The case: A 16-year-old pregnant teenager (gravida 1, para 0) presented at 32 weeks' gestation to a local emergency department in late December 2006 with a 5-day history of increasing dyspnea, low-grade fever, nausea and vomiting. She had taken amoxicillin for 3 days based on a presumptive diagnosis of pneumonia, but without any clinical benefit. Her past medical history included mild asthma. She was in acute respiratory distress (respiratory rate 44 breaths/min; oxygen saturation 54% on room air) and required immediate intubation and transfer to the intensive care unit. Despite empiric intravenous therapy with ceftriaxone (1 g/d), azithromycin (250 mg/d), betamethasone and heparin, she remained hypoxic. Chest radiography revealed bilateral, lower lobe, dense consolidation, and computed tomography was negative for pulmonary embolus. When her condition failed to improve, the patient was transferred to a tertiary care centre, mechanical ventilation with high-frequency oscillation was begun, the ceftriaxone dose was increased (2 g every 12 hours intravenously), and treatment was extended to include levofloxacin (500 mg/d intravenously), vancomycin (1 g every 12 hours intravenously) and oseltamivir (75 mg twice daily via oral gastric tube). At 58 hours after presentation, extracorporeal membrane oxygenation was started because of progressive hypoxia and increasing respiratory acidosis that was unresponsive to conventional treatment. An ineffective extracorporeal membrane oxygenation flow rate resulting from uterine compression prompted an emergency cesarean section, with delivery of a 1300-g infant (cord blood pH 6.84). The extracorporeal membrane oxygenation flow rate subsequently reached normal levels.
Multiple investigations were undertaken to identify the cause of the acute respiratory failure. No bacterial pathogens were detected in blood cultures or endotracheal aspirates. Results of serologic testing for HIV and hepatitis A, B and C antibodies were negative. Respiratory samples, obtained with nasopharyngeal swabs and bronchoalveolar lavage, and a serum sample collected at admission were positive for influenza A (subtype H1) by means of nucleic acid testing. Multiple attempts to culture the virus for complete strain characterization were unsuccessful. Serologic testing of samples obtained during the acute and convalescent stages of the patient's illness was conducted at the National Microbiology Laboratory and showed a significant rise in titre (from 4 to 128) of influenza A/New Caledonia/ 20/99 (H1N1). This strain had been included in the 2006 trivalent inactivated influenza vaccine. During the patient's routine prenatal care, she had not received influenza vaccine, even though vaccination is publicly funded and was available in the patient's health region.
After 71 days in hospital — including 36 days in the intensive care unit, during which extracorporeal membrane oxygenation was performed for 13 days — the patient was discharged home. Her course of treatment in hospital was compounded by numerous medical complications, including a mild anoxic brain injury requiring neurocognitive rehabilitation, acute respiratory distress syndrome, acute renal failure requiring renal replacement therapy, multiple nosocomial infections, stress-induced gastrointestinal bleeding, pancreatitis and critical illness polyneuropathy. The infant required support in the neonatal intensive care unit for 27 days and has a number of conditions related to prematurity, including hyaline membrane disease, apnea and bradycardia, anemia, retinopathy and right-sided hydrocele. The infant has required readmission to hospital many times since discharge.
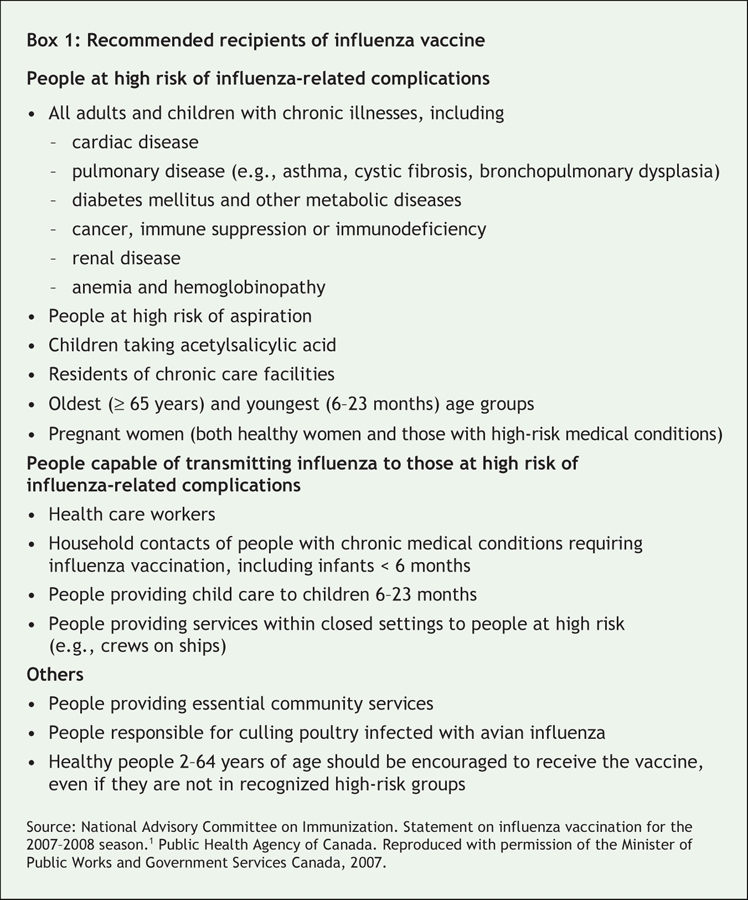
Influenza epidemics occur every year in North America, usually between November and March. Depending on the specific strain of influenza, 5%–20% of the population may be affected. Although the incidence and severity of disease varies markedly from season to season, certain populations are known to be at high risk for influenza-related morbidity and death (Box 1).1 Vaccination is an effective way to prevent serious influenza-related complications. In the PRISMA study,2 vaccination decreased the requirement for admission to hospital by 87% among those less than 65 years old with high-risk factors and by 48% among those aged 65 and older. Vaccination also reduced mortality, resulting in 78% fewer deaths among those less than 65 years old and 50% fewer deaths among those 65 and older. In a new 2007/08 statement on influenza vaccination, the National Advisory Committee on Immunization included pregnancy as a high-risk condition for influenza-related complications and recommended routine vaccination of all pregnant women.1 Before 2007, the committee recommended vaccination of pregnant women who had comorbidities, as well as those who did not have comorbidities in their third trimester if they were expected to deliver during the influenza season, since they would then be the household contacts for infants less than 6 months old, a group recognized to be at high risk for influenza-related complications.3
Box 1.
For many years, pregnant women have been recognized as being at increased risk of complications and death associated with pandemic influenza. During the 1918/19 and 1957 influenza pandemics, the mortality among pregnant women with influenza exceeded 50%.4 Maternal influenza infection has also been associated with fetal loss and neonatal deaths.5 During prepandemic periods of influenza infection, increased rates of admission to hospital and use of health resources by pregnant women are associated with influenza.6,7 Recently, Dodds and colleagues6 described a significant increase in the rate of hospital admissions because of respiratory illness among women who were pregnant during the influenza season relative to the year before conception (relative risk 5.1). Among those with medical comorbidities, the increase was greater (relative risk 7.9). This is further evidence that pregnancy acts independently as a risk factor for serious influenza infection.
Data specifically supporting maternal influenza vaccination as a means of preventing maternal influenza-related morbidity and mortality are still lacking and must be inferred from other populations in which the vaccine's efficacy is well established.2 There is significant evidence of infant benefit from maternal vaccination. Infants are at increased risk for complications and death from influenza, but they are not candidates for influenza vaccine until they are more than 6 months old. During an influenza epidemic, one-third of newborn infants may become infected during their first 6 months of life, a period during which maternal antibodies may still confer protection.8 Prospective studies have demonstrated higher levels of influenza A antibodies in umbilical cord blood samples from infants born to mothers who had been vaccinated during the pregnancy relative to those whose mothers had not been vaccinated, as well as a delay in the onset and severity of influenza illness in babies born with higher antibody levels.9
The safety of inactivated influenza vaccine has been well documented for all stages of pregnancy.10 During 7 years of follow-up, no significant increase in adverse reactions among mothers or infants was documented for 2291 doses of inactivated influenza vaccine administered to pregnant patients.11 Conversely, the role of antiviral therapy in pregnancy-related influenza is unknown. The safety of oseltamivir in pregnancy has yet to be determined in human studies (it is currently classified as a pregnancy category C drug by the US Food and Drug Administration).12 Certainly a strategy of disease avoidance in pregnancy through the use of a vaccine with a proven safety record is preferable to using antiviral therapies with unknown consequences.
Despite convincing evidence of both safety and potential value of influenza vaccination in reducing maternal and fetal morbidity, influenza vaccination rates among pregnant women remain below 10%.6,13 Furthermore, women with underlying chronic medical conditions are no more likely to be vaccinated than women without comorbidities. Based on the National Advisory Committee on Immunization guidelines, the patient we have described would have been a candidate for influenza vaccination on the basis of her asthma, irrespective of her pregnancy status.3 Data suggest that a significant lack of knowledge and comfort regarding the safety and efficacy of influenza vaccine among both primary care providers and obstetricians contributes to the poor vaccine compliance during pregnancy.13
Maternal vaccination with inactivated influenza trivalent vaccine has the potential to reduce the significant maternal, fetal and infant morbidity and mortality associated with influenza infection. Although the case we have described represents an extreme presentation of severe influenza illness, we hope that it highlights the importance of ensuring that this simple and safe preventive intervention is offered to all eligible patients.
Michael D. Parkins MD MSc Department of Medicine, University of Calgary Calgary Health Region Kevin Fonseca PhD Department of Microbiology and Infectious Diseases, University of Calgary Provincial Laboratory for Public Health Adam D. Peets MD MSc Kevin B. Laupland MD MSc Khaled Shamseddin MD Departments of Medicine and Critical Care Medicine, University of Calgary Calgary Health Region M. John Gill MD Departments of Medicine and of Microbiology and Infectious Diseases, University of Calgary Calgary Health Region Calgary, Alta.
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
REFERENCES
- 1. National Advisory Committee on Immunization (NACI) statement on influenza vaccination for the 2007–2008 season. Can Commun Dis Rep 2007;33(ACS-7):1–38. Available: www.phac-aspc.gc.ca/publicat/ccdr-rmtc/07vol33/acs-07/index_e.html (accessed 2007 Aug 30). [PubMed]
- 2.Hak E, Buskens E, van Essen GA, et al. Clinical effectiveness of influenza vaccination in persons younger than 65 years with high-risk medical conditions: the PRISMA study. Arch Intern Med 2005;165:274-80. [DOI] [PubMed]
- 3.National Advisory Committee on Immunization (NACI) statement on influenza vaccination for the 2006–2007 season. Can Commun Dis Rep 2006;32 (ACS-7):1–28. Available: www.phac-aspc.gc.ca/publicat/ccdr-rmtc/06vol32/acs-07/index.html (accessed 2007 Aug 30). [PubMed]
- 4.Harris JW. Influenza occurring in pregnant women. JAMA 1919;14:978-80.
- 5.Yawn DH, Pyeatte JC, Joseph JM, et al. Transplacental transfer of influenza virus. JAMA 1971;216:1022-3. [PubMed]
- 6.Dodds L, McNeil SA, Fell DB, et al. Impact of influenza exposure on rates of hospital admissions and physician visits because of respiratory illness among pregnant women. CMAJ 2007;176: 463-8. [DOI] [PMC free article] [PubMed]
- 7.Neuzil KM, Reed GW, Mitchel EF, et al. Impact of influenza on acute cardiopulmonary hospitalizations in pregnant women. Am J Epidemiol 1998;148:1094-102. [DOI] [PubMed]
- 8.Glezen WP, Payne AA, Snyder DN, et al. Mortality and influenza. J Infect Dis 1982;146:313-21. [DOI] [PubMed]
- 9.Reuman PD, Ayoub EM, Small PA. Effect of passive maternal antibody on influenza illness in children: a prospective study of influenza A in mother–infant pairs. Pediatr Infect Dis J 1987;6:398-403. [DOI] [PubMed]
- 10.Englund JA. Maternal immunization with inactivated influenza vaccine: rationale and experience. Vaccine 2003;21:3460-4. [DOI] [PubMed]
- 11.Heinonen O, Slone D, Shapiro S. Immunizing agents. Littleton (MA): Publishing Sciences Group; 1977.
- 12.Oseltamivir phosphate capsules [Tamiflu product information]. Nutley (NJ): Roche Laboratories; 1999. Available: www.fda.gov/cder/foi/label/1999/21087lbl.pdf (accessed 2007 Aug 27).
- 13.Silverman NS, Greif A. Influenza vaccination during pregnancy. Patients' and physicians' attitudes. J Reprod Med 2001;46:989-94. [PubMed]


