Abstract
Purpose
The stroke mortality rate for African Americans aged 45-64 is three to four times higher than for whites of the same age, with a decreasing black-to-white mortality ratio with increasing age. There is also a “Stroke Belt” with higher stroke mortality in the Southeastern US. This study assesses if there are also geographic variations in the magnitude of the excess stroke mortality for African Americans.
Methods
The age- and sex-specific black-to-white mortality ratio was calculated for each of 26 states with a sufficient African American population for stable estimates. The southern excess was calculated as the percentage excess of southern over non-southern rates.
Results
Across age and sex strata, the black-to-white stroke mortality ratio was consistently higher for southern states, with an average black-to-white stroke mortality ratio that ranged from 6% to 21% higher among southern states than in non-southern states.
Conclusions
The increase in stroke mortality rates for African Americans in southern states is even larger than expected. That southern states that are not part of the “Stroke Belt” (Virginia and Florida) also have an elevated black-to-white mortality ratio suggests the mechanism of higher risk for African Americans may be independent of the causes contributing to “Stroke Belt.”
Keywords: Cerebrovascular accident, mortality, continental population groups, African Americans, geography
Introduction
The “Stroke Belt” was first identified in 1965 as a region with approximately 50% higher stroke mortality rates in the southeastern US.1 While there are different definitions of the region, it frequently includes 8 southern states: North Carolina, South Carolina, Georgia, Tennessee, Mississippi, Alabama, Louisiana, and Arkansas. While this region of excess stroke mortality rate has been persistent and very well-documented,1-7 the contributing causes have remained a mystery with at least 10 hypothesized potential contributing causes.8,9 As there are limited national data on stroke incidence, it is not clear whether the excess in stroke mortality is primarily associated with higher stroke incidence or case fatality following stroke events.8,9 Within the Stroke Belt, a “Buckle” region along the coastal plain of North Carolina, South Carolina, and Georgia has even higher stroke mortality (approximately twice the national rate).4,5
In addition, stroke mortality rates are approximately 50% higher in African Americans than whites, with a larger difference at younger ages; at age 55 the risk of dying from stroke is 3 times greater for blacks than whites.10-13 Data from the Greater Cincinnati/Northern Kentucky Stroke Study suggest the excess mortality rate is primarily attributable to higher incidence of stroke (rather than higher case fatality) among African Americans.14 As with the excess stroke mortality in the Southeast, the known contributing factors for the excess stroke mortality in blacks (primarily higher prevalence of hypertension and diabetes, and a lower socio-economic status) explain only a fraction of the overage.15-17
The geographic variations in overall stroke mortality risk raise the question whether there are also variations in the black-to-white ratio of stroke mortality.13 That is, in a comparison of African Americans and whites by state or region, does the relative excess of stroke mortality among African Americans vary? Are there regions where the black-to-white stroke mortality ratio is even greater than the national average?
Previously we noted differences in the age-adjusted black-to-white stroke mortality ratio (without stratification by age) among the states. For example, in Florida African Americans have 1.92 times the rate of whites, whereas in New York African Americans have 1.06 times the rate of whites.13 In this report we explore age-specific black-to-white mortality ratios for each sex by state and by aggregations of states classified as non-southern or southern.
Methods
State stroke mortality rates were calculated for sex and age strata (45-54, 55-64, 65-74, 75-84, and 85 or older) on the basis of U.S. vital statistics 1997 to 2000,18 and a population estimate from the midpoint of 1999.19 Stable estimates of stroke mortality ratios require a substantial population in each group of interest. All 50 states have sufficient numbers of white residents to provide stable estimates, but 24 states have a small African American population, so our analysis had to be restricted to 26 states that were classified as non-southern (California, Illinois, Indiana, Kentucky, Maryland, Michigan, New Jersey, New York, Ohio, Oklahoma, Pennsylvania, and Texas) or southern (Alabama, Arkansas, Florida, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, and Virginia). Without any knowledge of states' stroke mortality ratios, we selected all states with at least 25,000 people older than 45 years in each race-sex strata (white men, white women, black men, and black women) (specific data available upon request). We note that many African Americans are in the southern states, and in non-southern states including Texas, California, the northeastern states, the populous states around the Great Lakes. We also note that “non-southern states” omits many Midwestern, Great Plain and northwestern states all of which have small African American populations.
To produce stable state estimates of the stroke mortality rate for the age-sex strata, we calculated the mean number of stroke deaths for a 5-year period (1997–2001). The number of deaths was then divided by the state population for the age-sex strata according to the Census population estimates from1999 (mid-year for the range of years of death data). Pooling deaths for multiple years is well accepted in demography.20 The age- and sex-specific black-to-white mortality ratio was then calculated for each state by dividing the estimated African American stroke mortality rate by the estimated white stroke mortality rate for each age stratum. The ratios of the mean mortality ratios for the states within each category (non-southern and southern) were calculated to address the central question to be answered by this analysis, and “excess” mortality in the southern states was defined as the percentage that the mortality ratio for the southern states was above the mortality ratio for the non-southern states.
Results
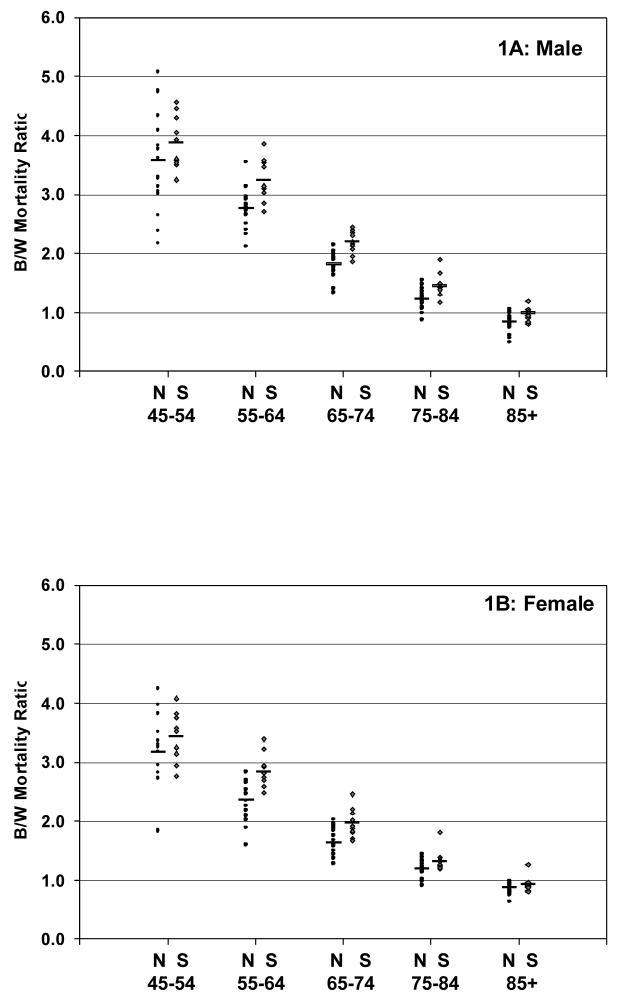
Age-specific white and African American stroke mortality rates and the age specific black-to-white mortality ratio are in Tables 1A (men) and 1B (women). Review of the black-to-white mortality ratios shows a clear pattern with southern states having greater values than non-southern states. The geographic differences in the distributions of stroke mortality ratios by groups of states are shown in Figures 1A and 1B.
Table 1A.
Stroke mortality rates (per 1000) for men and black-to-white mortality ratio by state
| State | Men aged 45-54 | Men aged 55-64 | Men aged 65-74 | Men aged 75-84 | Men aged 85 or older | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mortality | Ratio | Mortality | Ratio | Mortality | Ratio | Mortality | Ratio | Mortality | Ratio | |||||||
| White | Black | White | Black | White | Black | White | Black | White | Black | |||||||
| Non-Southern | California | 0.15 | 0.45 | 3.05 | 0.42 | 1.12 | 2.66 | 1.42 | 2.67 | 1.88 | 4.96 | 6.50 | 1.31 | 15.40 | 15.14 | 0.98 |
| Connecticut | 0.09 | 0.27 | 3.01 | 0.30 | 0.74 | 2.50 | 1.16 | 1.54 | 1.33 | 4.29 | 4.26 | 0.99 | 12.78 | 7.13 | 0.56 | |
| Illinois | 0.13 | 0.57 | 4.33 | 0.37 | 1.31 | 3.54 | 1.36 | 2.42 | 1.78 | 5.08 | 5.44 | 1.07 | 15.44 | 12.09 | 0.78 | |
| Indiana | 0.14 | 0.53 | 3.77 | 0.39 | 1.15 | 2.92 | 1.63 | 2.64 | 1.62 | 5.72 | 5.60 | 0.98 | 16.47 | 14.65 | 0.89 | |
| Kentucky | 0.17 | 0.40 | 2.38 | 0.49 | 1.18 | 2.39 | 1.61 | 2.61 | 1.62 | 5.28 | 6.64 | 1.26 | 15.99 | 13.79 | 0.86 | |
| Maryland | 0.11 | 0.43 | 4.08 | 0.32 | 0.89 | 2.83 | 1.33 | 2.50 | 1.88 | 4.79 | 6.08 | 1.27 | 15.25 | 12.33 | 0.81 | |
| Massachusetts | 0.11 | 0.23 | 2.17 | 0.27 | 0.64 | 2.33 | 1.15 | 2.02 | 1.76 | 4.14 | 4.89 | 1.18 | 13.14 | 6.50 | 0.49 | |
| Michigan | 0.12 | 0.57 | 4.77 | 0.39 | 1.07 | 2.73 | 1.39 | 2.68 | 1.93 | 5.07 | 5.45 | 1.08 | 15.23 | 13.36 | 0.88 | |
| Missouri | 0.15 | 0.58 | 3.83 | 0.42 | 1.22 | 2.93 | 1.40 | 2.69 | 1.92 | 5.17 | 6.78 | 1.31 | 16.60 | 15.43 | 0.93 | |
| New Jersey | 0.13 | 0.42 | 3.27 | 0.34 | 0.96 | 2.82 | 1.18 | 2.25 | 1.90 | 3.89 | 5.06 | 1.30 | 11.14 | 11.24 | 1.01 | |
| New York | 0.12 | 0.32 | 2.65 | 0.32 | 0.68 | 2.11 | 1.06 | 1.48 | 1.40 | 3.34 | 2.87 | 0.86 | 9.68 | 5.83 | 0.60 | |
| Ohio | 0.13 | 0.46 | 3.61 | 0.37 | 1.03 | 2.78 | 1.41 | 2.41 | 1.70 | 4.85 | 6.48 | 1.34 | 14.74 | 15.50 | 1.05 | |
| Oklahoma | 0.15 | 0.50 | 3.28 | 0.44 | 1.30 | 2.96 | 1.48 | 3.17 | 2.14 | 5.21 | 7.29 | 1.40 | 17.45 | 13.00 | 0.75 | |
| Pennsylvania | 0.11 | 0.54 | 4.74 | 0.36 | 1.03 | 2.83 | 1.33 | 2.63 | 1.98 | 4.62 | 5.32 | 1.15 | 14.06 | 12.91 | 0.92 | |
| Texas | 0.16 | 0.49 | 3.13 | 0.43 | 1.14 | 2.66 | 1.40 | 3.01 | 2.15 | 4.79 | 7.39 | 1.54 | 16.08 | 16.28 | 1.01 | |
| Wisconsin | 0.11 | 0.58 | 5.08 | 0.37 | 1.17 | 3.13 | 1.54 | 3.13 | 2.04 | 5.56 | 8.19 | 1.47 | 16.67 | 13.73 | 0.82 | |
| Average | 0.13 | 0.46 | 3.57 | 0.38 | 1.04 | 2.76 | 1.37 | 2.49 | 1.81 | 4.80 | 5.89 | 1.22 | 14.76 | 12.43 | 0.83 | |
| Southern | Alabama | 0.18 | 0.64 | 3.57 | 0.55 | 1.49 | 2.71 | 1.54 | 3.34 | 2.16 | 5.16 | 6.76 | 1.31 | 15.15 | 12.29 | 0.81 |
| Arkansas | 0.19 | 0.68 | 3.61 | 0.60 | 2.12 | 3.54 | 1.70 | 4.05 | 2.39 | 6.35 | 9.12 | 1.44 | 17.93 | 18.99 | 1.06 | |
| Florida | 0.16 | 0.51 | 3.25 | 0.39 | 1.21 | 3.11 | 1.06 | 2.59 | 2.44 | 3.60 | 6.83 | 1.90 | 11.56 | 13.86 | 1.20 | |
| Georgia | 0.18 | 0.63 | 3.51 | 0.44 | 1.58 | 3.58 | 1.65 | 3.44 | 2.08 | 5.44 | 7.52 | 1.38 | 15.49 | 15.09 | 0.97 | |
| Louisiana | 0.14 | 0.65 | 4.57 | 0.47 | 1.43 | 3.02 | 1.48 | 2.89 | 1.95 | 4.66 | 6.09 | 1.31 | 14.42 | 13.01 | 0.90 | |
| Mississippi | 0.18 | 0.70 | 3.94 | 0.58 | 1.64 | 2.84 | 1.70 | 3.15 | 1.86 | 5.37 | 6.30 | 1.17 | 15.00 | 12.58 | 0.84 | |
| North Carolina |
0.15 | 0.60 | 4.05 | 0.45 | 1.57 | 3.48 | 1.65 | 3.52 | 2.14 | 5.89 | 8.30 | 1.41 | 18.39 | 18.55 | 1.01 | |
| South Carolina |
0.21 | 0.74 | 3.53 | 0.50 | 1.95 | 3.86 | 1.76 | 3.90 | 2.21 | 5.71 | 9.56 | 1.67 | 17.91 | 18.69 | 1.04 | |
| Tennessee | 0.15 | 0.66 | 4.46 | 0.52 | 1.62 | 3.14 | 1.62 | 3.82 | 2.35 | 6.04 | 8.28 | 1.37 | 17.74 | 16.61 | 0.94 | |
| Virginia | 0.11 | 0.46 | 4.31 | 0.40 | 1.25 | 3.14 | 1.36 | 3.13 | 2.31 | 5.12 | 7.65 | 1.49 | 17.04 | 17.31 | 1.02 | |
| Average | 0.17 | 0.63 | 3.88 | 0.49 | 1.59 | 3.24 | 1.55 | 3.38 | 2.19 | 5.33 | 7.64 | 1.45 | 16.06 | 15.70 | 0.98 | |
| Southern Excess | 27% | 37% | 9% | 31% | 53% | 18% | 14% | 36% | 21% | 11% | 30% | 19% | 9% | 26% | 17% | |
Table 1B.
Stroke mortality rates (per 1000) for women and AA-to-white mortality ratio by state and age strata.
| STATE | Women aged 45-54 | Women aged 55-64 | Women aged 65-74 | Women aged 75-84 | Women aged 85 or older | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mortality | Ratio | Mortality | Ratio | Mortality | Ratio | Mortality | Ratio | Mortality | Ratio | |||||||
| White | Black | White | Black | White | Black | White | Black | White | Black | |||||||
| Non-Southern | California | 0.12 | 0.39 | 3.37 | 0.32 | 0.79 | 2.52 | 1.15 | 2.20 | 1.91 | 4.59 | 6.27 | 1.37 | 17.28 | 17.10 | 0.99 |
| Connecticut | 0.10 | 0.19 | 1.84 | 0.18 | 0.51 | 2.83 | 0.88 | 1.28 | 1.45 | 3.72 | 4.92 | 1.32 | 14.08 | 11.51 | 0.82 | |
| Illinois | 0.09 | 0.39 | 4.25 | 0.30 | 0.80 | 2.67 | 1.11 | 1.67 | 1.50 | 4.30 | 5.03 | 1.17 | 16.65 | 13.02 | 0.78 | |
| Indiana | 0.13 | 0.38 | 2.94 | 0.33 | 0.70 | 2.09 | 1.25 | 2.31 | 1.84 | 4.88 | 5.96 | 1.22 | 18.50 | 15.05 | 0.81 | |
| Kentucky | 0.13 | 0.36 | 2.72 | 0.36 | 0.76 | 2.10 | 1.29 | 2.04 | 1.58 | 5.01 | 5.07 | 1.01 | 17.60 | 16.51 | 0.94 | |
| Massachusetts | 0.08 | 0.14 | 1.83 | 0.21 | 0.34 | 1.59 | 0.84 | 1.21 | 1.43 | 3.70 | 4.18 | 1.13 | 14.23 | 12.14 | 0.85 | |
| Maryland | 0.08 | 0.32 | 3.97 | 0.26 | 0.63 | 2.46 | 1.03 | 1.72 | 1.67 | 4.19 | 4.86 | 1.16 | 16.88 | 13.05 | 0.77 | |
| Michigan | 0.12 | 0.39 | 3.35 | 0.29 | 0.63 | 2.18 | 1.07 | 1.88 | 1.75 | 4.47 | 5.10 | 1.14 | 16.61 | 14.65 | 0.88 | |
| Missouri | 0.11 | 0.40 | 3.82 | 0.35 | 0.70 | 2.02 | 1.17 | 1.87 | 1.60 | 4.70 | 4.57 | 0.97 | 17.07 | 12.73 | 0.75 | |
| New Jersey | 0.09 | 0.35 | 3.83 | 0.23 | 0.62 | 2.69 | 0.83 | 1.68 | 2.03 | 3.27 | 4.35 | 1.33 | 12.10 | 11.72 | 0.97 | |
| New York | 0.09 | 0.26 | 2.73 | 0.24 | 0.46 | 1.89 | 0.80 | 1.09 | 1.36 | 2.93 | 2.63 | 0.90 | 10.82 | 6.85 | 0.63 | |
| Ohio | 0.11 | 0.37 | 3.30 | 0.31 | 0.74 | 2.35 | 1.14 | 1.78 | 1.57 | 4.37 | 4.93 | 1.13 | 15.84 | 14.71 | 0.93 | |
| Oklahoma | 0.17 | 0.47 | 2.82 | 0.37 | 0.83 | 2.25 | 1.31 | 1.68 | 1.28 | 5.23 | 6.83 | 1.31 | 17.64 | 15.47 | 0.88 | |
| Pennsylvania | 0.10 | 0.31 | 3.18 | 0.28 | 0.75 | 2.64 | 1.00 | 1.88 | 1.88 | 4.16 | 4.92 | 1.18 | 15.34 | 14.86 | 0.97 | |
| Texas | 0.12 | 0.40 | 3.25 | 0.33 | 0.88 | 2.64 | 1.16 | 2.26 | 1.94 | 4.77 | 6.08 | 1.27 | 17.85 | 16.98 | 0.95 | |
| Wisconsin | 0.11 | 0.37 | 3.51 | 0.27 | 0.77 | 2.83 | 1.14 | 1.45 | 1.27 | 4.62 | 6.60 | 1.43 | 17.81 | 15.99 | 0.90 | |
| Average | 0.11 | 0.34 | 3.17 | 0.29 | 0.68 | 2.36 | 1.07 | 1.75 | 1.63 | 4.31 | 5.14 | 1.19 | 16.02 | 13.90 | 0.86 | |
| Southern | Alabama | 0.13 | 0.41 | 3.14 | 0.36 | 1.02 | 2.81 | 1.26 | 2.28 | 1.81 | 4.77 | 5.68 | 1.19 | 17.02 | 14.01 | 0.82 |
| Arkansas | 0.15 | 0.56 | 3.83 | 0.46 | 1.18 | 2.59 | 1.52 | 2.59 | 1.70 | 5.76 | 7.15 | 1.24 | 20.32 | 18.01 | 0.89 | |
| Florida | 0.12 | 0.34 | 2.94 | 0.26 | 0.85 | 3.22 | 0.84 | 2.05 | 2.45 | 3.33 | 5.99 | 1.80 | 12.73 | 16.01 | 1.26 | |
| Georgia | 0.13 | 0.44 | 3.25 | 0.38 | 0.94 | 2.48 | 1.32 | 2.46 | 1.87 | 4.91 | 6.11 | 1.24 | 17.24 | 13.92 | 0.81 | |
| Louisiana | 0.14 | 0.51 | 3.52 | 0.32 | 0.93 | 2.92 | 1.14 | 2.18 | 1.91 | 4.23 | 5.82 | 1.38 | 15.92 | 14.15 | 0.89 | |
| Mississippi | 0.14 | 0.56 | 4.08 | 0.41 | 1.12 | 2.74 | 1.27 | 2.11 | 1.67 | 4.75 | 5.78 | 1.22 | 15.34 | 13.25 | 0.86 | |
| North Carolina |
0.11 | 0.41 | 3.76 | 0.32 | 0.80 | 2.48 | 1.27 | 2.33 | 1.83 | 5.18 | 6.55 | 1.26 | 20.32 | 18.42 | 0.91 | |
| South Carolina |
0.13 | 0.46 | 3.58 | 0.35 | 1.17 | 3.39 | 1.26 | 2.78 | 2.21 | 5.35 | 7.18 | 1.34 | 20.40 | 19.03 | 0.93 | |
| Tennessee | 0.14 | 0.37 | 2.76 | 0.41 | 1.11 | 2.69 | 1.32 | 2.81 | 2.13 | 5.58 | 6.74 | 1.21 | 19.69 | 16.99 | 0.86 | |
| Virginia | 0.10 | 0.34 | 3.52 | 0.27 | 0.80 | 2.94 | 1.15 | 2.30 | 2.01 | 4.70 | 6.20 | 1.32 | 18.16 | 17.34 | 0.96 | |
| Average | 0.13 | 0.44 | 3.44 | 0.35 | 0.99 | 2.83 | 1.24 | 2.39 | 1.96 | 4.86 | 6.32 | 1.32 | 17.71 | 16.11 | 0.92 | |
| Southern Excess | 18% | 28% | 8% | 22% | 45% | 20% | 15% | 37% | 20% | 13% | 23% | 11% | 11% | 16% | 6% | |
Figure 1A (men) and 1B (women).
Stroke mortality ratios (black-to-white) for non-southern (N) and southern (S) states, by age strata and sex.
A pattern of declining black-to-white mortality ratios with increasing age is apparent for both men and women in all 26 states, reflecting the previously described decline in racial disparity as people age9-13 (Tables 1A and 1B, Figures 1A, 1B, and 2); however, the focus of this report is on the geographic differences in excess mortality for blacks.
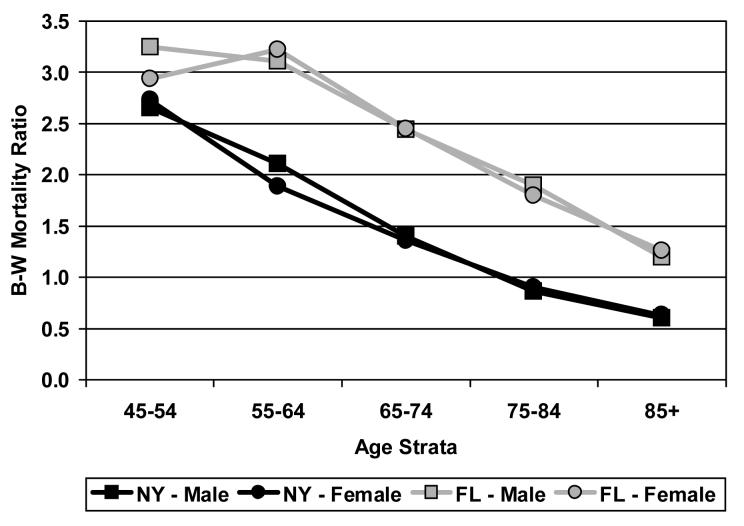
Figure 2.
Black-to-white stroke mortality ratio for men and women from New York and Florida, by age strata.
On a percentage basis the regional differences in black-to-white mortality ratios (i.e., the southern excess) were greatest for people aged 65 to 74: for men in non-southern states the average mortality ratio was 1.81 (range from 1.33 to 2.15) and 2.19 (range from 1.86 to 2.44) in southern states, resulting in an average mortality ratio 21% higher in the south than in the non-south. For women aged 65 to 74, in non-southern states the average mortality ratio was 1.63 (range from 1.27 to 2.03) and 1.96 in southern states (range from 1.70 to 2.45), an average that was also 20% higher in the south. These differences are substantial when one notes that for both men and women, the lowest mortality ratio for a southern state is about the same as the average mortality ratio for non-southern states.
The percentage excess in the black-to-white stroke mortality ratio in southern states was nearly as large for people aged 55 to 64: for men in non-southern states, the black-to-white mortality ratio averaged 2.76 (range from 2.11 to 3.54) compared with an average of 3.24 for men in southern states (range from 2.71 to 3.86). Hence, the average black-to-white mortality ratio averaged 18% higher in the southern states. Likewise for women in the same age stratum in non-southern states, the average black-to-white mortality ratio averaged 2.36 (range from 1.59 to 2.83) and 2.83 for women in southern states (range from 2.48 to 3.39), resulting in an average mortality ratio 20% higher for southern states. Again, the lowest mortality ratio for a southern state is about the same as the average mortality ratio for the non-southern states.
For men, the excess in black-to-white stroke mortality persists for those older than 75. For men aged 75 to 84, the average black-to-white stroke mortality is 19% higher in the southern states than in the non-southern states, and it is 17% higher on average for men older than 85. It is noteworthy that this 17% higher black-to-white mortality for the oldest age stratum is a result of about equal mortality for African Americans and whites living in southern states (average black-to-white mortality of 0.98), while in the non-southern states African Americans are at lower risk than whites (average black-to-white mortality of 0.83).
The southern excess black-to-white mortality persists but is somewhat attenuated for women older than 75. For women aged 75 to 84, the average black-to-white mortality ratio is 11% higher in southern states than in non-southern states, and for women aged 85, the average mortality ratio is only 6% higher in southern states than in non-southern states. For women older than age 85, the mortality rate was lower for African Americans than for whites in both southern and non-southern states.
Although the absolute levels of the black-to-white mortality ratios are greatest for people aged 45 to 54, the excess mortality in southern states was relatively modest for both men (9%) and women (8%) in this age range.
Although differences in the average black-to-white ratio of stroke mortality comparing southern to non-southern states are striking, the mortality ratios for selected states are particularly noteworthy. The black-to-white mortality ratios are particularly high for Florida, which had the highest black-to-white stroke mortality ratio for each of the three oldest age strata (65 to 74, 75 to 84, and 85 or older) for both men and women. At the other end of the spectrum are several states in the northeast (e.g., New York State) which has generally low black-to-white stroke mortality ratios for both men and women in all age strata. Data for Florida and New York are shown in Figure 2. Although not as consistently high as Florida, mortality ratios for Arkansas, South Carolina, and Tennessee tended to be substantially above average for most age strata for both men and women. And, although not as consistently low as those for New York, mortality ratios for California, Connecticut, Illinois, Indiana, Kentucky, and Massachusetts were relatively low for men and women in most age strata.
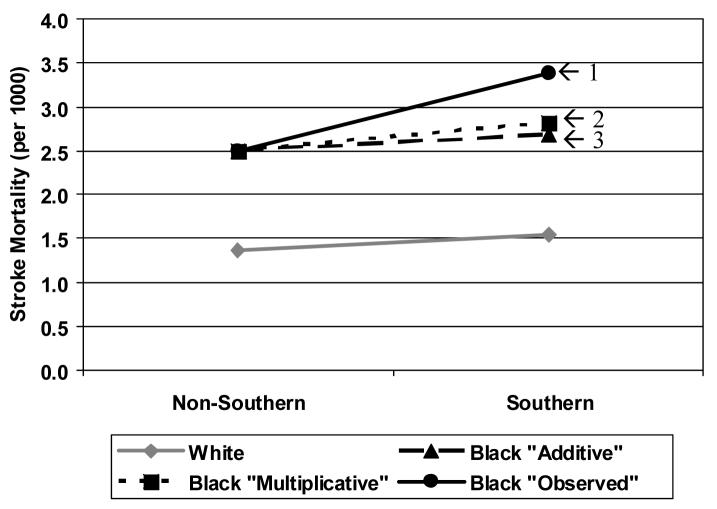
The finding that the mortality ratio is greater than expected for southern African American is equivalent to reporting a statistical interaction between race and region for stroke mortality. In this context, it is important to note that the magnitude of the excess is larger than would be expected by either an additive model (absolute scale) or a multiplicative model (relative scale). Consider, for example, the average mortality rates for men aged 65-to-74 shown in Figure 3. In the non-southern states, the mortality rate for white men was 1.37 per 1000, whereas the mortality rate for African Americans was 2.49. Likewise in southern states the mortality rate for white men was 1.55 per 1000 and higher for blacks under either the additive or the multiplicative model. Under an additive interaction model (which expects parallel effects on an absolute scale), the expected mortality rate for African Americans in southern states is 2.67 per 1000 (1.37 + (1.55−1.37) + (2.49−1.37) = 2.67). Under a multiplicative model (which expects parallel effects on a relative scale), the expected mortality rate for African Americans in southern states is 2.82 per 1000 (2.49 * (1.55/1.37) = 2.82). These expected values from both the additive or multiplicative models are each substantially below the observed mortality rate of 3.38 for southern African Americans. Calculations for other age strata of each sex show that the observed higher rates for African Americans in southern states is consistently above expected on the basis of either model.
Figure 3.
Observed stroke mortality for white men aged 65 to 74 (gray). Observed (#1, solid black line) and expected (#2 and #3) mortality rates are shown for black men aged 65 to 74. Expected rates are shown if the pattern was similar to the pattern for whites on a multiplicative or relative scale (#2: square and short dashed line) or on an additive scale (#3: triangle and long dashed line).
Discussion
Except at the oldest ages, African Americans are at higher risk of death from stroke than are whites, a finding that held in all the states we studied. The excess in stroke mortality for non-southern African Americans is substantial: for men there was an average black-to-white stroke mortality ratio across non-southern states of 2.76 (1.04/0.38) at age 55 to 64; 1.81 (2.49/1.37) at age 65 to 74; and 1.22 (5.89/4.80) at age 75 to 84. Similar excesses were found for women. However, this report documents that the excess in stroke mortality for African Americans is substantially larger in southern than in non-southern states. In the same age strata, for southern men the ratios of risk for African Americans were 3.24 (1.59/0.49) at age 55 to 64, 2.19 (3.38/1.55) at age 65 to74, and 1.45 (7.64/5.33) at age 75 to 84. Similar higher rates were found for southern women in these age strata. As such, the black-to-white mortality ratios averaged nearly 20% higher in southern states than in non-southern states. This implies that about one-in-five strokes deaths among southern African Americans would not have occurred had the higher risk for African Americans been no greater in the southern states than in the non-southern states.
For reasons that are poorly understood, the magnitude of the southern excess in the black-to-white mortality ratios appears to be relatively small for people aged 45-54: 9% for men and 8% for women. For men, this southern excess in black-to-white stroke mortality is approximately 20% higher for people aged 55 or older. While for women this 20% excess is observed in ages 55 to 74 only. For women older than this age, the excess is attenuated somewhat to 11% for those aged 75 to 84 and to 6% for those older than 85. We speculate that one reason for this increasing pattern in men could be that a large proportion of strokes at age 45 to 55 are associated with an unusual underlying cause, such as non-traditional risk factors or diverse mechanisms. The pattern in women shows a similar increasing trend with a decrease at older ages, and perhaps a similar association with “nontraditional” risk factors is present in women at both ends of the age spectrum.
Because African Americans constitute a large proportion of the population of the southern states, the financial and public health burden of this higher risk is substantial. Of 19,002 stroke deaths among U.S. African Americans during 2001, 8,807 (46%) were in the 10 southern states selected for this report.21 The average (for both sexes and all age strata) southern excess of stroke mortality was 14.9%. The effect of reducing African American stroke mortality by 15% would correspond to an annual reduction of 1,500 deaths from stroke among African Americans in these 10 southern states alone. If one assumed that stroke case-fatality was about 30%, the reduction of 1,500 deaths would be associated with a reduction of about 5,000 incident stroke events. These additional events represent an immense burden and disruption to the stroke victims and their families, increased care-giver burden, lower quality of life, and lost-quality years of life. In addition, using the Stroke PORT estimate of $104,000 as the life-time cost (both direct and indirect) of having a stroke,22 this additional stroke mortality among southern African Americans (above the expected higher rate for African Americans in the non-south) is associated with an annual increase in public health burden of $520 million.
There are at least 10 published explanations for the stroke belt;8,9 and there are currently few data to address these hypotheses. The REGARDS study, and other longitudinal cohort studies, are currently underway to provide these data.23 The potential contributors to this larger excess for African Americans are so broad that speculation of the causes will certainly omit important potential contributors than could be discussed; however, some of the potential causes include:
The higher prevalence of hypertension and diabetes clearly contribute to the excess stroke mortality among African Americans,12, 15 and it is possible that there is a geographic differential in the racial disparity of these important risk factors.27, 28
Socio-economic factors have also been hypothesized as a contributor to the stroke belt, 8, 9, 29 and these factors could fall disproportionately on southern African Americans. In addition, wealthier white individuals are moving to the Southeast, and these individuals are at lower risk for stroke both by their higher socio-economic status and their pre-selection to be sufficiently healthy to move. This is in contrast to less mobile African Americans. This migration of low risk whites could result in a higher average stroke risk for white in the non-south and a lower average stroke risk for whites in the south.
The observed higher mortality among southern African Americans could be confounded with the rural or urban nature of their environment: a larger proportion of non-southern than southern African Americans live in urban areas, and the urban/rural status of participants could influence other factors such as access or quality of care. For example, according to the 2000 Census, in the “south” region of the United States 69% of whites and 83% of African Americans live in urban areas, whereas in the “northeastern” region 80% of whites and 98% of African Americans live in urban areas.24 A very large proportion of non-southern African Americans live in urban areas in the region where we observe the lowest black-to-white stroke mortality ratios.
Environmental exposures including micronutrients in the drinking water and food supply have been hypothesized as a contributor to the stroke belt, 8, 9 and there could be geographic differences in these exposures by the different race groups.
Lifestyle choices, including diet and exercise, have been hypothesized as a contributor to the stroke belt, 8, 9 and again there could be geographic differences in the difference between the races for these factors. There could also be geographic differences by race for lifestyle choices that are acknowledged as major stroke risk factors such as cigarette smoking.
There are considerable within-state variations in stroke mortality, and it is also possible that southern African Americans live in regions of specific states with high stroke mortality. For example, the northern counties of Florida have a higher proportion of African Americans than the southern counties,25 and these counties also have higher stroke mortality than the southern counties.4 Unfortunately, restricting analyses to relatively small regions of states results in estimated stroke mortality ratios that are inherently unstable, making direct assessment of this possible explanation problematic.
This list of potential contributing causes should be considered partial and speculative, but it clearly underscores the need for further investigations to identify the causes of this disparity and targeting of interventions to reduce it. We have attempted elsewhere26 to assess the confounding of race and region on stroke mortality and found that only about 5% of the excess risk observed for the African American population is attributable to a higher proportion of African Americans than whites living in regions with high risk.
In conclusion African Americans living in the south are at higher risk of death from stroke because they are African American, and they are at additional risk because they live in the south. However, we observed that the difference in risk of death from stroke for African Americans living in the south is actually greater than expected on the basis of either an additive or a multiplicative increase in risk associated with geographic location and race. The magnitude of this extraordinary risk is substantial, accounting for 6% to 21% of strokes among African Americans living in the southern region. Since about one-half of all strokes among African Americans occur in the south, the effect of this excess on the total burden of stroke in African Americans is substantial. Additional research is needed to understand and reduce this huge disparity. Key to these efforts will the collection of population-based data allowing critically important (but currently unanswered) questions to be addressed. The lack of data include the relative contributions of stroke incidence versus case fatality to the excess stroke mortality, and how these two factors contribute to the larger disparities for African Americans living in the south. In addition, important questions remain regarding the effect of confounding with socioeconomic status and access to care, regional differences in the racial disparity of risk factor levels (hypertension, diabetes, etc.) or life-style choices (diet, exercise, cigarette smoking, etc.), or the effects of nativity or birth weight, or differential sensitivity to risk factors for African Americans and whites in different regions.
Acknowledgments
The research reported in this article was partially supported by cooperative agreement U01 NS 041588 from the National Institute of Neurological Disorders and Stroke
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention
Footnotes
No authors have a conflict of interest with information presented in this report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Borhani NO. Changes and geographic distribution of mortality from cerebrovascular disease. Am J Public Health. 1965;55:673–681. doi: 10.2105/ajph.55.5.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lanska DJ. Geographic distribution of stroke mortality in the United States: 1939-1941 to 1979 to 1981. Neurology. 1993;43:1839–1851. doi: 10.1212/wnl.43.9.1839. [DOI] [PubMed] [Google Scholar]
- 3.Casper ML, Wing S, Anda RF, Knowles M, Pollard RA. The shifting stroke belt: chances in the geographic pattern of stroke mortality in the United States, 1962 to 1988. Stroke. 1995;26:755–760. doi: 10.1161/01.str.26.5.755. [DOI] [PubMed] [Google Scholar]
- 4.Casper ML, Barnett E, Williams GI, Jr., Halverson JA, Braham VE, Greenlund KJ. Atlas of Stroke Mortality: Racial, Ethnic, and Geographic Disparities in the United States. Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA: 2003. [Google Scholar]
- 5.Howard G, Anderson R, Johnson NJ, Sorlie P, Russell G, Howard VJ. Evaluation of social status as a contributing factor to the stroke belt of the United States. Stroke. 1997;28:936–940. doi: 10.1161/01.str.28.5.936. [DOI] [PubMed] [Google Scholar]
- 6.Howard G, Evans GW, Pearce K, Howard VJ, Bell RA, Mayer EJ, Burke GL. Is the stroke belt disappearing: an analysis of racial, temporal and age effects. Stroke. 1995;26:1153–1158. doi: 10.1161/01.str.26.7.1153. [DOI] [PubMed] [Google Scholar]
- 7.Howard G, Howard VJ, Katholi C, Oli MK, Huston S. Decline in US stroke mortality: an analysis of temporal patterns by sex, race, and geographic region. Stroke. 2001;32:2213–20. doi: 10.1161/hs1001.096047. [DOI] [PubMed] [Google Scholar]
- 8.Perry HM, Roccella EJ. Conference report on stroke mortality in the Southeastern United States. Hypertension. 1998;31:1205–1215. doi: 10.1161/01.hyp.31.6.1206. [DOI] [PubMed] [Google Scholar]
- 9.Howard G. Why do we have a stroke belt in the southeastern United States? A review of unlikely and uninvestigated potential causes. Am J Med Sci. 1999;317:160–7. doi: 10.1097/00000441-199903000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Howard G, Anderson R, Sorlie P, Andrews VC, Backlund E, Burke GL. Ethnic differences in stroke mortality between non-Hispanic Whites, Hispanic whites, and blacks: the National Longitudinal Mortality Study. Stroke. 1994;25:2120–2125. doi: 10.1161/01.str.25.11.2120. [DOI] [PubMed] [Google Scholar]
- 11.Cooper ES. Cardiovascular diseases and stroke in African Americans: a call for action. J Natl Med Assoc. 1993;85:97–100. [PMC free article] [PubMed] [Google Scholar]
- 12.Gillum RF. Stroke mortality in blacks. Disturbing trends. Stroke. 1999;30:1711–5. doi: 10.1161/01.str.30.8.1711. [DOI] [PubMed] [Google Scholar]
- 13.Howard G, Howard VJ. Ethnic disparities in stroke: the scope of the problem. Ethn Dis. 2001;11:761–8. [PubMed] [Google Scholar]
- 14.Kissela B, Schneider A, Kleindorfer D, Khoury J, Miller R, Alwell K, Woo D, Szafarski J, Gerbel J, Moomaw C, Pancioli A, Jauch E, Shukla R, Broderick J. Stroke in a biracial population: the excess burden of stroke among blacks. Stroke. 2004;35:426–431. doi: 10.1161/01.STR.0000110982.74967.39. [DOI] [PubMed] [Google Scholar]
- 15.Kittner SJ, White LR, Losonczy KG, Wolf PA, Hebel JR. Black-white differences in stroke incidence in a national sample. The contribution of hypertension and diabetes mellitus. JAMA. 1990;264:1267–70. [PubMed] [Google Scholar]
- 16.Giles WH, Kittner SJ, Hebel JR, Losonczy KG, Sherwin RW. Determinants of black-white differences in the risk of cerebral infarction. The National Health and Nutrition Examination Survey Epidemiologic Follow-up Study. Arch Intern Med. 1995;155:1319–1324. [PubMed] [Google Scholar]
- 17.Rosamond WD, Folsom AR, Chambless LE, Wang CH, McGovern PG, Howard G, Cooper L. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke. 1999;30:736–43. doi: 10.1161/01.str.30.4.736. [DOI] [PubMed] [Google Scholar]
- 18.Arias E, Anderson RN, Kung HC, Murphy SL, Kochanek KD. Deaths: final data for 2001. National vital statistics reports. 3. Vol. 52. National Center for Health Statistics; Hyattsville, Maryland: 2003. [PubMed] [Google Scholar]
- 19.U.S. Census Bureau . State population estimates and demographic components of population change: July 1, 1998 to July 1, 1999. U.S. Census Bureau; Washington, DC: 1999. Available at: http://www.census.gov/population/estimates/state/st-99-1.txt. [Google Scholar]
- 20.Shryock HS, Siegel JS. The methods and materials of demography. Academic Press; New York: 1976. [Google Scholar]
- 21.Centers for Disease Control and Prevention . Deaths from 358 selected causes by 5-year age groups, race, and sex: each state and the District of Columbia, 1999-2001. CDC, National Center for Health Statistics; Hyattsville, MD: Available at: http://www.cdc.gov/nchs/data/statab/mortfinal2001_workIIIpt4v.pdf. [Google Scholar]
- 22.Matchar DB, Ducan PW. Cost of stroke. Stroke Clin Updates. 1994;5:9–12. [Google Scholar]
- 23.Howard VJ, Cushman M, Pulley L, Gomez C, Go R, Prineas RJ, Graham A, Moy CS, Howard G. The REasons for Geographic And Racial Differences in Stroke (REGARDS) Study: Objectives and Design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 24.U.S. Census Bureau . GCT-P6. Race and Hispanic or Latino: 2000: data set: census 2000 summary file 1 (SF 1) 100-percent data. Bureau of the Census; Washington, DC: 2000. Available at http://factfinder.census.gov/servlet/GCTTable?_bm=y&-geo_id=01000US&-_box_head_nbr=GCT-P6&-ds_name=DEC_2000_SF1_U&-format=US-9. [Google Scholar]
- 25.Brewer CA, Suchan TA. Census Special Reports, Series CENSR/01-1: Mapping census 2000: the geography of U.S. diversity. Government Printing Office; Washington, DC: 2001. [Google Scholar]
- 26.Yang D, Howard G, Coffey CS, Roseman J. The confounding of race and geography: how much of the excess stroke mortality among African Americans is explained by geography? Neuroepidemiology. 2004;23:118–22. doi: 10.1159/000075954. [DOI] [PubMed] [Google Scholar]
- 27.Howard G, Prineas R, Moy C, Cushman M, Kellum M, Temple E, Graham A, Howard VJ. Racial and Geographic Differences in Awareness, Treatment and Control of Hypertension: The REasons for Geographic And Racial Differences in Stroke (REGARDS) Study. Stroke. 2006:1171–1178. doi: 10.1161/01.STR.0000217222.09978.ce. [DOI] [PubMed] [Google Scholar]
- 28.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment and control of hypertension in the United States, 1988-2000. JAMA. 2003;290:199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 29.Kleindorfer D, Safford M, Cantrell, Howard J, McClure L, Howard Socioeconomic status and control of stroke risk factors: The REasons for Geographic And Racial Differences in Stroke Study. Stroke. 2006;37:668. (abstract) [Google Scholar]