Myiasis (Myia: “Fly” in Greek), the term coined by Hope in 18401,2 is the infestation of living body tissues of animals by fly larvae.3,4,5 In 1965, Zumpt1 defined it as infestation of live humans and vertebrates with dipterous larvae, which at least for a certain period feed on the host's dead or living tissue, liquid body substances or ingested food.1 Flies causing myiasis belong to the order Diptera.1,2
In orofacial myiasis, soft tissues of the oral cavity are invaded by parasitic larvae of flies. Lawrence1 first described oral myiasis in 1909.1 It has been reported mainly in developing countries such as those of Asia and very rarely in developed countries.1
We present the case of a patient in whom orofacial myiasis was accidentally discovered during histopathological examination. A 63‐year‐old woman reported with swelling in the left cheek, gradually increasing in size for 1 year. On clinical examination, the swelling measured 3×2 cm and was firm, irregular in shape and of rough texture. It was located submucosally, deep in the buccinator muscle. The patient's medical history, review of symptoms and family history were non‐contributory.
A clinical diagnosis of minor salivary gland adenoma was carried out. During surgery, on surgical excision, the surgeon noticed nothing unusual.
Histopathological examination revealed parasite sections submucosally. The sections showed fibrous tissue with florid, diffuse, mixed inflammatory cell infiltrate of chronic inflammatory cells, eosinophils and multinucleated giant cells. These cells were concentrated around the dead hyalinised larvae, suggestive of parasitic infection (fig 1).
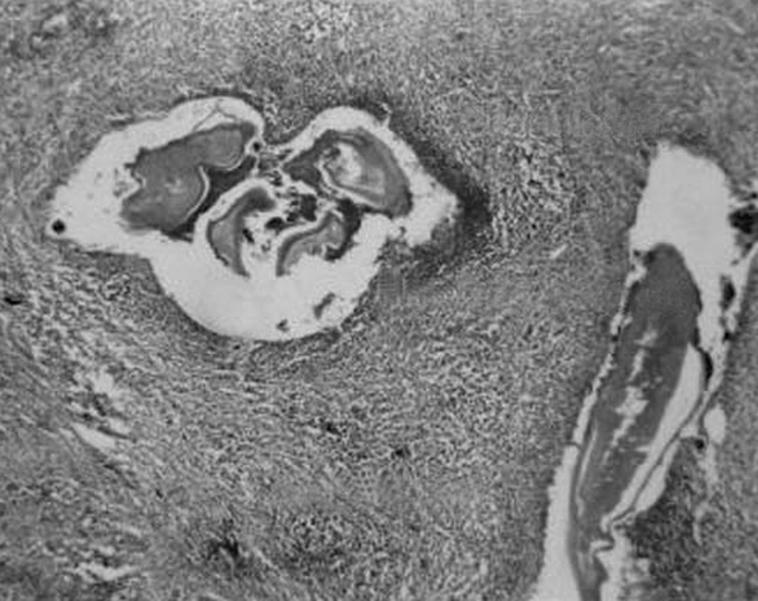
Figure 1 A photomicrograph showing dead hyalinised larvae along with their cuticles. The worms are surrounded by mixed inflammatory cell infiltrate, consisting mainly of lymphocytes, with few plasma cells and eosinophils (H&E staining, ×4).
Oral involvement in myiasis has been reported in extraction wounds, in patients with epilepsy who sustained trauma in the facial area without attention being given to the wounds, in people with very poor oral hygiene and in mouth breathers and thumb suckers where the mouth is kept open during sleep.3
In the presence of favourable conditions, the female fly deposits eggs. After hatching, the larvae develop in the warm, moist environment, burrow into oral tissues, obtain nutrition and grow larger. This causes progressive tissue destruction and cavitation. The subsequent host‐tissue reaction produces a fibrous capsule to which the larvae adhere. The larvae may also move out of the tissue through small orifices1 or may get entrapped in a closed space and die, and eventually get hyalinised, which was evident in the present case.
For the diagnosis of oral myiasis, a thorough history including recent travel and occupation is important, as the lesion, although rare overall, is reported more in the tropics,1 especially during summer. The possibility of oral myiasis should come to mind in relation to oral mucosal swellings with no apparent diagnosis in patients from areas where parasites that cause myiasis are endemic. Even though it is an infrequently reported disease in humans, the careful histopathological evaluation of every specimen obtained after surgery will help in understanding the aetiology and pathogenesis of such unusual cases.
This case has been reported to sound an alert for suspecting oral myiasis in such clinical settings, in tropical areas or in people travelling to tropical regions.
Footnotes
Competing interests: None.
References
- 1.Bhatt A P, Jayakrishnan A. Oral myiasis: a case report. Int J Paediatr Dent 20001067–70. [DOI] [PubMed] [Google Scholar]
- 2.Gunbay S, Bicakci N, Canda S. A case of myiasis gingiva. J Periodontol 199566892–895. [DOI] [PubMed] [Google Scholar]
- 3.Lata J, Kapila B K, Aggarwal P. Oral myiasis. A case report. Int J Oral Maxillofac Surg 199625455–456. [DOI] [PubMed] [Google Scholar]
- 4.Novelli M R, Haddock A, Eveson J W. Orofacial myiasis. Br J Oral Maxillofac Surg 19933136–37. [DOI] [PubMed] [Google Scholar]
- 5.Bozzo L, Lima I A, de Almeida O P.et al Oral myiasis caused by sarcophagidae in an extraction wound. Oral Surg Oral Med Oral Pathol 199274733–735. [DOI] [PubMed] [Google Scholar]


