Abstract
To test cognitive models of panic disorder, a range of information processing biases were examined among persons with panic disorder (N=43) and healthy control participants (N=38). Evidence for automatic associations in memory was assessed using the Implicit Association Test, interference effects related to attention biases were assessed using a modified supraliminal Stroop task, and interpretation biases were assessed using the Brief Body Sensations Interpretation Questionnaire. In addition, the relationship between information processing biases and clinical markers of panic (including affective, behavioral, and cognitive symptom measures) was investigated, along with the relationships among biases. Results indicated more threat biases among the panic (relative to control) group on each of the information processing measures, providing some of the first evidence for an implicit measure of panic associations. Further, structural equation modeling indicated that the information processing bias measures were each unique predictors of panic symptoms, but that the bias indicators did not relate to one another. These findings suggest that cognitive factors may independently predict panic symptoms, but not covary. Results are discussed in terms of their support for cognitive models of panic and the potential for automatic versus strategic processing differences across the tasks to explain the low relationships across the biases.
Keywords: information processing, panic disorder, interpretation, attention, implicit associations, automatic
The choice to observe one’s pounding heart without jumping to the conclusion that it is a sign of a heart attack or other impending disaster is thought by cognitive theorists to be the key to unraveling panic attacks. The cognitive model of panic disorder was developed in part from observations of pharmacological and neurochemical studies of agents that promoted panic attacks, but only in select individuals - those who tended to interpret the bodily sensations induced by the agents in a disastrous way (Clark, 1986). This led Clark (1986) to suggest that panic attacks occur because certain bodily sensations are misinterpreted as indicating a catastrophe, such as a heart attack or loss of control (see also Goldstein & Chambless, 1978).
The specific cognitive model of panic derives from more general cognitive theories to explain anxiety and fear. The general model proposes that maladaptive schemata (cognitive frameworks) influence information processing so that vulnerable individuals are more attentive to potentially threatening cues, more likely to interpret ambiguous cues as threatening, and more likely to remember cues relevant to fear (e.g., Beck, 1976; Beck & Emery with Greenberg, 1985). These cognitive biases are thought to maintain anxiety and panic by keeping threat cues salient (see Clark, 1999; Young, 1999). Despite the strong theoretical emphasis on anxious schemata, there has been little empirical support for the schema construct, in part because of the difficulty in operationalizing the concept of interconnected associations in memory (the definition for schema advocated by Segal, 1988, which we follow here). In the current study, we examined a range of information processing biases expected to be present among persons with panic disorder in order to evaluate: (a) evidence for panic associations in memory, (b) the relationship among information processing biases, and (c) the relationship of information processing biases to clinical markers of panic.
Examining Panic Associations and Relationships among Information Processing Biases
There have been numerous prior studies investigating the independent role of one panic-related information processing bias or another, but few studies that have examined the relations among different information processing biases or that have tried to operationalize panic associations at an implicit level to capture elements of the schemata construct (specifically, associations in memory that are activated automatically). These missing pieces are critical to fully characterize the role of cognitive processing in emotional disorders (Wells & Matthews, 1996). Further, while there is considerable evidence for different types of information processing biases in panic disorder (attention: e.g., Beck, Stanley, Averill, Baldwin, & Deagle, 1992; Ehlers, Margraf, Davies, & Roth, 1988; Hope, Rapee, Heimberg, & Dombeck, 1990; interpretation: e.g., Clark et al., 1997; McNally & Foa, 1987; memory: e.g., Cloitre, Shear, Cancienne, & Zeitlin, 1994; Nunn, Stevenson, & Whalan, 1984), there are also many null findings that are challenging to explain based on current cognitive models (see Austin & Richards, 2001; Casey, Oei, & Newcombe, 2004; Coles & Heimberg, 2002).
Investigating single information processing biases in isolation makes it difficult to compare discrepant results because of the possibility that sample differences may explain inconsistent findings. Further, examining information processing biases individually leaves critical theoretical proposals unexamined. For instance, in their seminal work on the cognitive model for anxiety disorders, Beck and colleagues suggested, “When specific schemas or a constellation of schemas is activated, their content directly influences the content of a person’s perceptions, interpretations, associations, and memories at a given time” (Beck et al. 1985, p. 55). This implies that we should expect to see significant relationships between different cognitive processes. Variations of this expectation have been described in more recent models that offer refinements to the generic schema theory, such as Beck and Clark’s (1997) discussion of automatic and strategic biases in anxiety, Wells’ (1997) review of cognitive theories of anxiety, and Wells and Matthews’ (1996) model of Self-Regulatory Executive Function (S-REF). Moreover, the theoretical expectation of inter-relations among information processing biases is implicit in Clark’s (1986) writings on panic.
At the same time, other cognitive theories have challenged this assumption, at least tacitly, based on proposals that only certain information processing biases will be related to a given disorder (thus, presumably the biases may not be strongly related). For instance, Williams, Watts, MacLeod, and Mathews (1997) differentiated between early processing of stimuli, where information is primed in the system, versus later elaboration of information. They suggest that anxiety disorders are characterized by biased processing of threatening information that occurs mainly at the priming stage, affecting automatic aspects of encoding and retrieval. Hence, researchers see a robust attentional bias, but not a consistent explicit memory bias. In contrast, depression is characterized by biased elaborative processing, leading to more consistent memory effects (though see important modifications of this position described in Mathews & MacLeod, 2005). Currently, the field is at a challenging juncture with little consensus about when to expect biases to be related and when to predict independence.
It is surprising that the relationship among information processing biases has not received more empirical attention, given the remarkable impact of cognitive models of anxiety (see Hirsch, Clark, & Mathews, 2006). Yet, we found few published studies that investigated multiple panic-related information processing measures within the same sample. Further, many of the studies that did include multiple bias measures did not report the relationship among the measures (e.g., Beck, Stanley, & Averill, 1992; Lim & Kim, 2005). Among the few studies that have examined multiple biases in the same sample and reported on their relationship, the results have generally suggested no significant correlations. Lundh, Czyzykow and Öst (1997) found no relationship between measures of explicit and implicit memory biases among patients with panic disorder and agoraphobia (see similar findings from Baños, Medina, & Pascual, 2001, and Cloitre, Shear, & Cancienne, 1994). Further, Lundh, Wikstrom and Westerlund (1999) found no correlation between memory and attention biases. While small in number, these results are problematic for those cognitive models that hypothesize significant relationships among biased processes, suggesting either that the models need to be revised or that there are concerns about the validity and/or reliability of the paradigms used to reflect the information processing biases.
To date, we are unaware of any studies that have looked at measures related to interference/attention, interpretation and automatic associations in the same study. Evaluating this broad range of biases is important not only to reflect different types and stages of cognitive processing and their inter-relations, but also to capture both automatic (outside of conscious awareness or control) and strategic (deliberate and available to self-report) biases in information processing (see Beck & Clark, 1997). Of course, we recognize that most paradigms capture a range of processes and implicit/explicit components (see Conrey, Sherman, Gawronski, Hugenberg, & Groom, 2005; Jacoby, 1991), rather than truly looking at these issues in isolation. Thus, when we refer to attention versus interpretation or implicit versus explicit (or the related constructs, automatic versus strategic), we are referring to the dominant - rather than exclusive - mode of processing measured by a given task. Keeping in mind this caveat, we evaluated measures tied to: (a) panic associations that are automatic in the sense of being involuntary, (b) interference effects activated by panic cues (associated with selective attention to threat information), and (c) interpretation of ambiguous situations tied to bodily sensations (reflecting somewhat more elaborative thinking).
Measuring Information Processing Biases and their Relation to Panic Symptoms
Our goal in assessing the three different information processing biases was to determine not only how they show known-group differences (i.e., differentiate between persons with and without panic disorder), but also how they inter-relate and predict clinical markers of panic. Thus, we assessed self-reported panic symptom severity, agoraphobic avoidance, and subjective distress during a panic-related provocation (task designed to elicit mild suffocation sensations). In addition, we assessed anxiety sensitivity, which is a measure of explicit threat appraisals related to the meaning of anxiety symptoms. This follows McNally’s (2001) recommendation to include both appraisal and information processing approaches when trying to understand cognitive functioning in anxiety. This multi-modal assessment of panic symptoms has two primary advantages: (1) it takes into account the frequently observed desynchrony across indicators of anxiety (Lang, 1985) by measuring a variety of responses, so that it is possible to look at convergence across measures, and (2) it provides continuous (rather than dichotomous) symptom measures that can show variance among persons with and without panic disorder, which can help address, though admittedly not resolve, the problem of examining correlations among measures in an extreme-groups design.
Based on general information processing models of anxiety (Beck et al., 1985; Beck & Clark, 1997) and the cognitive model of panic (Clark, 1986), it was hypothesized that each of the information processing biases would differentiate persons with and without panic disorder, and also predict the continuous measures of panic-related symptoms. These hypotheses are not particularly novel for the attention and interpretation bias measures, but this study is unique in trying to establish evidence for implicit measures of panic disorder associations.
In an earlier study investigating information processing biases among individuals high and low in anxiety sensitivity (a known vulnerability marker for panic; Schmidt, Lerew, & Jackson, 1997), Teachman (2005) found that a measure of implicit associations in memory differentiated the anxiety sensitive groups and was positively related to anxiety and panic symptoms. This measure examined associations with the self (versus others) as panicked versus calm (using the Implicit Association Test; Greenwald, McGhee, & Schwartz, 1998). Given its established validity in an anxiety sensitive sample, we will use this same measure in the current study to investigate panic associations in a diagnosed sample. An additional implicit measure of panic associations tied specifically to beliefs about the dangerousness of bodily sensations (reflecting Clark’s, 1986, model) will also be included.
As noted, each of the information processing bias measures is expected to distinguish individuals diagnosed with panic disorder from healthy control participants, and each bias measure is anticipated to predict a range of panic symptoms. However, the relationships among the information processing measures are considerably harder to predict. On the one hand, many theoretical models of anxiety and panic (e.g., Beck et al. 1985; Clark, 1986) suggest that the different cognitive processes should be interrelated. On the other hand, some models are more cautious in this regard, and the limited available data have not supported this hypothesis, finding no significant correlations among bias measures in samples diagnosed with panic disorder. Further, mixed results were observed in Teachman’s (2005) study with a high anxiety sensitive sample, which used similar bias measures to those used in the current study.
Thus, McNally, Hornig, Hoffman and Han’s (1999) suggestion that cognitive factors may independently present risk for panic but not covary is quite compelling. While this idea was based on their evaluation of anxiety sensitivity and its low relation to interpretive, attentional, and memory tasks (they did not report correlations among the information processing measures), their suggestion may be informative for panic disorder as well. Perhaps, as McNally and colleagues suggest, “it is entirely possible that within the cognitive domain, risk factors may function independently of one another and not figure as different aspects of the same construct” (p. 52). If independence among the measures were evident in the current study, it would imply unrelated correlates or maintaining factors for panic. We tentatively hypothesized little relationship among the information processing measures in the present study, following from the lack of significant relationships observed in prior research.
Method
Participants
Participants with panic disorder were recruited as part of a larger treatment study through newspaper, television, email, radio, print ads and flyers posted around the Charlottesville-Albemarle community and University of Virginia campus that invited individuals who had experienced panic attacks to contact our confidential phone line. Interested individuals were then screened over the phone to evaluate whether they would likely meet criteria for panic disorder, and to confirm they had experienced a panic attack over the past month. Other inclusion criteria, also assessed by phone, included: (1) minimum 18 years of age, (2) mastery of written and spoken English (to complete the assessment battery), and (3) no history of completing a prior course of cognitive-behavioral therapy (CBT) for panic (due to previous discussion of cognitive biases associated with panic). In addition, the phone screen inquired about substance abuse or dependence within the past year, current psychosis, and unmanaged manic symptoms, as these were all exclusion criteria given their potential influence on information processing biases. Other comorbidity, including current depression and other anxiety disorders, as well as other prior or current medication or psychosocial treatments were not grounds for exclusion (though we asked that participants be stable in their treatment course for at least six weeks).
Individuals who met the inclusion criteria were then invited to come to our clinic to complete the Structured Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbon & Williams, 1995) in order to establish a diagnosis of panic disorder with or without agoraphobia, check for suicidal ideation (an additional exclusion criterion), and assess current or lifetime history of other Axis I disorders. All phone screens and SCID interviews were conducted by trained doctoral students in clinical psychology with at least one year assessment experience, and all cases were presented to the first author and other interviewers during a weekly meeting to establish diagnostic consensus. Tape review and follow-up questions were used if there was any doubt about diagnoses. Of the approximately 155 individuals who completed the phone screen, 64 (41%) were appropriate and interested in coming in for the SCID evaluation. Of the remaining 155, 37 (24%) individuals were appropriate for participation but were not interested in completing the SCID and 54 (35%) individuals were not appropriate for participation based on the study exclusion criteria. From the group of 64, 59 were eligible following the intake evaluation (the other five were excluded based on further diagnostic information that emerged during the SCID) and were invited to complete the assessment battery at a separate session. Forty-three people completed the assessment battery, which was administered as the pre-treatment evaluation for a larger treatment study (thus, all individuals in the sample had agreed to, but not yet started, treatment).
The final sample for the panic disorder group (N=43; 70% with agoraphobic avoidance) was 70% female, mean age was 37.95 years old (SD=15.19, Range=18–70), and 88% were Caucasian (7% African-American, 2% described themselves as biracial, and 2% indicated “other” for ethnicity). The mean duration between participants’ first panic attack and intake was 158.21 months (SD=165.09, Range=2–612 months). Although panic disorder was the primary diagnosis in all cases (based on participant’s report of current interference and/or symptom severity), current comorbid Axis I diagnoses at intake included: 35% had other anxiety or related disorders (Specific Phobia, Generalized Anxiety Disorder, Obsessive Compulsive Disorder, Social Phobia, Post Traumatic Stress Disorder, and Trichotillomania), 26% had mood disorders (21% Major Depressive Disorder, 2% Bipolar I Disorder, and 2% Bipolar II Disorder), and 7% had eating disorders (Binge Eating Disorder and Eating Disorder NOS). In addition, 58% of the sample reported current psychotropic medication use at intake: 42% on antidepressants, 2% on antipsychotics, 30% on benzodiazepines, 2% on beta-blockers, and 9% on mood-stabilizers. Further, 17% reported ongoing psychosocial treatment at intake (for issues other than CBT for panic).
The healthy control group (N=38) was recruited through the psychology participant pool (using a prescreening measure) and through flyers posted around the community inviting individuals with no serious anxiety problems to call our confidential phone line. The prescreening written measure and phone screen inquired about current and past anxiety disorders, as well as current mood disorders, substance abuse, or dependence. All phone screens were completed by trained doctoral students in clinical psychology. During the testing session, participants were interviewed using a modified Mini International Neuropsychiatric Interview (MINI Plus, version 5.0, 2003; original by Sheehan et al., 1998), a brief structured diagnostic interview to confirm that the participant did not have a current or past anxiety disorder, or current mood, eating or psychotic disorder, nor a substance abuse or dependence diagnosis over the past year. (The MINI was used for the control sample because it is a relatively brief instrument that has been widely used to screen healthy participants, and can be administered more rapidly than the SCID, while obtaining comparable diagnostic information to assess inclusion/exclusion criteria.) This interview resulted in exclusion of 9 participants, leaving a final sample of 38. The final control sample was 53% female, mean age was 33.13 years old (SD=17.11, Range=18–78), and 90% were Caucasian (3% Asian, and 8% did not report ethnicity). A chi-square test indicated that the panic and healthy control groups did not differ by gender (χ2=2.51, p>.10), and an independent samples t-test indicated no significant age difference between groups (t79=1.34, p>.10, Cohen’s d=.30).
Materials
Measures of Mood and Anxiety Symptoms
Anxiety Sensitivity Index (ASI; Reiss, Peterson, Gursky & McNally, 1986)
This 16-item questionnaire measures concern over the symptoms associated with anxiety (e.g., “It scares me when my heart beats rapidly”), and has adequate psychometric properties (Telch, Shermis, & Lucas, 1989).
Beck Depression Inventory (BDI-II; Beck, Steer & Brown, 1996)
The BDI-II is a 21-item self-report inventory that measures severity of symptoms associated with depression.
General Measures of Panic Symptoms and Avoidance
Fear Questionnaire - Agoraphobia subscale (FQ-Agoraphobia; Marks & Mathews, 1979)
This 5-item subscale measures participants’ level of phobic avoidance toward common situations, such as crowded shops.
Panic Disorder Severity Scale (PDSS; Shear et al., 1997)
This 7-item scale has good inter-rater reliability, and provides a composite severity score of frequency, distress and impairment associated with panic attacks. Although this measure was designed as a clinician-administered instrument, several prior studies have had participants complete it as a self-report measure (e.g., Otto, Pollack, Penava, & Zucker 1999; Penava, Otto, Maki, & Pollack, 1998; Teachman, 2005). The instrument was modified slightly for this study by adding a description of panic attacks to the instructions so that it could be completed in a self-report format.
Behavioral Avoidance Test (BAT) and Subjective Distress
A BAT was conducted to activate mild suffocation sensations in order to evaluate avoidance of physical sensations and subjective distress during a panic-relevant provocation. Participants were asked to breathe through a thin straw for up to two minutes. This is a harmless activity, based on the interoceptive exposure used in Taylor and Rachman (1994), which typically produces some very temporary dizziness and lightheaded feelings. Participants were explicitly told they could stop the task at any point and that we did not expect everyone to complete the task. The task ended when participants had either reached the two-minute point or reported that they did not wish to proceed further. Immediately after the task ended, participants were asked to report their peak level of anxiety during the task using a Subjective Units of Distress Scale (SUDS) ranging from 0 (very low) to 100 (very high) to measure subjective distress (participants also reported their anticipatory anxiety before the task began, but after the instructions had been explained).
Measures of Information Processing
Automatic Panic Associations: Implicit Association Test (IAT; Greenwald, McGhee, & Schwartz, 1998)
The IAT measures automatic associations. Associations are automatic in the sense that evaluations occur outside conscious control, and at times, outside conscious awareness. Further, the evaluations reflect interconnected associations in memory, thus appearing to share some of the qualities ascribed to schemata (Segal, 1988). The IAT has adequate psychometric properties (Greenwald & Nosek, 2001), and like many tasks used by social cognition researchers (Fazio, 2001), it is a reaction time task that purportedly reflects strength of association between concepts in memory. The computerized version of the IAT requires items to be classified while two category labels are paired on either side of the screen. (See http://implicit.harvard.edu/implicit/for more information and a sample test.) Specifically, the task involves comparing the time taken to classify stimuli when paired categories match a person’s automatic associations (e.g., the concept ‘panicked’ is paired with the self for a person with panic disorder) versus the time taken when paired categories contradict automatic associations (e.g., the concept ‘calm’ is paired with the self for a person with panic disorder). It is expected that when categories are paired to match a person’s automatic associations, he or she will be able to classify the stimuli more quickly.
The task has a number of features that make it particularly suitable for panic research. First, the methodology minimizes the influence of self-presentational concerns (Greenwald et al., 1998). Second, the IAT uses a within-subject design, so the influence of state affect is held constant because the anxiety-evoking stimuli are present in both conditions being compared, permitting a relatively clean evaluation of cognitive processing.
The IAT is a relative task, so comparison categories are required for both the target and descriptor categories. In the first IAT task, which evaluated a panic self-concept (referred to as ‘IAT Panicked > Me’), the category ‘Calm’ was used as a comparison to the category ‘Panicked’ because it reflects the opposing emotional response. These categories were compared while being paired with descriptor categories to reflect the self versus others. Specifically, the categories ‘Panicked’ and ‘Me’ were paired at the top left of the computer screen while ‘Calm’ and ‘Not me’ were simultaneously paired at the top right. Participants were told to classify any stimuli that belonged to either the ‘Panicked’ or ‘Me’ categories on the left, and any stimuli that belonged to either the ‘Calm’ or ‘Not me’ categories on the right. They were not reporting on their evaluation of the stimuli and they had previously seen a list indicating which stimuli belonged in which category (so knew the correct answer); they were simply asked to complete the categorization task. Because participants did not directly report their evaluation, it was an indirect measure of associations. The dependent variable was speed of classification across a series of trials. Following this category pairing condition, the labels were switched and the same categorization task was completed while pairing ‘Panicked’ with ‘Not me’ and ‘Calm’ with ‘Me’. Thus, for each IAT task, two sets of category pairs were presented simultaneously.
A second IAT task was included to focus more specifically on Clark’s (1986) prediction of catastrophic misinterpretation of bodily sensations among persons with panic disorder (referred to as ‘IAT Bodily Changes > Alarming’). Here, the target categories ‘Bodily Changes’ versus ‘Body Parts’ were paired with the descriptors ‘Meaningless’ versus ‘Alarming’. ‘Body Parts’ was selected as the comparison category because of the semantic parallel to the ‘Bodily Changes’ category. (Unfortunately, this design assumed that body parts, like shoulder and ear, would not have negative, alarming associations for either group, an assumption that may have been unreasonable given the relationship between panic and other somatic and bodily concerns.; Bourque, 2004). The expectation in the current study was that the panic group would more readily associate feeling panicked with the self, and evaluate bodily changes as being more alarming than would the healthy control group. It should be noted that the first IAT task (‘IAT Panicked > Me’) is a previously validated measure, in terms of established known-group and predictive validity (in an anxiety sensitive sample; Teachman, 2005), whereas the second IAT task (‘IAT Bodily Changes > Alarming’) is a novel modification of an IAT, and hence reflects a more exploratory measure.
Based on recommendations from Nosek, Greenwald, and Banaji (2006), four representative items were selected for each category (see Appendix for category labels and stimuli). In each IAT task, there were two critical trial blocks: one block of trials where the target and descriptor categories reflected negative panic-relevant associations and one block in which the categories reflected non-panic associations. Each critical block consisted of 36 classification trials, and was preceded by a 20-trial practice block (the practice trials were not used in analyses because a shortened version of the IAT was employed that did not include single categorization blocks; similar to that used in Teachman & Woody, 2003). Participants first completed an unrelated practice IAT task to familiarize them with the procedure and then completed the two IAT tasks in random order. In addition, the ordering of the panic-consistent versus inconsistent blocks was counterbalanced, and the order of stimuli presentation within blocks was random. Participants were instructed to respond as quickly and as accurately as possible, and were provided error feedback throughout the task so they could correct any misclassifications before moving on to the next trial.
Interpretation Bias: Brief Body Sensations Interpretation Questionnaire (BBSIQ; Clark et al., 1997)
The BBSIQ is a 14-item version of the Body Sensations Interpretation Questionnaire, which is modified from McNally and Foa’s (1987) Interpretation Questionnaire. In the present study, very minor wording modifications were made to make the measure more prototypic of American rather than British English. Participants are presented with ambiguous events and then asked to rank order three alternative explanations for why the event might have occurred. One option is always negative, whereas the other responses are either neutral and/or positive. Half of the items refer to events consistent with the theoretical prediction of a catastrophic misinterpretation of bodily sensations (referred to as ‘Panic’ items), and the remaining items (referred to as ‘External Threat’ items) reflect other potentially threatening events (related mainly to fears of negative social evaluation). An example of a panic item is, “You notice that your heart is beating quickly and pounding.” The three alternative explanations are, “because you have been physically active,” “because there is something wrong with your heart,” or “because you are feeling excited.” After ranking these options, participants rate the extent to which they believe each of the explanations on a 0–8 Likert scale. Clark et al. (1997) found the measure had satisfactory internal consistency and effectively discriminated between individuals with panic and other anxiety problems.
This particular measure of interpretation bias was selected for the current study because of its close alignment with Clark’s model regarding catastrophic misinterpretation of bodily sensations, which was deemed important because the IAT tapping into this construct was not yet validated and we felt it critical to include an established measure that could assess this bias. Further, the BBSIQ was desirable because it is not a reaction time paradigm (in contrast to the other tasks, like the IAT), so would permit evaluation of biases that follow more deliberate, elaborative processing (again, unlike the other tasks). In this way, it was possible to include a mix of measures that reflected both relatively more automatic (e.g., the IAT) and more strategic (e.g., BBSIQ) processing.
Interference/Attentional Bias: Emotional Stroop Test (modified from the Stroop task; Stroop, 1935)
The most commonly used paradigm to assess attentional bias in emotional disorders is the modified or emotional Stroop test (Williams, Mathews, & MacLeod, 1996). It is a reaction time task that measures latency to name a word attribute, such as ink color, for threat-relevant versus neutral or other emotion words. It is based on the assumption that threat words will be named more slowly because of interference caused by their semantic content. The difference in response time for naming the ink color across the various word stimuli is typically interpreted as evidence of an attentional bias. However, this has been disputed, with some researchers arguing that Stroop effects more clearly demonstrate interference from personally-relevant stimuli, rather than a clean attentional bias (see Dalgleish & Watts, 1990; Williams et al., 1997).
The word stimuli for the present study (see Appendix) included one panic-relevant category (panic/physical threat words) and three control categories (social threat, positive and neutral words). Stimuli were selected from the word lists published in Beck et al.’s (1992) examination of attention for threat in panic disorder. Twelve words from their initial list of 20 were selected that were thought to best reflect the category of interest for the present study. The panic, social, and positive words had previously been matched by independent raters for level of emotionality. The social threat category was included to permit evaluation of the specificity of threat biases associated with panic, given findings of common processing biases in panic disorder and social phobia (e.g., Heinrichs, Hofmann, & Barlow, 2004; Hicks, Leitenberg, & Barlow, 2005). The Stroop blocks were administered in random order to control for possible order effects, and semantically-related neutral words (all household items) were used to control for potential priming effects. Procedures were modeled after those described in Holle, Neely and Heimberg (1997) using a blocked presentation (this choice was made because of evidence from Holle et al. that the blocked, but not random presentation, resulted in stronger effects). Participants first completed a brief practice task (naming the ink color of 12 musical instrument words). The four critical blocks of word categories were then presented with each block consisting of 48 trials (so each word was presented four times, and each ink color was used with equal frequency). The ink colors (red, green, blue, yellow) were used in random order. Error feedback was given in the form of a red exclamation mark on the screen and the incorrect color name needed to be corrected before the program would proceed to the next trial. The percentage of correct responses and the average response time in milliseconds was presented at the end of each block. Participants were instructed to respond as quickly and as accurately as possible by pressing one of four keys that were clearly marked with either an R for red, G for green, B for blue or Y for yellow. They were told to ignore the meaning of the word and to simply press the correct color key. One participant’s Stroop data were deleted due to an unusually high error rate (approximately 13%), and one participant’s data were deleted because he reported being color blind. Remaining participants had little difficulty with this response format as indicated by a 98% correct response rate across the critical blocks.
Given concerns about precisely what Stroop effects demonstrate, we refer to this task as a measure of interference/attentional bias. Resolving the debate about this measure is beyond the scope of the current study. Rather, the Stroop was selected not as a pure measure of attention but as the most-widely used measure of biases in panic disorder that captures involuntary processing of emotional information (see McNally, 1995). Use of this task thus provides a useful comparison to past research in panic disorder with a measure whose mechanisms have been well-researched.
Procedure
Informed consent was obtained before the SCID interview. At the testing session, participants completed the three information processing bias measures and a series of questionnaires. Order of the information processing tasks (IATs, Stroop, BBSIQ) and the questionnaire set (BDI, FQ-Agoraphobia, ASI, PDSS) was counterbalanced, order within the questionnaire set was randomized, and order of the IAT blocks (i.e., panicked + me/not me, and bodily changes + alarming/meaningless) was counterbalanced. Based on availability of testing space, some participants completed the computer tasks and questionnaires in an individual testing room, while others completed the tasks in a group testing room that included multiple testing carrels, separated by dividers. Headphones could be worn for the group administration if a participant desired, but all other procedures were identical and participants could not observe one another’s responses. Finally, all participants completed the straw breathing BAT in a private room. This task was always completed last because of concerns that residual anxiety from the task could contaminate responding on the other measures.
Results
Sample Characteristics
As anticipated, independent samples t-tests indicated that the panic and healthy control groups differed on each of the mood and panic symptom measures in the expected direction (see Table 1). This was true for both the questionnaires (BDI: t79=6.44, p<.001, d=1.45; FQ-Agoraphobia: t79=5.13, p<.001, d=1.15; ASI: t79=11.93, p<.001, d=2.68; PDSS: t79=19.08, p<.001, d=4.29), where the panic group reported more depressive symptoms, agoraphobic avoidance, anxiety sensitivity and panic severity, and for the straw-breathing BAT1, where the panic group indicated greater subjective distress (anticipatory anxiety: t72=5.17, p<.001, d=1.16; peak anxiety: t72=5.34, p<.001, d=1.20). To assess avoidance during the straw-breathing BAT, a median split was conducted on the time spent in the task because the variable was not normally distributed. As expected, the panic group spent less time in the task, indicating greater avoidance of physical sensations, than did the healthy control group (t72=2.13, p=.04, d=.50).
Table 1.
Sample characteristics
| Full Sample | Panic Disorder | Healthy Control | ||||
|---|---|---|---|---|---|---|
| Measure | M | SD | M | SD | M | SD |
| Beck Depression Inventory | 8.99 | 9.53 | 14.21 | 10.06 | 3.08 | 3.72 |
| Anxiety Sensitivity Index | 22.24 | 14.68 | 33.24 | 10.87 | 9.79 | 5.67 |
| Fear Questionnaire - Agoraphobia subscale | 6.59 | 8.09 | 10.37 | 9.11 | 2.32 | 3.46 |
| Panic Disorder Severity Scale | 7.04 | 7.29 | 13.22 | 4.24 | .05 | .32 |
| BAT Straw Breathing Anticipatory Anxiety | 23.90 | 21.57 | 35.05 | 23.86 | 12.74 | 10.89 |
| BAT Straw Breathing Peak Anxiety | 48.32 | 27.02 | 62.62 | 26.42 | 34.03 | 19.03 |
| BAT Straw Breathing Time (ms) | 62.32 | 36.59 | 57.92 | 35.88 | 66.73 | 37.24 |
Group Differences in Information Processing Biases2
Automatic Panic Associations
The IAT data were scored according to the new scoring algorithm developed by Greenwald, Nosek & Banaji (2003), because this approach maximizes convergent validity as assessed by the relationship between implicit and explicit measures, and improves the psychometric properties of the tool by taking into account each respondent’s latency variability. Using this approach, no participants’ IAT data needed to be eliminated (based on either high error rates and/or unusually fast or slow response times). Positive IAT effects, known as D scores3, reflect relatively faster response times for panic-relevant automatic associations. An omnibus test was first conducted to determine whether follow-up, focused tests examining the individual IAT tasks were justified. A repeated measures analysis of variance (ANOVA) with panic group (2-level) as the between-subjects factor and IAT (2-level) as the within-subjects factor was conducted. There was a significant group by IAT interaction, F (1, 79) = 7.35, p=.008, η2=.09 (and not a significant main effect of group, p>.10), thus follow-up tests examining the source of the interaction were conducted. As expected, the panic group responded more quickly to self-evaluations with panic (IAT Panicked > Me: t79=2.12, p=.04, d=.48) than did the healthy control group4, providing support for automatic panic associations (see Figure 1).
Figure 1. Group differences in panic schema (on the IAT) with standard error bars.
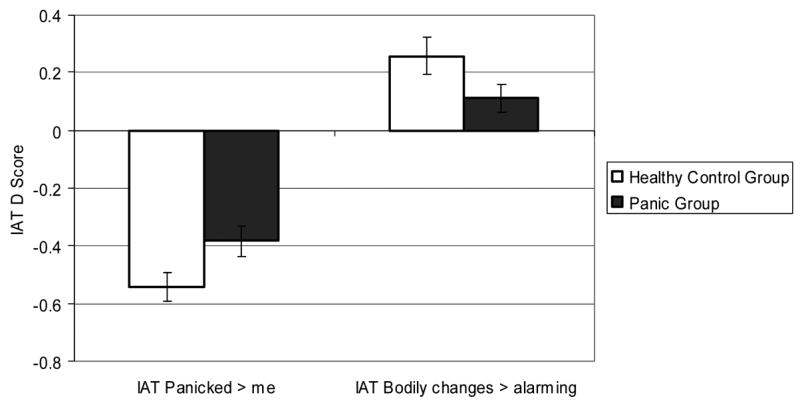
Note. IAT=Implicit Association Test. The IAT tasks are relative in nature, so higher IAT Panicked>me scores indicate relatively greater panicked (versus calm) associations with the self (versus others), and higher IAT Bodily changes>alarming scores indicate relatively greater associations between bodily changes (versus body parts) and alarming (versus meaningless).
The IAT task measuring catastrophic misinterpretation of bodily sensations did not indicate a significant group difference (t79=1.81, p=.07, d=.41). Surprisingly, there was a trend for higher scores for the healthy control group. Unfortunately, these results are somewhat difficult to interpret because this version of the IAT had not previously been validated (unlike the IAT Panicked > Me task). The task itself may have been complicated for participants because of the unusual category classifications. Specifically, use of the category ‘Body parts’ may have raised somatic concerns for the panic participants, making it a poor comparison for the primary category of interest, ‘Bodily changes.’ These results seem to suggest that individuals with panic disorder see both body-relevant categories as equally alarming (as evident by a mean close to the zero point, indicating no preference for one category pairing over another).
Interpretation Bias
Based on the scoring of the BBSIQ in Clark et al. (1997), four threat-relevant dependent variables are derived from the scale: panic ranking, panic rating, external threat ranking, external threat rating. Given the large number of variables, an omnibus test was first conducted to establish a significant overall between-subjects effect (to determine whether more focused tests comparing the groups on the four variables was justified). A repeated measures ANOVA with group (2-level) as the between-subjects factor and BBSIQ (4-level) as the within-subjects factor was conducted (given the different measurement scales for the rank and rating responses, z scores were used). As expected, results yielded a significant between-subjects group effect (F (1, 79) = 19.43, p<.001, η2=.20), and there was no significant group by BBSIQ interaction (p>.10). Thus, follow-up t-tests were conducted to evaluate the specific group differences. The panic group both ranked and rated the threat interpretations more highly than the healthy control group for all indices (panic items - ranking: t79=4.32, p<.001, d=.97; rating: t79=3.63, p=.001, d=.82; external threat items - ranking: t79=4.03, p<.001, d=.91; rating: t79=2.13, p=.04, d=.48). These results suggest a threat-oriented interpretation bias associated with panic disorder that is present both for bodily sensation and external threat-relevant ambiguous scenarios. See Figure 2.
Figure 2. Group differences in interpretation biases (on the BBSIQ) with standard error bars.
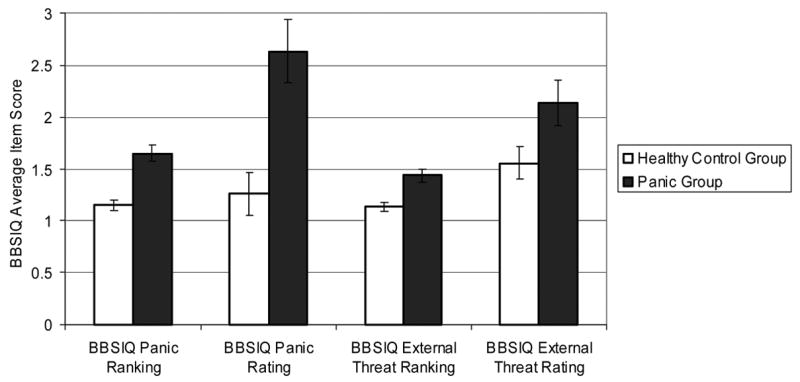
Note. BBSIQ=Brief Body Sensations Interpretation Questionnaire (range for rank data = 1–3, range for rating data = 0–8).
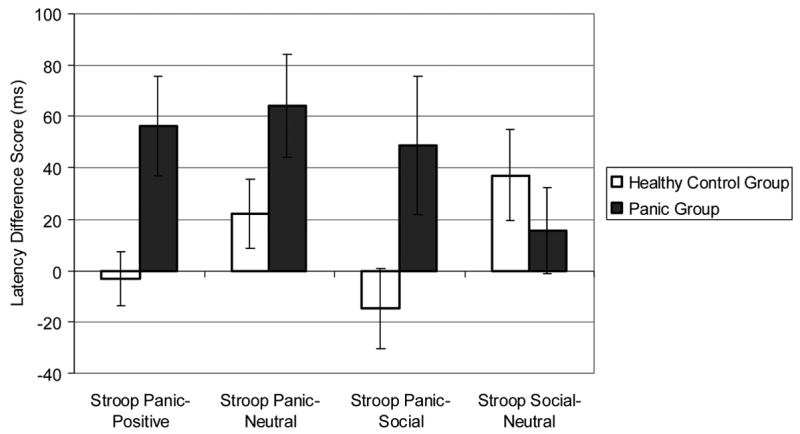
Interference/Attention Bias
The panic group was expected to have difficulty naming the color of panic words due to interference from the semantic content of these words. Results indicated slower naming of panic words by the panic group, relative to the healthy control group (t77=3.86, p<.001, d=.88). To control for individual differences in overall color-naming speed, the Stroop effect was calculated by subtracting the average latency for color-naming positive words from the average latency for color-naming panic/physical threat-relevant words. In addition, trials slower than 2500 ms or faster than 333 ms were excluded following Gilboa & Gotlib, 1997. The same difference score was obtained for the neutral and social threat word categories (subtracted from the panic words). Again, given the large number of variables, an omnibus test was first conducted to establish a significant overall between-subjects effect. A repeated measures ANOVA with group (2-level) as the between-subjects factor and Stroop difference scores (3-level) as the within-subjects factor was conducted. As hypothesized, results yielded a significant between-subjects group effect (F (1, 77) = 5.47, p=.02, η2=.07), and there was no significant group by Stroop interaction (p>.10). Follow-up t-tests were thus conducted to evaluate the specific group differences. Significant group differences were observed on the Stroop Panic-Positive indicator (t77=2.59, p=.01, d=.59), and there was a trend for differences on the Stroop Panic-Neutral indicator (t77=1.69, p=.095, d=.39), and the Stroop Panic-Social indicator (t77=1.97, p=.05, d=.45), all suggesting slower panic (versus other word) naming latencies for the panic group. Further, there was no group difference on the control Stroop Social-Neutral indicator (t77=.89, p>.10, d=.20), suggesting the interference/attention bias was specific to panic words. See Figure 3.
Figure 3. Group differences in attention biases (on the Stroop) with standard error bars.
Relationships between Information Processing Biases and Prediction of Panic Symptoms
To simultaneously evaluate the relationships among the information processing biases and their unique prediction of panic symptoms, we compared a series of nested structural equation models (SEM) that varied the constraints on the paths connecting the bias measures and those predicting panic symptoms (see Figure 4). This approach allows for simultaneous consideration of relations between multiple bias predictors and panic symptom dependent variables, along with direct tests of the hypothesized relationships between the bias and symptom measures. Further, using SEM makes it possible to build a latent measure of panic symptoms in order to model inter-individual differences while taking into account intra-individual variability and measurement error across indicators. This latter point is important because there is debate regarding whether low relations among anxiety measures reflect meaningful individual desynchrony or poor psychometric properties of measures (see Zinbarg, 1998).
Figure 4. Information processing biases predicting panic symptoms: Structural equation model with standardized coefficients noted (for both the full sample and panic group alone).
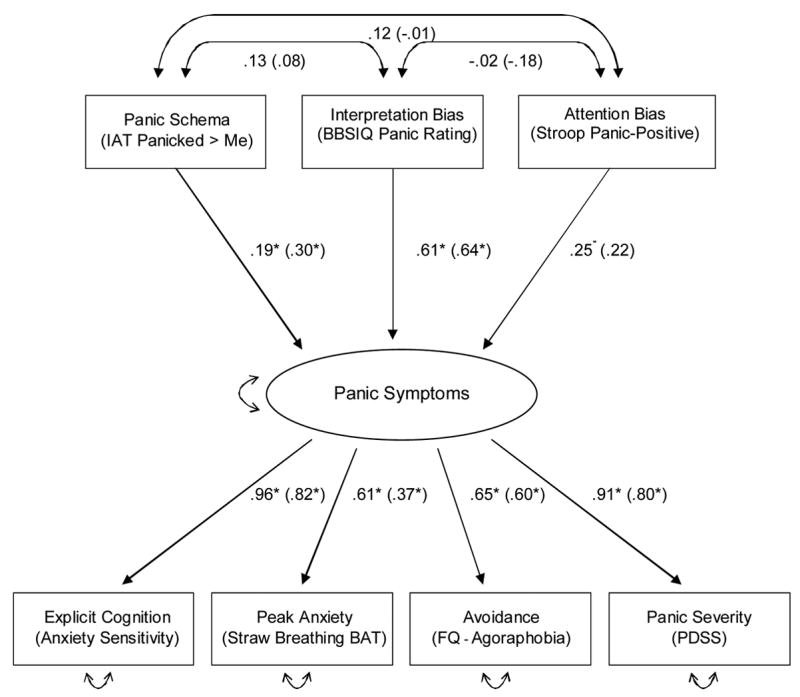
Note.
 indicate error terms. * = p<.05
indicate error terms. * = p<.05
The numbers in brackets reflect the standardized coefficients for the model run with only the panic group, and the numbers not in brackets reflect the coefficients for the full sample.
A model was developed to parsimoniously test the hypotheses that each of the biases would uniquely predict panic symptoms, and that there would be little relationship among the measures of automatic associations, interference/attention, and interpretation bias. A single indicator was selected to reflect each of the information processing biases based on the marker that most clearly tapped the theoretical expectation of bias associated with panic. The rationale for developing the model in this way was to maximize interpretability of the model and minimize the number of parameters being estimated to insure adequate power. (Also, only one of the Stroop variables could be included in the model given the lack of independence among the Stroop difference score variables because each included the same panic latency measure). The IAT Panicked > Me task was selected because of the centrality of panic self-concept, and the previously established validity of this IAT task (relative to the IAT Bodily Changes > Alarming task). The BBSIQ panic rating was selected because it focuses on catastrophic misinterpretations of bodily sensations, the key premise in Clark’s (1986) model, and has a continuous dependent variable (unlike the rank variable, which would require a different modeling approach because of its categorical nature). Finally, the Stroop Panic-Positive indicator of attention bias was chosen because it helps control for individual differences in response speed (by using a difference score), and controls for the impact of simply processing emotional information (by using the Positive comparison word category). These three indicators were allowed to inter-correlate in the baseline model (see Figure 4) so that these paths could subsequently be tested to check for significant relationships among bias measures, and so that their common variance would be controlled to look at how each bias measure uniquely predicted panic symptoms.
The next step in developing the model was to build a “true score” latent factor of panic symptoms. This approach is advantageous because the factor then reflects the variance common to the different panic indicators, thus minimizing the impact of measurement error and intra-individual variability across symptom indicators. This latent factor was comprised of an overall measure of panic severity (using the PDSS), and one indicator for each of three fear response channels: (1) affect (based on peak anxiety rating on the straw breathing BAT), (2) behavioral avoidance (using the FQ-agoraphobia subscale), and (3) explicit cognition (using the ASI). To examine the internal validity of the proposed factor, correlations among the indicators within the latent factor were evaluated to determine the empirical support for the selected combination of indicators. Significant correlations were observed among each of the panic symptom indicators, so all were retained on the factor (see Table 2).
Table 2.
Correlations among model indicators (full sample)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Peak Anxiety (Straw Breathing BAT) | ||||||
| 2. Explicit Cognition (Anxiety Sensitivity Index) | .61** | |||||
| 3. Avoidance (FQ-Agoraphobia Subscale) | .31** | .59** | ||||
| 4. Panic Severity (Panic Disorder Severity Scale) | .53** | .88** | .66** | |||
| 5. Panic Self-Schema (IAT Panicked > Me) | .25* | .26* | .30** | .30** | ||
| 6. Interpretation Bias (BBSIQ Panic Rating) | .46** | .65** | .38** | .49** | .13 | |
| 7. Attention Bias (Stroop Panic-Positive) | −.03 | .20+ | .36** | .33** | .12 | −.03 |
Note.
=p<.10,
=p<.05,
=p<.001.
These correlations should be interpreted with caution because the original sample was pre-selected to have a bimodal distribution on panic symptoms.
A series of nested structural regression models were then compared (see McArdle & Hamagami, 1996). Comparing the change in fit for nested structural models allows alternative hypotheses to be evaluated systematically by testing the change in chi-square value, with lower values indicating better fit (Joreskog & Sorbom, 1979). All models were fit to the data using AMOS, and full information maximum likelihood methods were used so that incomplete data were treated as missing at random (Little & Rubin, 1987). The baseline model (referred to as Model 1 in Table 3) freely estimated all of the paths connecting the information processing bias indicators and those predicting panic symptoms. Figure 4 depicts this baseline model with standardized coefficients noted and significant coefficients labeled with an asterisk. As expected, each of the information processing bias measures was a significant and unique predictor of panic symptoms, and each of the panic symptom indictors loaded significantly onto the latent factor. Further, none of the information processing bias indicators were significantly inter-correlated. These results provide considerable support for the hypothesized relationships, but are more convincing when compared to alternative models that directly test each of the hypothesized relationships.
Table 3.
Fit statistics for the baseline and competing, nested models
| Goodness-of-fit indices | |||||||
|---|---|---|---|---|---|---|---|
| X2 | df | ΔX2/Δdf | p < .05 | ΔNFI | CFI | RMSEA | |
| Model 1: Baseline Model (Figure 4) | 33.56 | 11 | --- | --- | .88 | .91 | .16 |
| Competing models evaluating absence of relationships among information processing indicators: | |||||||
| Model 2: Panic schema & attention bias corr. set to zero | 34.62 | 12 | −1.06/1 | No | .88 | .91 | .15 |
| Model 3: Panic schema & interpretation bias corr. set to zero | 34.92 | 12 | −1.36/1 | No | .87 | .91 | .16 |
| Model 4: Interpretation bias & attention bias corr. set to zero | 33.61 | 12 | −.05/1 | No | .88 | .91 | .15 |
| Competing models evaluating paths from information processing indicators to panic symptoms factor: | |||||||
| Model 5: Path from panic schema set to zero | 38.27 | 12 | −4.71/1 | Yes | .86 | .89 | .17 |
| Model 6: Path from interpretation bias set to zero | 70.20 | 12 | −36.64/1 | Yes | .75 | .77 | .25 |
| Model 7: Path from attention bias set to zero | 158.19 | 12 | −124.63/1 | Yes | .43 | .41 | .39 |
| Check that Baseline Model fit does not depend on common variance with explicit cognitive indicator: | |||||||
| Model 8: Baseline Model without the Anxiety Sensitivity Index | 14.89 | 6 | --- | --- | .89 | .92 | .14 |
| Check that a similar pattern of relationships is evident when the Baseline Model is run within the panic group alone: | |||||||
| Model 9: Baseline Model in panic group alone | 26.16 | 11 | --- | --- | .72 | .77 | .18 |
Note: Δχ2/Δdf =change in chi-square and degrees of freedom relative to the baseline model; p < .05 indicates whether the alternate model is significantly different from the baseline model based on Δχ2 tested on a χ2 distribution with df equal to the Δdf between the models; NFI = Normed Fit Index; CFI = Comparative Fit Index; RMSEA = root-mean-square error of approximation.
Two sets of competing models were examined. First, to evaluate the relationships among the information processing indicators, Models 2 through 4 each constrained one of the paths connecting the bias measures to zero. If the changes in fit between the baseline and competing models are non-significant, this implies that the null hypothesis of non-significant estimates cannot be rejected. On the other hand, if any of the changes in fit are significant, this implies that the model fit is improved by including the inter-correlation between bias measures. Second, to investigate the unique prediction of panic symptoms by the information processing indicators, Models 5 through 7 each constrained one of the paths connecting the bias measure to the panic symptoms to zero. Here it was expected that setting any of the paths to zero would result in significant loss of fit, relative to the baseline model, implying that there are significant relationships between the information processing bias and symptom measures.
Table 3 outlines the goodness of fit indices and the change in fit (Δχ2 on Δdf) between the baseline model and each of the competing, nested models. The primary outcomes of interest were the change in relative fit for the competing models and the evidence for significant coefficients indicating predictive validity for the bias measures. Nonetheless, assessment of absolute model fit was also examined, including the root-mean-square error of approximation index (RMSEA; less than .08 can be considered an acceptable fit as defined by Browne & Cudeck, 1993; lower numbers are better), the comparative fit index (CFI) and normed fit index (NFI). Both the CFI and NFI vary from 0–1, with values above .90 indicating an acceptable fit (Hu & Bentler, 1999; higher numbers are better).
Results indicated strong support for the hypothesized baseline model. As noted earlier, all of the bias measures were unique, significant predictors of panic symptoms, and did not significantly inter-correlate. The fit indices for the baseline model indicated adequate fit according to the NFI and CFI, though the RMSEA was somewhat high. Most importantly, the nested model comparisons indicated no significant loss of fit (based on Δχ2 tested on a χ2 distribution with df equal to the Δdf between the models) when the relationships among the information processing bias measures were set to zero. In contrast, setting any of the paths from the bias measures to the latent panic symptoms factor to zero resulted in a significant loss of fit.
Next, we reran the baseline model omitting the explicit cognition (ASI) indicator from the panic symptoms factor (referred to as Model 8 in Table 3). Although we feel anxiety sensitivity is an important component of panic and should be included based on Lang’s (1985) three-systems model, we were concerned that because it is a cognitive measure and shares variance with the information processing bias indicators, ASI scores could potentially have exaggerated the observed relationships between the bias and symptom measures. Results indicated that the modified model without the ASI replicated the results from the earlier baseline model. Specifically, each of the bias indicators continued to significantly predict panic symptoms, and the information processing bias measures were not related to one another. This implies that the information processing measures predict panic symptoms above and beyond any common variance with explicit threat cognitions on the ASI.
Finally, given the limitations when examining relationships using an extreme groups design, the baseline model was also run within the panic group alone to establish whether the predictive validity of the information processing measures still held. As evident in Figure 4, the standardized coefficients (noted in brackets) were quite similar to the model with the full sample. Again, the panic symptom indicators all loaded significantly onto their latent factor. Moreover, there continued to be no significant relationships among the information processing bias measures. Further, in general, the bias indicators continued to significantly predict panic symptoms. The one exception to this finding was that the Stroop indicator, which had been a significant predictor within the full sample, no longer reached significance (p=.11). Note, however, that the parameter estimate changed very little, suggesting the difference in power due to the smaller sample size likely accounts for the change in significance. Finally, the fit statistics for this model are noted in Table 3 (see Model 9). While the fit statistics were slightly weaker than those for the model with the full sample and do not meet traditional thresholds (not altogether surprising given the lower sample size), the more critical issue is that the findings overall suggest a similar pattern of relationships – information processing biases predict panic symptoms, but do not relate to one another – regardless of whether the model is examined within or across groups.
Discussion
To evaluate cognitive models of panic disorder, a range of information processing biases were examined among individuals with and without panic disorder, including measures designed to reflect biases in automatic panic associations, interference/attention and interpretation of threatening information. The goal in assessing this broad array of biases was to: 1) establish evidence for implicitly measured panic associations, 2) examine the relationship between information processing biases and clinical markers of panic, and 3) investigate the relationship among information processing biases. Results provided strong support for the presence and predictive validity of information processing biases in panic disorder. When compared to the healthy control group, the panic group demonstrated greater interference from/attention to panic-relevant cues, more frequent and more extreme threatening interpretations of ambiguous scenarios, and lower implicit associations with the self as being calm, and in turn, relatively higher associations with the self as being panicked. Further, each of these biases was a unique predictor of a cluster of panic symptoms, including self-reported panic symptom severity, agoraphobic avoidance, explicit threat appraisals, and subjective distress during a panic-related provocation that involved breathing through a thin straw. Interestingly, despite finding that the information processing biases consistently predicted panic symptoms, the biases showed little relationship to one another.
Demonstration of biases across different cognitive processes and utilization of tools that vary in their relative reliance on automatic versus strategic responding (e.g., the IAT compared to the BBSIQ) allows for a broad assessment of Beck and Clark’s (1997) suggestion of different stages of information processing biases in pathological anxiety. The finding of implicit panic associations on the IAT is particularly important because this task reflects involuntary processing. Participants often find it difficult to control their responses on the IAT even though they can easily identify the stimuli being classified, and perhaps even the purpose of the task (Greenwald et al., 1998). Establishing these involuntary associations in panic is significant because the uncontrollable nature of threat processing is thought to be the hallmark of automaticity in pathological anxiety (see McNally, 1995). This finding is also valuable because the IAT measures automatic associations in memory, thereby capturing some of the critical aspects of the schema construct (as defined by Segal, 1988), a central element of cognitive models of anxiety that has been notoriously difficult to operationalize.
Beyond simply demonstrating the existence of the various information processing biases, we were interested in establishing the effectiveness of the biases in predicting clinical outcomes of interest. Note that these findings do not test causal relationships between information processing biases and panic, nor do they afford longitudinal prediction given the cross-sectional nature of the assessment. However, the findings do indicate that the biases were each related to a variety of important clinical markers of panic pathology, supporting their predictive validity. The interpretation bias measure showed a particularly strong association with the panic symptoms factor, perhaps due to the specific cognitive process being assessed (misinterpretations are central to Clark’s, 1986, model of panic). Alternatively, the strong relationship may be due to shared self-report method variance (the BBSIQ was the only information processing measure that used an un-timed, self-report methodology, which was also used for some of the panic indicators). Notably, the nested model comparisons in SEM suggested that taking away any of the biases as a predictor of panic symptoms would hurt the overall fit of the model.
It is particularly interesting that the information processing biases were each unique predictors of panic symptoms, but the biases showed minimal relationships with one another. As noted in the introduction, the expectation of minimal relationships among information processing biases was tentative, given that multiple theoretical models of anxiety and panic (e.g., Beck et al. 1985; Clark, 1986) suggest that the different cognitive processes should be inter-related. Yet, despite the predictions posited by these models, other models have at least tacitly assumed that the biases may not always be interdependent (e.g., Williams et al., 1997), and there has been little data to support the proposal of related biases (e.g., Baños et al., 2001; Cloitre et al., 1994; Lundh et al., 1997, 1999). Our study suggests considerable independence among different bias indicators. It is hard to explain this finding away in terms of measurement error or methodological limitations within a specific task, given that each of the tasks demonstrated known-groups convergent validation and predictive validity of panic symptoms. Further, the absence of relationships was evident when the data were examined for the full sample or within the panic group alone.
Perhaps the most parsimonious account of the low relationships among the bias measures follows McNally and colleagues’ (McNally et al., 1999) suggestion that cognitive risk factors for panic may function mostly independently, and each may maintain (or increase risk for) panic without being part of the same overarching construct. Cognitive biases may not be part of the same construct in so far as attention and interpretation may reflect separable processing steps. Instead, it may be the shared or divergent automatic versus strategic processes that determine which cognitive biases will inter-relate. Both the IAT and Stroop tasks reflect automatic processing in that the effects are largely uncontrollable, but the tasks differ in terms of whether semantic processing of threat stimuli is intentional or not (intentional for the IAT, but not for the Stroop; see Bargh, 1994; Gawronski & Bodenhausen, in press). Further, the BBSIQ differs from both the IAT and Stroop in that responses on this measure permit elaborative, strategic processing. Thus, each task differs from the others regarding its relative reliance on automatic and strategic processes, which may help explain why there was little relationship across the information processing tasks. Note, this idea that different processing requirements can explain dissociations among cognitive tasks has recently been considered in the depression field; Barry, Naus, and Rehm (2004) use Roediger and Blaxton’s (1987) ‘Transfer Appropriate Processing’ framework to understand the inconsistent implicit/explicit memory findings among persons with depressed mood.
We are not suggesting that this automatic versus strategic distinction fully explains the findings, but it is striking that many of the prior studies that observed little relationship among biases in panic disorder also compared tasks that differed on some feature of automaticity (see Bargh, 1994, for a discussion of automaticity features). For instance, Lundh et al. (1997), Baños et al. (2001), and Cloitre et al. (1994) all found no relationship between measures of explicit memory (using either cued or free recall) and implicit memory (using word stem completion) biases. On the other hand, Hirsch, Clark, and Mathews (2006) posited a “combined cognitive biases hypothesis,” suggesting that cognitive biases influence one another to impact disorders more substantively than they would in isolation. In their model, Hirsch and colleagues focus on the reciprocal relationship between negative imagery and interpretation biases in social phobia. Perhaps the evidence they find for a relationship between these biases stems from their shared strategic processing requirements (e.g., consciously resolving ambiguity). To date, there are not sufficient data to determine whether relationships among information processing biases can be predicted by their composition of automatic and strategic processes, but we think it is a worthwhile question to pursue to help explain why tasks measuring different processing steps (e.g., attention, interpretation) do not show consistent relationships.
Our findings also raise a number of intriguing, potential clinical implications. It will be important for future longitudinal research to consider the independence of cognitive vulnerability factors for the onset of panic and also whether the information processing bias measures change in tandem or separately over the course of treatment. The current study suggests that it may be necessary to assess a broad range of information processing biases to determine risk for panic because being low on one type of bias may not provide protection from another. Similarly, observing change on one type of bias following treatment may not indicate that other biases are also reduced, so vulnerability to relapse may remain. This issue of potentially harmful residual biases raises the possibility that it may be necessary to specifically target a range of information processing biases in treatment (e.g., selective attention, interpretation, etc.), rather than assuming change across cognitive processes.
Many open questions about the relationships among information processing biases remain, but at this point, it appears that the commonly observed desynchrony across different modalities of anxiety symptoms (e.g., behavior, psychophysiology, verbal report, etc.; Lang, 1985) may also exist within the various components of the cognitive domain. It remains a fascinating question (and source of debate; e.g., Zinbarg, 1998) why fear markers show such independence. Fear profiles can be highly idiographic at the symptom level (e.g., one person expresses their fear mainly through avoidance, while another shows little dysregulation in behavior but is overwhelmed by a rapid heart beat). Perhaps information processing biases are similarly idiographic, such that selective attention to threat information can lead to heightened anxiety for some people, without necessarily leading to overestimations of threat when the context is ambiguous, and vice versa. Thus, information processing biases may reflect the principle of equifinality, where a given end state (panic in this case) can be reached by many pathways.
The current findings need to be interpreted in light of the study’s limitations. In particular, the IAT task that was designed to reflect associations about the alarming nature of bodily sensations did not effectively distinguish the groups. An alternate version of this task was similarly ineffective in an earlier study with an anxiety sensitive sample (Teachman, 2005). In both cases, we suspect the requirement of a relative comparison category for the IAT led to the confusing findings. It is not obvious what category would serve as an appropriate contrast to bodily sensations. Future research that uses an implicit measure of associations that does not require the relative comparison category will be helpful. In addition, while the choice to use an extreme groups design was made because of the interest in evaluating the IAT and other information processing measures, this design choice has a clear limitation in that it makes correlations somewhat difficult to interpret because of the bimodal distribution. It is notable, however, that a similar pattern of relationships was observed when the model was examined within the panic group alone, suggesting this design choice cannot likely explain away the findings. Further, it would have been ideal to also include an anxious control group to determine the specificity of the information processing biases to panic. Our guess is that a number of the observed biases would likely be evident across anxiety problems, given that panic group biases were evident for all threat scenarios on the BBSIQ (not solely the bodily sensations scenarios), and given that a lack of calmness (which we assessed with the IAT), and even occurrence of panic attacks, is common across anxiety problems. Finally, a choice was made to include panic disordered participants who had a range of other comorbid diagnoses (e.g., depression). This design decision was made to increase the external validity of the clinical sample, but has the disadvantage that the comorbid conditions might have influenced the information processing measures (though see footnote 2, which suggests the primary findings cannot be explained by a particular comorbid condition or the presence of psychotropic medications).
Despite these limitations, the current study provides a remarkably consistent picture of information processing biases in panic disorder. Across a range of cognitive processes and strategic and automatic measurement approaches, the panic group repeatedly demonstrated a bias toward threatening information, relative to the healthy control group. Moreover, each of the information processing biases was a unique predictor of a variety of panic symptoms. These results provide strong support for cognitive and information processing models of panic. At the same time, the absence of significant relationships among a number of the information processing biases presents a challenge to those models that posit a cascade of inter-related biases that culminate in panic and pathological anxiety. Instead, it seems that each of the biases may independently present risk for elevated panic symptoms, without necessarily relating to one another.
Acknowledgments
The authors are thankful to the clinical interviewers, the research assistance provided by members of the PACT lab at the University of Virginia, and to Adam Radomsky for comments on an earlier version of the manuscript. This research was supported by an NIMH R03 PA-03-039 grant to Bethany Teachman.
Appendix
| Stroop Word List | ||||
|---|---|---|---|---|
| Panic/physical threat | Social threat | Positive | Neutral (Household) | |
| Collapse | inept | applause | lounge | |
| Tremble | worthless | superb | cushion | |
| Emergency | hated | achievement | furnished | |
| Attack | humiliated | excellent | ornament | |
| Illness | inferior | terrific | shower | |
| Ambulance | unsuccessful | delight | staircase | |
| Tingling | stupid | comfort | lamp | |
| Death | hopeless | merry | mantelpiece | |
| Faint | ridicule | confident | shelves | |
| Choking | foolish | enthusiasm | vase | |
| Sweat | lonely | celebration | chimney | |
| Dizzy | unfriendly | praise | upstairs | |
| Implicit Association Test Word List | ||||
| IAT Task 1: Panicked vs. Calm paired with Me vs. Not me | ||||
| Category Label: | Panicked | Calm | Me | Not me |
| Stimuli: | Panicked | Calm | Me | Not me |
| Scared | Relaxed | Self | Other | |
| Anxious | Serene | I | Them | |
| Frightened | Tranquil | My | They | |
| IAT Task 2: Bodily Changes vs. Body Parts paired with Meaningless vs. Alarming | ||||
| Category Label: | Bodily Changes | Body Parts | Meaningless | Alarming |
| Stimuli: | Heart racing | Arm | Meaningless | Alarming |
| Rapid pulse | Leg | Trivial | Scary | |
| Sweating | Shoulder | Insignificant | Terrifying | |
| Dizzy | Ear | Irrelevant | Dangerous | |
Footnotes
Due to an administrative error, straw-breathing data were not collected for seven participants (1 from the control group, 6 from the panic group).
Given the heterogeneity of the panic group sample with regard to diagnoses and medication use, a series of additional analyses examining group differences in information processing biases were run that isolated the different panic disorder subsamples [e.g., with and without a current mood disorder; with and without a current anxiety disorder (beyond panic and agoraphobia); current use of psychotropic medications]. These analyses suggested that the primary findings could not be explained by any particular comorbid condition or the presence of psychotropic medications.
IAT D scores reflect the difference in mean reaction time across critical blocks divided by the standard deviations across blocks, which is conceptually similar to Cohen’s d (see Greenwald et al., 2003).
Note that the absolute value of the IAT D measures (less than zero) reflect more automatic associations with calm, relative to panicked, for both groups. The finding of a positive absolute value for self-evaluations, even in clinical samples, is not unusual on the IAT (e.g., Buhlmann, Teachman, Gerbershagen, Kikul, & Rief, in press). It is the group comparison that is critical because the absolute value of the IAT score cannot be interpreted outside the context of the relative nature of the task.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Austin DW, Richards JC. The catastrophic misinterpretation model of panic disorder. Behaviour Research and Therapy. 2001;39:1277–1291. doi: 10.1016/s0005-7967(00)00095-4. [DOI] [PubMed] [Google Scholar]
- Baños RM, Medina PM, Pascual J. Explicit and implicit memory biases in depression and panic disorder. Behaviour Research and Therapy. 2001;39:619–629. doi: 10.1016/s0005-7967(99)00158-8. [DOI] [PubMed] [Google Scholar]
- Bargh JA. The Four Horsemen of automaticity: Awareness, efficiency, intention, and control in social cognition. In: Wyer RS Jr, Srull TK, editors. Handbook of social cognition. 2. Hillsdale, NJ: Erlbaum; 1994. pp. 1–40. [Google Scholar]
- Barry E, Naus MJ, Rehm LP. Depression and Implicit memory: Understanding mood congruent memory bias. Cognitive Therapy and Research. 2004;28:387–414. [Google Scholar]
- Beck AT. Cognitive therapy and the emotional disorders. New York: International Universities Press; 1976. [Google Scholar]
- Beck AT, Clark DA. An information processing model of anxiety: Automatic and strategic processes. Behaviour Research and Therapy. 1997;35:49–58. doi: 10.1016/s0005-7967(96)00069-1. [DOI] [PubMed] [Google Scholar]
- Beck AT, Emery G, Greenberg RI. Anxiety disorders and phobias. New York: Basic Books; 1985. [Google Scholar]
- Beck JG, Stanley MA, Averill PM. Attention and memory for threat in panic disorder. Behaviour Research and Therapy. 1992;30:49–58. doi: 10.1016/0005-7967(92)90007-4. [DOI] [PubMed] [Google Scholar]
- Beck JG, Stanley MA, Averill PM, Baldwin LE, Deagle EA., III Attention and memory for threat in panic disorder. Behaviour Research and Therapy. 1992;30:619–629. doi: 10.1016/0005-7967(92)90007-4. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory—II Manual. San Antoino, TX: The Psychological Corporation; 1996. [Google Scholar]
- Bourque LM. Interpretation bias in panic disorder: Specific or generalized? Dissertation Abstracts International: Section B: The Sciences and Engineering. 2004;64(11B):5773. [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Buhlmann U, Teachman BA, Gerbershagen A, Kikul J, Rief W. Implicit and explicit self-esteem and attractiveness beliefs among individuals with body dysmorphic disorder. Cognitive Therapy and Research in press. [Google Scholar]
- Casey LM, Oei TPS, Newcombe P. An Integrated Cognitive Model of Panic Disorder: The Role of Positive and Negative Cognitions. Clinical Psychology Review. 2004;24:529 –555. doi: 10.1016/j.cpr.2004.01.005. [DOI] [PubMed] [Google Scholar]
- Clark DM. A cognitive approach to panic. Behaviour Research and Therapy. 1986;24:461–470. doi: 10.1016/0005-7967(86)90011-2. [DOI] [PubMed] [Google Scholar]
- Clark DM. Anxiety disorders: why they persist and how to treat them. Behaviour Research and Therapy. 1999;37:S5–27. doi: 10.1016/s0005-7967(99)00048-0. [DOI] [PubMed] [Google Scholar]
- Clark DM, Salkovskis PM, Öst Lars-Göran, Breitholtz E, Koehler KA, Westling BE, Jeavons A, Gelder M. Misinterpretation of body sensations in panic disorder. Journal of Consulting and Clinical Psychology. 1997;65:203–213. doi: 10.1037//0022-006x.65.2.203. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Shear KM, Cancienne J. Implicit and explicit memory for catastrophic associations to bodily sensation words in panic disorder. Cognitive Therapy and Research. 1994;18:225–240. [Google Scholar]
- Cloitre M, Shear KM, Cancienne J, Zeitlin SB. Implicit and explicit memory for catastrophic associations to bodily sensation words in panic disorder. Cognitive Therapy and Research. 1994;18:225–240. [Google Scholar]
- Coles ME, Heimberg RG. Memory biases in the anxiety disorders: Current status. Clinical Psychology Review. 2002;22:587–627. doi: 10.1016/s0272-7358(01)00113-1. [DOI] [PubMed] [Google Scholar]
- Conrey FR, Sherman JW, Gawronski B, Hugenberg K, Groom C. Separating multiple processes in implicit social cognition: The Quad-Model of implicit task performance. Journal of Personality and Social Psychology. 2005;89:469–487. doi: 10.1037/0022-3514.89.4.469. [DOI] [PubMed] [Google Scholar]
- Dalgleish T, Watts FN. Biases of attention and memory in disorders of anxiety and depression. Clinical Psychology Review. 1990;10:589–604. [Google Scholar]
- Ehlers A, Margraf J, Davies S, Roth WT. Selective processing of threat cues in participants with panic attack. Cognition and Emotion. 1988;2:201–219. [Google Scholar]
- Fazio RH. On the automatic activation of associated evaluations: An overview. Cognition and Emotion. 2001;15:115–141. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I disorders. Washington, DC: American Psychiatric Association; 1995. [Google Scholar]
- Gawronski B, Bodenhausen GV. Unraveling the processes underlying evaluation: Attitudes from the perspective of the APE Model. Social Cognition in press. [Google Scholar]
- Gilboa E, Gotlib IH. Cognitive biases and affect persistence in previously dysphoric and never-dysphoric individuals. Cognition and Emotion. 1997;11:517–538. [Google Scholar]
- Goldstein AJ, Chambless DL. A reanalysis of agoraphobia. Behavior Therapy. 1978;9:47–59. [Google Scholar]
- Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: The implicit association test. Journal of Personality and Social Psychology. 1998;74:1464–1480. doi: 10.1037//0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- Greenwald AG, Nosek BA. Health of the Implicit Association Test at Age 3. Zeitschrift für Experimentelle Psychologie. 2001;48:85–93. doi: 10.1026//0949-3946.48.2.85. [DOI] [PubMed] [Google Scholar]
- Greenwald AG, Nosek BA, Banaji MR. Understanding and using the Implicit Association Test: 1. An improved scoring algorithm. Journal of Personality and Social Psychology. 2003;85:197–216. doi: 10.1037/0022-3514.85.2.197. [DOI] [PubMed] [Google Scholar]
- Heinrichs N, Hofmann SG, Barlow DH. Non-specific encoding of threat in social phobia and panic disorder. Cognitive Behaviour Therapy. 2004;33:126–136. doi: 10.1080/16506070410021692. [DOI] [PubMed] [Google Scholar]
- Hicks TV, Leitenberg H, Barlow DH. Physical, Mental, and Social Catastrophic Cognitions as Prognostic Factors in Cognitive-Behavioral and Pharmacological Treatments for Panic Disorder. Journal of Consulting and Clinical Psychology. 2005;73:506–514. doi: 10.1037/0022-006X.73.3.506. [DOI] [PubMed] [Google Scholar]
- Hirsch CR, Clark DM, Mathews A. Imagery and interpretations in social phobia: Support for the combined cognitive biases hypothesis. Behavior Therapy. 2006;37:223–236. doi: 10.1016/j.beth.2006.02.001. [DOI] [PubMed] [Google Scholar]
- Holle C, Neely JH, Heimberg RG. The effects of blocked versus random presentation and semantic relatedness of stimulus words on response to a modified Stroop Task among social phobics. Cognitive Therapy and Research. 1997;21:681–697. [Google Scholar]
- Hope DA, Rapee RM, Heimberg RG, Dombeck MJ. Representations of the self in social phobia: Vulnerability to social threat. Cognitive Therapy and Research. 1990;14:177–189. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Jacoby LL. A process dissociation framework: Separating automatic from intentional uses of memory. Journal of Memory and Language. 1991;30:513–541. [Google Scholar]
- Joreskog KG, Sorbom D. Advances in factor analysis and structural equation models. Cambridge, MA: Abt Books; 1979. [Google Scholar]
- Lang PJ. The cognitive psychophysiology of emotion: Fear and anxiety. In: Tuma AH, Maser JD, editors. Anxiety and the anxiety disorders. Hillsdale, NJ: Lawrence Erlbaum; 1985. pp. 131–170. [Google Scholar]
- Lim SL, Kim JH. Cognitive processing of emotional information in depression, panic, and somatoform disorder. Journal of Abnormal Psychology. 2005;114:50–61. doi: 10.1037/0021-843X.114.1.50. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. New York: John Wiley; 1987. [Google Scholar]
- Lundh LG, Czyzykow SÖst. Explicit and implicit memory bias in panic disorder with agoraphobia. Behaviour Research and Therapy. 1997;35:1003–1014. doi: 10.1016/s0005-7967(97)00063-6. [DOI] [PubMed] [Google Scholar]
- Lundh LG, Wikstrom J, Westerlund J. Preattentive bias for emotional information in panic disorder with agoraphobia. Journal of Abnormal Psychology. 1999;108:222–232. doi: 10.1037//0021-843x.108.2.222. [DOI] [PubMed] [Google Scholar]
- Marks IM, Mathews AM. Brief standard self-rating for phobic patients. Behaviour Research and Therapy. 1979;17:263–267. doi: 10.1016/0005-7967(79)90041-x. [DOI] [PubMed] [Google Scholar]
- Mathews A, MacLeod C. Cognitive vulnerability to emotional disorders. Annual Review of Clinical Psychology. 2005;1:67–95. doi: 10.1146/annurev.clinpsy.1.102803.143916. [DOI] [PubMed] [Google Scholar]
- McArdle JJ, Hamagami F. Multilevel models from a multiple group structural equation perspective. In: Marcoulides G, Schumacker R, editors. Advanced structural equation modeling techniques. Hillsdale, NJ: Lawrence Erlbaum Associates; 1996. pp. 89–124. [Google Scholar]
- McNally RJ. Automaticity and the anxiety disorders. Behaviour Research and Therapy. 1995;33:747–754. doi: 10.1016/0005-7967(95)00015-p. [DOI] [PubMed] [Google Scholar]
- McNally RJ. On the scientific status of cognitive appraisal models of anxiety disorder. Behaviour Research and Therapy. 2001;39:513–521. doi: 10.1016/s0005-7967(00)00073-5. [DOI] [PubMed] [Google Scholar]
- McNally RJ, Foa EB. Cognition and agoraphobia: Bias in the interpretation of threat. Cognitive Therapy and Research. 1987;11:567–581. [Google Scholar]
- McNally RJ, Hornig CD, Hoffman EC, Han EM. Anxiety sensitivity and cognitive biases for threat. Behavior Therapy. 1999;30:51–61. [Google Scholar]
- Nosek BA, Greenwald AG, Banaji MR. The Implicit Association Test at age 7: A methodological and conceptual review. In: Bargh JA, editor. Social Psychology and the Unconscious: The Automaticity of Higher Mental Processes. Psychology Press; 2006. pp. 265–292. [Google Scholar]
- Nunn JD, Stevenson RJ, Whalan G. Selective memory effects in agoraphobic patients. British Journal of Clinical Psychology. 1984;23:195–201. doi: 10.1111/j.2044-8260.1984.tb00646.x. [DOI] [PubMed] [Google Scholar]
- Otto MW, Pollack MH, Penava SJ, Zucker BG. Group cognitive-behavior therapy for patients failing to respond to pharmacology for panic disorder: A clinical case series. Behaviour Research and Therapy. 1999;37:763–770. doi: 10.1016/s0005-7967(98)00176-4. [DOI] [PubMed] [Google Scholar]
- Penava SJ, Otto MW, Maki KM, Pollack MH. Rate of improvement during cognitive-behavioral group treatment for panic disorder. Behaviour Research and Therapy. 1998;36:665–673. doi: 10.1016/s0005-7967(98)00035-7. [DOI] [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Roediger HL, Blaxton TA. Retrieval modes produce dissociations in memory for surface information. In: Gorfein DS, Hoffman RR, editors. Memory and learning: The Ebbinghaus Centennial Conference. Hillsdale, NJ: Erlbaum; 1987. [Google Scholar]
- Schmidt NB, Lerew DR, Jackson RJ. The role of anxiety sensitivity in the pathogenesis of panic: Prospective evaluation of spontaneous panic attacks during acute stress. Journal of Abnormal Psychology. 1997;106:355–364. doi: 10.1037//0021-843x.106.3.355. [DOI] [PubMed] [Google Scholar]
- Segal ZV. Appraisal of the self-schema construct in cognitive models of depression. Psychological Bulletin. 1988;103:147–162. doi: 10.1037/0033-2909.103.2.147. [DOI] [PubMed] [Google Scholar]
- Shear MK, Brown TA, Barlow DH, Money R, Sholomskas DE, Woods SW, Gorman JM, Papp LA. Multicenter collaborative Panic Disorder Severity Scale. American Journal of Psychiatry. 1997;154:1571–1575. doi: 10.1176/ajp.154.11.1571. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Harnett-Sheehan K, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar G. The Mini International Neuropsychiatric Interview (M.I.N.I.): The Development and Validation of a Structured Diagnostic Psychiatric Interview. Journal of Clinical Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- Stroop JR. Studies of interference in verbal reactions. Journal of Experimental Psychology. 1935;12:242–248. [Google Scholar]
- Taylor S, Rachman S. Klein’s suffocation theory of panic. Archives of General Psychiatry. 1994;51:505–6. doi: 10.1001/archpsyc.1994.03950060069011. [DOI] [PubMed] [Google Scholar]
- Teachman BA. Information processing and anxiety sensitivity: Cognitive vulnerability to panic reflected in interpretation and memory biases. Cognitive Therapy and Research. 2005;29:483–503. [Google Scholar]
- Teachman BA, Woody S. Automatic processing among individuals with spider phobia: Change in implicit fear associations following treatment. Journal of Abnormal Psychology. 2003;112:100–109. [PubMed] [Google Scholar]
- Telch MJ, Shermis M, Lucas J. Anxiety sensitivity: unitary personality trait or domain-specific appraisals? Journal of Anxiety Disorders. 1989;3:25–32. [Google Scholar]
- Wells A. Cognitive therapy of anxiety disorders. Chichester, England: John Wiley and Sons; 1997. [Google Scholar]
- Wells A, Matthews G. Modelling cognition in emotional disorder: The S-REF model. Behaviour Research and Therapy. 1996;34:881–888. doi: 10.1016/s0005-7967(96)00050-2. [DOI] [PubMed] [Google Scholar]
- Williams JMG, Mathews A, MacLeod C. The emotional Stroop task and psychopathology. Psychological Bulletin. 1996;120:3–24. doi: 10.1037/0033-2909.120.1.3. [DOI] [PubMed] [Google Scholar]
- Williams JMG, Watts FN, MacLeod C, Mathews A. Cognitive psychology and emotional disorders. 2. Chichester, England: John Wiley and Sons; 1997. [Google Scholar]
- Young JE. Cognitive therapy for personality disorders: A schema-focused approach. 3. Sarasota, FL, USA: Professional Resource Press/Professional Resource Exchange, Inc; 1999. [Google Scholar]
- Zinbarg R. Concordance and synchrony in measures of anxiety and panic reconsidered: A hierarchical model of anxiety and panic. Behavior Therapy. 1998;29:301–323. [Google Scholar]


