Abstract
Objective
Eating in response to negative emotions is associated with binge or loss of control (LOC) eating in adults. Although children report engaging in LOC eating, data on emotional eating among youth are limited.
Method
We adapted the adult Emotional Eating Scale (Arnow et al., Int J Eat Disord, 18, 79–90, 1995) to be used with children and adolescents (EES-C). Fifty-nine overweight (BMI ≥ 95th percentile for age and sex) and 100 non-overweight (BMI 5th–94th percentile) participants (mean age ± SD 14.3 ± 2.4 years) completed the EES-C, and measures of recent LOC eating and general psychopathology. Test-retest reliability was assessed in 64 children over a 3.4 ± 2.6 month interval.
Results
A factor analysis generated three subscales: eating in response to anxiety, anger, and frustration (EES-C-AAF), depressive symptoms (EES-C-DEP), and feeling unsettled (EES-C-UNS). Internal consistency for the subscales was established; Cronbach’s alphas for the EES-C-AAF, EES-C-DEP, and EES-C-UNS were 0.95, 0.92, and 0.83, respectively. The EES-C had good convergent validity: children reporting recent LOC eating episodes scored higher on all subscales (p’s < 0.05). The EES-C-AAF and EES-CUNS subscales demonstrated good discriminant validity and the EES-C-DEP revealed adequate discriminant validity. Intra-class correlation coefficients revealed good temporal stability for each subscale (EES-C-AAF = 0.59, EES-C-DEP = 0.74, EES-C-UNS = 0.66; p’s < 0.001).
Conclusion
The EES-C has good convergent and discriminant validity, and test-retest reliability for assessing emotional eating in children. Further investigation is required to clarify the role emotional eating may play in children’s energy intake and body weight.
Keywords: emotional eating, binge eating, loss of control eating, children and adolescents, overweight
Introduction
Emotional eating has been defined as “eating in response to a range of negative emotions such as anxiety, depression, anger, and loneliness to cope with negative affect.”1 The relationship between emotional eating and episodes of binge eating in adults with binge eating disorder (BED; American Psychiatric Association)2 has been established.3–8 Adults with BED often endorse eating in response to negative affect both during and outside of binge episodes, and episodes of binge eating are often precipitated by stress and adverse mood states.4,7,8 Apart from being associated with binge eating, data suggest that adults who report eating in response to negative affect may be at risk for excessive weight gain.9
Despite data suggesting that only a small subset of adolescents10–13 and even fewer children14–16 meet full DSM-IV-TR criteria for BED, binge eating and the experience of loss of control (LOC) while eating (regardless of the amount of food ingested) appear to be quite common among youth.14,16–20 Therefore, increased attention has been paid to understanding the construct of binge and LOC eating in children. In an effort to characterize children who endorse such eating episodes, Marcus and Kalarchian21 proposed a new set of criteria for BED, designed specifically for children. Under Criterion B is “food seeking in response to negative affect (e.g., sadness, boredom, restlessness).” To date, only one recent study has tested this provisional diagnosis using a brief measure designed expressly to assess the proposed criteria.22 The Children’s Binge Eating Disorder Scale is a 7-item measure which includes Marcus and Kalarchian’s criteria. One item asks, “Do you ever eat because you feel bad, sad, bored, or any other mood?” to which children respond “yes” or “no.” Based on the administration of the Children’s Binge Eating Disorder Scale to 55 English-speaking children (aged 5–13 years) seeking weight loss treatment, 30% of the sample reported BED according to Marcus and Kalarchian’s criteria21 and 63% of all children in the sample endorsed eating in response to negative affect (question no. 3).22 Notably, emotional eating was the most commonly endorsed criterion in this treatment-seeking sample.
A limited number of studies outside of the U.S. have also examined emotional eating in adolescents and children. In two studies of adolescent females, the emotional eating subscale score of the Dutch Eating Behavior Questionnaire was significantly correlated with constructs of disturbed eating23,24 and symptoms of depression and anxiety.24 The latter study also reported that emotional eating was predictive of overeating in cross-sectional structural models.24 In studies of preadolescent children (9–14 years) using a parent report version of the Dutch Eating Behavior Questionnaire, the emotional eating subscale was unrelated to body weight in one sample of Italian children,25 but associated with obesity and recalled food intake among a Dutch-speaking sample.26 Finally, among overweight treatment-seeking children, those endorsing LOC eating were more likely to endorse emotional eating than those without LOC.15 These studies are limited in that the emotional eating subscale of the Dutch Eating Behavior Questionnaire does not differentiate between various types of emotions. Rather, eating in response to frustration (e.g., irritation, anger), sadness (e.g., depression, loneliness, disappointment, failure), and anxiety (e.g., fear, restlessness) are grouped into one subscale. Therefore, it is difficult to distinguish which aspects of emotional eating are most salient to disturbed eating and body weight in children using this existing measure.
To our knowledge, no measure has been designed to assess eating in response to a variety of emotions among children. Therefore, we adapted the Emotional Eating Scale (EES),27 a measure developed for use in obese adults with BED, for children and adolescents (EES-C). The EES for adults generates three subscales reflecting the urge to eat in response to: anger/frustration, anxiety, and depression. We hypothesized that the EES-C would: (1) have a sub-scale structure similar to that of the EES; (2) demonstrate good convergent validity, in that subjects reporting LOC eating episodes would have higher emotional eating scores than participants not endorsing LOC eating; (3) demonstrate good discriminant validity; given the increased specificity of the EES-C compared to other measures of emotional eating, each EES-C subscale would be uncorrelated with measures of corresponding general psychopathology; and (4) have good test-retest reliability, in that emotional eating at baseline and follow-up would demonstrate acceptable agreement.
Method
Participants
Subjects were 159 children and adolescents participating in nonintervention, metabolic studies at the National Institutes of Health (NIH). See Table 1. Recruitment is described elsewhere.14 None of the children was undergoing weight loss treatment, and all were aware that they would not receive treatment as part of the study protocol. Participants had no significant medical disease, and each child had normal hepatic, renal, and thyroid function. Children provided written assent and parents gave written consent for participation in the protocol. This study was approved by the National Institute of Child Health and Human Development Institutional Review Board, NIH.
TABLE 1.
Characteristics of study participantsa
| LOC Eating(n = 18) | No LOC Eating(n = 137) | p Value | |
|---|---|---|---|
| Age (y) | 13.1 (2.7) | 14.4 (2.3) | 0.07 |
| Sex (%) | 56.6% male; 44.4% female | 46.0% male; 54.0% female | 0.46 |
| Race | 61.1% White 33.3% Black 5.6% Hispanic 0.0% Other | 59.1% White 29.9% Black 4.4% Hispanic 6.6% Other | 0.73 |
| Pubertal stage (median) | 3.5 | 4.0 | 0.19 |
| Socioeconomic status (median) | 2.0 | 3.0 | 0.36 |
| BMI Z-scoreb | 1.6 (0.9) | 1.0 (1.1) | 0.05 |
LOC = loss of control based upon responses to the Questionnaire on Eating and Weight Patterns (QEWP-A).
Five children did not complete the QEWP-A; Values are expressed as frequency for categorical variables and mean (SD) for continuous variables.
BMI (body mass index) Z score is a standard deviation score for children’s BMI accounting for age and sex, calculated according to the Centers for Disease Control formula.28
Procedure
Participants completed all assessments during an out-patient visit. In a convenience sample of children who returned for another visit to the clinic between two weeks and up to a year following the baseline administration, the EES-C was administered a second time.
Questionnaires
The EES—Adapted for Children and Adolescents (EES-C), designed for use with 8 to 17-year-old children, was adapted from the EES27 for adults. The EES is a 25-item self-report measure used to assess the urge to cope with negative affect by eating.27 Respondents rate their desire to eat in response to each emotion on a 5-point scale (No desire, Small desire, Moderate desire, Strong urge, and Overwhelming urge to eat). Higher scores indicate a greater reported desire to eat in response to negative mood states. The EES generates three subscales based upon the mean of items reflecting the urge to eat in response to anger/frustration, anxiety, and depression. The EES has demonstrated good internal consistency,27,29 adequate temporal stability,27 and good construct27,29 and discriminant27 validity in adult samples.
In developing the EES-C, we made minor revisions to the EES’s instructions so that the language would be more accessible to children. In addition, we included an example question and response so that children observed that in response to feeling “starving” one might have “a very strong desire to eat.” A stem (“When I feel this way, I have”) was added to the list of emotions to which children respond with their desire to eat, on a 5-point scale from “I have no desire to eat” through “I have a very strong desire to eat.” The following emotion terms were changed: “inadequate” was replaced with “not doing enough,” “rebellious” was replaced with “disobedient,” “blue” replaced with “down,” and “jittery” with “stressed out.” During development of the questionnaire, we added the term “happy” to the end of the list, as recent data in adults suggests that eating in response to happiness is associated with binge eating and eating disordered psychopathology.8 We also added a column to the right of the 5-point scale options querying “On average, how many days a week do you eat because you feel this way?” to determine whether the approximate number of days per week that they ate in response to each emotion was associated with body weight (see Appendix).
To assess the presence or absence of LOC eating episodes, each participant completed the Questionnaire of Eating and Weight Patterns-Adolescent Version (QEWP-A).10 The QEWP-A has been used with children as young as 6 years48 and has adequate concurrent validity when correlated with measures of abnormal eating attitudes10 as well as acceptable test-retest reliability.30 Based on their responses to the QEWP-A, children were categorized into two eating behavior groups for analysis: those endorsing at least one eating episode with LOC within the past six months, and those with no reported LOC eating episodes.
To assess general depressive symptoms, each child completed the Children’s Depression Inventory (CDI),31 a 27-item measure used to evaluate depressive symptomatology in children. Internal consistency (alphas) for the CDI total score ranges from 0.70 to 0.86.32 Anxiety was measured with the State-Trait Anxiety Inventory for Children (STAIC),33 a 40-item self-report measure of state and trait anxiety developed for use with elementary school children. In a sample of school-aged children, internal consistency for the state scale was good, with alphas of 0.82 for males and 0.87 for females.33 Similarly, alphas for the trait anxiety scale were 0.78 and 0.81 for males and females, respectively.33 Participants’ parents completed the Child Behavior Checklist for ages 4–18 (CBCL),34 an empirically derived measure with excellent norms that assesses a range of internalizing and externalizing symptoms and which yields age-appropriate T-scores for both types of problems. The CBCL has established reliability; internal consistency for the Internalizing scale (α = 0.90), the Externalizing scale (0.94) and Total problems scale (0.97).35
Physical Measures
Weight and height were measured as described previously36 using calibrated electronic instruments. BMI standard deviation (BMI-Z) scores were calculated according to the Centers for Disease Control and Prevention 2000 standards.28
Pubertal breast and pubic hair stage were assigned through physical examination by a pediatric endocrinologist or trained pediatric nurse practitioner to one of the five standards of Tanner.37,38 Testicular volume (in cc) for boys was also assessed using an orchidometer. Pubertal stage and testicular volume can be considered surrogate measurements of neurocognitive maturity as well as objective measures of physical maturity.37,38
Statistical Analysis
All analyses were conducted using SPSS for Windows, 12.0.39 To determine whether the EES-C generated sub-scales similar to the original EES, all items (other than “happy”) from the first administration of the EES-C were subjected to a principal components analysis with a vari-max rotation. Internal consistency was examined using item-total correlations and Cronbach’s alpha’s are reported. To assess convergent validity, comparisons between groups (LOC versus No LOC) were performed using analysis of covariance (ANCOVA). To determine relevant covariates, we entered age, race, socioeconomic status (SES),40 sex, pubertal stage and BMI-Z score into each full model. A Bonferroni-Hochberg post hoc correction was applied for multiple comparisons within each family of variables. Means ± standard errors are reported, with means adjusted for ANCOVA models given where appropriate. To assess discriminant validity, partial correlations were used to determine whether or not the EES-C subscale scores were significantly related to the corresponding measure of general psychopathology. For the assessment of test-retest reliability, intraclass correlations were calculated to determine the degree of agreement between the first and second administrations of the EES-C. Differences and associations were considered significant when p values were ≤0.05.
Results
Participants were 159 children (37.1% were overweight, BMI ≥ 95th percentile for age and sex) ranging in age from 8 to 18 years. Based on their responses to the QEWP-A, 18 (11.7%) children endorsed engaging in LOC eating at least once over the past six months. Sample demographics are presented in Table 1.
Of the 26 items listed on the EES-C, children most commonly endorsed eating in response to feeling happy (68.4%), while feeling bored was the second most common emotion (55.7%) reported. Table 2 lists the percentage of children endorsing each item on the measure.
TABLE 2.
Percentage of participants endorsing eating in response to each EES-C emotion
| Percentage (%) Endorsed | |
|---|---|
| Happya | 68.4 |
| Bored | 55.7 |
| Excited | 55.3 |
| Worn out | 53.5 |
| Not doing enough | 52.2 |
| Lonely | 45.3 |
| Sad | 45.3 |
| Stressed out | 44.7 |
| Discouraged | 43.4 |
| Nervous | 42.1 |
| Down | 40.9 |
| Worried | 39.6 |
| Uneasy | 39.0 |
| Frustrated | 38.4 |
| Resentful | 37.7 |
| Irritated | 36.7 |
| Upset | 36.5 |
| Confused | 35.4 |
| Shaky | 34.6 |
| Helpless | 34.0 |
| On edge | 33.3 |
| Angry | 32.1 |
| Guilty | 32.1 |
| Jealous | 32.1 |
| Furious | 28.3 |
| Disobedient | 23.9 |
EES-C, Emotional Eating Scale adapted for Children and Adolescents.
The item “happy” was added to a revised version of the EES-C and, therefore, was completed by a subset of the sample (n = 38).
Conducting a factor analysis using a scree-test and simple structure criteria using the 25 items from the original EES (i.e., not containing the additional item, “happy”), three factors were extracted that accounted for 67.2% of the variance. The first factor had loadings from 12 items, accounting for 29.4% of the variance (Eigenvalue = 14.3), and represented eating in response to anxiety, anger and frustration (anxiety/anger/frustration subscale; EES-C-AAF). Seven items comprised the second factor, which was related to symptoms of depression (depression subscale; EES-C-DEP). This factor accounted for 22.9% of the variance (Eigenvalue = 1.5). The third factor consisted of four items (14.9% of the variance; Eigenvalue = 1.0) and represented eating in response to feeling unsettled (unsettled subscale; EES-C-UNS). Only two items, “shaky” and “worn out,” did not load onto any of the factors. The rotated component matrix of the three factors is presented in Table 3.
TABLE 3.
Rotated component matrix
| Factor 1 EES-C-AAF | Factor 2 EES-C-DEP | Factor 3 EES-C-UNS | |
|---|---|---|---|
| Resentful | 0.70 | ||
| Discouraged | 0.58 | 0.63 | |
| Shaky | |||
| Worn out | |||
| Not doing enough | 0.57 | ||
| Excited | 0.52 | ||
| Disobedient | 0.72 | ||
| Down | 0.84 | ||
| Stressed out | 0.79 | ||
| Sad | 0.73 | ||
| Uneasy | 0.73 | ||
| Irritated | 0.64 | 0.50 | |
| Jealous | 0.68 | ||
| Worried | 0.60 | 0.62 | |
| Frustrated | 0.60 | ||
| Lonely | 0.51 | 0.68 | |
| Furious | 0.79 | ||
| On edge | 0.73 | ||
| Confused | 0.74 | ||
| Nervous | 0.68 | ||
| Angry | 0.64 | ||
| Guilty | 0.69 | ||
| Bored | 0.58 | ||
| Helpless | 0.61 | ||
| Upset | 0.63 | 0.57 |
EES-C-AAF, emotional eating scale adapted for children and adolescents-anger, anxiety and frustration subscale; EES-C-DEP, emotional eating scale adapted for children and adolescents-depression subscale; EES-C-UNS, emotional eating scale adapted for children and adolescents-unsettled subscale.
Internal Consistency
All three subscales demonstrated good internal consistency for the first administration of the EES-C. Cronbach’s alphas for the EES-C-AAF, EES-C-DEP, and EES-C-UNS were 0.95, 0.92, and 0.83, respectively. Since the items “discouraged, irritated, worried, lonely and upset” loaded onto more than one subscale, we removed these items in a second analysis of internal consistency. The removal of these items did not improve or substantially change internal consistency of the EES-C subscales in that alphas for the EES-C-AAF, EES-C-DEP, and EES-C-UNS were 0.94, 0.89, and 0.73, respectively. Cronbach’s alphas for the second administration were 0.91 (EES-C-AAF), 0.87 (EES-C-DEP), and 0.65 (EES-C-UNS).
Convergent Validity
Compared to boys, girls were significantly more likely to endorse eating in response to depressive symptoms (0.71 ± 0.1 vs. 1.1 ± 0.1, p = 0.007) and to feeling unsettled (0.46 ± 0.1 vs. 0.76 ± 0.1, p = 0.016). Participants with greater pubertal development were more likely to report eating in response to depressive symptoms (r = 0.20, p = 0.013). Therefore, we controlled for sex in analyses involving the EES-C-DEP and EES-C-UNS subscales and for Tanner stage in models of the EES-C-DEP scale. Participants endorsing LOC had significantly higher EES-C scores on all three subscales. Those with LOC had significantly higher EES-C-AAF (F = 5.4, p < 0.02), EES-C-DEP (F = 13.2, p < 0.001), and EES-C-UNS (F = 12.4, p = 0.001) scores compared to those without LOC, suggesting that our measure of emotional eating demonstrated good convergent validity with LOC eating (Fig. 1). Although overweight children were more likely to endorse LOC eating (p = 0.04), none of the EES-C subscales were significantly related to BMI-Z score or overweight as defined by a BMI ≥ 95th percentile for age and sex41 (all p’s > 0.2). Moreover, the average number of days per week that children endorsed eating in response to their emotions was unassociated with BMI Z-score (r2 = 0.004, p = 0.78).
FIGURE 1.
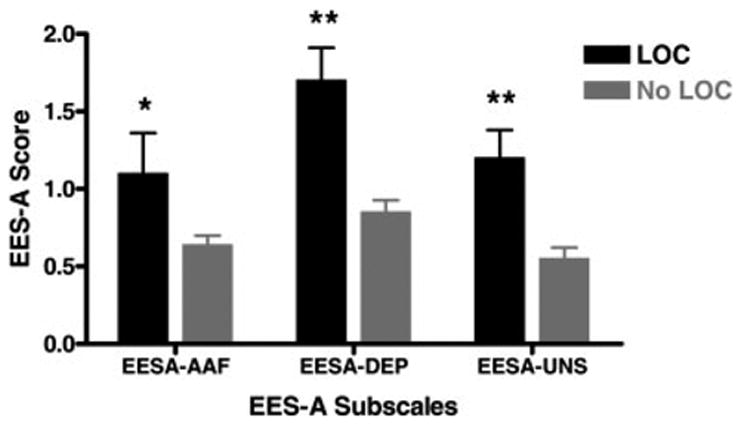
Emotional eating scale—adapted for children and adolescents subscales by LOC eating status. Participants endorsing LOC reported significantly higher EES-C-AAF ( p < 0.02), EES-C-DEP ( p < 0.001), and EES-C-UNS ( p = 0.001) scores compared to those without LOC.
Discriminant Validity
To determine whether the EES-C-AAF subscale discriminated from measures of general anxiety, anger and frustration, we conducted correlations with the STAIC trait and state anxiety scales, and the externalizing problems T-score of the CBCL. The EES-C-AAF was unrelated to measures of trait anxiety (r = 0.08; p = 0.35), state anxiety (r = 0.03; p = 0.72), or externalizing behaviors (r = 0.05; p = 0.55), indicating that the subscale captures a construct distinct from general anxiety or misconduct related to anger and/or frustration.
After accounting for sex and pubertal stage, the EES-C-DEP subscale was significantly related to the CDI Total score (r = 0.28, p = 0.001), indicating inadequate discriminant validity. However, to determine whether or not the EES-C-DEP captured a specific construct in addition to depressive symptoms, we examined the subscale by LOC status after accounting for the CDI Total score. Participants with LOC continued to have significantly higher EES-C-DEP scores compared to those without LOC (1.5 ± 0.22 vs. 0.87 ± 0.08; F = 6.4; p = 0.01), suggesting that the subscale may discriminate from general measures of depressive symptomatology.
The EES-C-UNS subscale was unrelated to the CBCL internalizing (r = 0.10, p = 0.24) or externalizing (r = 0.002, p = 0.98) T-score scales. Since the EES-C-UNS is not similar to any of the adult loadings, we investigated whether or not it was related to measures of depressive symptoms and anxiety. The EES-C-UNS subscale was unrelated to any of the CDI subscales or total score after correcting for multiple comparisons, and was unrelated to state and trait anxiety (Data not shown, but available upon request).
Test-Retest Reliability
To assess the test-retest reliability of the EES-C, 64 participants completed the measure twice, over an average interval period of 3.35 (SD: 2.6) months ranging between 0.39 and 11.6 months. Intraclass correlations demonstrated good agreement between the first and second administrations of the questionnaire. Intraclass correlations for the EES-C-AAF sub-scale (0.59), EES-C-DEP subscale (0.74), and the EES-C-UNS subscale (0.66; all p’s < 0.001) are indicative of the temporal stability of the measure.
Conclusion
In this investigation of a pediatric adaptation of the adult Emotional Eating Scale,27 we found that the EES—Adapted for Children and Adolescents generated child-specific subscales that differed from the adult version. All three subscales demonstrated good convergent validity with LOC eating, and the Anxiety/Anger/Frustration and Unsettled subscales exhibited good discriminant validity with measures of general psychopathology. Although the Depression subscale correlated significantly with the Children’s Depression Inventory, it appears to assess a construct of eating in response to depressive symptoms above and beyond children’s reports of depressive symptoms. After controlling for reported depressive symptoms, children with LOC eating had significantly higher EES-C Depression scores than children without LOC. Nevertheless, the lack of definitive discriminant validity may be related to limitations of the Children’s Depression Inventory and to measuring depressive symptoms in children. Indeed, data suggest that the CDI can be an unstable measure,42 and depressive symptoms can vary greatly based upon age and sex.43 All three subscales exhibited good test-retest reliability over a three and a half month period. While the long and variable interval between the first and second administrations of the measure may not have been optimal, it speaks to the stability of the EES-C as the longer the interval, the more likely that individuals completing the measure may have changed their behaviors and responses.
A factor analysis of the EES-C generated somewhat different subscales than the original EES. The EES-C-AAF subscale included a number of the same items that comprise both the EES Anger/Frustration and EES Anxiety subscales. It maybe that children are unable to distinguish between eating in response to emotions during which they feel negatively energized. As such, youth may experience such feelings similarly and cluster them together as a general construct. By contrast, the items from the EES-C-DEP subscale were primarily concordant with the EES, suggesting that similar to the adult subscale, a subset of children do appear to eat specifically in response to feeling depressed. Interestingly, internal consistency for the EES-C subscales was quite good. Cronbach’s α for the EES-C-AAF was 0.95, while the alphas for the EES Anger/Frustration and Anxiety subscales were both 0.78. Similarly, the EES-C-DEP scale had an α of 0.92, which is compared to the 0.72 α for the EES depression subscale.27 The EES-C-UNS subscale is new, unrelated to any adult loading, and is composed of three items from the Anger/Frustration subscale and one item (excited) from the Anxiety subscale of the original EES. Eating in response to feeling unsettled maybe a construct particular to youth and be representative of feelings of confusion. Adults may have a greater capacity to identify their emotions and, as a result, the unsettled scale has not emerged in adult samples. However, further data replicating this subscale are required for a number of reasons; first, only four items generated the EES-C-UNS, likely contributing to the large difference between internal consistency alphas at the first and second administration of the measure (0.83 at Time 1 and 0.65 at Time 2); the items do not appear to generate a distinct construct; and the scale accounted for less than 15% of the variance. Moreover, future research should consider incorporating related items to the EES-C-UNS subscale to determine whether eating in response to feeling unsettled is a viable and meaningful construct in children and adolescents.
In our sample, eating in response to feeling “happy” was the most commonly endorsed emotion. Although this finding should be interpreted cautiously since only a subset of children completed the EES-C version that included the additional item, it may be consistent with the hypothesis that children who report LOC eating episodes may do so during happy occasions, such as celebrations or at restaurants, when more palatable foods may be available. Alternatively, children in our sample may have interpreted this item as reflecting an association rather than directionality (for example, “I ate while I was happy,” as opposed to, “I ate in response to feeling happy”). Eating in response to boredom was the second most commonly endorsed emotion. Based upon their clinical work with children, Marcus and Kalarchian provided eating in response to “sadness,” “boredom,” and “restlessness” as examples to describe emotional eating in their proposed criteria for childhood BED.21 Moreover, to assess emotional eating in Shapiro and colleagues’ Children’s Binge Eating Disorder Scale, the questionnaire asks, “Do you ever eat because you feel bad, sad, bored, or any other mood?”22 Further research is required to determine how children interpret the construct of boredom and why a substantial percentage of children feel compelled to eat in response to the emotion.
Similar to adults with binge eating and consistent with Goossens et al.’s findings among overweight youth,15 children who endorsed LOC eating were more likely to report eating in response to negative emotions. Interestingly, although similar numbers of boys and girls reported LOC eating, girls were more likely to report eating in response to depressive symptoms and to feeling unsettled than were boys. This finding is also supported by the adult literature.5 As suggested by research in the area of sex differences and psychopathology, gender-specific behaviors and socialization may interact with developmental challenges that put girls at greater risk for depressive symptoms44–47 and potentially eating in response to emotions of depression.
We found that none of the EES-C subscales were related to body size. Furthermore, the number of days that children reported emotional eating over the past week was unrelated to BMI Z-score. Our findings support those of Caccialanza et al. who found no relationship between body weight and emotional eating among youth of all weight strata25 and to some8 but not all9 adult studies. Although we did not find a cross-sectional relationship between body size and emotional eating, prospective data are required to determine whether or not children who eat in response to emotional cues are at greater risk for excessive weight gain in the future.
Strengths of the present study include the relatively large sample size, the representation of both Caucasian and African American youth, as well as the use of non-treatment-seeking, healthy children as participants. However, the present study is limited in that participants were not recruited in a population-based fashion. Families in the studied sample chose to respond to our notices and thus may be more health-conscious than the general population, limiting the external validity of the study. Furthermore, because the factors generated from our sample did not replicate the adult sub-scales, the measures of general psychopathology may have not fully captured the same constructs as our EES-C subscales. Further exploration of the EES-C using a wider range of measures of child psychopathology is required. A final limitation is the finding that a number of items loaded onto more than one subscale. While removal of these items did not impact the internal consistency of the scales, it could be argued that these items be removed from future iterations of the EES-C. Moreover, since data suggest that self-report and interview methods are non-concordant with regard to the assessment of LOC eating in children,48 another potential limitation is our use of a questionnaire to examine eating behaviors. Finally, until the EES-C factor structure is replicated with independent samples, findings from the present investigation should be regarded as preliminary.
In conclusion, our adapted version of the EES (1) appears to demonstrate good convergent validity and temporal stability. The Anxiety/Anger/Frustration and Unsettled subscales were discriminated well from measures of general psychopathology, and the Depression subscale demonstrated adequate discriminant validity. Given that children endorse eating in response to a variety of emotions, we believe the EES-C may prove useful for investigations of emotional eating in youth. Moreover, with further replication of its psychometric properties, the EES-C may serve as tool to identify targets for treatment intervention with children who are overweight, at-risk for overweight or those presenting with disordered eating patterns.
Acknowledgments
We thank Dr. Bruce Arnow for granting permission to adapt the Emotional Eating Scale.
Appendix. EES Adapted for Children and Adolescents
We all react to different feelings in different ways. Some types of feelings make us want to eat. Please let us know how much the following feelings make you want to eat by checking the appropriate box.
| EXAMPLE | ||||||
|---|---|---|---|---|---|---|
| WHEN I FEEL THIS WAY | I have no desire to eat | I have a small desire to eat | I have a moderate desire to eat | I have a strong desire to eat | I have a very strong desire to eat | On average, how many days a week do you eat because you feel this way? (0–7) |
| Starving | X | 3 | ||||
| WHEN I FEEL THIS WAY | I have no desire to eat | I have a small desire to eat | I have a moderate desire to eat | I have a strong desire to eat | I have a very strong desire to eat | On average, how many days a week do you eat because you feel this way? (0–7) |
| Resentful | ||||||
| Discouraged | ||||||
| Shaky | ||||||
| Worn Out | ||||||
| Not doing enough | ||||||
| Excited | ||||||
| Disobedient | ||||||
| Down | ||||||
| Stressed out | ||||||
| Sad | ||||||
| Uneasy | ||||||
| Irritated | ||||||
| Jealous | ||||||
| Worried | ||||||
| Frustrated | ||||||
| Lonely | ||||||
| Furious | ||||||
| On edge | ||||||
| Confused | ||||||
| Nervous | ||||||
| Angry | ||||||
| Guilty | ||||||
| Bored | ||||||
| Helpless | ||||||
| Upset | ||||||
| Happy | ||||||
Footnotes
Portions of this manuscript were presented at the 2006 Pediatric Academic Societies’ Annual Meeting.
This article is a U.S. Government work and, as such, is in the public domain in the United States of America.
Supported by grant ZO1-HD-00641 (NICHD, NIH) from NIH to JAY. Dr. J. Yanovski is a Commissioned Officer in the United States Public Health Services, DHHS.
References
- 1.Faith MS, Allison DB, Geliebter A. Emotional eating and obesity: Theorectical considerations and practical recommendations. In: Dalton S, editor. Obesity and Weight Control: The Health Professional’s Guide to Understanding and Treatment. Gaithersburg, MD: Aspen; 1997. pp. 439–465. [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 3.Eldredge KL, Agras WS. Weight and shape overconcern and emotional eating in binge eating disorder. Int J Eat Disord. 1996;19:73–82. doi: 10.1002/(SICI)1098-108X(199601)19:1<73::AID-EAT9>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 4.Kenardy J, Arnow B, Agras WS. The aversiveness of specific emotional states associated with binge-eating in obese subjects. Aust N Z J Psychiatry. 1996;30:839–844. doi: 10.3109/00048679609065053. [DOI] [PubMed] [Google Scholar]
- 5.Tanofsky MB, Wilfley DE, Spurrell EB, Welch R, Brownell KD. Comparison of men and women with binge eating disorder. Int J Eat Disord. 1997;21:49–54. doi: 10.1002/(sici)1098-108x(199701)21:1<49::aid-eat6>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 6.Greeno CG, Wing RR, Shiffman S. Binge antecedents in obese women with and without binge eating disorder. J Consult Clin Psychol. 2000;68:95–102. [PubMed] [Google Scholar]
- 7.Telch CF, Agras WS. Do emotional states influence binge eating in the obese? Int J Eat Disord. 1996;20:271–279. doi: 10.1002/(SICI)1098-108X(199611)20:3<271::AID-EAT6>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 8.Masheb RM, Grilo CM. Emotional overeating and its associations with eating disorder psychopathology among overweight patients with binge eating disorder. Int J Eat Disord. 2006;39:141–146. doi: 10.1002/eat.20221. [DOI] [PubMed] [Google Scholar]
- 9.Eldredge KL, Agras WS, Arnow B. The last supper: Emotional determinants of pretreatment weight fluctuation in obese binge eaters. Int J Eat Disord. 1994;16:83–88. doi: 10.1002/1098-108x(199407)16:1<83::aid-eat2260160109>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 10.Johnson WG, Grieve FG, Adams CD, Sandy J. Measuring binge eating in adolescents: Adolescent and parent versions of the questionnaire of eating and weight patterns. Int J Eat Disord. 1999;26:301–314. doi: 10.1002/(sici)1098-108x(199911)26:3<301::aid-eat8>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 11.Stice E, Killen JD, Hayward C, Taylor CB. Age of onset for binge eating and purging during late adolescence: A 4-year survival analysis. J Abnorm Psychol. 1998;107:671–675. doi: 10.1037//0021-843x.107.4.671. [DOI] [PubMed] [Google Scholar]
- 12.Glasofer DR, Tanofsky-Kraff M, Eddy KT, Yanovski SZ, Theim K, Mirch M, et al. Binge eating in overweight treatment-seeking adolescents. J Pediatr Psychol. 2007;32:95–105. doi: 10.1093/jpepsy/jsl012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Decaluwe V, Braet C. Prevalence of binge-eating disorder in obese children and adolescents seeking weight-loss treatment. Int J Obes Relat Metab Disord. 2003;27:404–409. doi: 10.1038/sj.ijo.0802233. [DOI] [PubMed] [Google Scholar]
- 14.Tanofsky-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, Yanovski JA. Eating disordered behaviors, body fat, and psychopathology in overweight and normal weight children. J Consult Clin Psychol. 2004;72:53–61. doi: 10.1037/0022-006X.72.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goossens L, Braet C, Decaluwe V. Loss of control over eating in obese youngsters. Behav Res Ther. 2007;45:1–9. doi: 10.1016/j.brat.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 16.Morgan C, Yanovski S, Nguyen T, McDuffie J, Sebring N, Jorge M, et al. Loss of control over eating, adiposity, and psychopathology in overweight children. Int J Eat Disord. 2002;31:430–441. doi: 10.1002/eat.10038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Decaluwe V, Braet C, Fairburn CG. Binge eating in obese children and adolescents. Int J Eat Disord. 2003;33:78–84. doi: 10.1002/eat.10110. [DOI] [PubMed] [Google Scholar]
- 18.Greenfeld D, Quinlan DM, Harding P, Glass E, Bliss A. Eating behavior in an adolescent population. Int J Eat Disord. 1987;6:99–111. [Google Scholar]
- 19.Isnard P, Michel G, Frelut ML, Vila G, Falissard B, Naja W, et al. Binge eating and psychopathology in severely obese adolescents. Int J Eat Disord. 2003;34:235–243. doi: 10.1002/eat.10178. [DOI] [PubMed] [Google Scholar]
- 20.Tanofsky-Kraff M, Faden D, Yanovski SZ, Wilfley DE, Yanovski JA. The perceived onset of dieting and loss of control eating behaviors in overweight children. Int J Eat Disord. 2005;38:112–122. doi: 10.1002/eat.20158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marcus MD, Kalarchian MA. Binge eating in children and adolescents. Int J Eat Disord. 2003;34 (Suppl):S47–S57. doi: 10.1002/eat.10205. [DOI] [PubMed] [Google Scholar]
- 22.Shapiro JR, Woolson SL, Hamer RM, Kalarchian MA, Marcus MD, Bulik CM. Evaluating binge-eating disorder in children: Development of the children’s binge eating disorder scale (C-BEDS) Int J Eat Disord. 2007;40:82–89. doi: 10.1002/eat.20318. [DOI] [PubMed] [Google Scholar]
- 23.van Strien T. On the relationship between dieting and “obese” and bulimic eating patterns. Int J Eat Disord. 1996;19:83–92. doi: 10.1002/(SICI)1098-108X(199601)19:1<83::AID-EAT10>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 24.van Strien T, Engels RC, Van Leeuwe J, Snoek HM. The Stice model of overeating: Tests in clinical and non-clinical samples. Appetite. 2005;45:205–213. doi: 10.1016/j.appet.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 25.Caccialanza R, Nicholls D, Cena H, Maccarini L, Rezzani C, Antonioli L, et al. Validation of the Dutch eating behaviour questionnaire parent version (DEBQ-P) in the Italian population: A screening tool to detect differences in eating behaviour among obese, overweight and normal-weight preadolescents. Eur J Clin Nutr. 2004;58:1217–1222. doi: 10.1038/sj.ejcn.1601949. [DOI] [PubMed] [Google Scholar]
- 26.Braet C, Van Strien T. Assessment of emotional, externally induced and restrained eating behaviour in nine to twelve-year-old obese and non-obese children. Behav Res Ther. 1997;35:863–873. doi: 10.1016/s0005-7967(97)00045-4. [DOI] [PubMed] [Google Scholar]
- 27.Arnow B, Kenardy J, Agras WS. The emotional eating scale: The development of a measure to assess coping with negative affect by eating. Int J Eat Disord. 1995;18:79–90. doi: 10.1002/1098-108x(199507)18:1<79::aid-eat2260180109>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 28.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC growth charts for the United States: Methods and development. Vital Health Stat 11. 2002;246:1–190. [PubMed] [Google Scholar]
- 29.Waller G, Osman S. Emotional eating and eating psychopathology among non-eating-disordered women. Int J Eat Disord. 1998;23:419–424. doi: 10.1002/(sici)1098-108x(199805)23:4<419::aid-eat9>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 30.Johnson WG, Kirk AA, Reed AE. Adolescent version of the questionnaire of eating and weight patterns: Reliability and gender differences. Int J Eat Disord. 2001;29:94–96. doi: 10.1002/1098-108x(200101)29:1<94::aid-eat16>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 31.Kovacs M. Children’s Depression Inventory (CDI) Manual. Toronto, ON: Multi-Health Systems; 1992. [Google Scholar]
- 32.Kovacs M. The children’s depression inventory (CDI) Psycho-pharmacol Bull. 1985;21:995–998. [PubMed] [Google Scholar]
- 33.Spielberger CD, Edwards CD, Lushene RE, Montuori J, Platzek D. STAIC Preliminary Manual. Palo Alto, CA: Consulting Psychologist Press; 1973. [Google Scholar]
- 34.Achenbach TM, Elderbrock C. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington, VT: Department of Psychiatry, University of Vermont; 1991. [Google Scholar]
- 35.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms and Profiles. Burlington, VT: Research Center for Children, Youth, and Families, University of Vermont; 2001. [Google Scholar]
- 36.Nicholson JC, McDuffie JR, Bonat SH, Russell DL, Boyce KA, McCann S, et al. Estimation of body fatness by air displacement plethysmography in African American and white children. Pediatric Res. 2001;50:467–473. doi: 10.1203/00006450-200110000-00008. [DOI] [PubMed] [Google Scholar]
- 37.Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969;44:291–303. doi: 10.1136/adc.44.235.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in boys. Arch Dis Child. 1970;45:13–23. doi: 10.1136/adc.45.239.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.SPSS 12.0. Chicago, IL: SPSS; 2004. [Google Scholar]
- 40.Hollingshead A. Four factor index of social status. New Haven: Yale University; 1975. [Google Scholar]
- 41.Ogden CL, Kuczmarski RJ, Flegal KM, Mei Z, Guo S, Wei R, et al. Centers for disease control and prevention 2000 growth charts for the United States: Improvements to the 1977 National Center for health statistics version. Pediatrics. 2002;109:45–60. doi: 10.1542/peds.109.1.45. [DOI] [PubMed] [Google Scholar]
- 42.Cole DA, Martin NC. The longitudinal structure of the children’s depression inventory: Testing a latent trait-state model. Psychol Assess. 2005;17:144–155. doi: 10.1037/1040-3590.17.2.144. [DOI] [PubMed] [Google Scholar]
- 43.Angold A, Erkanli A, Silberg J, Eaves L, Costello EJ. Depression scale scores in 8–17-year-olds: Effects of age and gender. J Child Psychol Psychiatry. 2002;43:1052–1063. doi: 10.1111/1469-7610.00232. [DOI] [PubMed] [Google Scholar]
- 44.Brody L, Hall J. Gender and emotion. In: Lewis M, Haviland J, editors. The Handbook of Emotions. New York: Guilford; 1993. pp. 447–460. [Google Scholar]
- 45.Crick NR, Zahn-Waxler C. The development of psychopathology in females and males: Current progress and future challenges. Dev Psychopathol. 2003;15:719–742. [PubMed] [Google Scholar]
- 46.Zahn-Waxler C, Klimes-Dougan B, Slattery MJ. Internalizing problems of childhood and adolescence: Prospects, pitfalls, and progress in understanding the development of anxiety and depression. Dev Psychopathol. 2000;12:443–466. [PubMed] [Google Scholar]
- 47.Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychol Bull. 1994;115:424–443. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- 48.Tanofsky-Kraff M, Morgan CM, Yanovski SZ, Marmarosh C, Wilfley DE, Yanovski JA. Comparison of assessments of children’s eating-disordered behaviors by interview and questionnaire. Int J Eat Disord. 2003;33:213–224. doi: 10.1002/eat.10128. [DOI] [PubMed] [Google Scholar]


