine Y, Hommura S, Harada S. Frequency of glutathione‐S‐transferase 1 gene deletion and its possible correlation with cataract formation. Exp Eye Res 199560159–163. [DOI] [PubMed] [Google Scholar]
- 19.Oz O, Aras Ates N, Tamer L.et al Glutathione S‐transferase M1, T1, and P1 gene polymorphism in exudative age‐related macular degeneration: a preliminary report. Eur J Ophthalmol 200616105–110. [DOI] [PubMed] [Google Scholar]
- 20.Yilmaz A, Tamer L, Ates N A.et al Is GST gene polymorphism a risk factor in developing exfoliation syndrome? Curr Eye Res 200530575–581. [DOI] [PubMed] [Google Scholar]
- 21.Yildirim O, Ates N A, Tamer L.et al May glutathione S‐transferase M1 positive genotype afford protection against primary open‐angle glaucoma? Graefe's Arch Clin Exp Ophthalmol 2005243327–333. [DOI] [PubMed] [Google Scholar]
- 22.Jansson M, Rada A, Tomic L.et al Analysis of the glutathione S‐transferase M1 gene using pyrosequencing and multiplex PCR—no evidence of association to glaucoma. Exp Eye Res 200377239–243. [DOI] [PubMed] [Google Scholar]
- 23.Anttila S, Luostarinen L, Hirvonen A.et al Pulmonary expression of glutathione S‐transferase M3 in lung cancer patients: association with GSTM1 polymorphism, smoking, and asbestos exposure. Cancer Res 1995553305–3309. [PubMed] [Google Scholar]
- 24.Nakajima T, Elovaara E, Anttila S.et al Expression and polymorphism of glutathione S‐transferase in human lungs: risk factors in smoking‐related lung cancer. Carcinogenesis 199516707–711. [DOI] [PubMed] [Google Scholar]
- 25.Yang J, Tezel G, Patil R V.et al Serum autoantibody against glutathione S‐transferase in patients with glaucoma. Invest Ophthalmol Vis Sci 2001421273–1276. [PubMed] [Google Scholar]
- 26.Ada A O, Suzen S H, Iscan M. Polymorphisms of cytochrome P450 1A1, glutathione S‐transferases M1 and T1 in a Turkish population. Toxicol Lett 2004151311–315. [DOI] [PubMed] [Google Scholar]
- 27.Barroso Duarte E C, Da Silva M S, Gomez M V.et al GSTT1 polymorphism and oral leukoplakia. Anticancer Res 200626427–430. [PubMed] [Google Scholar]
- 28.Boccia S, La Torre G, Gianfagna F.et al Glutathione S‐transferase T1 status and gastric cancer risk: a meta‐analysis of the literature. Mutagenesis 200621115–123. [DOI] [PubMed] [Google Scholar]
- 29.Tars K, Larsson A K, Shokeer A.et al Structural basis of the suppressed catalytic activity of wild‐type human glutathione transferase T1‐1 compared to its W234R mutant. J Mol Biol 200635596–105. [DOI] [PubMed] [Google Scholar]
- 30.Johansson A S, Mannervik B. Interindividual variability of glutathione transferase expression. In: Pacifici GM, Pelkonen O, eds. Interindividual variability of glutathione transferase expression. London: Taylor & Francis, 2001460–519.