Cowden disease (CD) is a rare autosomal dominant disease with variable expression, affecting a number of systems in the form of multiple hamartomatous neoplasms of ectodermal, mesodermal, and endodermal origin1 (multiple hamartoma neoplasia syndrome). CD usually presents in late adolescence and is caused by a germ mutation in the PTEN gene.2 Classically, the mucocutaneous features of CD are tricholemmomas, oral fibromas, acral keratoses, palmar pits, and gingival and palatal papules. These mucocutaneous signs are important markers for systemic findings; in particular breast carcinoma (20%), which is often bilateral,3,4 thyroid carcinoma (8%) and endometrial carcinomas.2 Various manifestations of the central nervous system (mental retardation,5 seizures, ganglinoneuromas), musculoskeletal system (craniomegaly, kyphoscoliosis and high arched palate) and gastrointestinal system (multiple hamartomatous polyps, adenocarcinomas arising in the polyps) are well documented. In addition, ovarian cysts and menstrual abnormalities are known to occur in the female genital tract.6
Bannayan–Ruvalcaba–Riley syndrome has many clinical features in common with CD, including mucocutaneous manifestations and an increased risk of gastrointestinal polyps and malignancy.7 Several other similar phenotypes caused by mutations in the PTEN gene have been described After studying 64 unrelated families with Cowden‐like features, Marsh et al proposed that these different entities lie within a spectrum; they referred to these conditions as the PTEN hamartoma tumour syndrome (PHTS).7,8,9
We report a case of an 18‐year‐old man of Fitzpatrick type 1 skin and freckles who developed a non‐tender, 10 mm erythematous nodule on his back over few months. The clinical differential diagnosis included an amelanotic melanoma, vascular tumour or a dermatofibroma. His past medical history included Pierre Robin syndrome (the triad of glossoptosis (downward displacement of the tongue), micrognathia (small jaw) and cleft palate), moderately severe learning difficulties and dyspraxia.
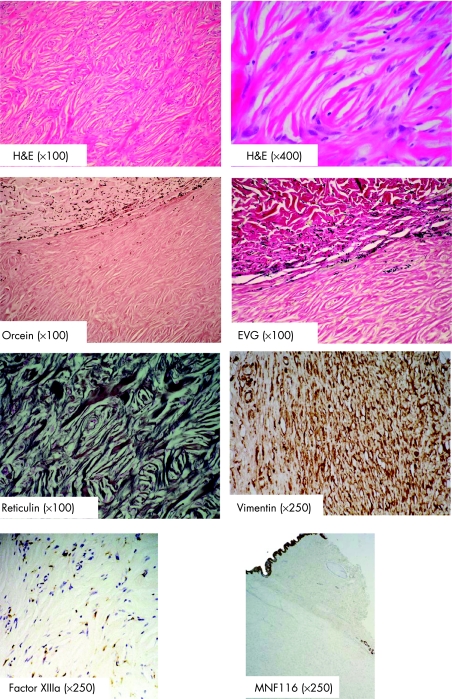
The nodule was excised. Microscopic examination (fig 1) showed a paucicellular (although a cellular variant has been reported10) well‐circumscribed dermal nodule composed chiefly of collagen bundles with a distinctive interweaving, storiform pattern with prominent elongated clefts between them, typical of a storiform collagenoma.11 Tinctorial stains showed absence of elastic fibres (Orcein and EVG) within the lesion and reticulin fibres were seen prominently (Reticulin). Immunohistochemistry showed negative staining with CEA, EMA or keratin staining. Most of the cells within the nodule stained positively for vimentin, and factor XIIIa stain highlighted scattered dermal dendritic cells.11 On the basis of similar fibrotic changes observed in dermatofibroma, it has been speculated that storiform collagenoma may have diverse origins. This issue has been resolved by showing that type 1 collagen synthesis indicates fibroblastic origin of storiform collagenoma.12 Furthermore, storiform collagenoma is distinguished from dermatofibrom by an epidermis overlying amorphous, eosinophilic bundles in a laminated pattern extending into the deep dermis.13,14
Figure 1 Histopathological and immunohistochemical typical appearance of circumscribed storiform collagenoma (original magnification indicated in brackets).
Storiform collagenoma has been described in association with CD but can also arise sporadically.11 It occurs most often in young and middle‐aged adults6 and usually presents as a slow growing solitary nodule up to 1 cm in diameter on the head and neck or upper extremities. Typical histopathological, histochemical and immunohistochemical appearances as described by Metcalf et al11 were present in our patient.
The combination of a storiform collagenoma and mental retardation in our patient raised the possibility of CD/PHTS. Further clinical evaluation identified numerous shiny papules on the buccal mucosa and gingival, giving a deeply furrowed (“scrotal”) tongue (fig 2A) and a “cobblestone” appearance to the buccal mucosa (fig 2B). There were no facial or acral lesions and no skeletal abnormalities. There were no other cutaneous lesions. His younger brother and maternal aunt also had mild learning difficulties. Chromosomal analysis for mutation in the suspected PTEN gene on chromosome 10p23 is awaited to confirm the clinical diagnosis of storiform collagenoma in association with CD.
Figure 2 (A) Deeply furrowed (scrotal) tongue. (B) “Cobblestone” appearance of the buccal mucosa. Informed consent was obtained for publication of this figure.
In our case, the first presenting feature of CD was with a histologically diagnosed storiform collagenoma. Subsequent clinical examination raised the suspicion of CD.
Serious systemic complications of CD include carcinomas of the thyroid, breast and endometrium. Genetic counselling and appropriate screening of index cases and family members is advocated.
Multiple trichilemmomas have been classically regarded as the cutaneous hallmark of CD.15 We here emphasise that storiform collagenoma of the skin is another cutaneous clue of this entity, which may also be helpful in an early diagnosis. To the best of our knowledge, this is the first report in the English literature where a circumscribed storiform collagenoma has led to this important diagnosis, highlighting the importance of the awareness of cutaneous manifestations of systemic diseases.
In summary, a thorough systemic examination is of paramount importance in CD, which usually presents with cutaneous manifestations, as the patients and their relatives are at risk of developing serious medical conditions.
Finally, we report the first case where a circumscribed storiform collagenoma lead to the diagnosis of CD/PHTS; the patient and his relatives are receiving genetic counselling.
Acknowledgements
The authors thank Mr Roy Indrasenan for his great help during preparation of this manuscript.
Footnotes
Competing interests: None declared.
References
- 1.Lloyd K M, 2nd, Dennis M. Cowden's disease. A possible new symptom complex with multiple system involvement. Ann Intern Med 196358136–142. [DOI] [PubMed] [Google Scholar]
- 2.Hanssen A M, Fryns J P. Cowden syndrome. J Med Genet 199532117–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schrager C A, Schneider D, Gruener A C.et al Clinical and pathological features of breast disease in Cowden's syndrome: an underrecognized syndrome with an increased risk of breast cancer. Hum Pathol 19982947–53. [DOI] [PubMed] [Google Scholar]
- 4.Schrager C A, Schneider D, Gruener A C.et al Similarities of cutaneous and breast pathology in Cowden's syndrome. Exp Dermatol 19987380–390. [DOI] [PubMed] [Google Scholar]
- 5.Padberg G W, Schot J D, Vielvoye G J.et al Lhermitte‐Duclos disease and Cowden disease: a single phakomatosis. Ann Neurol 199129517–523. [DOI] [PubMed] [Google Scholar]
- 6.Starink T M, van der Veen J P, Arwert F.et al The Cowden syndrome: a clinical and genetic study in 21 patients. Clin Genet 198629222–233. [DOI] [PubMed] [Google Scholar]
- 7.Marsh D J, Kum J B, Lunetta K L.et al PTEN mutation spectrum and genotype‐phenotype correlations in Bannayan‐Riley‐Ruvalcaba syndrome suggest a single entity with Cowden syndrome. Hum Mol Genet 199981461–1472. [DOI] [PubMed] [Google Scholar]
- 8.Weary P E, Gorlin R J, Gentry W C., Jret al Multiple hamartoma syndrome (Cowden's disease). Arch Dermatol 1972106682–690. [PubMed] [Google Scholar]
- 9.Barax C N, Lebwohl M, Phelps R G. Multiple hamartoma syndrome. J Am Acad Dermatol 198717342–346. [DOI] [PubMed] [Google Scholar]
- 10.Rudolph P, Schubert C, Parwaresch R. Cellular storiform collagenoma. Am J Dermatopathol 200325167–171. [DOI] [PubMed] [Google Scholar]
- 11.Metcalf J S, Maize J C, LeBoit P E. Circumscribed storiform collagenoma (sclerosing fibroma). Am J Dermatopathol 199113122–129. [DOI] [PubMed] [Google Scholar]
- 12.Shitabata P K, Crouch E C, Fitzgibbon J F.et al Cutaneous sclerotic fibroma. Immunohistochemical evidence of a fibroblastic neoplasm with ongoing type I collagen synthesis. Am J Dermatopathol 199517339–343. [DOI] [PubMed] [Google Scholar]
- 13.Pujol R M, de Castro F, Schroeter A L.et al Solitary sclerotic fibroma of the skin: a sclerotic dermatofibroma? Am J Dermatopathol 199618620–624. [DOI] [PubMed] [Google Scholar]
- 14.Starink T M, Meijer C J, Brownstein M H. The cutaneous pathology of Cowden's disease: new findings. J Cutan Pathol 19851283–93. [DOI] [PubMed] [Google Scholar]
- 15.Requena L, Gutierrez J, Sanchez Y E. Multiple sclerotic fibromas of the skin. A cutaneous marker of Cowden's disease. J Cutan Pathol 199219346–351. [DOI] [PubMed] [Google Scholar]