Abstract
This study was designed to evaluate the role and effectiveness of gallium 67 imaging in the diagnosis of acute myocarditis that mimics acute myocardial infarction. Of 315 consecutive acute myocardial infarction patients admitted to our institution over a 4-year period, 5 (2 men, 3 women) were suspected of having acute myocarditis. These 5 patients ranged in age from 23 to 69 years (median, 32 yr). All had experienced diarrhea or flu-like symptoms within the preceding 4 weeks, and each presented with signs, symptoms, and electrocardiographic findings consistent with acute myocardial infarction. Echocardiography revealed decreased left ventricular systolic function.
Gallium 67 myocardial scintigraphy was performed in 4 patients, 72 hours after intravenous injection of 9 mCi of gallium citrate Ga 67, and sooner than that in one. In all 5 patients, the results were positive, consistent with a diagnosis of acute myocarditis. One patient died of progressive heart failure 4 days after admission. Within 1 month of beginning medical therapy, the 4 surviving patients experienced resolution of abnormal ventricular function and symptoms. During a median follow-up period of 64 months, no cardiovascular events were observed, and the prognoses were deemed excellent.
We suggest that gallium 67 scintigraphy is a useful method by which to identify acute myocarditis in patients in whom the condition is suspected. To our knowledge, this is the 1st report of the use of gallium 67 myocardial scanning to differentiate acute myocarditis from acute myocardial infarction.
Key words: Diagnosis, differential; gallium radioisotopes/diagnostic use; heart/radionuclide imaging; methods; myocardial infarction/diagnosis; myocarditis/diagnosis/radionuclide imaging; sensitivity and specificity
The clinical spectrum of acute myocarditis ranges from asymptomatic electrocardiographic (ECG) abnormalities reported during community outbreaks of Coxsackie B viral infection to fulminant heart failure, cardiogenic shock, ventricular fibrillation, and death.1,2 A subset of patients may present with chest pain and ECG findings that suggest acute myocardial infarction. Acute myocarditis can mimic acute myocardial infarction in that the myocarditis is typically focal or multifocal in distribution on histologic study, segmental wall motion abnormalities may be present, and associated myocyte necrosis often leads to elevation of serum creatine kinase and cardiac troponin I.3,4 The standard diagnostic method, endomyocardial biopsy, is invasive and has a low diagnostic success rate.4–8 Gallium myocardial scanning has been suggested as a useful tool in the detection of myocarditis in patients who have Kawasaki disease.9 Gallium scanning has shown a sensitivity of 36% and a specificity of 98% in the detection of myocarditis in patients who have dilated cardiomyopathy.10 However, the role of gallium scanning has not been well established in patients who have acute myocarditis that mimics acute myocardial infarction. Differentiation between acute myocarditis and acute myocardial infarction is very important, because treatment differs markedly. This study investigated the role and effectiveness of gallium citrate 67 (Ga 67) scintigraphy in the diagnosis of acute myocarditis when acute myocardial infarction was initially suspected.
Patients and Methods
Patient Selection
From January 1998 through December 2001, we evaluated 315 consecutive patients who were admitted to our hospital with a diagnosis of acute myocardial infarction. This diagnosis required that a patient's condition satisfy 2 or more of these criteria: 1) chest pain suggestive of myocardial ischemia that lasted ≥30 minutes; 2) enzymatic evidence of acute myocardial necrosis (an increase in the serum creatine kinase level to ≥2 times the normal value, with a >4% increase in the creatine kinase–MB isoenzyme); and 3) new ECG changes, including the development of Q waves or ST-T changes, that lasted ≥48 hours.
Acute myocarditis was suspected when patients had no fever, presented with indistinct heart-failure symptoms (onset over a period of weeks to months before admission), and were hemodynamically stable or required only low doses of vasopressors (<5 μg of dopamine or dobutamine per kg/min) for the improvement of renal perfusion. From this subgroup of patients, study partici-pants were chosen on the basis of symptoms of upper respiratory or gastrointestinal tract infections (such as coughing, dizziness, vomiting, or diarrhea) that preceded the apparent acute myocardial infarction.
Table I shows the baseline characteristics of the 5 patients who met the criteria, provided written informed consent, and underwent Ga 67 myocardial scintigraphy for suspected acute myocarditis. There were 3 women and 2 men. Their ages ranged from 23 to 69 years (median, 32 yr). No patient had a cardiac risk factor or admitted to having used cocaine before the development of chest pain. At presentation, all patients had experienced <12 hours of typical anginal chest pain and a preceding illness that had involved the upper respiratory or gastrointestinal tract. One patient also presented with cardiogenic shock.
TABLE I. Baseline Characteristics, Results of Positive Gallium 67 Myocardial Scanning in the LV Myocardium, and Outcomes of 5 Patients
Evaluation of Clinical and Left Ventricular Function
Clinical presentations, coronary risk factors, ECG findings, durations of illness, and the locations and extent of left ventricular wall motion abnormalities were evaluated. Histories of smoking were determined by asking whether the patients had smoked more than 10 cigarettes per day for a year or more during their lifetimes. Diabetes mellitus was defined as diabetic disease that required dietary or medical therapy. Hypercholesterolemia was defined as a serum total cholesterol level of >200 mg/dL. Hypertension was defined as a blood pressure >140/90 mmHg or as a history of having received medical therapy for the condition. Initial left ventricular ejection fractions and segmental wall motion abnormalities were evaluated serially by 2-dimensional echocardiographic studies as recommended by the American Society of Echocardiography.11 Left ventricular dysfunction was defined as an ejection fraction <0.50.
Electrocardiographic Findings
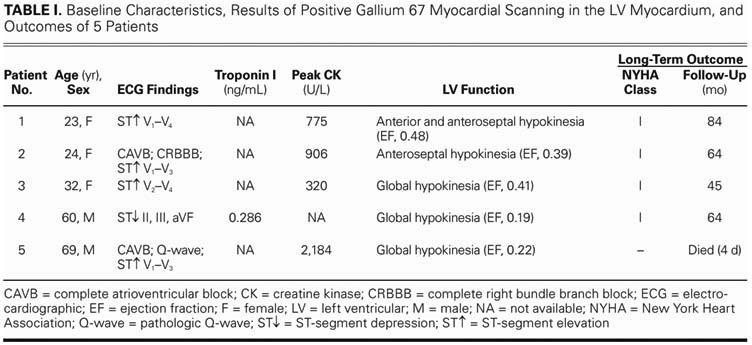
The varied ECG findings on admission included ST-segment elevation in the anterior precordial leads in patients 1, 2 (Fig. 1A), 3, and 5 (Fig. 2A). Also noted were ST-segment depression in patient 4 and pathologic Q waves in patient 5 (Fig. 2A). All patients had persistent anterior T-wave inversions during admission (Fig. 1B).
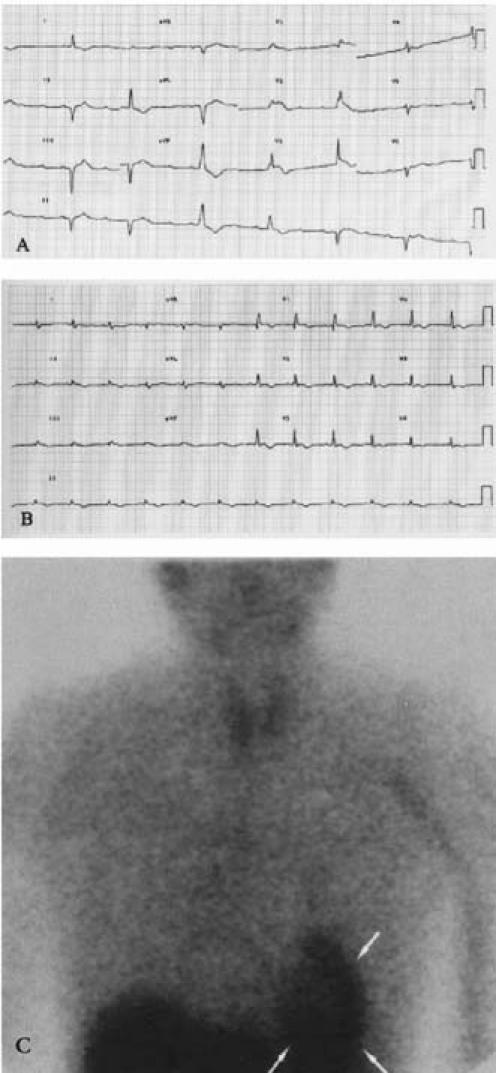
Fig. 1 Patient 2. A) Baseline electrocardiogram shows complete right bundle branch block, complete atrioventricular block, and ST-segment elevation in leads V1 through V3. B) Follow-up electrocardiogram (4 days later) shows sinus rhythm and resolution of the ST-segment elevation. C) Gallium 67 myocardial scanning in anterior–posterior projection shows diffuse uptake in the left ventricle (arrows).
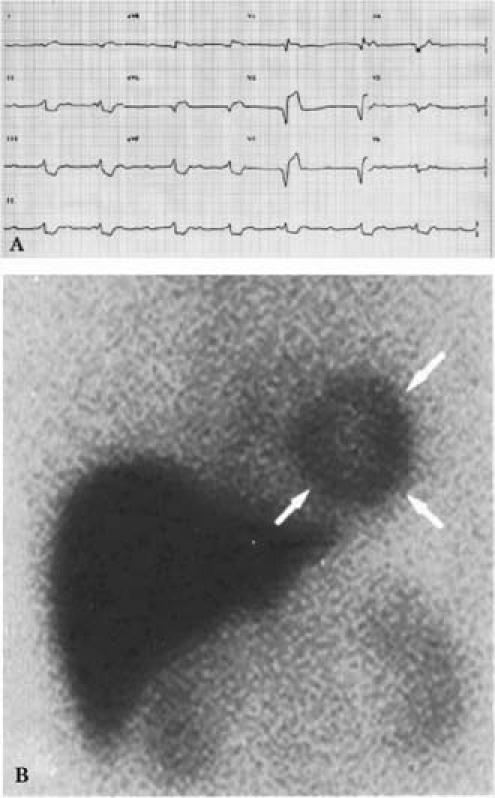
Fig. 2 Patient 5. A) Baseline electrocardiogram at presentation shows complete atrioventricular block, along with ST-segment elevation and a pathologic Q-wave in leads V1 through V3. There was associated cardiogenic shock. B) Gallium 67 imaging (left anterior–oblique 30° projection) shows diffuse and intense myocardial uptake (arrows).
Evaluation of the Coronary Arteries
Intracoronary methylergonovine maleate (Methergin®, Novartis International AG; Basel, Switzerland) testing was performed as previously described12 in order to exclude the possibility of coronary vasospasm in patients who exhibited no evidence of hemodynamically signi-ficant coronary artery disease (defined as >50% stenosis in the lu-men diameter of the major coronary arteries). A positive finding of intracoronary ergonovine provocation testing for coronary vasospasm was defined as a decrease >70% in the diameter of an arterial lumen, with concurrent chest pain and ischemic ST-segment changes during testing. Examination included lumen reduction, evaluation of chest pain, detection of simultaneous ST-segment changes in leads I and II by aVR ECG during intracoronary ergonovine testing, and (in patient 3 only) angiography. All 5 patients refused cardiac biopsy. Only patient 3 consented to undergo cardiac catheterization, which showed normal coronary arteries and no vasospasm.
After hospitalization and before Ga 67 scintigraphy, complete atrioventricular block occurred in patient 2 (Fig. 1A) and patient 5 (Fig. 2A). Patient 2, who also experienced right bundle branch block, required transvenous temporary pacemaker insertion via a femoral approach. Patient 5 experienced a return to sinus rhythm after 8 hours without intervention. Peak creatine kinase levels ranged from 320 to 2,184 U/L, with rise and fall following the pattern typical of acute myocardial infarction. Echocardiography revealed decreased left ventricular systolic function in all patients; ejection fractions ranged from 0.19 to 0.48.
Gallium 67 Myocardial Scintigraphy
The patients received a 9-mCi intravenous injection of Ga 67 on the 3rd day after admission, and Ga 67 myocardial scintigraphy was performed in 4 patients 72 hours after the injection. Due to the unstable condition of patient 5, who was experiencing refractory cardiogenic shock, the Ga 67 imaging of that patient was performed earlier, on day 4 after admission. The images were taken with a gamma camera with a large field of view (Varicam, GE Healthcare–Elscint; Haifa, Israel). The camera was capable of detecting the 93, 185, and 300 keV Ga 67 peaks to 625,000 counts.
For the whole-body survey, anterior and posterior views were obtained. If the results were ambiguous, right and left lateral views and single-photon-emission computed tomographic images of the chest were obtained, with most of the liver excluded from the region of interest. All images were processed by use of a nu–clear medicine computer with a 128 × 128 matrix (XPert Workstation, GE Healthcare) and enhanced by less than 20% of the maximal pixel. The activity of gallium uptake in the heart was compared with that in the sternum. Scans were interpreted as positive when the heart's uptake activity was equal to or greater than that in the sternum; had the activity been less than that in the sternum, a scan would have been considered equivocal.
Results
The Ga 67 myocardial imaging in all 5 patients was positive for acute myocarditis (Figs. 1C and 2B). Table I shows the scan results and the outcomes of the patients.
Patient 5 died 4 days after admission due to rapidly progressive heart failure and irreversible cardiogenic shock. Follow-up data on the surviving patients were obtained from the outcomes of their monthly visits to staff physicians in the outpatient clinic, and from hospital records and telephone interviews. The events recorded in this analysis were death (cardiac or noncardiac), nonfatal reinfarction, and recurrent angina.
The left ventricular ejection fractions of the 4 surviving patients returned to normal within 1 month after treatment with captopril, carvedilol, isosorbide dinitrate, and furosemide. During a median follow-up period of 64 months (range, 45–84 mo), the patients remained in New York Heart Association functional class I.
Discussion
This study found Ga 67 myocardial scintigraphy to be an invaluable means of differentiating acute myocarditis from acute myocardial infarction when endomyocardial biopsy and coronary angiography were not performed. To our knowledge, this is the 1st report of the use of Ga 67 myocardial scintigraphy to differentiate acute myocarditis from acute myocardial infarction.
Previous Studies
Despite the limited sensitivity and specificity of endo-myocardial biopsy, it remains the gold standard for diagnosis of acute myocarditis.4–8 This method has been criticized, however, for its disadvantages (associated morbidity, cost, and sampling error). Diagnosis of acute myocarditis depends in large part on clinical suspicion13 and should not be made on the basis of histologic findings alone.
It should be emphasized that Ga 67 scintigraphy detects areas of inflammation. Although early studies suggested that Ga 67 could be used to identify inflammatory components of myocardial infarction or bacterial endocarditis, this procedure has not proved clinically useful.14 Strain and associates15 found that a positive Ga 67 scan appeared to be concordant with a biopsy-proven diagnosis of inflammatory myocarditis. They found that Ga 67 scanning had a sensitivity of 44%, speci-ficity of 100%, and a positive predictive value of 58% in detecting inflammatory myocarditis when endomyocardial biopsy was used as the diagnostic standard. Similar sensitivity and specificity of Ga 67 scanning were also reported in patients who were found to have dilated cardiomyopathy.10
Creatine kinase levels are often elevated in acute myo-carditis. Smith and colleagues4 showed that measurement of cardiac troponin I more accurately detected myocyte injury in acute myocarditis than did interpretations of creatine kinase–MB isoenzyme levels. Myocardial infarction remains a relatively uncommon occurrence in patients younger than 40 years of age. Histologically verified myocarditis has been detected in a high proportion of patients younger than 40 years of age who have angiographically normal coronary arteries, but acute myocarditis that presents as acute myocardial infarction can also occur in older persons.16 In a study of younger patients aged 26.3 ± 10.0 years in whom myocarditis was suspected but had not been verified by biopsy, Paillard and coworkers17 found more abnormal regional wall motion on echocardiography than did Dec and associates.16
Present Study
In our series of patients, features suggestive of acute myocarditis included young age at presentation (3 patients were <35 years old), a history of diarrhea or flu-like symptoms within the preceding 4 weeks, and a paucity of conventional risk factors for accelerated atherosclerosis despite clinical signs, symptoms, and ECG findings that were highly suggestive of acute myo-cardial ischemia or infarction. In comparison with the patients of Dec and associates,16 our patients had a similar incidence of anterior ECG findings, higher creatine kinase elevation, and more wall motion abnormalities. The higher creatine kinase levels, which indicate a larger area of myocardial injury, are consistent with our findings of more wall motion abnormalities.
Because inflammation in myocarditis is potentially reversible, effective attempts to modify the natural course of this illness depend upon early identification of the myocardial infiltrates. Early Ga 67 imaging, especially when (as in our study) coronary angiography and endomyocardial biopsy are not performed, can identify acute myocarditis. Although Ga 67 imaging is useful in screening for inflammation, several technique-dependent sources of error can decrease its sensitivity. Scans should be performed 72 hours after injection of the isotope, because if imaging is performed at 24 hours, the Ga 67 may not clear the blood pool, and false-positive Ga 67 imaging will result. Also, imaging the heart with high background (inadequate clearance of Ga 67 from the cardiac blood pool) may decrease sensitivity if the imaging is performed at 48 hours. From our limited experience in patient 5, we speculate that Ga 67 imaging may be performed within 48 hours after isotope injection in patients who are responding poorly to medical treatment.
Positioning of the gamma camera is very important. Scanning should be performed in both the anterior and the oblique projections so that localized uptake can be confirmed as myocardial in origin. Most of the liver should be excluded from the field of view, because Ga 67 tends to accumulate in reticuloendothelial elements of the liver and bone marrow. This may introduce ambi-guities into regions of the scan where these tissues are adjacent to the left ventricle. A potential source of confusion is inadequate separation of normal activity in the liver from activity in myocarditis, especially when the latter is diaphragmatic in location.
Although immunosuppression has been reported to ameliorate autoimmune myocarditis,18 it is not recommended for the routine treatment of patients who have myocarditis.19 Supportive care remains the 1st line of therapy for patients who have acute myocarditis.13 We found that all of our surviving patients experienced a return to normal left ventricular function under supportive care within 1 month after Ga 67 scanning identified acute myocarditis.
Conclusion
The limited experience gained as a result of this study suggests that Ga 67 scintigraphy is a useful screening method by which to identify patients who have acute myocarditis that mimics acute myocardial infarction.
Footnotes
Address for reprints: Ming-Jui Hung, MD, Section of Cardiology, Department of Medicine, Chang Gung Memorial Hospital, 222 Mai-Chin Road, Keelung 204, Taiwan. E-mail: miran888@ms61.hinet.net
References
- 1.Spodick DH. Infection and infarction. Acute viral (and other) infection in the onset, pathogenesis, and mimicry of acute myocardial infarction. Am J Med 1986;81:661–8. [DOI] [PubMed]
- 2.Lopez JA, Treistman B, Massumi A. Myocarditis-associated ventricular fibrillation. An unusual cause of syncope in Wolff-Parkinson-White syndrome. Tex Heart Inst J 1995;22:335–8. [PMC free article] [PubMed]
- 3.Stratmann HG. Acute myocarditis versus myocardial infarction: evaluation and management of the young patient with prolonged chest pain–case reports. Angiology 1988;39(3 Pt 1):253–8. [DOI] [PubMed]
- 4.Smith SC, Ladenson JH, Mason JW, Jaffe AS. Elevations of cardiac troponin I associated with myocarditis. Experimental and clinical correlates. Circulation 1997;95:163–8. [PubMed]
- 5.Mason JW. Endomyocardial biopsy: the balance of success and failure. Circulation 1985;71:185–8. [DOI] [PubMed]
- 6.Narula J, Khaw BA, Dec GW Jr, Palacios IF, Southern JF, Fallon JT, et al. Brief report: recognition of acute myocarditis masquerading as acute myocardial infarction. N Engl J Med 1993;328:100–4. [DOI] [PubMed]
- 7.Mason JW, O'Connell JB, Herskowitz A, Rose NR, McMan-us BM, Billingham ME, Moon TE. A clinical trial of immunosuppressive therapy for myocarditis. The Myocarditis Treatment Trial Investigators. N Engl J Med 1995;333:269–75. [DOI] [PubMed]
- 8.Angelini A, Calzolari V, Calabrese F, Boffa GM, Maddalena F, Chioin R, Thiene G. Myocarditis mimicking acute myocardial infarction: role of endomyocardial biopsy in the differential diagnosis. Heart 2000;84:245–50. [DOI] [PMC free article] [PubMed]
- 9.Matsuura H, Ishikita T, Yamamoto S, Umezawa T, Ito R, Hashiguchi R, et al. Gallium-67 myocardial imaging for the detection of myocarditis in the acute phase of Kawasaki disease (mucocutaneous lymph node syndrome): the usefulness of single photon emission computed tomography. Br Heart J 1987;58:385–92. [DOI] [PMC free article] [PubMed]
- 10.O'Connell JB, Henkin RE, Robinson JA, Subramanian R, Scanlon PJ, Gunnar RM. Gallium-67 imaging in patients with dilated cardiomyopathy and biopsy-proven myocarditis. Circulation 1984;70:58–62. [DOI] [PubMed]
- 11.Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 1989;2:358–67. [DOI] [PubMed]
- 12.Hung MJ, Cherng WJ, Cheng CW, Li LF. Comparison of serum levels of inflammatory markers in patients with coronary vasospasm without significant fixed coronary artery disease versus patients with stable angina pectoris and acute coronary syndromes with significant fixed coronary artery disease. Am J Cardiol 2006;97:1429–34. [DOI] [PubMed]
- 13.Feldman AM, McNamara D. Myocarditis. N Engl J Med 2000;343:1388–98. [DOI] [PubMed]
- 14.Berger HJ, Zaret BL. Nuclear cardiology (first of two parts). N Engl J Med 1981;305:799–807. [DOI] [PubMed]
- 15.Strain JE, Fine EJ, Grose RM, Kramer DC, Cho S, Factor SM. Comparison of myocardial biopsy and gallium-67 imaging for diagnosing myocarditis [abstract]. Circulation 1983; 68:III–208.6883660
- 16.Dec GW Jr, Waldman H, Southern J, Fallon JT, Hutter AM Jr, Palacios I. Viral myocarditis mimicking acute myocardial infarction. J Am Coll Cardiol 1992;20:85–9. [DOI] [PubMed]
- 17.Paillard F, de Place C, Lebreton H, Mabo P, Almange C, Daubert C. Acute myocarditis with favourable outcome mimicking acute myocardial infarction [abstract]. Circulation 1990;82(4 Suppl III):III–118.
- 18.Bilinska ZT, Grzybowski J, Szajewski T, Stepinska J, Michalak E, Walczak E, et al. Active lymphocytic myocarditis treated with murine OKT3 monoclonal antibody in a patient presenting with intractable ventricular tachycardia. Tex Heart Inst J 2002;29:113–7. [PMC free article] [PubMed]
- 19.Heart Failure Society of America (HFSA) practice guidelines. HFSA guidelines for management of patients with heart failure caused by left ventricular systolic dysfunction–pharmacological approaches [published erratum appears in J Card Fail 2000;6:74]. J Card Fail 1999;5:357–82. [PubMed]


